Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (11): 2456-2465.doi: 10.12122/j.issn.1673-4254.2025.11.18
Previous Articles Next Articles
Qingqing HUANG1,4( ), Jingjing YANG4, Xuening JIANG4, Wenjing ZHANG1, Yu WANG4, Lugen ZUO2,4, Lian WANG2,4, Yueyue WANG1,4, Xiaofeng ZHANG3,4, Xue SONG3,4, Jianguo HU1,4(
), Jingjing YANG4, Xuening JIANG4, Wenjing ZHANG1, Yu WANG4, Lugen ZUO2,4, Lian WANG2,4, Yueyue WANG1,4, Xiaofeng ZHANG3,4, Xue SONG3,4, Jianguo HU1,4( )
)
Received:2025-04-15
Online:2025-11-20
Published:2025-11-28
Contact:
Jianguo HU
E-mail:hqq10100@163.com;jghu9200@bbmc.edu.cn
Qingqing HUANG, Jingjing YANG, Xuening JIANG, Wenjing ZHANG, Yu WANG, Lugen ZUO, Lian WANG, Yueyue WANG, Xiaofeng ZHANG, Xue SONG, Jianguo HU. Hypaphorine alleviates Crohn's disease-like colitis in mice by inhibiting intestinal epithelial inflammatory response and protecting intestinal barrier function[J]. Journal of Southern Medical University, 2025, 45(11): 2456-2465.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.11.18
| Gene name | Primer sequences |
|---|---|
| TNF-α | Forward:5'-CAGGCGGTGCCTATGTCTC-3' |
| Reverse:5'-CGATCACCCCGAAGTTCAGTAG-3' | |
| IL-6 | Forward:5'-TCTATACCACTTCACAAGTCGGA-3' |
| Reverse:5'-GAATTGCCATTGCACAACTCTTT-3' | |
| IL-1β | Forward:5'-GAAATGCCACCTTTTGACAGTG-3' |
| Reverse:5'-TGGATGCTCTCATCAGGACAG-3' | |
| GAPDH | Forward:5'-AGGTCGGTGTGAACGGATTTG-3' |
| Reverse:5'-GGGGTCGTTGATGGCAACA-3' |
Tab.1 Primer sequences for qRT-PCR in this study
| Gene name | Primer sequences |
|---|---|
| TNF-α | Forward:5'-CAGGCGGTGCCTATGTCTC-3' |
| Reverse:5'-CGATCACCCCGAAGTTCAGTAG-3' | |
| IL-6 | Forward:5'-TCTATACCACTTCACAAGTCGGA-3' |
| Reverse:5'-GAATTGCCATTGCACAACTCTTT-3' | |
| IL-1β | Forward:5'-GAAATGCCACCTTTTGACAGTG-3' |
| Reverse:5'-TGGATGCTCTCATCAGGACAG-3' | |
| GAPDH | Forward:5'-AGGTCGGTGTGAACGGATTTG-3' |
| Reverse:5'-GGGGTCGTTGATGGCAACA-3' |

Fig.1 HYP treatment alleviates CD-like colitis in TNBS-treated mice. A: Body weight changes. B: DAI score. C: Gross observation of the dissected colon from each groups. D: Colon length in each group. E: HE staining of colonic sections of the mice from each group (scale bar=1 mm or 100 μm). F: Colonic inflammation scores in each group. *P<0.05 vs WT, #P<0.05 vs TNBS.

Fig.2 HYP treatment reduces the levels of inflammatory mediators in the colonic mucosa of TNBS-treated mice. A-C: Expression levels of TNF-α, IL-6 and IL-1β mRNAs in mouse colonic mucosal tissue. D-F: Expression levels of TNF-α, IL-6 and IL-1β proteins in mouse colonic mucosal tissue. *P<0.05 vs WT, #P<0.05 vs TNBS.

Fig.3 HYP ameliorates intestinal barrier damage in TNBS-treated mice. A: TEER values of mouse colon tissues in each group. B-D: Bacterial translocation rate in the mesenteric lymph nodes, liver, and spleen. E, F: Serum levels of I-FABP and FD4 in each group. G: AB-PAS and immunohistochemical staining of colonic sections (scale bar=100 μm). H, I: Number of goblet cells per crypt and MUC2 expression level in mouse colon tissue in the 3 groups. J, L: Immunofluorescence staining of colonic sections from each group (scale bar=100 μm). K, M: Expression levels of claudin-1 and ZO-1 in mouse colon tissues in each group. *P<0.05 vs WT, #P<0.05 vs TNBS.
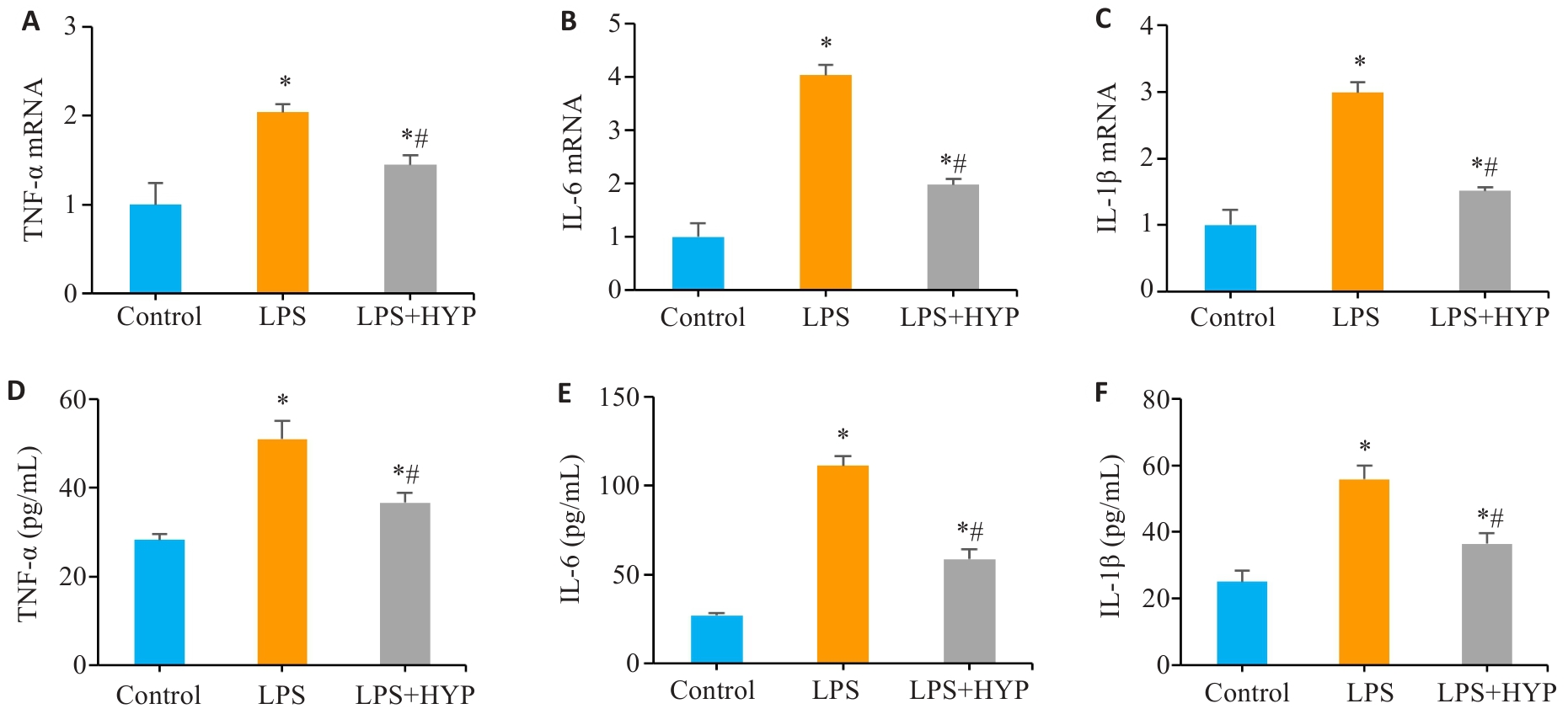
Fig.4 HYP treatment reduces inflammatory mediator levels in LPS-induced Caco-2 cells. A-C: Expression levels of TNF-α, IL-6 and IL-1β mRNAs in Caco-2 cells with different treatments. D-F: Protein levels of TNF-α, IL-6 and IL-1β in Caco-2 cells with different treatments. *P<0.05 vs Control, #P<0.05 vs LPS.
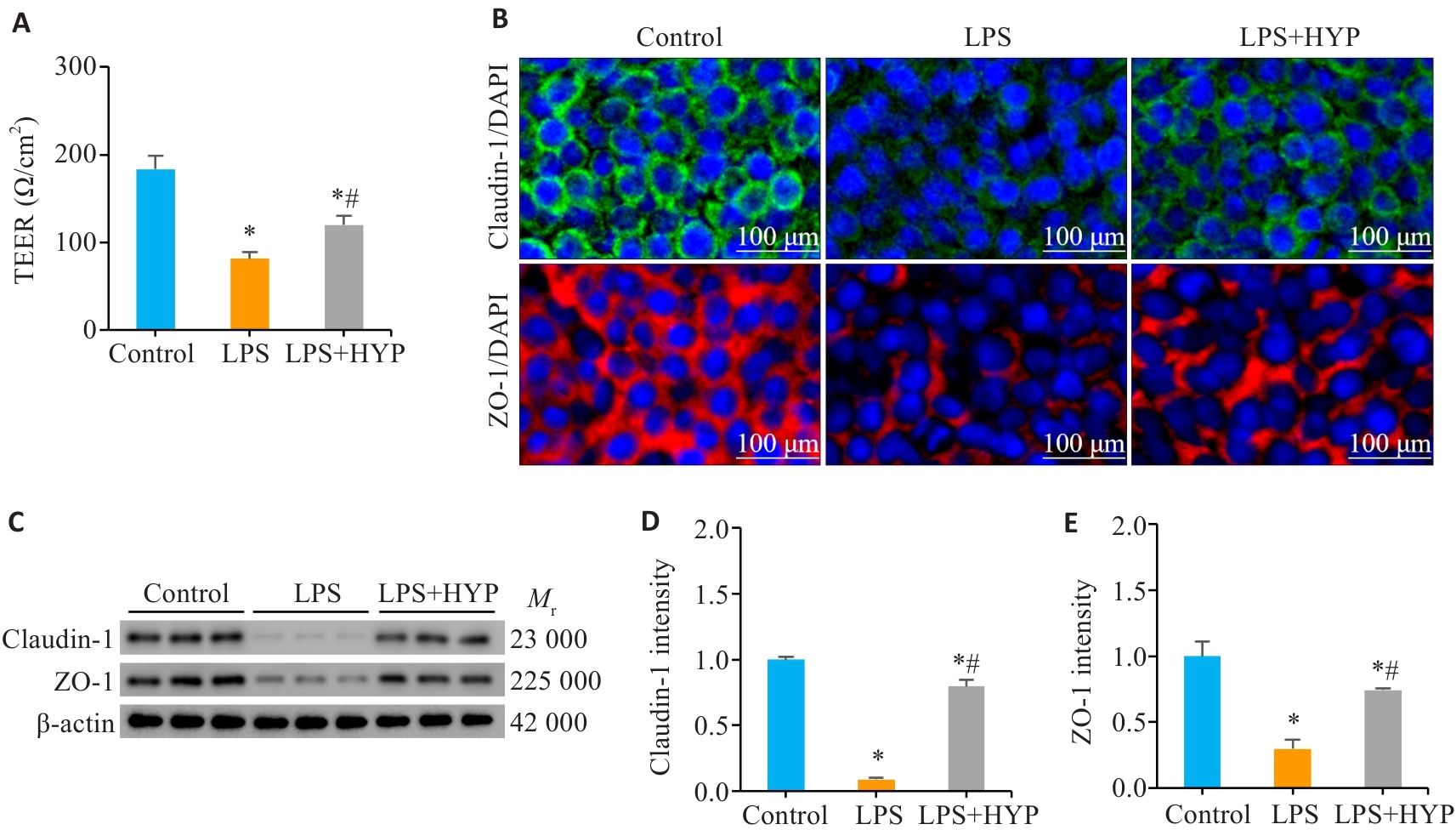
Fig.5 HYP treatment ameliorates LPS-induced barrier damage in Caco-2 cells. A: TEER value of Caco-2 cells. B: Immunofluorescence staining of Caco-2 cells with different treatments (scale bar=100 μm). C-E: Expression levels of claudin-1 and ZO-1 in Caco-2 cells with different treatments. *P<0.05 vs Control, #P<0.05 vs LPS.
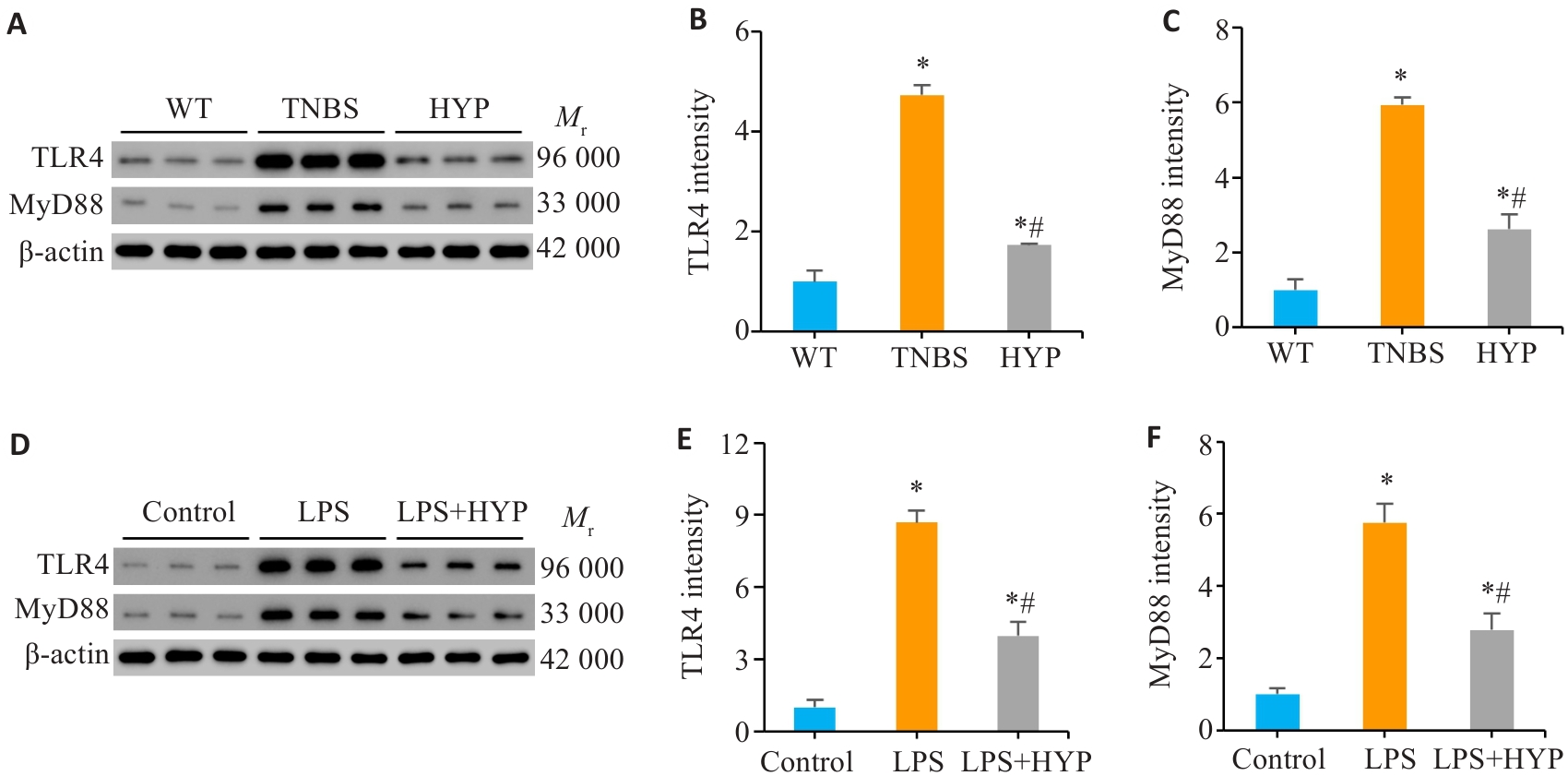
Fig.7 HYP downregulates the TLR4/MyD88 signaling pathway in both the mouse and cell models. A-C: Protein levels of TLR4 and MyD88 in mouse colonic mucosa tissues. D-F: Protein levels of TLR4 and MyD88 in Caco-2 cells with different treatments. *P<0.05 vs WT or Control, #P<0.05 vs TNBS or LPS.
| [1] | Torres J, Mehandru S, Colombel JF, et al. Crohn's disease[J]. Lancet, 2017, 389(10080): 1741-55. doi:10.1016/s0140-6736(16)31711-1 |
| [2] | Roda G, Chien Ng S, Kotze PG, et al. Crohn's disease[J]. Nat Rev Dis Primers, 2020, 6(1): 22. doi:10.1038/s41572-020-0156-2 |
| [3] | Leibovitzh H, Lee SH, Raygoza Garay JA, et al. Immune response and barrier dysfunction-related proteomic signatures in preclinical phase of Crohn's disease highlight earliest events of pathogenesis[J]. Gut, 2023, 72(8): 1462-71. doi:10.1136/gutjnl-2022-328421 |
| [4] | Song X, Zhang XF, Zhang M, et al. The JNK/P38 signalling pathway activated by testin protects the intestinal epithelial barrier against Crohn's disease-like colitis[J]. Chem Biol Interact, 2024, 403: 111222. doi:10.1016/j.cbi.2024.111222 |
| [5] | Yang Y, Guo LQ, Wei L, et al. Da-Yuan-Yin decoction alleviates ulcerative colitis by inhibiting complement activation, LPS-TLR4/NF‑κB signaling pathway and NET formation[J]. J Ethno-pharmacol, 2024, 332: 118392. doi:10.1016/j.jep.2024.118392 |
| [6] | Wang Y, Li M, Zha AS. Adjuvant treatment of Crohn's disease with traditional Chinese medicine: a meta-analysis[J]. Evid Based Complement Alternat Med, 2019, 2019: 6710451. doi:10.1155/2019/6710451 |
| [7] | Gomollón F, Dignass A, Annese V, et al. 3rd European evidence-based consensus on the diagnosis and management of Crohn's disease 2016: part 1: diagnosis and medical management[J]. J Crohns Colitis, 2017, 11(1): 3-25. doi:10.1093/ecco-jcc/jjw168 |
| [8] | Spinelli A, Sacchi M, Fiorino G, et al. Risk of postoperative recurrence and postoperative management of Crohn's disease[J]. World J Gastroenterol, 2011, 17(27): 3213-9. |
| [9] | Cushing K, Higgins PDR. Management of crohn disease: a review[J]. JAMA, 2021, 325(1): 69-80. doi:10.1001/jama.2020.18936 |
| [10] | Doherty G, Katsanos KH, Burisch J, et al. European Crohn's and colitis organisation topical review on treatment withdrawal ['Exit strategies'] in inflammatory bowel disease[J]. J Crohns Colitis, 2018, 12(1): 17-31. doi:10.1093/ecco-jcc/jjx101 |
| [11] | Barnes EL. Postoperative Crohn's disease management[J]. Curr Opin Gastroenterol, 2020, 36(4): 277-83. doi:10.1097/mog.0000000000000638 |
| [12] | Xie J, Huang Y, Wu HG, et al. Acupuncture and moxibustion for treatment of Crohn's disease: a brief review[J]. World J Gastroenterol, 2022, 28(25): 3001-3. doi:10.3748/wjg.v28.i25.3001 |
| [13] | Yuan S, Li Y, Li J, et al. Traditional Chinese medicine and natural products: potential approaches for inflammatory bowel disease[J]. Front Pharmacol, 2022, 13: 892790. doi:10.3389/fphar.2022.892790 |
| [14] | Sałaga M, Zatorski H, Sobczak M, et al. Chinese herbal medicines in the treatment of IBD and colorectal cancer: a review[J]. Curr Treat Options Oncol, 2014, 15(3): 405-20. doi:10.1007/s11864-014-0288-2 |
| [15] | Zhang ZN, Zuo LG, Song X, et al. Arjunolic acid protects the intestinal epithelial barrier, ameliorating Crohn’s disease-like colitis by restoring gut microbiota composition and inactivating TLR4 signalling[J]. Phytomedicine, 2024, 123: 155223. doi:10.1016/j.phymed.2023.155223 |
| [16] | 马博凯, 钱 冲, 王茂媛, 等. 超高效液相色谱-串联质谱法测定药材牛大力中刺桐碱、芒柄花素和高丽槐素[J]. 分析科学学报, 2022, 38(2): 203-8. |
| [17] | 曹斯琼, 吴文平, 罗宇琴, 等. 王不留行炮制前后的UPLC指纹图谱比较及刺桐碱和王不留行黄酮苷的含量测定[J]. 中国药房, 2020, 31(19): 2365-70. |
| [18] | Sun H, Zhu X, Cai W, et al. Hypaphorine attenuates lipopolysaccharide-induced endothelial inflammation via regulation of TLR4 and PPAR-γ dependent on PI3K/Akt/mTOR signal pathway[J]. Int J Mol Sci, 2017, 18(4): E844. doi:10.3390/ijms18040844 |
| [19] | Ding YH, Miao RX, Zhang Q. Hypaphorine exerts anti-inflammatory effects in sepsis induced acute lung injury via modulating DUSP1/p38/JNK pathway[J]. Kaohsiung J Med Sci, 2021, 37(10): 883-93. doi:10.1002/kjm2.12418 |
| [20] | Li QQ, Li J, Yin LX, et al. Sophoricoside improved Crohn's disease-like colitis by inhibiting intestinal epithelial cell apoptosis through PI3K/AKT signaling[J]. Int Immunopharmacol, 2024, 131: 111886. doi:10.1016/j.intimp.2024.111886 |
| [21] | Zhang Y, Huang J, Gan L, et al. Hepatoprotective effects of Niudali (Callerya speciosa) root aqueous extracts against tetrachloro-methane-induced acute liver injury and inflammation[J]. Food Sci Nutr, 2023, 11(11): 7026-38. doi:10.1002/fsn3.3626 |
| [22] | 蔡维维, 侯 豹, 陈旭红, 等. 王不留行中刺桐碱的分离鉴定及抗炎活性研究[J]. 天然产物研究与开发, 2018, 30(4): 616-20. |
| [23] | Wang L, Song X, Zhou YQ, et al. Sclareol protected against intestinal barrier dysfunction ameliorating Crohn's disease-like colitis via Nrf2/NF-B/MLCK signalling[J]. Int Immunopharmacol, 2024, 133: 112140. doi:10.1016/j.intimp.2024.112140 |
| [24] | Yang T, Liu DD, Li YL, et al. Chemoproteomics reveals Sofalcone inhibits the inflammatory response of Caco-2 cells by covalently targeting HMGB1[J]. Chem Commun, 2023, 59(58): 8981-4. doi:10.1039/d3cc00577a |
| [25] | Geng Z, Zuo L, Li J, et al. Ginkgetin improved experimental colitis by inhibiting intestinal epithelial cell apoptosis through EGFR/PI3K/AKT signaling[J]. FASEB J, 2024, 38(14): e23817. doi:10.1096/fj.202400211rr |
| [26] | Neurath M, Fuss I, Strober W. TNBS-colitis[J]. Int Rev Immunol, 2000, 19(1): 51-62. doi:10.3109/08830180009048389 |
| [27] | Antoniou E, Margonis GA, Angelou A, et al. The TNBS-induced colitis animal model: an overview[J]. Ann Med Surg, 2016, 11: 9-15. doi:10.1016/j.amsu.2016.07.019 |
| [28] | 蔡维维, 张仕杰, 文嫄媛, 等. 刺桐碱促伤口愈合的网络药理学分析及实验验证[J]. 天然产物研究与开发, 2024, 36(11):1959-71,1958. |
| [29] | Matar A, Damianos JA, Jencks KJ, et al. Intestinal barrier impairment, preservation, and repair: an update[J]. Nutrients, 2024, 16(20): 3494. doi:10.3390/nu16203494 |
| [30] | Neurath MF, Artis D, Becker C. The intestinal barrier: a pivotal role in health, inflammation, and cancer[J]. Lancet Gastroenterol Hepatol, 2025, 10(6): 573-92. doi:10.1016/s2468-1253(24)00390-x |
| [31] | Qiao YR, He CE, Xia YX, et al. Intestinal mucus barrier: a potential therapeutic target for IBD[J]. Autoimmun Rev, 2025, 24(2): 103717. doi:10.1016/j.autrev.2024.103717 |
| [32] | Wang Z, Shen J. The role of goblet cells in Crohn' s disease[J]. Cell Biosci, 2024, 14(1): 43. doi:10.1186/s13578-024-01220-w |
| [33] | Macura B, Kiecka A, Szczepanik M. Intestinal permeability disturbances: causes, diseases and therapy[J]. Clin Exp Med, 2024, 24(1): 232. doi:10.1007/s10238-024-01496-9 |
| [34] | Luo X, Yu Z, Deng C, et al. Baicalein ameliorates TNBS-induced colitis by suppressing TLR4/MyD88 signaling cascade and NLRP3 inflammasome activation in mice[J]. Sci Rep, 2017, 7(1): 16374. doi:10.1038/s41598-017-12562-6 |
| [35] | Li CZ, Xi YB, Li S, et al. Berberine ameliorates TNBS induced colitis by inhibiting inflammatory responses and Th1/Th17 differentiation[J]. Mol Immunol, 2015, 67(2): 444-54. doi:10.1016/j.molimm.2015.07.013 |
| [36] | Shen JC, Qi Q, Han D, et al. Moxibustion improves experimental colitis in rats with Crohn's disease by regulating bile acid enterohepatic circulation and intestinal farnesoid X receptor[J]. J Integr Med, 2023, 21(2): 194-204. doi:10.1016/j.joim.2023.01.001 |
| [37] | Stephens M, von der Weid PY. Lipopolysaccharides modulate intestinal epithelial permeability and inflammation in a species-specific manner[J]. Gut Microbes, 2020, 11(3): 421-32. doi:10.1080/19490976.2019.1629235 |
| [38] | Pereira M, Durso DF, Bryant CE, et al. The IRAK4 scaffold integrates TLR4-driven TRIF and MYD88 signaling pathways[J]. Cell Rep, 2022, 40(7): 111225. doi:10.1016/j.celrep.2022.111225 |
| [39] | Endale M, Park SC, Kim S, et al. Quercetin disrupts tyrosine-phosphorylated phosphatidylinositol 3-kinase and myeloid differentiation factor-88 association, and inhibits MAPK/AP-1 and IKK/NF‑κB-induced inflammatory mediators production in RAW 264.7 cells[J]. Immunobiology, 2013, 218(12): 1452-67. doi:10.1016/j.imbio.2013.04.019 |
| [1] | Rongmao HE, Zeyang FANG, Yunyun ZHANG, Youliang WU, Shixiu LIANG, Tao JI, Kequan CHEN, Siqi WANG. Diagnostic and predictive value of ferroptosis-related genes in patients with ulcerative colitis [J]. Journal of Southern Medical University, 2025, 45(9): 1927-1937. |
| [2] | Chenfei LIU, Wei ZHANG, Yao ZENG, Yan LIANG, Mengting WANG, Mingfang ZHANG, Xinyuan LI, Fengchao WANG, Yanqing YANG. 2,6-dimethoxy-1,4-benzoquinone alleviates dextran sulfate sodium-induced ulcerative colitis in mice by suppressing NLRP3 inflammasome activation [J]. Journal of Southern Medical University, 2025, 45(8): 1654-1662. |
| [3] | Minzhu NIU, Lixia YIN, Tong QIAO, Lin YIN, Keni ZHANG, Jianguo HU, Chuanwang SONG, Zhijun GENG, Jing LI. Ecliptasaponin A ameliorates DSS-induced colitis in mice by suppressing M1 macrophage polarization via inhibiting the JAK2/STAT3 pathway [J]. Journal of Southern Medical University, 2025, 45(6): 1297-1306. |
| [4] | Lin SHEN, Cuihao SONG, Congmin WANG, Xi GAO, Junhong AN, Chengxin LI, Bin LIANG, Xia LI. Risk factors for malnutrition in ulcerative colitis complicated with pyoderma gangrenosum and construction of a lasso regression-based prediction model [J]. Journal of Southern Medical University, 2025, 45(3): 514-521. |
| [5] | Lixia YIN, Minzhu NIU, Keni ZHANG, Zhijun GENG, Jianguo HU, Jiangyan LI, Jing LI. Cimifugin ameliorates Crohn's disease-like colitis in mice by modulating Th-cell immune balance via inhibiting the MAPK pathway [J]. Journal of Southern Medical University, 2025, 45(3): 595-602. |
| [6] | Keni¹ ZHANG, Tong¹ QIAO, Lin¹ YIN, Ju HUANG, Zhijun GENG, Lugen³ ZUO, Jianguo HU, Jing LI. Pinostrobin targets the PI3K/AKT/CCL2 axis in intestinal epithelial cells to inhibit intestinal macrophage infiltration and alleviate dextran sulfate sodium-induced colitis in mice [J]. Journal of Southern Medical University, 2025, 45(10): 2199-2209. |
| [7] | Na ZHAO, Mengdi SHEN, Rui ZHAO, Di AO, Zetan LUO, Yinliang ZHANG, Zhidong XU, Fangtian FAN, Hailun ZHENG. column:Sanguinarine alleviates ulcerative colitis in mice by regulating the Nrf2/NF-κB pathway [J]. Journal of Southern Medical University, 2024, 44(8): 1467-1475. |
| [8] | Guanzheng YU, Weiqiang CHENG, Xing TU, Man ZHANG, Hong LI, Juan NIE. Therapeutic mechanism of Cynanchum wilfordii for ulcerative colitis: an analysis using UPLC-QE-MS, network pharmacology and metabolomics [J]. Journal of Southern Medical University, 2024, 44(8): 1485-1496. |
| [9] | Shuo LIU, Jing LI, Xingwang WU. Swertiamarin ameliorates 2,4,6-trinitrobenzenesulfonic acid-induced colitis in mice by inhibiting intestinal epithelial cell apoptosis [J]. Journal of Southern Medical University, 2024, 44(8): 1545-1552. |
| [10] | Minzhu NIU, Lixia YIN, Ting DUAN, Ju HUANG, Jing LI, Zhijun GENG, Jianguo HU, Chuanwang SONG. Asperosaponin VI alleviates TNBS-induced Crohn's disease-like colitis in mice by reducing intestinal epithelial cell apoptosis via inhibiting the PI3K/AKT/NF-κB signaling pathway [J]. Journal of Southern Medical University, 2024, 44(12): 2335-2346. |
| [11] | Jianguo QIU, Yitong QIU, Guorong LI, Linsheng ZHANG, Xue ZHENG, Yongjiang YAO, Xidan WANG, Haiyang HUANG, Fengmin ZHANG, Jiyan SU, Xuebao ZHENG, Xiaoqi HUANG. Huangqin Decoction alleviates ulcerative colitis in mice by reducing endoplasmic reticulum stress [J]. Journal of Southern Medical University, 2024, 44(11): 2172-2183. |
| [12] | SONG Zejun, DONG Haibin, MA Na, REN Yutang, JIANG Bo. Value of Improved Mayo Endoscopic Score for evaluating treatment efficacy for active ulcerative colitis [J]. Journal of Southern Medical University, 2023, 43(7): 1204-1213. |
| [13] | ZHANG Xuefang, CHEN Yanhua, LI Zongheng, SHANG Jing, YUAN Zeting, DENG Wanli, LUO Ying, HAN Na, YIN Peihao, YIN Jun. Analysis of therapeutic mechanism of Liushen Wan against colitis-associated colorectal cancer based on network pharmacology and validation in mice [J]. Journal of Southern Medical University, 2023, 43(7): 1051-1062. |
| [14] | SHAO Rongrong, YANG Zi, ZHANG Wenjing, ZHANG Nuo, ZHAO Yajing, ZHANG Xiaofeng, ZUO Lugen, GE Sitang. Pachymic acid protects against Crohn's disease-like intestinal barrier injury and colitis in mice by suppressing intestinal epithelial cell apoptosisviainhibiting PI3K/AKT signaling [J]. Journal of Southern Medical University, 2023, 43(6): 935-942. |
| [15] | YANG Zi, ZHAO Tianhao, CHENG Yang, ZHOU Yueqing, LI Yuetong, WANG Xinru, ZHANG Xiaofeng, ZUO Lugen, GE Sitang. Diosmetin regulates intestinal immune balance by inhibiting PI3K/AKT signaling to relieve 2,4,6-trinitrobenzene sulfonic acid-induced Crohn's disease-like colitis in mice [J]. Journal of Southern Medical University, 2023, 43(3): 474-482. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||