Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (12): 2598-2606.doi: 10.12122/j.issn.1673-4254.2025.12.07
Junjie CUI1( ), Ruiyin LAI1, Suheng CHEN1, Shanshan QU1, Yue LIAO1, Xue MA1, Yulan LI2(
), Ruiyin LAI1, Suheng CHEN1, Shanshan QU1, Yue LIAO1, Xue MA1, Yulan LI2( )
)
Received:2025-05-27
Online:2025-12-20
Published:2025-12-22
Contact:
Yulan LI
E-mail:cuijj2023@lzu.edu.cn;liyul@lzu.edu.cn
Supported by:Junjie CUI, Ruiyin LAI, Suheng CHEN, Shanshan QU, Yue LIAO, Xue MA, Yulan LI. Overwork damages myocardial energy metabolism homeostasis in mice[J]. Journal of Southern Medical University, 2025, 45(12): 2598-2606.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.12.07
| Gene | Sequence of primers |
|---|---|
| CPT1B | F: GCACACCAGGCAGTAGCTTT |
| R: CAGGAGTTGATTCCAGACAGGTA | |
| PPARα | F: AGAGCCCCATCTGTCCTCTC |
| R: ACTGGTAGTCTGCAAAACCAAA | |
| PFKM | F: TGTGGTCCGAGTTGGTATCTT |
| R: GCACTTCCAATCACTGTGCC | |
| PKM2 | F: GCCGCCTGGACATTGACTC |
| R: CCATGAGAGAAATTCAGCCGAG | |
| ACTB | F: GGCTGTATTCCCCTCCATCG |
| R: CCAGTTGGTAACAATGCCATGT |
Tab.1 Primer sequence for RT-qPCR
| Gene | Sequence of primers |
|---|---|
| CPT1B | F: GCACACCAGGCAGTAGCTTT |
| R: CAGGAGTTGATTCCAGACAGGTA | |
| PPARα | F: AGAGCCCCATCTGTCCTCTC |
| R: ACTGGTAGTCTGCAAAACCAAA | |
| PFKM | F: TGTGGTCCGAGTTGGTATCTT |
| R: GCACTTCCAATCACTGTGCC | |
| PKM2 | F: GCCGCCTGGACATTGACTC |
| R: CCATGAGAGAAATTCAGCCGAG | |
| ACTB | F: GGCTGTATTCCCCTCCATCG |
| R: CCAGTTGGTAACAATGCCATGT |
| Group | Modeling time (weeks) | ||||||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | |
| CON | 20.45±0.29 | 21.13±0.23 | 22.02±0.31a | 22.54±0.47a | 23.18±0.47a | 23.96±0.37a | 24.3±0.38a |
| W2 | 20.00±0.37 | 19.94±0.50 | 20.13±0.40d | ||||
| W4 | 20.50±0.19 | 20.24±0.24 | 20.41±0.19d | 20.90±0.24b | 21.14±0.30c | ||
| W6 | 19.89±0.19 | 20.51±0.20 | 20.85±0.25c | 20.35±0.48c | 20.80±0.49d | 21.29±0.52d | 21.54±0.45d |
Tab.2 Changes of body weight of the mice in each group during modeling (g, Mean±SD, n=8)
| Group | Modeling time (weeks) | ||||||
|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | 5 | 6 | |
| CON | 20.45±0.29 | 21.13±0.23 | 22.02±0.31a | 22.54±0.47a | 23.18±0.47a | 23.96±0.37a | 24.3±0.38a |
| W2 | 20.00±0.37 | 19.94±0.50 | 20.13±0.40d | ||||
| W4 | 20.50±0.19 | 20.24±0.24 | 20.41±0.19d | 20.90±0.24b | 21.14±0.30c | ||
| W6 | 19.89±0.19 | 20.51±0.20 | 20.85±0.25c | 20.35±0.48c | 20.80±0.49d | 21.29±0.52d | 21.54±0.45d |

Fig.1 Heart weight index (A) and echocardiography (B) in each group (mg/g, Mean±SD, n=8). #P>0.05 vs CON group. CON: Control group. W2: overwork for 2 weeks group; W4: overwork for 4 weeks group; W6: overwork for 6 weeks group.
| Group | LVIDs (mm) | LVIDd (mm) | EF% | FS% | LVPWd (mm) |
|---|---|---|---|---|---|
| CON | 2.06±0.52 | 3.03±0.02 | 65.29±0.32 | 35.01±0.50 | 0.84±0.03 |
| W2 | 2.01±0.33 | 3.06±0.03 | 65.76±0.44 | 35.14±0.79 | 0.84±0.01 |
| W4 | 2.10±0.09 | 3.11±0.06 | 64.99±0.79 | 36.26±0.21 | 0.85±0.05 |
| W6 | 2.11±0.06 | 3.18±0.01 | 64.87±0.55 | 35.28±0.43 | 0.85±0.01 |
Tab.3 Cardiac function changes in each group (Mean±SD, n=3)
| Group | LVIDs (mm) | LVIDd (mm) | EF% | FS% | LVPWd (mm) |
|---|---|---|---|---|---|
| CON | 2.06±0.52 | 3.03±0.02 | 65.29±0.32 | 35.01±0.50 | 0.84±0.03 |
| W2 | 2.01±0.33 | 3.06±0.03 | 65.76±0.44 | 35.14±0.79 | 0.84±0.01 |
| W4 | 2.10±0.09 | 3.11±0.06 | 64.99±0.79 | 36.26±0.21 | 0.85±0.05 |
| W6 | 2.11±0.06 | 3.18±0.01 | 64.87±0.55 | 35.28±0.43 | 0.85±0.01 |
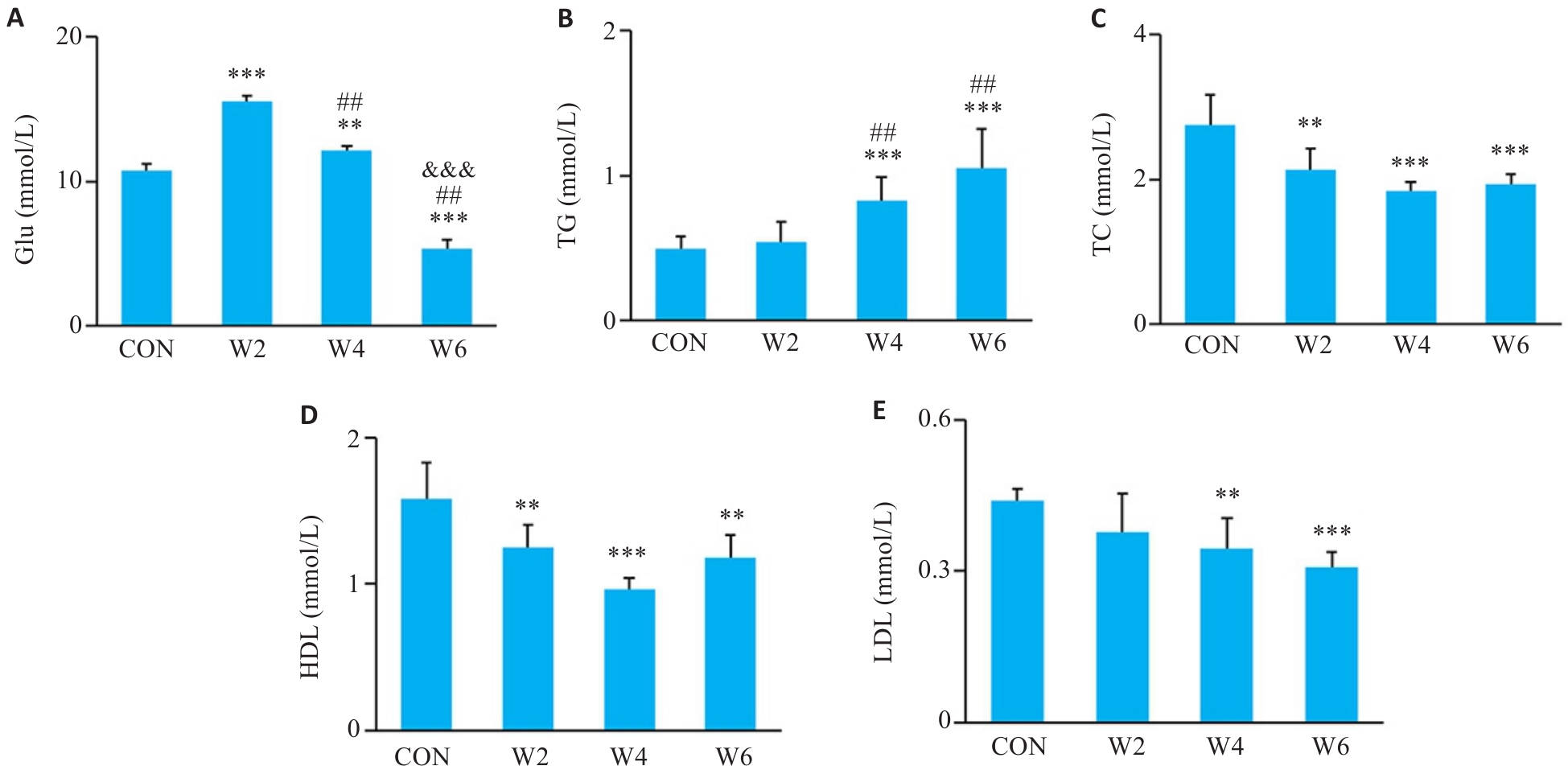
Fig.2 Changes of blood glucose and blood lipids in each group (Mean±SD, n=6). A-E: Blood glucose (Glu), triglycerides (TG), cholesterol (TC), high-density lipoprotein cholesterol (HDL), and low-density lipoprotein cholesterol (LDL) levels, respectively. **P<0.01, ***P<0.001 vs CON group; ##P<0.01 vs W2 group; &&&P<0.001 vs W4 group.
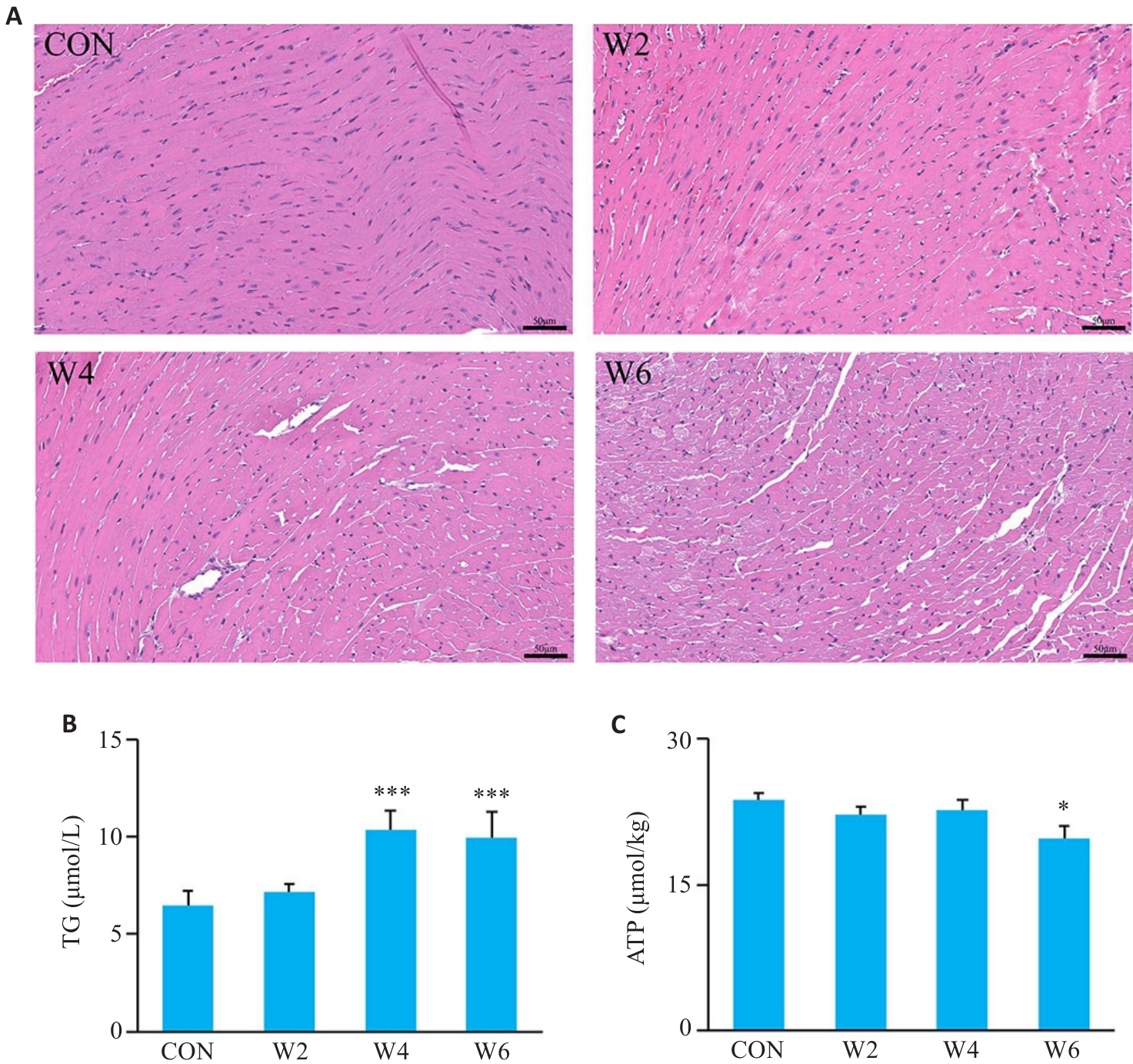
Fig.3 Histopathological changes of the myocardial tissues and changes in myocardial TG and ATP levels in each group. A: HE staining (Scale bar=50 μm). B: Myocardial TG level (n=6; ***P<0.001 vs CON group). C: Myocardial ATP level (n=6; *P<0.05 vs CON group).
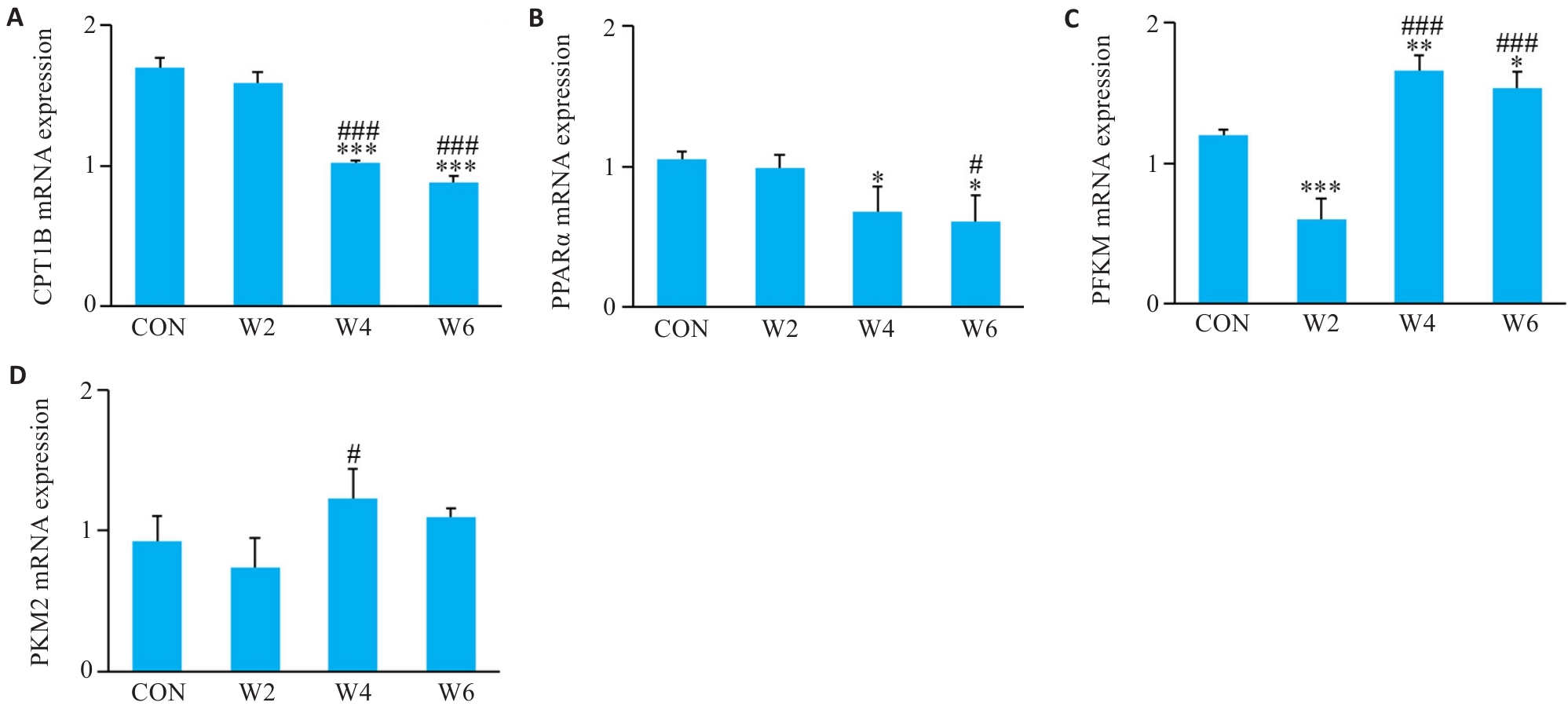
Fig.4 Relative expression levels of CPT1B (A), PPARα (B), PFKM (C), and PKM2 (D) mRNA in each group (n=3). *P<0.05, **P<0.01, ***P<0.001 vs CON group; #P<0.05, ###P<0.001 vs W2 group.
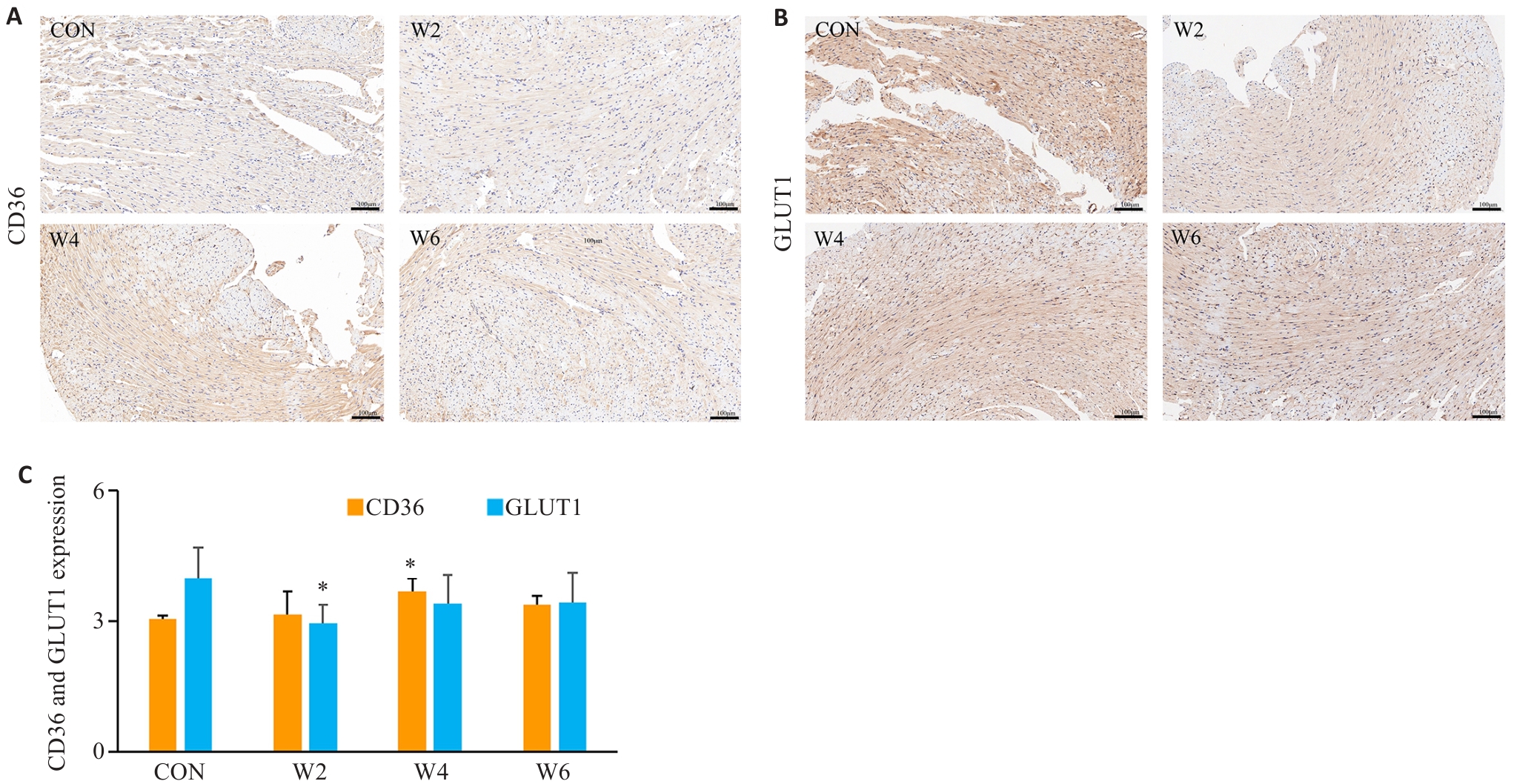
Fig.5 Expression of CD36 and GLUT1 protein and the area of positive cells (%) in the myocardium in each group. A, B: Immunohistochemical staining (Scale bar=100 μm). C: CD36 and GLUT1 protein expression levels. *P<0.05 vs CON group.
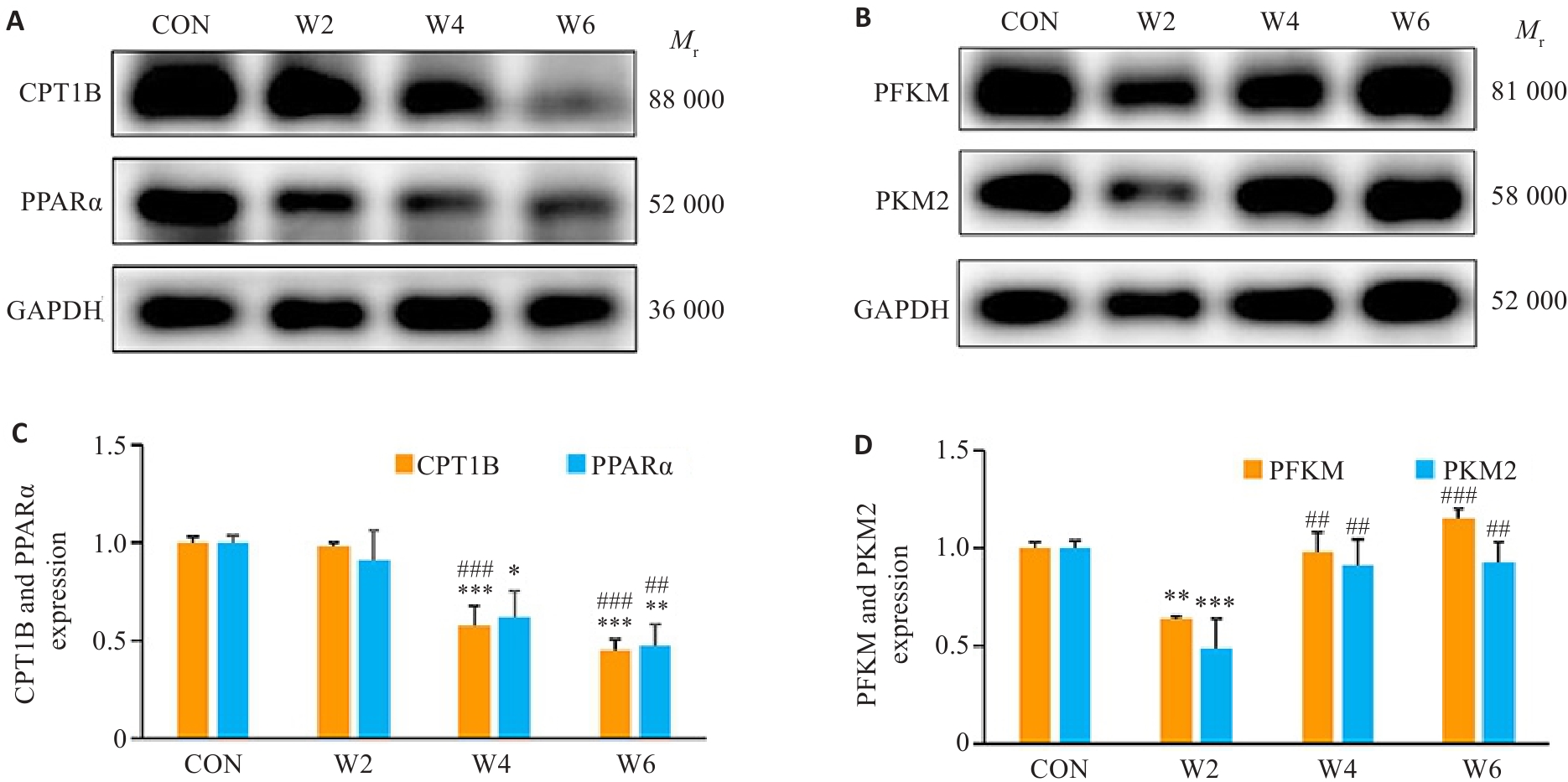
Fig.6 Relative protein expressions of CPT1B, PPARα, PFKM and PKM2 in the myocardium in each group. A, B: Protein bands in Western blotting. C, D: CPT1B, PPARα, PFKM, and PKM2 protein expression levels in each group. *P<0.05, **P<0.01, ***P<0.001 vs CON group; ##P<0.01, ###P<0.001 vs W2 group.
| [1] | Kivimäki M, Jokela M, Nyberg ST, et al. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603, 838 individuals[J]. Lancet, 2015, 386(10005): 1739-46. doi:10.1016/s0140-6736(15)60295-1 |
| [2] | Pega F, Náfrádi B, Momen NC, et al. Global, regional, and national burdens of ischemic heart disease and stroke attributable to exposure to long working hours for 194 countries, 2000-2016: a systematic analysis from the WHO/ILO Joint Estimates of the Work-related Burden of Disease and Injury[J]. Environ Int, 2021, 154: 106595. doi:10.1016/j.envint.2021.106595 |
| [3] | Eguchi H, Wada K, Smith DR. Recognition, compensation, and prevention of karoshi, or death due to overwork[J]. J Occup Environ Med, 2016, 58(8): e313-4. doi:10.1097/jom.0000000000000797 |
| [4] | Al-Madhagi HA. Unveiling the global surge: unraveling the factors fueling the spread of karoshi syndrome[J]. Risk Manag Healthc Policy, 2023, 16: 2779-82. doi:10.2147/rmhp.s444900 |
| [5] | Lopaschuk GD, Karwi QG, Tian R, et al. Cardiac energy metabolism in heart failure[J]. Circ Res, 2021, 128(10): 1487-513. doi:10.1161/circresaha.121.318241 |
| [6] | Flam E, Jang C, Murashige D, et al. Integrated landscape of cardiac metabolism in end-stage human nonischemic dilated cardiomyopathy[J]. Nat Cardiovasc Res, 2022, 1(9): 817-29. |
| [7] | Piché ME, Tchernof A, Després JP. Obesity phenotypes, diabetes, and cardiovascular diseases[J]. Circ Res, 2020, 126(11): 1477-500. doi:10.1161/circresaha.120.316101 |
| [8] | 李嘉敏, 苏锐冰, 于晓军, 等. 大鼠过劳死模型的建立及基于模型的能量代谢和氧化应激的蛋白质组学和代谢组学分析[J]. 生物化学与生物物理进展, 2024, 51(8): 1935-49. |
| [9] | Miao Q, Li J, Pan YP, et al. Three cases of karoshi without the typical pathomorphological features of cardiovascular/cerebrovascular disease[J]. Am J Forensic Med Pathol, 2020, 41(4): 305-8. doi:10.1097/paf.0000000000000600 |
| [10] | 刘艳艳, 程静茹, 余克强, 等. 疲劳型亚健康小鼠模型的研制[J]. 广东医学, 2012, 33(1): 21-4. |
| [11] | 邓三春, 陈苏衡, 于恺华, 等. 过度劳累对小鼠脾脏造血功能的影响[J]. 陆军军医大学学报, 2024(5): 427-33. |
| [12] | Matsui T, Ishikawa T, Ito H, et al. Brain glycogen superco-mpensation following exhaustive exercise[J]. J Physiol, 2012, 590(3): 607-16. doi:10.1113/jphysiol.2011.217919 |
| [13] | Lee WD, Liang LF, AbuSalim J, et al. Impact of acute stress on murine metabolomics and metabolic flux[J]. Proc Natl Acad Sci USA, 2023, 120(21): e2301215120. doi:10.1073/pnas.2301215120 |
| [14] | Lightman SL, Birnie MT, Conway-Campbell BL. Dynamics of ACTH and Cortisol secretion and implications for disease[J]. Endocr Rev, 2020, 41(3): bnaa002. doi:10.1210/endrev/bnaa002 |
| [15] | Chen YY, Gao TH, Bai J, et al. Ren-Shen-Bu-Qi decoction alleviates exercise fatigue through activating PI3K/AKT/Nrf2 pathway in mice[J]. Chin Med, 2024, 19(1): 154. doi:10.1186/s13020-024-01027-4 |
| [16] | Flockhart M, Tischer D, Nilsson LC, et al. Reduced glucose tolerance and insulin sensitivity after prolonged exercise in endurance athletes[J]. Acta Physiol (Oxf), 2023, 238(4): e13972. doi:10.1111/apha.13972 |
| [17] | Zhang QL, Shen XT, Yuan X, et al. Lipopolysaccharide binding protein resists hepatic oxidative stress by regulating lipid droplet homeostasis[J]. Nat Commun, 2024, 15(1): 3213. doi:10.1038/s41467-024-47553-5 |
| [18] | Geng J, Zhang XL, Guo YJ, et al. Moderate-intensity interval exercise exacerbates cardiac lipotoxicity in high-fat, high-calories diet-fed mice[J]. Nat Commun, 2025, 16(1): 613. doi:10.1038/s41467-025-55917-8 |
| [19] | 廖 阅, 马 雪, 邓三春, 等. 过劳诱导小鼠血管内皮屏障功能障碍[J]. 南方医科大学学报, 2024, 44(9): 1814-20. |
| [20] | Kim HG, Lee JS, Lee JS, et al. Hepatoprotective and antioxidant effects of Myelophil on restraint stress-induced liver injury in BALB/c mice[J]. J Ethnopharmacol, 2012, 142(1): 113-20. doi:10.1016/j.jep.2012.04.023 |
| [21] | Raposeiras-Roubin S, Rosselló X, Oliva B, et al. Triglycerides and residual atherosclerotic risk[J]. J Am Coll Cardiol, 2021, 77(24): 3031-41. doi:10.1016/j.jacc.2021.04.059 |
| [22] | Nordestgaard BG. Triglyceride-rich lipoproteins and atherosclerotic cardiovascular disease: new insights from epidemiology, genetics, and biology[J]. Circ Res, 2016, 118(4): 547-63. doi:10.1161/circresaha.115.306249 |
| [23] | Miller M, Stone NJ, Ballantyne C, et al. Triglycerides and cardiovascular disease: a scientific statement from the American Heart Association[J]. Circulation, 2011, 123(20): 2292-333. doi:10.1161/cir.0b013e3182160726 |
| [24] | 陈苏衡, 甘 露, 庄 苗, 等. 过度劳累对大鼠动脉血管壁细胞外基质的影响[J]. 中国医学科学院学报, 2022, 44(2): 262-9. |
| [25] | Zhang YF, Yu MY, Chen Y, et al. High-density lipoprotein in cardiovascular diseases: From high quantity to high quality[J]. Clin Chim Acta, 2026, 578: 120574. doi:10.1016/j.cca.2025.120574 |
| [26] | Ljones K, Ness HO, Solvang-Garten K, et al. Acute exhaustive aerobic exercise training impair cardiomyocyte function and calcium handling in Sprague-Dawley rats[J]. PLoS One, 2017, 12(3): e0173449. doi:10.1371/journal.pone.0173449 |
| [27] | Oláh A, Németh BT, Mátyás C, et al. Cardiac effects of acute exhaustive exercise in a rat model[J]. Int J Cardiol, 2015, 182: 258-66. doi:10.1016/j.ijcard.2014.12.045 |
| [28] | 马 雪, 廖阅, 邓三春, 等.过劳不同时间对小鼠心肌细胞焦亡的影响[J], 解放军医学杂志, 2025, 50(6): 756-761. |
| [29] | Haynie KR, Vandanmagsar B, Wicks SE, et al. Inhibition of carnitine palymitoyltransferase1b induces cardiac hypertrophy and mortality in mice[J]. Diabetes Obes Metab, 2014, 16(8): 757-60. doi:10.1111/dom.12248 |
| [30] | He L, Kim T, Long QQ, et al. Carnitine palmitoyltransferase-1b deficiency aggravates pressure overload-induced cardiac hypertrophy caused by lipotoxicity[J]. Circulation, 2012, 126(14): 1705-16. doi:10.1161/circulationaha.111.075978 |
| [31] | 高瑞芳, 常 芸, 刘云清, 等. 力竭运动后大鼠心肌组织结构改变及不同时相PPARα表达的变化[J]. 中国运动医学杂志, 2009, 28(3): 264-8. |
| [32] | O’Connell RP, Musa H, Gomez MSM, et al. Free fatty acid effects on the atrial myocardium: membrane ionic currents are remodeled by the disruption of T-tubular architecture[J]. PLoS One, 2015, 10(8): e0133052. doi:10.1371/journal.pone.0133052 |
| [33] | Schulze PC, Drosatos K, Goldberg IJ. Lipid use and misuse by the heart[J]. Circ Res, 2016, 118(11): 1736-51. doi:10.1161/circresaha.116.306842 |
| [34] | Gibb AA, Hill BG. Metabolic coordination of physiological and pathological cardiac remodeling[J]. Circ Res, 2018, 123(1): 107-28. doi:10.1161/circresaha.118.312017 |
| [35] | Kemppainen J, Fujimoto T, Kalliokoski KK, et al. Myocardial and skeletal muscle glucose uptake during exercise in humans[J]. J Physiol, 2002, 542(Pt 2): 403-12. doi:10.1113/jphysiol.2002.018135 |
| [36] | Wang X, Zhu XX, Jiao SY, et al. Cardiomyocyte peroxisome proliferator-activated receptor α is essential for energy metabolism and extracellular matrix homeostasis during pressure overload-induced cardiac remodeling[J]. Acta Pharmacol Sin, 2022, 43(5): 1231-42. doi:10.1038/s41401-021-00743-z |
| [37] | Gibb AA, Epstein PN, Uchida S, et al. Exercise-induced changes in glucose metabolism promote physiological cardiac growth[J]. Circulation, 2017, 136(22): 2144-57. doi:10.1161/circulationaha.117.028274 |
| [1] | Changlong FU, Ruolan CHEN, Shiqi XU, Jinxin YOU, Qing LIN, Yanfeng HUANG. Morinda officinalis polysaccharide delays osteoarthritis mouse chondrocyte degeneration by modulating the glycolysis-pyroptosis axis via targeting the lncRNA XIST [J]. Journal of Southern Medical University, 2025, 45(12): 2541-2550. |
| [2] | Hui LU, Bowen SONG, Jinran SHI, Shunyin WANG, Xiaohua CHEN, Jingjing YANG, Sitang GE, Lugen ZUO. SF3B3 overexpression promotes proliferation of gastric cancer cells and correlates with poor patient prognosis [J]. Journal of Southern Medical University, 2025, 45(10): 2240-2249. |
| [3] | Songqi HE, Yang LIU, Mengchen QIN, Chunyu HE, Wentao JIANG, Yiqin WANG, Sirui TAN, Haiyan SUN, Haitao SUN. Traditional Chinese medicine for regulating glycolysis to remodel the tumor immune microenvironment: research progress and future prospects [J]. Journal of Southern Medical University, 2025, 45(10): 2277-2284. |
| [4] | Qing SHI, Suye RAN, Lingyu SONG, Hong YANG, Wenjuan WANG, Hanlin LIU, Qi LIU. NLRP6 overexpression improves nonalcoholic fatty liver disease by promoting lipid oxidation and decomposition in hepatocytes through the AMPK/CPT1A/PGC1A pathway [J]. Journal of Southern Medical University, 2025, 45(1): 118-125. |
| [5] | Yue LIAO, Xue MA, Sanchun DENG, Suheng CHEN, Yulan LI. Overwork induces vascular endothelial barrier dysfunction in mice [J]. Journal of Southern Medical University, 2024, 44(9): 1814-1820. |
| [6] | Xiaohui WEN, Shiya HUANG, Xuehong LIU, Kunyin LI, Yongge GUAN. Role of Notch 1 signaling and glycolysis in the pathogenic mechanism of adenomyosis [J]. Journal of Southern Medical University, 2024, 44(8): 1599-1604. |
| [7] | Mengdong ZHENG, Yan LIU, Jiaojiao LIU, Qiaozhen KANG, Ting WANG. Effect of deletion of protein 4.1R on proliferation, apoptosis and glycolysis of hepatocyte HL-7702 cells [J]. Journal of Southern Medical University, 2024, 44(7): 1355-1360. |
| [8] | MAN Hao, WANG Jianwei, WU Mao, SHAO Yang, YANG Junfeng, LI Shaoshuo, LÜ Jinye, ZHOU Yue. Jisuikang formula promotes spinal cord injury repair in rats by activating the YAP/PKM2 signaling axis in astrocytes [J]. Journal of Southern Medical University, 2024, 44(4): 636-643. |
| [9] | WANG Zining, YANG Ming, LI Shuanglei, CHI Haitao, WANG Junhui, XIAO Cangsong. A transcriptomic analysis of correlation between mitochondrial function and energy metabolism remodeling in mice with myocardial fibrosis following myocardial infarction [J]. Journal of Southern Medical University, 2024, 44(4): 666-674. |
| [10] | CUI Jianing, LIU Wenjia, YAN Fei, ZHAO Yanan, CHEN Weijie, LUO Chuncai, ZHANG Xinghua, LI Tao. Predictive value of cardiac magnetic resonance imaging for adverse left ventricular remodeling after acute ST-segment elevation myocardial infarction [J]. Journal of Southern Medical University, 2024, 44(3): 553-562. |
| [11] | YAN Qiuxia, ZENG Peng, HUANG Shuqiang, TAN Cuiyu, ZHOU Xiuqin, QIAO Jing, ZHAO Xiaoying, FENG Ling, ZHU Zhenjie, ZHANG Guozhi, HU Hong, CHEN Cairong. RBMX overexpression inhibits proliferation, migration, invasion and glycolysis of human bladder cancer cells by downregulating PKM2 [J]. Journal of Southern Medical University, 2024, 44(1): 9-16. |
| [12] | FENG Wen, LAI Yuexing, WANG Jing, XU Ping. Long non-coding RNA ABHD11-AS1 promotes glycolysis in gastric cancer cells to accelerate tumor progression [J]. Journal of Southern Medical University, 2023, 43(9): 1485-1492. |
| [13] | WANG Qiusheng, ZHANG Zhen, WANG Lian, WANG Yu, YAO Xinyu, WANG Yueyue, ZHANG Xiaofeng, GE Sitang, ZUO Lugen. High expression of death-associated protein 5 promotes glucose metabolism in gastric cancer cells and correlates with poor survival outcomes [J]. Journal of Southern Medical University, 2023, 43(7): 1063-1070. |
| [14] | WANG Huijie, SUN Zhengui, ZHAO Wenying, GENG Biao. S100A10 promotes proliferation and invasion of lung adenocarcinoma cells by activating the Akt-mTOR signaling pathway [J]. Journal of Southern Medical University, 2023, 43(5): 733-740. |
| [15] | . Long non-coding RNA UPK1A-AS1 promotes glycolysis in hepatocellular carcinoma cells via stabilization of HIF-1α [J]. Journal of Southern Medical University, 2021, 41(2): 193-199. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||