Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (12): 2551-2560.doi: 10.12122/j.issn.1673-4254.2025.12.03
Qian ZHANG1( ), Bowen LIU1, Li LEI1, Ye WANG1, Xinyue ZHANG1, Zhangkun MAO1, Peng TANG2, Jinmei ZHANG2, Jiayi YANG1, Yanxi PENG3, Ze LIU4(
), Bowen LIU1, Li LEI1, Ye WANG1, Xinyue ZHANG1, Zhangkun MAO1, Peng TANG2, Jinmei ZHANG2, Jiayi YANG1, Yanxi PENG3, Ze LIU4( )
)
Received:2025-05-01
Online:2025-12-20
Published:2025-12-22
Contact:
Ze LIU
E-mail:zhangqian@xnu.edu.cn;582842343@qq.com
Qian ZHANG, Bowen LIU, Li LEI, Ye WANG, Xinyue ZHANG, Zhangkun MAO, Peng TANG, Jinmei ZHANG, Jiayi YANG, Yanxi PENG, Ze LIU. SERPINE1 overexpression promotes proliferation and paclitaxel resistance of triple-negative breast cancer cells by inducing M2 macrophage polarization[J]. Journal of Southern Medical University, 2025, 45(12): 2551-2560.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.12.03
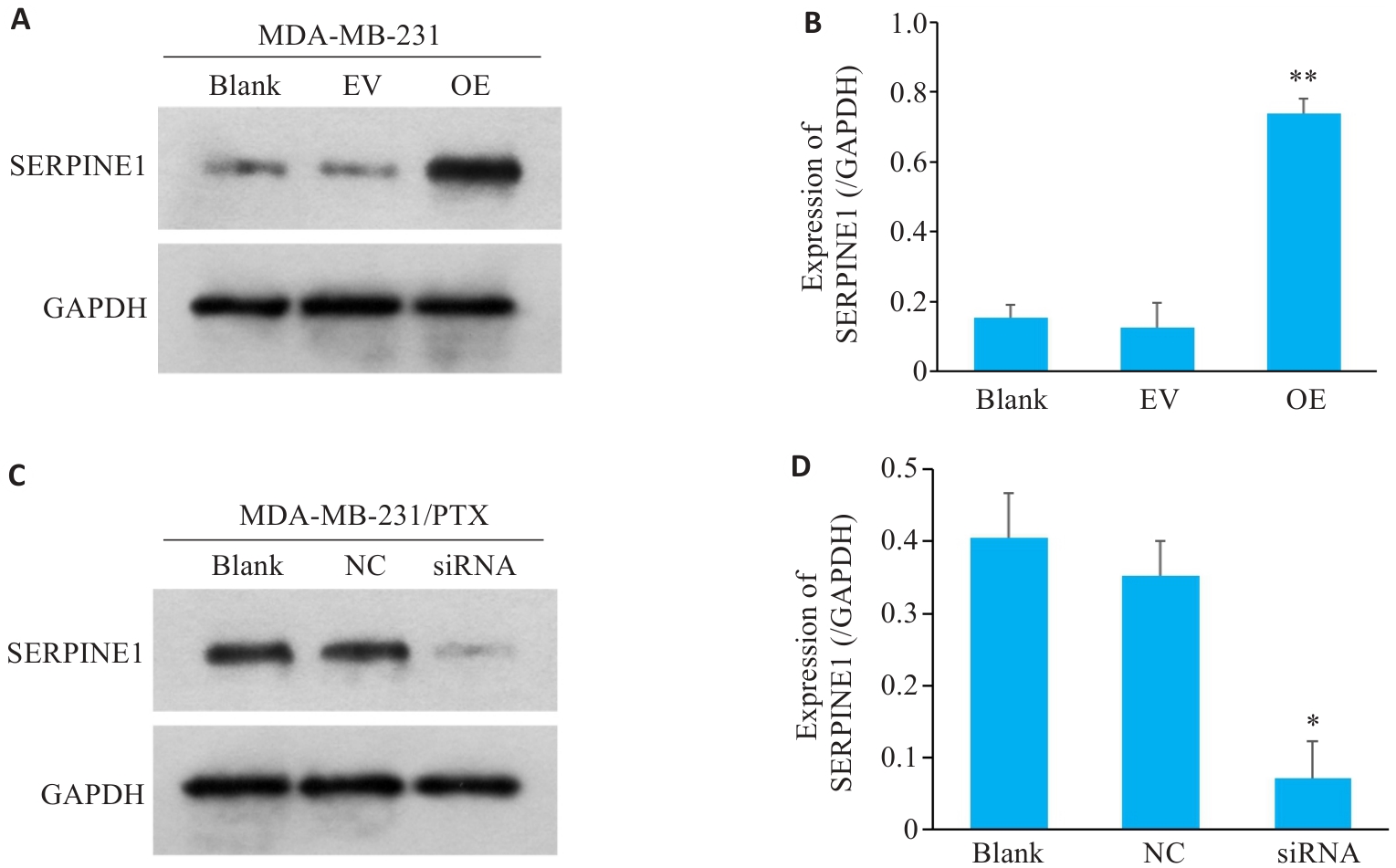
Fig.1 SERPINE1 overexpression in MDA-MB-231 cells and SERPINE1 knockdown in MDA-MB-231/PTX cells. A, B: Western blotting for detecting SERPINE1 protein expression in MDA-MB-231 cells transfected with pcDNA4.0-SERPINE1 and vector plasmid (**P<0.01 vs EV group, n=3); C, D: Western blotting for detecting SERPINE1 protein expression in MDA-MB-231/PTX cells transfected with SERPINE1-siRNA and NC-siRNA. GAPDH was used as the loading control (*P<0.05 vs NC group, n=3).
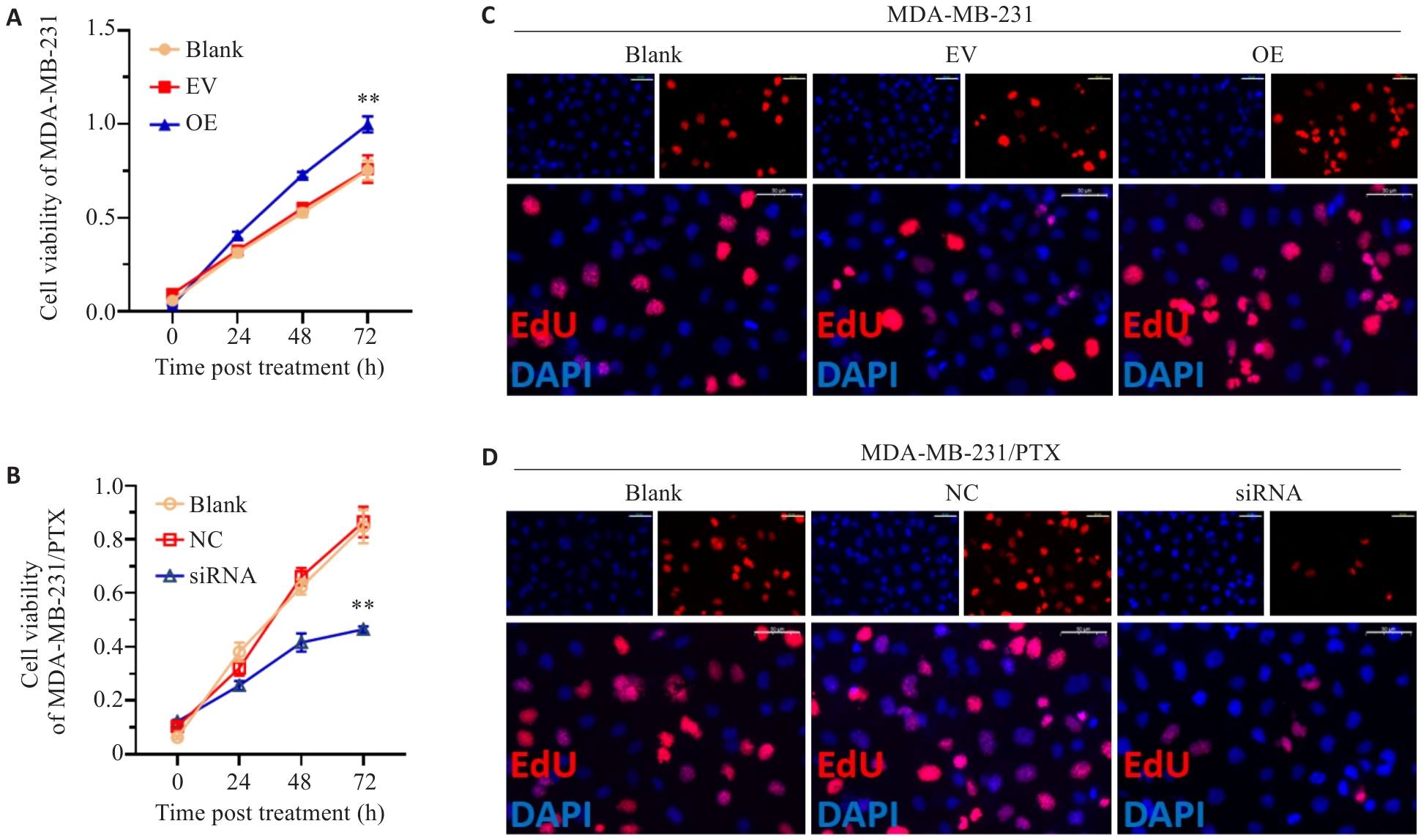
Fig.2 Proliferative activity of MDA-MB-231 cells with SERPINE1 overexpression and MDA-MB-231/PTX cells with SERPINE1 knockdown. A, B: Results of CCK-8 assay of MDA-MB-231 cells (A) transfected with pcDNA4.0-SERPINE1 or the vector plasmid and MDA-MB-231/PTX cells (B) transfected with SERPINE1-siRNA or NC-siRNA (**P<0.01 vs EV group or NC group). C, D: EdU staining of MDA-MB-231 cells with SERPINE1 overexpression and MDA-MB-231/PTX cells with SERPINE1 knockdown (scale bar=50 μm).
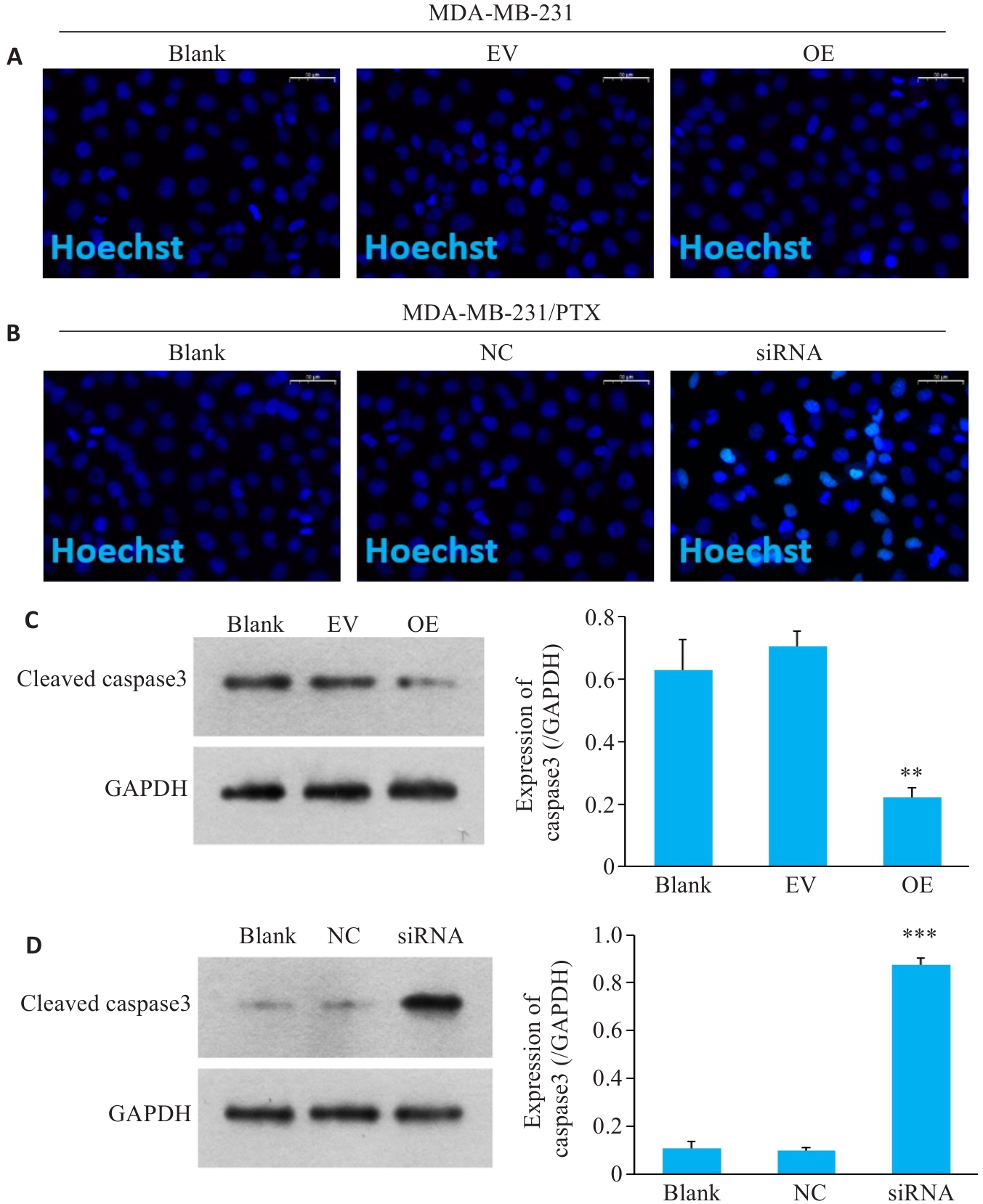
Fig.3 Changes in apoptosis of MDA-MB-231 cells with SERPINE1 overexpression and MDA-MB-231/PTX cells with SERPINE1 knockdown. A, B: DNA damage detected by Hoechst staining in MDA-MB-231 cells with SERPINE1 overexpression and in MDA-MB-231/PTX cells with SERPINE1 knockdown (scale bar=50 μm). C: Western blotting for detecting protein levels of cleaved caspase-3 in MDA-MB-231 cells transfected with pcDNA4.0-SERPINE1 versus the vector plasmid (**P<0.01 vs EV group). D: Western blotting for detecting protein levels of cleaved caspase-3 in MDA-MB-231/PTX cells transfected with SERPINE1-siRNA versus NC-siRNA (***P<0.001 vs NC group, n=3).
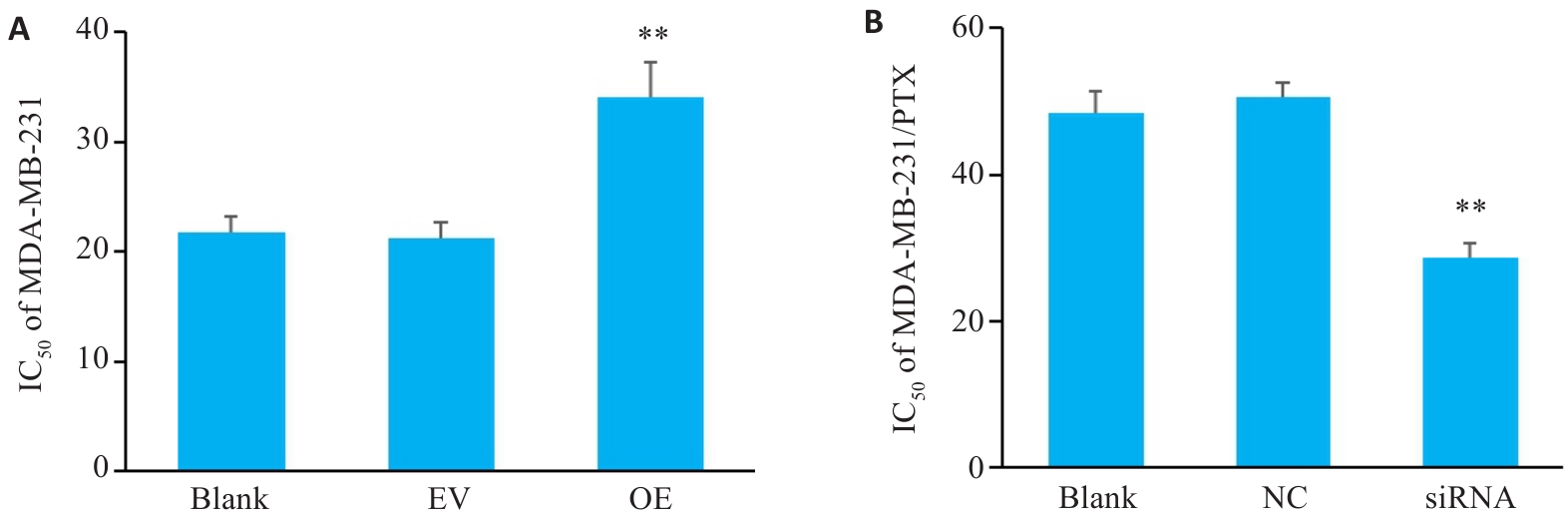
Fig.4 Changes in paclitaxel resistance of MDA-MB-231 cells with SERPINE1 overexpression and MDA-MB-231/PTX cells with SERPINE1 knockdown. A: CCK-8 assay for determining IC50 value of paclitaxel in MDA-MB-231 cells transfected with pcDNA4.0-SERPINE1 versus the vector plasmid (**P<0.01 vs EV group). B: CCK-8 assay for determining the IC50 value of paclitaxel in MDA-MB-231/PTX cells transfected with SERPINE1-siRNA versus NC-siRNA (**P<0.01 vs NC group, n=3).
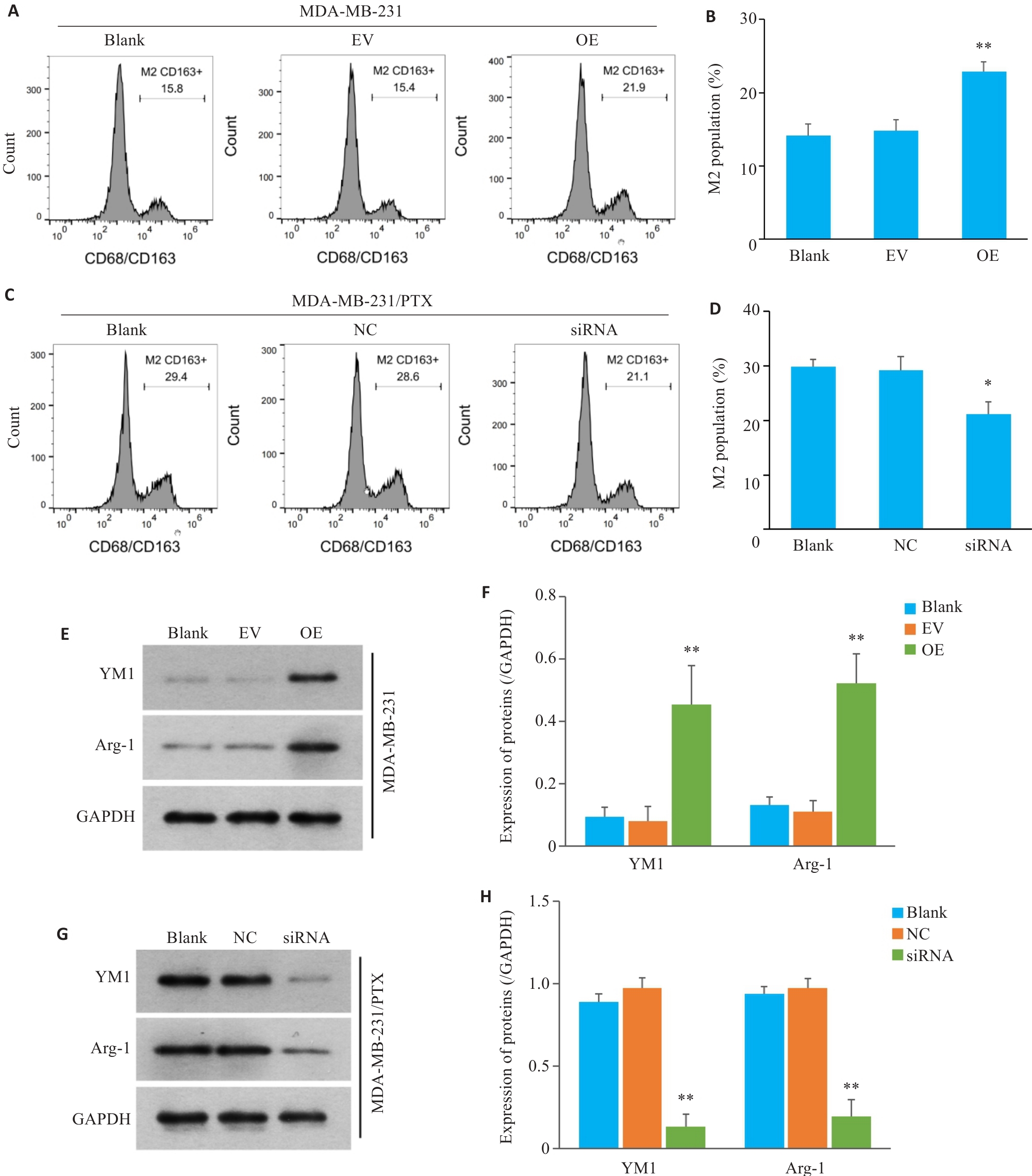
Fig.5 Effect of SERPINE1 overexpression in MDA-MB-231 cells and SERPINE1 knockdown in MDA-MB-231/PTX cells on M2 polarization of the co-cultured macrophages. A, B: Flow cytometry for analyzing the proportion of CD163+ macrophages co-cultured with SERPINE1-overexpressing MDA-MB-231 cells (**P<0.01 vs EV group). C, D: Flow cytometry for analyzing the proportion of CD163+ macrophages co-cultured with MDA-MB-231/PTX cells with SERPINE1 knockdown (*P<0.05 vs NC group). E, F: Western blotting for detecting the protein expression of YM1 and Arg-1 in the macrophages from the microenvironment of MDA-MB-231 cells with or without SERPINE1 overexpression (**P<0.01 vs EV group). G, H: Western blotting for detecting the protein expression of YM1 and Arg-1 in macrophages from the microenvironment of MDA-MB-231/PTX cells with or without SERPINE1 knockdown (**P<0.01 vs NC group, n=3).
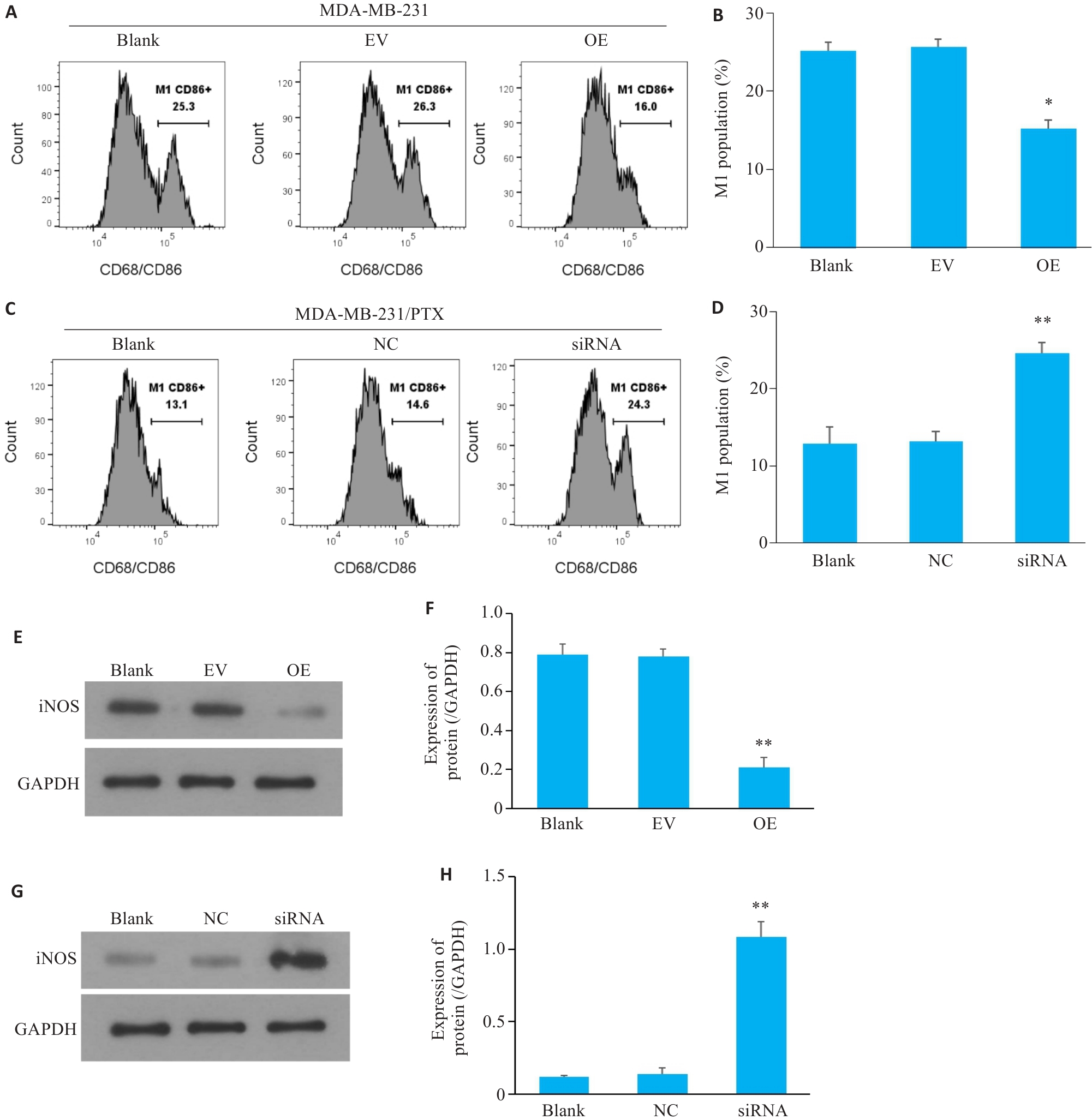
Fig.6 M1 polarization of the macrophages co-cultured with MDA-MB-231 cells with SERPINE1 overexpression or MDA-MB-231/PTX cells with SERPINE1 knockdown. A, B: Flow cytometry for analyzing the proportion of CD86+ macrophages co-cultured with MDA-MB-231 cells with SERPINE1 overexpression (*P<0.05 vs EV group). C, D: Flow cytometry for analyzing the proportion of CD86+ macrophages co-cultured with MDA-MB-231/PTX cells with SERPINE1 knockdown (**P<0.01 vs NC group). E, F: Western blotting for detecting the protein expression of iNOS in macrophages from the microenvironment of MDA-MB-231 cells with or without SERPINE1 overexpression (**P<0.01 vs EV group). G, H: Western blotting for detecting the protein expression of iNOS in macrophages from the microenvironment of MDA-MB-231/PTX cells with or without SERPINE1 knockdown (**P<0.01 vs NC group, n=3).
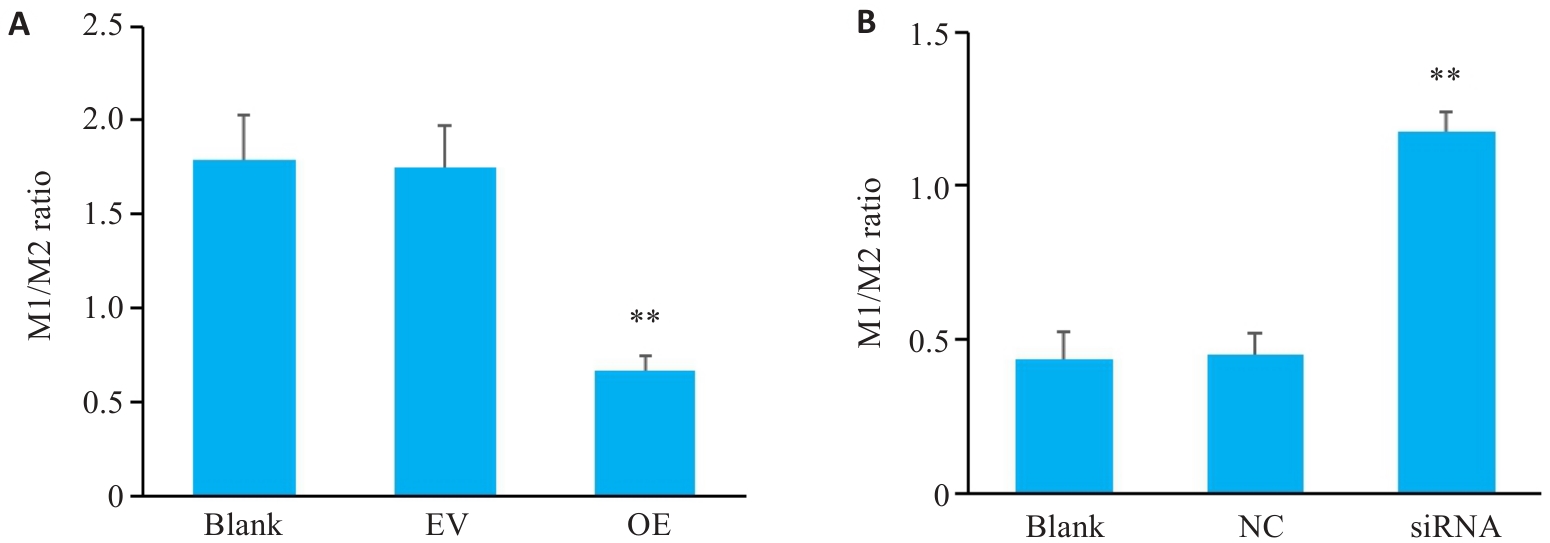
Fig.7 M1/M2 ratio of the macrophages co-cultured with MDA-MB-231 cells with SERPINE1 overexpression (A; **P<0.01 vs EV group) and MDA-MB-231/PTX cells with SERPINE1 knockdown (B; **P<0.01 vs blank group, n=3).
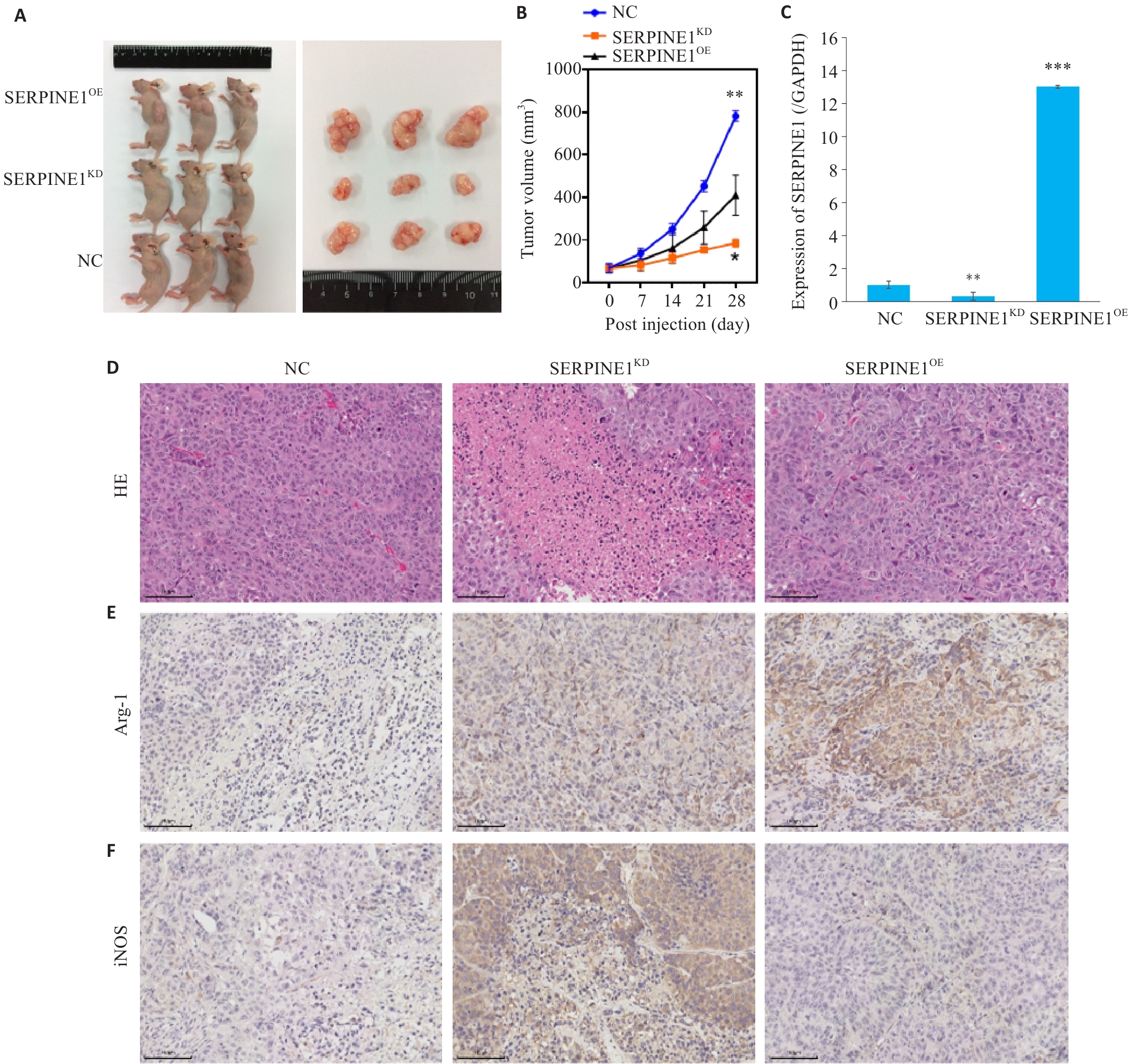
Fig.8 Regulatory effect of SERPINE1 expression level on growth of triple-negative breast cancer xenografts and macrophage polarization in nude mice. A: Appearance of the tumor-bearing nude mice and the dissected tumors. B: Tumor growth curves over time in each group. C: Protein expression level of SERPINE1 in the xenograft tumor tissues from each group. D: HE staining of xenograft tumor tissues. E: Immunohistochemistry for the M2 macrophage marker Arg-1 in xenograft tumor tissues. F: Immunohistochemistry for the M1 macrophage marker iNOS in xenograft tumor tissues (scale bar=100 μm). *P<0.05, **P<0.01, ***P<0.001 vs NC group. n=6.
| [1] | Li T, Zhang H, Lian M, et al. Global status and attributable risk factors of breast, cervical, ovarian, and uterine cancers from 1990 to 2021[J]. J Hematol Oncol, 2025, 18(1): 5. doi:10.1186/s13045-025-01660-y |
| [2] | Waks AG, Winer EP. Breast cancer treatment: a review[J]. JAMA, 2019, 321(3): 288-300. doi:10.1001/jama.2018.19323 |
| [3] | Nedeljković M, Damjanović A. Mechanisms of chemotherapy resistance in triple-negative breast cancer-how we can rise to the challenge[J]. Cells, 2019, 8(9): E957. doi:10.3390/cells8090957 |
| [4] | Bai XP, Ni J, Beretov J, et al. Triple-negative breast cancer therapeutic resistance: Where is the Achilles' heel[J]. Cancer Lett, 2021, 497: 100-11. doi:10.1016/j.canlet.2020.10.016 |
| [5] | Lyons TG. Targeted therapies for triple-negative breast cancer[J]. Curr Treat Options Oncol, 2019, 20(11): 82. doi:10.1007/s11864-019-0682-x |
| [6] | Deng M, Wang J, Chen Y, et al. Combination of SF1126 and gefitinib induces apoptosis of triple-negative breast cancer cells through the PI3K/AKT-mTOR pathway[J]. Anticancer Drugs, 2015, 26(4): 422-7. doi:10.1097/cad.0000000000000202 |
| [7] | Beniey M, Hubert A, Haque T, et al. Sequential targeting of PARP with carboplatin inhibits primary tumour growth and distant metastasis in triple-negative breast cancer[J]. Br J Cancer, 2023, 128(10): 1964-75. doi:10.1038/s41416-023-02226-w |
| [8] | Cardoso F, Paluch-Shimon S, Senkus E, et al. 5th ESO-ESMO international consensus guidelines for advanced breast cancer (ABC 5)[J]. Ann Oncol, 2020, 31(12): 1623-49. |
| [9] | Liao L, Zhang YL, Deng L, et al. Protein phosphatase 1 subunit PPP1R14B stabilizes STMN1 to promote progression and paclitaxel resistance in triple-negative breast cancer[J]. Cancer Res, 2023, 83(3): 471-84. doi:10.1158/0008-5472.can-22-2709 |
| [10] | Li SJ, Wei XH, He JY, et al. Plasminogen activator inhibitor-1 in cancer research[J]. Biomed Pharmacother, 2018, 105: 83-94. doi:10.1016/j.biopha.2018.05.119 |
| [11] | Li Y, Shen L, Tao K, et al. Key roles of p53 signaling pathway-related factors GADD45B and SERPINE1 in the occurrence and development of gastric cancer[J]. Mediators Inflamm, 2023, 2023: 6368893. doi:10.1155/2023/6368893 |
| [12] | Fox SB, Taylor M, Grøndahl-Hansen J, et al. Plasminogen activator inhibitor-1 as a measure of vascular remodelling in breast cancer[J]. J Pathol, 2001, 195(2): 236-43. doi:10.1002/path.931 |
| [13] | Li Y, Yu H, Han X, et al. Analyses of hypoxia-related risk factors and clinical relevance in breast cancer[J]. Front Oncol, 2024, 14: 1350426. doi:10.3389/fonc.2024.1350426 |
| [14] | Tong H, Li K, Zhou M, et al. Coculture of cancer cells with platelets increases their survival and metastasis by activating the TGFβ/Smad/PAI-1 and PI3K/AKT pathways[J]. Int J Biol Sci, 2023, 19(13): 4259-77. doi:10.7150/ijbs.85986 |
| [15] | Xu J, Zhang WW, Tang L, et al. Epithelial-mesenchymal transition induced PAI-1 is associated with prognosis of triple-negative breast cancer patients[J]. Gene, 2018, 670: 7-14. doi:10.1016/j.gene.2018.05.089 |
| [16] | Feng LR, Li GX, Li DB, et al. Cuproptosis-related gene SERPINE1 is a prognostic biomarker and correlated with immune infiltrates in gastric cancer[J]. J Cancer Res Clin Oncol, 2023, 149(12): 10851-65. doi:10.1007/s00432-023-04900-1 |
| [17] | Yagi T, Sawada K, Miyamoto M, et al. Continuous administration of anti-VEGFA antibody upregulates PAI-1 secretion from ovarian cancer cells via miR-143-3p downregulation[J]. Mol Cancer Res, 2023, 21(10): 1093-106. doi:10.1158/1541-7786.mcr-23-0015 |
| [18] | Pan JX, Qu F, Wang FF, et al. Aberrant SERPINE1 DNA methylation is involved in carboplatin induced epithelial-mesenchymal transition in epithelial ovarian cancer[J]. Arch Gynecol Obstet, 2017, 296(6): 1145-52. doi:10.1007/s00404-017-4547-x |
| [19] | Li XD, Dong P, Wei WS, et al. Overexpression of CEP72 promotes bladder urothelial carcinoma cell aggressiveness via epigenetic CREB-mediated induction of SERPINE1[J]. Am J Pathol, 2019, 189(6): 1284-97. doi:10.1016/j.ajpath.2019.02.014 |
| [20] | Thakore VP, Patel KD, Vora HH, et al. Up-regulation of extracellular-matrix and inflammation related genes in oral squamous cell carcinoma[J]. Arch Oral Biol, 2024, 161: 105925. doi:10.1016/j.archoralbio.2024.105925 |
| [21] | Liu Y, Liang YC, Su YJ, et al. Exploring the potential mechanisms of Yi-Yi-Fu-Zi-Bai-Jiang-San therapy on the immune-inflamed pheno-type of colorectal cancer via combined network pharmacology and bioinformatics analyses[J]. Comput Biol Med, 2023, 166: 107432. doi:10.1016/j.compbiomed.2023.107432 |
| [22] | Masuda T, Nakashima T, Namba M, et al. Inhibition of PAI-1 limits chemotherapy resistance in lung cancer through suppressing myofibroblast characteristics of cancer-associated fibroblasts[J]. J Cell Mol Med, 2019, 23(4): 2984-94. doi:10.1111/jcmm.14205 |
| [23] | Zhang Q, Lei L, Jing D. Knockdown of SERPINE1 reverses resistance of triple-negative breast cancer to paclitaxel via suppression of VEGFA[J]. Oncol Rep, 2020, 44(5): 1875-84. |
| [24] | Su YH, Wu YZ, Ann DK, et al. Obesity promotes radioresistance through SERPINE1-mediated aggressiveness and DNA repair of triple-negative breast cancer[J]. Cell Death Dis, 2023, 14(1): 53. doi:10.1038/s41419-023-05576-8 |
| [25] | Placencio VR, DeClerck YA. Plasminogen activator inhibitor-1 in cancer: rationale and insight for future therapeutic testing[J]. Cancer Res, 2015, 75(15): 2969-74. doi:10.1158/0008-5472.can-15-0876 |
| [26] | Xu Z, Cui Y, Li Y, et al. Research progress on nonspecific immune microenvironment in breast cancer[J]. Zhejiang da Xue Xue Bao Yi Xue Ban, 2018, 47(4): 426-34. |
| [27] | Wang S, Pang L, Liu Z, et al. SERPINE1 associated with remodeling of the tumor microenvironment in colon cancer progression: a novel therapeutic target[J]. BMC Cancer, 2021, 21(1): 767. doi:10.1186/s12885-021-08536-7 |
| [28] | 李文静, 张 磊, 赖娅娜, 等. 人乳腺癌多西紫杉醇耐药细胞株的建立及特性 [J]. 第三军医大学学报, 2011, 33(21): 3-11. |
| [29] | Leon-Ferre RA, Goetz MP. Advances in systemic therapies for triple negative breast cancer[J]. BMJ, 2023, 381: e071674. doi:10.1136/bmj-2022-071674 |
| [30] | Qiu XY, Qu Y, Guo BB, et al. Micellar paclitaxel boosts ICD and chemo-immunotherapy of metastatic triple negative breast cancer[J]. J Control Release, 2022, 341: 498-510. doi:10.1016/j.jconrel.2021.12.002 |
| [31] | Lovitt CJ, Shelper TB, Avery VM. Doxorubicin resistance in breast cancer cells is mediated by extracellular matrix proteins[J]. BMC Cancer, 2018, 18(1): 41. doi:10.1186/s12885-017-3953-6 |
| [32] | Yang CX, He LY, He PQ, et al. Increased drug resistance in breast cancer by tumor-associated macrophages through IL-10/STAT3/bcl-2 signaling pathway[J]. Med Oncol, 2015, 32(2): 14. doi:10.1007/s12032-014-0352-6 |
| [33] | Huang B, Chen ZH, Geng LL, et al. Mucosal profiling of pediatric-onset colitis and IBD reveals common pathogenics and therapeutic pathways[J]. Cell, 2019, 179(5): 1160-76. e24. doi:10.1016/j.cell.2019.10.027 |
| [34] | Zhang W, Xu J, Fang H, et al. Endothelial cells promote triple-negative breast cancer cell metastasis via PAI-1 and CCL5 signaling[J]. FASEB J, 2018, 32(1): 276-88. doi:10.1096/fj.201700237rr |
| [35] | Huang X, Wang L, Guo H, et al. Single-cell RNA sequencing reveals SERPINE1-expressing CAFs remodelling tumour microenviro-nment in recurrent osteosarcoma[J]. Clin Transl Med, 2024, 14(1): e1527. doi:10.1002/ctm2.1527 |
| [36] | Chen S, Morine Y, Tokuda K, et al. Cancer-associated fibroblast-induced M2-polarized macrophages promote hepatocellular carcinoma progression via the plasminogen activator inhibitor-1 pathway[J]. Int J Oncol, 2021, 59(2): 59. doi:10.3892/ijo.2021.5239 |
| [1] | Zhaojun ZHANG, Qiong WU, Miaomiao XIE, Ruyin YE, Chenchen GENG, Jiwen SHI, Qingling YANG, Wenrui WANG, Yurong SHI. Layered double hydroxide-loaded si-NEAT1 regulates paclitaxel resistance and tumor-associated macrophage polarization in breast cancer by targeting miR-133b/PD-L1 [J]. Journal of Southern Medical University, 2025, 45(8): 1718-1731. |
| [2] | Di CHEN, Ying LÜ, Yixin GUO, Yirong ZHANG, Ruixuan WANG, Xiaoruo ZHOU, Yuxin CHEN, Xiaohui WU. Dihydroartemisinin enhances doxorubicin-induced apoptosis of triple negative breast cancer cells by negatively regulating the STAT3/HIF-1α pathway [J]. Journal of Southern Medical University, 2025, 45(2): 254-260. |
| [3] | Songqi HE, Yang LIU, Mengchen QIN, Chunyu HE, Wentao JIANG, Yiqin WANG, Sirui TAN, Haiyan SUN, Haitao SUN. Traditional Chinese medicine for regulating glycolysis to remodel the tumor immune microenvironment: research progress and future prospects [J]. Journal of Southern Medical University, 2025, 45(10): 2277-2284. |
| [4] | Xinrong HE, Sili XIONG, Zhenru ZHU, Jingyuan SUN, Chuanhui CAO, Hui WANG. Overexpression of ubiquitin-conjugating enzyme 2T induces radiotherapy resistance in hepatocellular carcinoma by enriching regulatory T cells in the tumor microenvironment [J]. Journal of Southern Medical University, 2024, 44(6): 1149-1158. |
| [5] | Youqin ZENG, Siyu CHEN, Yan LIU, Yitong LIU, Ling ZHANG, Jiao XIA, Xinyu WU, Changyou WEI, Ping LENG. AKBA combined with doxorubicin inhibits proliferation and metastasis of triple-negative breast cancer MDA-MB-231 cells and xenograft growth in nude mice [J]. Journal of Southern Medical University, 2024, 44(12): 2449-2460. |
| [6] | WANG Li, YAN Zhirui, XIA Yaoxiong. Silencing RAB27a inhibits proliferation, invasion and adhesion of triple-negative breast cancer cells [J]. Journal of Southern Medical University, 2023, 43(4): 560-567. |
| [7] | LIU Junping, SHI Yutong, WU Minmin, XU Mengqi, ZHANG Fengmei, HE Zhiqiang, TANG Min. JAG1 promotes migration, invasion, and adhesion of triple-negative breast cancer cells by promoting angiogenesis [J]. Journal of Southern Medical University, 2022, 42(7): 1100-1108. |
| [8] | FANG Yuxiao, WANG Shumei, YANG Qian, YOU Songfan, XING Xiangling. Chaihu Guizhi Decoction plus or minus formula combined with capecitabine inhibits IL-6/STAT3 signaling to suppress triple-negative breast cancer xenografts in nude mice [J]. Journal of Southern Medical University, 2022, 42(6): 905-912. |
| [9] | GE Yu, LU Linming, TIAN Shuyu, XIAO Yu, XIE Shangfu, WANG Qi, ZHI Hui. Agkistrodon halys venom antitumor component-I inhibits vasculogenic mimicry in triple-negative breast cancer cells in vitro by down-regulating MMP2 [J]. Journal of Southern Medical University, 2022, 42(3): 438-442. |
| [10] | ZHAO Aiyue, SU Yunxia, FU Deqiang. MiR-4772 modulates tumor immune microenvironment by regulating immune-related genes in ovarian cancer [J]. Journal of Southern Medical University, 2022, 42(11): 1638-1645. |
| [11] | WANG Lu, ZHAO Lin, ZHANG Lifen, JING Xin, ZHANG Yujiao, SHAO Shan, ZHAO Xinhan, LUO Minna. Vascular endothelial growth factor promotes cancer stemness of triple-negative breast cancer via MAPK/ERK pathway [J]. Journal of Southern Medical University, 2021, 41(10): 1484-1491. |
| [12] | . EGFR tyrosine kinase inhibitor HS-10296 induces autophagy and apoptosis in triplenegative breast cancer MDA-MB-231 cells [J]. Journal of Southern Medical University, 2020, 40(07): 981-987. |
| [13] | . Long-chain non-coding RNA MALAT1 regulates paclitaxel resistance of breast cancer cells by targeting miR-485-3p [J]. Journal of Southern Medical University, 2020, 40(05): 698-702. |
| [14] |
.
Establishment of a NOD/SCID mouse model with human immune reconstitution bearing human triple-negative breast cancer [J]. Journal of Southern Medical University, 2015, 35(01): 56-. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||