南方医科大学学报 ›› 2024, Vol. 44 ›› Issue (10): 1965-1975.doi: 10.12122/j.issn.1673-4254.2024.10.15
杨玉梅( ), 刘雪柔, 刘伟, 周星琦, 张振, 胡妍, 刘培培, 李娴, 刘浩, 李姗姗(
), 刘雪柔, 刘伟, 周星琦, 张振, 胡妍, 刘培培, 李娴, 刘浩, 李姗姗( )
)
收稿日期:2024-04-07
出版日期:2024-10-20
发布日期:2024-10-31
通讯作者:
李姗姗
E-mail:1337781526@qq.com;lishanshan900122@163.com
作者简介:杨玉梅,在读硕士研究生,E-mail: 1337781526@qq.com
基金资助:
Yumei YANG( ), Xuerou LIU, Wei LIU, Xingqi ZHOU, Zhen ZHANG, Yan HU, Peipei LIU, Xian LI, Hao LIU, Shanshan LI(
), Xuerou LIU, Wei LIU, Xingqi ZHOU, Zhen ZHANG, Yan HU, Peipei LIU, Xian LI, Hao LIU, Shanshan LI( )
)
Received:2024-04-07
Online:2024-10-20
Published:2024-10-31
Contact:
Shanshan LI
E-mail:1337781526@qq.com;lishanshan900122@163.com
摘要:
目的 探究阿美替尼联合安罗替尼抑制非小细胞肺癌的作用。 方法 CCK-8法、集落克隆法和流式细胞术检测不同浓度阿美替尼和安罗替尼对PC-9细胞和HCC827细胞增殖、细胞存活和细胞凋亡的影响;SynergyFinder模型评价阿美替尼与安罗替尼的协同作用;Transwell小室实验检测阿美替尼联合安罗替尼对PC-9细胞和HCC827细胞侵袭及迁移的作用;Western blotting实验检测阿美替尼联合安罗替尼对PC-9细胞和HCC827细胞凋亡和侵袭迁移相关蛋白Bax、Bcl-2、E-Cadherin、Vimentin、MMP2和MMP9及PI3K-Akt通路关键蛋白表达的影响。 结果 阿美替尼作用于PC-9细胞的IC50为1.701 μmol/L,安罗替尼作用于PC-9细胞的IC50=4.979 μmol/L,协同得分(ZIP)为19.112;阿美替尼对HCC827细胞IC50=2.961 μmol/L,安罗替尼对HCC827细胞IC50=7.934 μmol/L,协同得分(ZIP)为12.325,阿美替尼联合安罗替尼能够显著抑制PC-9细胞和HCC827细胞增殖(P<0.05)。相比于单药组,集落克隆结果表明阿美替尼联合安罗替尼能够显著抑制PC-9细胞和HCC827细胞存活(P<0.01);流式细胞术结果表明,阿美替尼联合安罗替尼能够促进PC-9细胞和HCC827细胞发生凋亡(P<0.05);Transwell实验结果表明,阿美替尼联合安罗替尼能够显著抑制PC-9细胞和HCC827细胞的侵袭迁移能力(P<0.01);Western blotting实验结果表明,阿美替尼联合安罗替尼能够显著促进PC-9细胞和HCC827细胞中E-Cadherin和Bax蛋白的表达,抑制Bcl-2、Vimentin、MMP2和MMP9蛋白的表达(P<0.01),同时显著降低了PI3K-Akt通路中关键蛋白PI3K、Akt的磷酸化蛋白水平(P<0.01)。 结论 阿美替尼联合安罗替尼通过下调PI3K-Akt通路抑制NSCLC肿瘤细胞,这种联合治疗方式可能成为临床上治疗 NSCLC患者的一种潜在治疗策略。
杨玉梅, 刘雪柔, 刘伟, 周星琦, 张振, 胡妍, 刘培培, 李娴, 刘浩, 李姗姗. 阿美替尼联合安罗替尼通过下调PI3K/AKT通路抑制非小细胞肺癌细胞的增殖[J]. 南方医科大学学报, 2024, 44(10): 1965-1975.
Yumei YANG, Xuerou LIU, Wei LIU, Xingqi ZHOU, Zhen ZHANG, Yan HU, Peipei LIU, Xian LI, Hao LIU, Shanshan LI. Aumolertinib combined with anlotinib inhibits proliferation of non-small cell lung cancer cells by down-regulating the PI3K/AKT pathway[J]. Journal of Southern Medical University, 2024, 44(10): 1965-1975.
| Antibody name | Company | Dilution rate |
|---|---|---|
| Anti-beta actin | Affinity biosciences | 1:5000 |
| Anti-E-cadherin | Proteintech | 1:5000 |
| Anti-Vimentin | Proteintech | 1:1000 |
| Anti-Bax | Proteintech | 1:2000 |
| Anti-Bcl-2 | Proteintech | 1:2000 |
| Anti-MMP2 | Affinity biosciences | 1:1000 |
| Anti-MMP9 | Affinity biosciences | 1:1000 |
| Anti-PI3K | Proteintech | 1:1000 |
| Anti-AKT | Proteintech | 1:5000 |
| Anti-p-PI3K | Cell signaling technology | 1:1000 |
| Anti-p-AKT | Cell signaling technology | 1:2000 |
表1 抗体信息
Tab.1 Antibodies used in this study
| Antibody name | Company | Dilution rate |
|---|---|---|
| Anti-beta actin | Affinity biosciences | 1:5000 |
| Anti-E-cadherin | Proteintech | 1:5000 |
| Anti-Vimentin | Proteintech | 1:1000 |
| Anti-Bax | Proteintech | 1:2000 |
| Anti-Bcl-2 | Proteintech | 1:2000 |
| Anti-MMP2 | Affinity biosciences | 1:1000 |
| Anti-MMP9 | Affinity biosciences | 1:1000 |
| Anti-PI3K | Proteintech | 1:1000 |
| Anti-AKT | Proteintech | 1:5000 |
| Anti-p-PI3K | Cell signaling technology | 1:1000 |
| Anti-p-AKT | Cell signaling technology | 1:2000 |
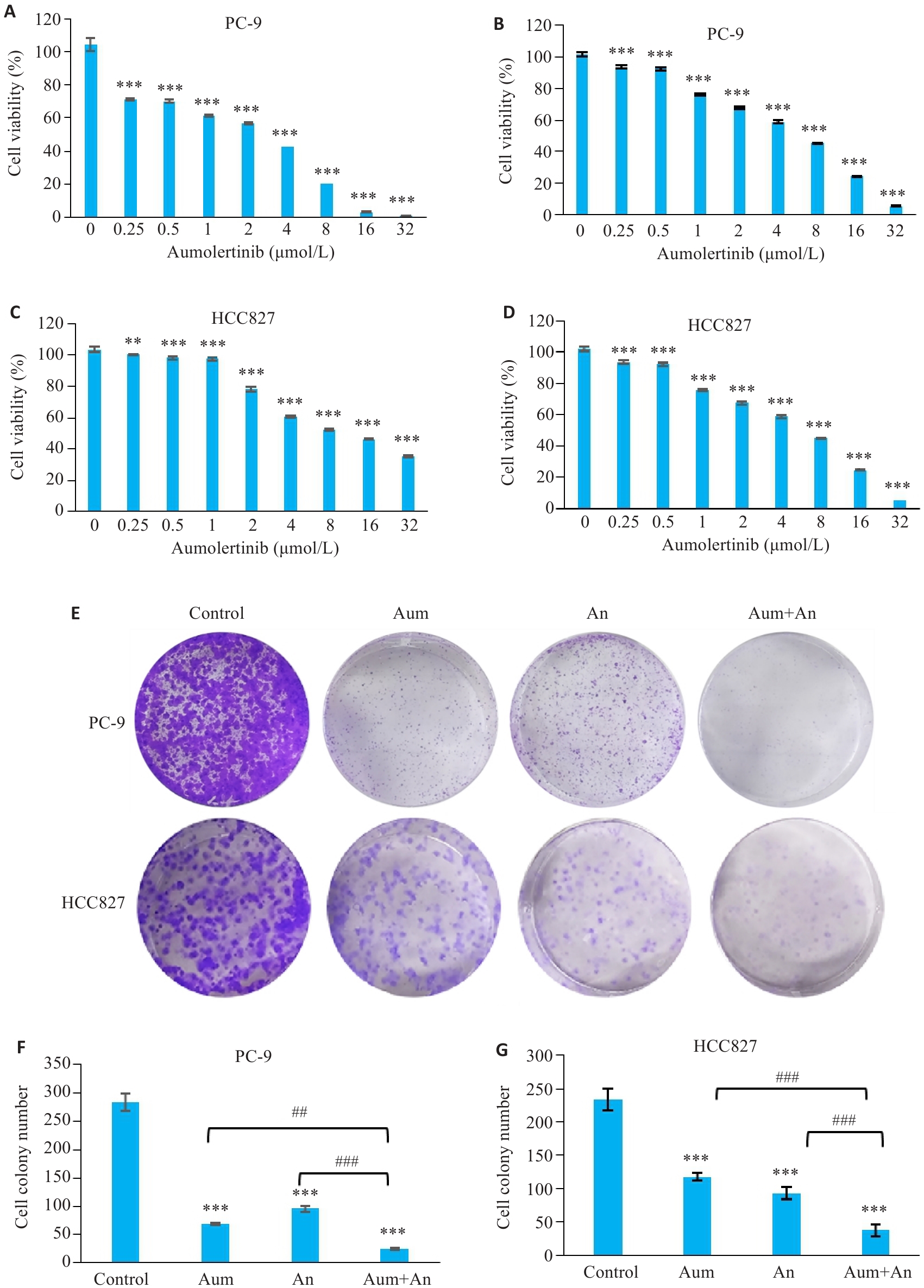
图1 Aum和An抑制NSCLC细胞增殖与存活
Fig.1 Aumolertinib (Aum), anlotinib (An) and their combination significantly inhibits NSCLC cell proliferation and survival. A: Effect of Aum on PC-9 cells. B: Inhibitory effect of An in PC-9 cells. C: Inhibitory effect of Aum in HCC827 cells. D. Inhibitory effect of An in HCC827 cells. E: Colony cloning. F, G: Statistics of colony formation in HCC827 cells, **P<0.01, ***P<0.001 vs 0 μmol/L Control, ##P<0.01, ###P<0.001.
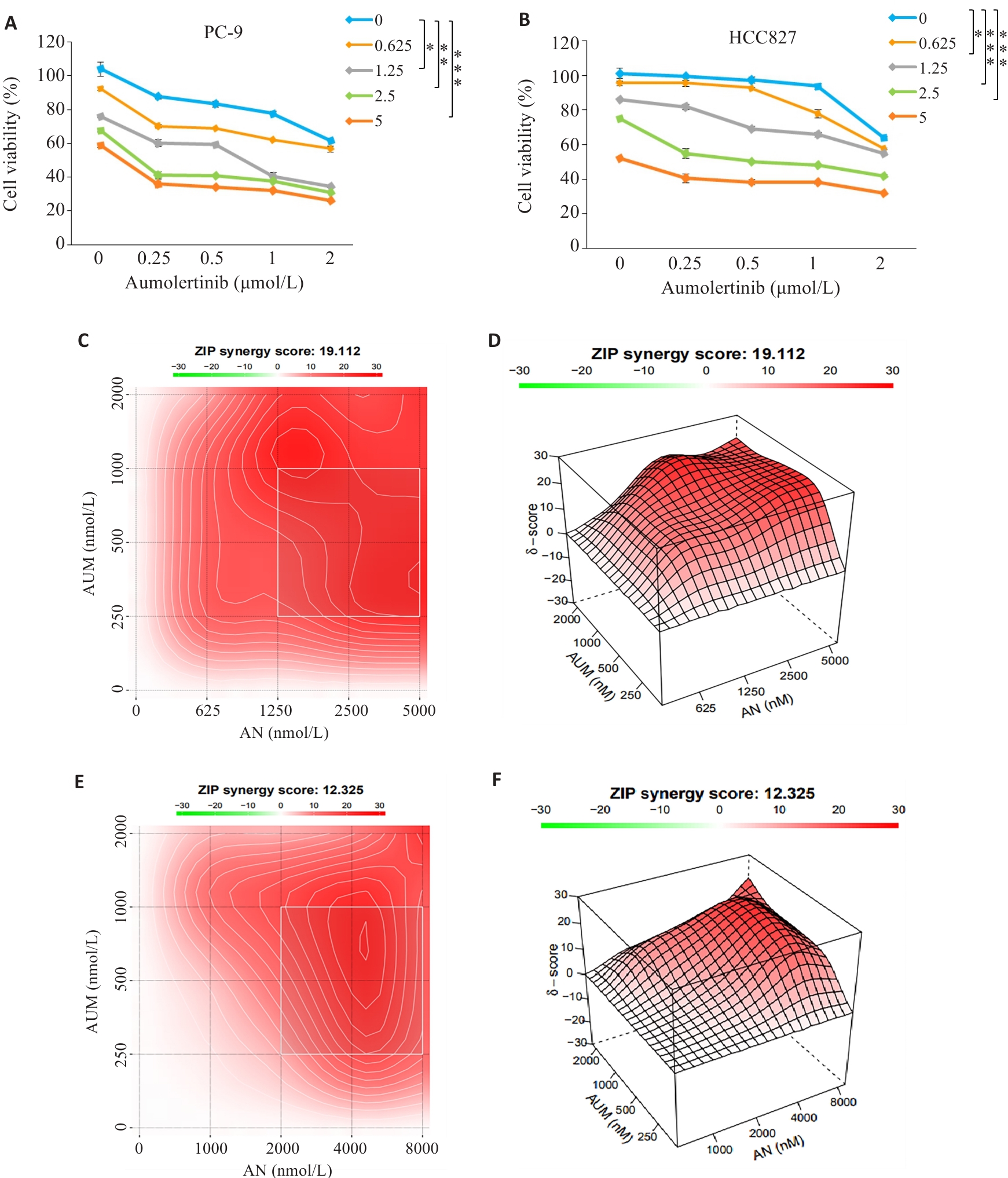
图2 Aum联合An对PC-9及HCC827细胞的抑制具有协同作用
Fig.2 Aumolertinib combined with anlotinib synergistically inhibit viability of PC-9 and HCC827 cells. A, B: CCK-8 assay. C, D: Synergy scores of Aumolertinib combined with anlotinib in PC-9 cells (ZIP<0 indicates an antagonistic effect of the two drugs, 0<ZIP<10 indicates that the two drugs have antagonistic effects, and 0<ZIP<10 indicates that the two drugs have antagonistic effect, and 0<ZIP<10 indicates that the two drugs have synergy effect). ZIP<10 indicates that the two drugs have additive effect, and 10<ZIP indicates that the two drugs have synergistic effect. E,F: Synergy scores of aumolertinib combined with anlotinib in HCC827 cells. *P<0.05, **P<0.01, ***P<0.001.
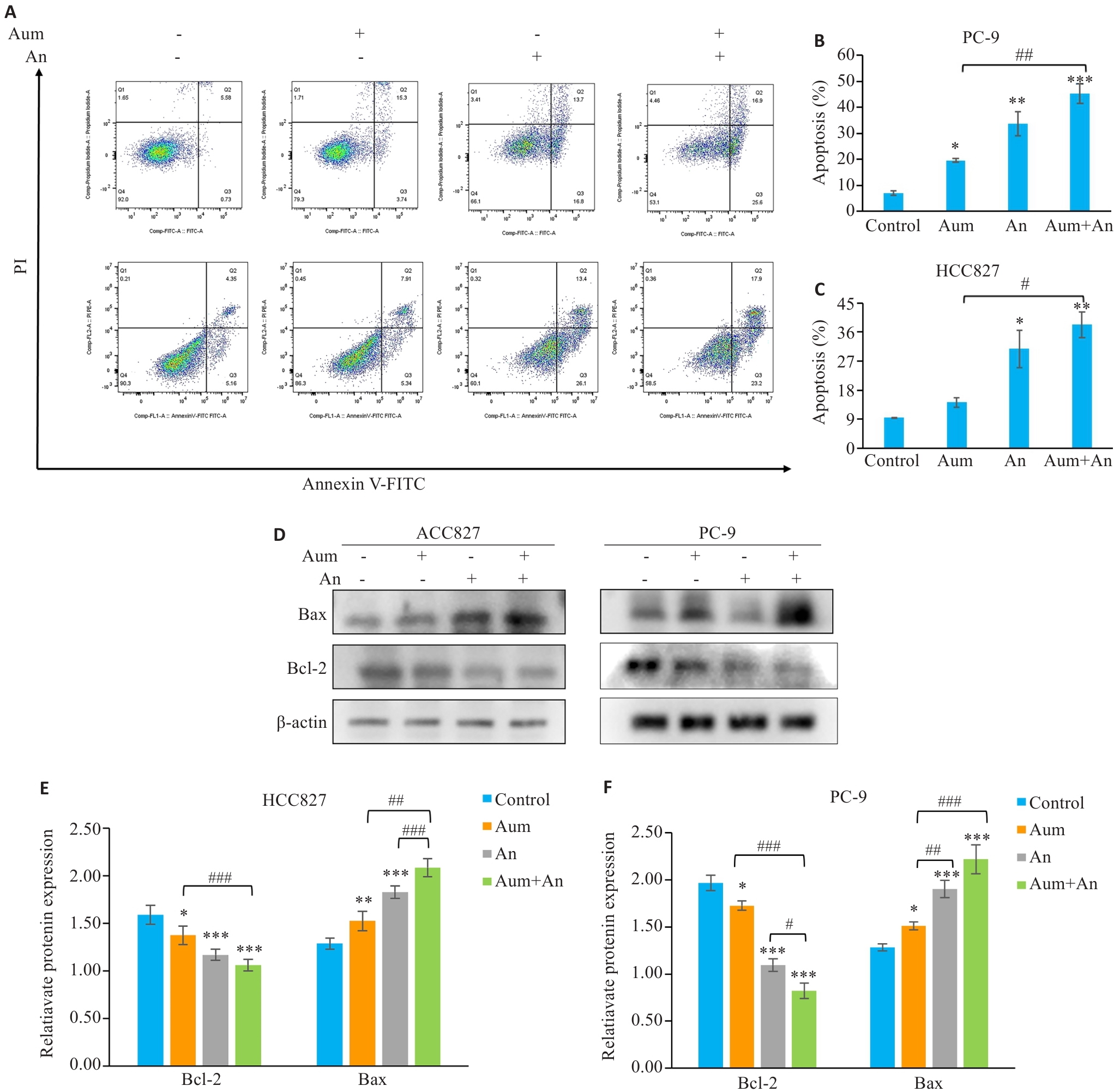
图 3 Aum联合An明显促进PC-9细胞及HCC827细胞的凋亡
Fig.3 Aumolertinib combined with anlotinib promotes apoptosis of PC-9 cells and HCC827 cells. A: Flow cytometric analysis of apoptosis in different treatment groups. B, C: Apoptosis rates in the 4 groups. D: Apoptosis-related proteins analyzed using protein immunoblotting; E,F: Quantitative analysis of apoptotic protein expression levels. *P<0.05, **P<0.01, ***P<0.001 vs control; #P<0.05, ##P<0.01, ###P<0.001.
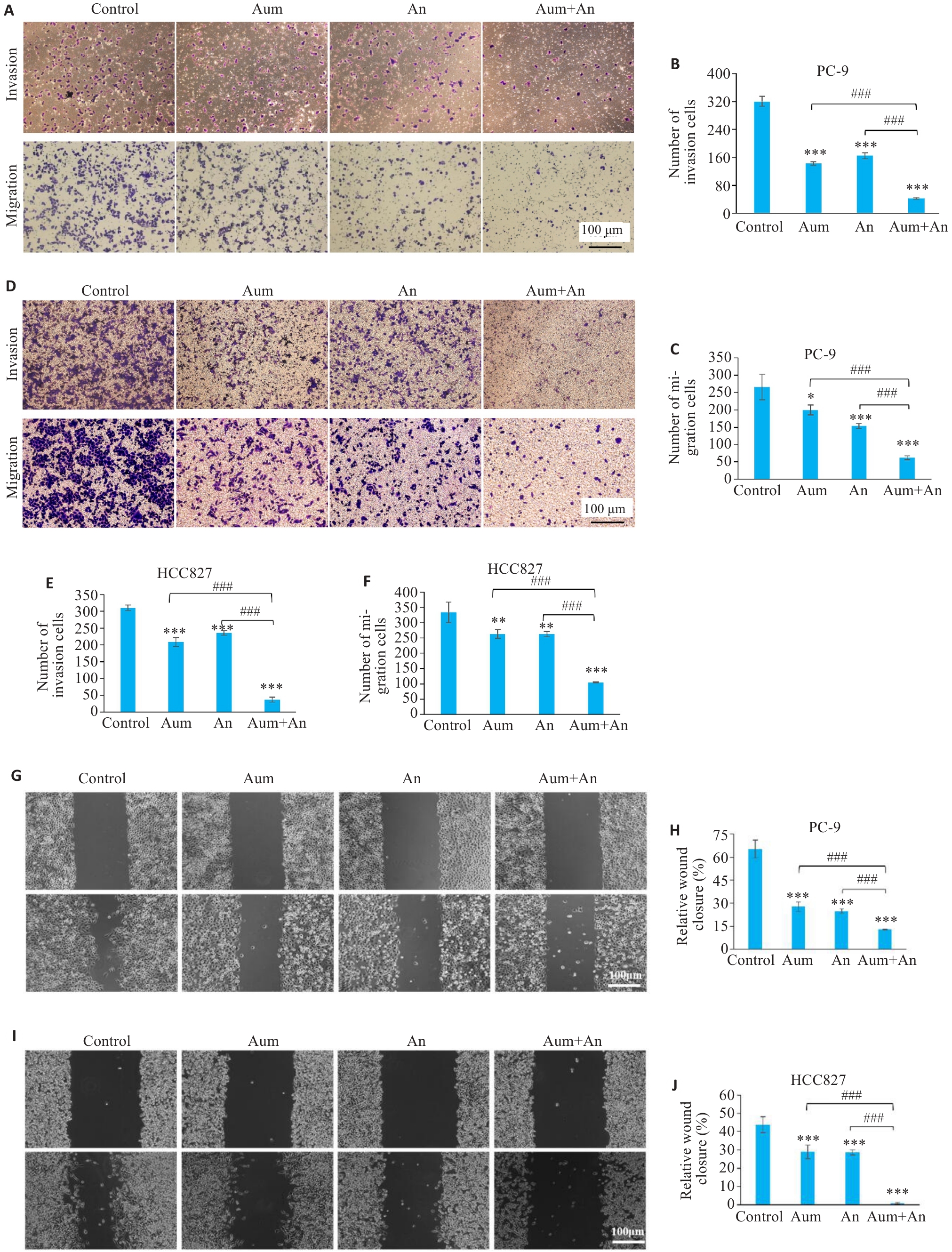
图4 Aum联合An抑制PC-9细胞及HCC827细胞的侵袭和迁移
Fig.4 Aumolertinib combined with anlotinib significantly inhibits invasion and migration of PC-9 cells and HCC827 cells. A,D: Transwell assay for assessing cell invasion and migration in different groups (crystalline violet staining, original magnification: ×200). G, I: Scratch assay for assessing migration ability of the cells in different groups (×200). H,J: Quantitative analysis of PC-9 and HCC827 cell migration. *P<0.05, **P<0.01, ***P<0.001 vs control; ###P<0.001.
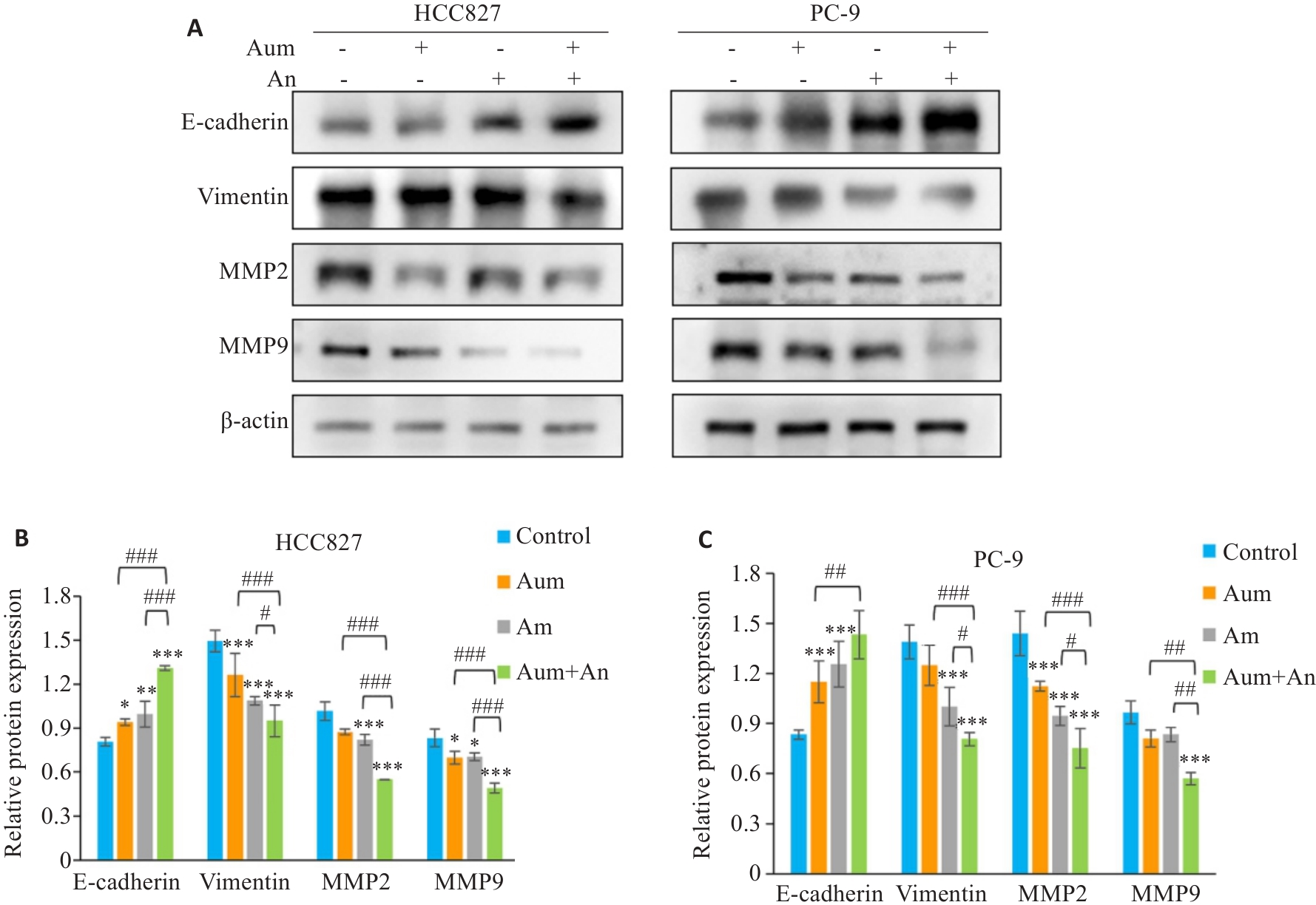
图 5 Aum联合An调控PC-9细胞及HCC827细胞的侵袭迁移相关蛋白的表达
Fig.5 Western blotting for the expression of E-cadherin, vimentin, MMP2 and MMP9 in PC-9 cells or HCC827 cells (A) and their relative of protein expression levels (B, C). *P<0.05, **P<0.05,***P<0.001 vs control; #P<0.05,##P<0.01, ###P<0.001.
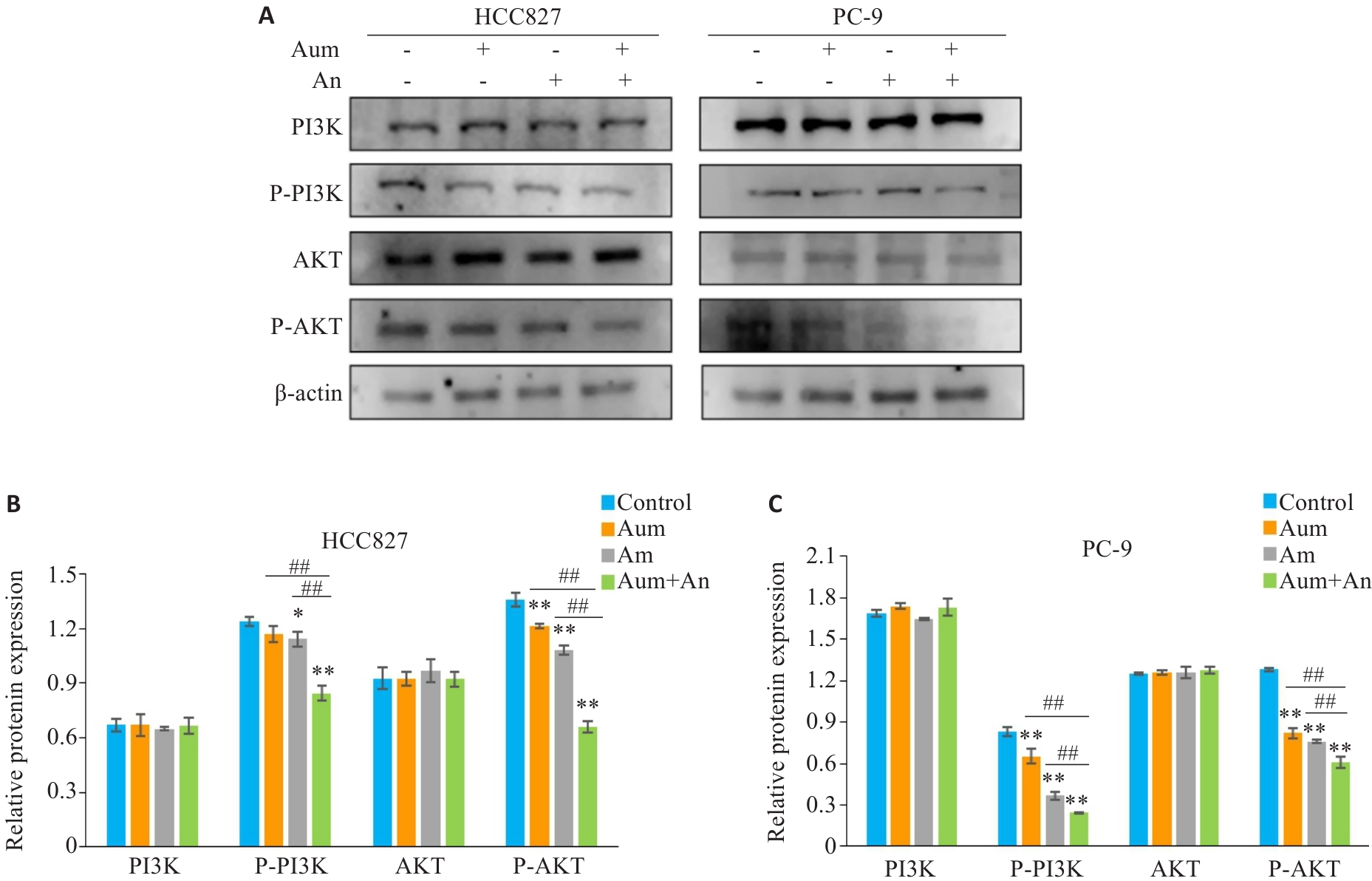
图6 Aum联合An通过阻断PI3K及Akt的磷酸化抑制PC-9细胞及HCC827细胞的侵袭和迁移
Fig.6 Aumolertinib combined with anlotinib inhibits invasion and migration of PC-9 cells and HCC827 cells by blocking phosphorylation of PI3K and Akt. A: Protein immunoblotting of PI3K-Akt pathway related proteins. B, C: Quantitative analysis of expression levels of PI3K-Akt pathway-related proteins. *P<0.05,**P<0.01 vs control,##P<0.01.
| 1 | Bray F, Laversanne M, Sung H, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2024, 74(3): 229-63. |
| 2 | Liang J, Guan XJ, Bao GY, et al. Molecular subtyping of small cell lung cancer[J]. Semin Cancer Biol, 2022, 86(Pt 2): 450-62. |
| 3 | Succony L, Rassl DM, Barker AP, et al. Adenocarcinoma spectrum lesions of the lung: detection, pathology and treatment strategies[J]. Cancer Treat Rev, 2021, 99: 102237. |
| 4 | Reck M, Remon J, Hellmann MD. First-line immunotherapy for non-small-cell lung cancer[J]. J Clin Oncol, 2022, 40(6): 586-97. |
| 5 | Zugazagoitia J, Paz-Ares L. Extensive-Stage Small-Cell Lung Cancer: First-Line and Second-Line Treatment Options [J]. J Clin Oncol, 2022, 40(6): 671-80. |
| 6 | Chaft JE, Shyr Y, Sepesi B, et al. Preoperative and postoperative systemic therapy for operable non-small-cell lung cancer[J]. J Clin Oncol, 2022, 40(6): 546-55. |
| 7 | Ge X, Zhang Y, Huang F, et al. EGFR tyrosine kinase inhibitor Almonertinib induces apoptosis and autophagy mediated by reactive oxygen species in non-small cell lung cancer cells[J]. Hum Exp Toxicol, 2021, 40(): S49-S62. |
| 8 | Han BH, Li K, Wang QM, et al. Effect of anlotinib as a third-line or further treatment on overall survival of patients with advanced non-small cell lung cancer: the ALTER 0303 phase 3 randomized clinical trial[J]. JAMA Oncol, 2018, 4(11): 1569-75. |
| 9 | Shen GS, Zheng FC, Ren DF, et al. Anlotinib: a novel multi-targeting tyrosine kinase inhibitor in clinical development[J]. J Hematol Oncol, 2018, 11(1): 120. |
| 10 | Syed YY. Anlotinib: first global approval[J]. Drugs, 2018, 78(10): 1057-62. |
| 11 | Hou ZW, Wu HG, Luo NN, et al. Almonertinib combined with anlotinib and temozolomide in a patient with recurrent glioblastoma with EGFR L858R mutation[J]. Oncologist, 2023, 28(5): 449-52. |
| 12 | Li T, Chang KJ, Qiu X, et al. A pilot study of anlotinib with third-generation epidermal growth factor receptor tyrosine kinase inhibitors in untreated EGFR-mutant patients with advanced non-small cell lung cancer[J]. Transl Lung Cancer Res, 2023, 12(6): 1256-63. |
| 13 | Chen LK, Chen J, Li MC, et al. OA03.03 aumolertinib plus anlotinib in advanced NSCLC with brain metastasis: a single-arm, phase II study[J]. J Thorac Oncol, 2023, 18(11): S48-9. |
| 14 | Yang Q, Jiang W, Hou P. Emerging role of PI3K/AKT in tumor-related epigenetic regulation[J]. Semin Cancer Biol, 2019, 59: 112-24. |
| 15 | Xu ZR, Han X, Ou DM, et al. Targeting PI3K/AKT/mTOR-mediated autophagy for tumor therapy[J]. Appl Microbiol Biotechnol, 2020, 104(2): 575-87. |
| 16 | Kim SH, Seung BJ, Cho SH, et al. Dysregulation of PI3K/akt/PTEN pathway in canine mammary tumor[J]. Animals, 2021, 11(7): 2079. |
| 17 | Lu T, Wang Y, Liu F, et al. Synergistic Inhibitory Effect of Berberine and Low-Temperature Plasma on Non-Small-Cell Lung Cancer Cells via PI3K-AKT-Driven Signaling Axis [J]. Molecules, 2023, 28(23). |
| 18 | Moghbeli M. PI3K/AKT pathway as a pivotal regulator of epithelial-mesenchymal transition in lung tumor cells[J]. Cancer Cell Int, 2024, 24(1): 165. |
| 19 | Chen CL, Guo Y, Huang QS, et al. PI3K inhibitor impairs tumor progression and enhances sensitivity to anlotinib in anlotinib-resistant osteosarcoma[J]. Cancer Lett, 2022, 536: 215660. |
| 20 | Zhang ZR, Zhang MX, Liu H, et al. AZD9291 promotes autophagy and inhibits PI3K/Akt pathway in NSCLC cancer cells[J]. J Cell Biochem, 2019, 120(1): 756-67. |
| 21 | Lv YH, Du TT, Ji M, et al. A novel PI3K/mTOR dual inhibitor XH002 exhibited robust antitumor activity in NSCLC[J]. J Drug Target, 2019, 27(4): 451-9. |
| 22 | Ciuffreda L, Incani UC, Steelman LS, et al. Signaling intermediates (MAPK and PI3K) as therapeutic targets in NSCLC[J]. Curr Pharm Des, 2014, 20(24): 3944-57. |
| 23 | Erira A, Velandia F, Penagos J, et al. Differential regulation of the EGFR/PI3K/AKT/PTEN pathway between low- and high-grade gliomas[J]. Brain Sci, 2021, 11(12): 1655. |
| 24 | Lin BY, Song XM, Yang DW, et al. Anlotinib inhibits angiogenesis via suppressing the activation of VEGFR2, PDGFRβ and FGFR1[J]. Gene, 2018, 654: 77-86. |
| 25 | Qin TT, Liu ZJ, Wang J, et al. Anlotinib suppresses lymphangiogenesis and lymphatic metastasis in lung adeno-carcinoma through a process potentially involving VEGFR-3 signaling[J]. Cancer Biol Med, 2020, 17(3): 753-67. |
| 26 | Hong C, Wei JP, Zhou T, et al. FGFR2-ERC1: a subtype of FGFR2 oncogenic fusion variant in lung adenocarcinoma and the response to anlotinib[J]. Onco Targets Ther, 2022, 15: 651-7. |
| 27 | Liang LJ, Hui KY, Hu CX, et al. Autophagy inhibition potentiates the anti-angiogenic property of multikinase inhibitor anlotinib through JAK2/STAT3/VEGFA signaling in non-small cell lung cancer cells[J]. J Exp Clin Cancer Res, 2019, 38(1): 71. |
| 28 | de Carlo E, Bertoli E, del Conte A, et al. Brain metastases management in oncogene-addicted non-small cell lung cancer in the targeted therapies era[J]. Int J Mol Sci, 2022, 23(12): 6477. |
| 29 | Sun JJ, Wu SK, Jin ZX, et al. Lymph node micrometastasis in non-small cell lung cancer[J]. Biomedecine Pharmacother, 2022, 149: 112817. |
| 30 | Tan AC. Targeting the PI3K/Akt/mTOR pathway in non-small cell lung cancer (NSCLC)[J]. Thorac Cancer, 2020, 11(3): 511-8. |
| 31 | Han D, Zhang JJ, Bao YW, et al. Anlotinib enhances the antitumor immunity of radiotherapy by activating cGAS/STING in non-small cell lung cancer[J]. Cell Death Discov, 2022, 8(1): 468. |
| 32 | Wang J, Xu Z, Lai Y, et al. Anlotinib Inhibiting Mantle Cell Lymphoma Proliferation and Inducing Apoptosis through PI3K/AKT/mTOR Pathway [J]. Current Molecular Medicine, 2024, 24. |
| 33 | Zhang LL, Wang LC, Wang JY, et al. Anlotinib plus icotinib as a potential treatment option for EGFR-mutated advanced non-squamous non-small cell lung cancer with concurrent mutations: final analysis of the prospective phase 2, multicenter ALTER-L004 study[J]. Mol Cancer, 2023, 22(1): 124. |
| 34 | Zhao HY, Yao WX, Min XH, et al. Apatinib plus gefitinib as first-line treatment in advanced EGFR-mutant NSCLC: the phase III ACTIVE study (CTONG1706)[J]. J Thorac Oncol, 2021, 16(9): 1533-46. |
| 35 | 杜宝萍, 梁诗欣, 余 辉, 等. EGFR T790M抑制剂联合安罗替尼治疗非小细胞肺癌疗效的回顾分析[J]. 今日药学, 2023, 33(12): 922-7. |
| 36 | Zhao Y, Li SY, Yang X, et al. Overall survival benefit of osimertinib and clinical value of upfront cranial local therapy in untreated EGFR-mutant nonsmall cell lung cancer with brain metastasis[J]. Int J Cancer, 2022, 150(8): 1318-28. |
| 37 | Lu W, Kang YB. Epithelial-mesenchymal plasticity in cancer progression and metastasis[J]. Dev Cell, 2019, 49(3): 361-74. |
| 38 | Lamouille S, Xu J, Derynck R. Molecular mechanisms of epithelial-mesenchymal transition[J]. Nat Rev Mol Cell Biol, 2014, 15(3): 178-96. |
| 39 | Jiang Y, Han QJ, Zhao HJ, et al. Promotion of epithelial-mesenchymal transformation by hepatocellular carcinoma-educated macrophages through Wnt2b/β‑catenin/c-Myc signaling and reprogramming glycolysis[J]. J Exp Clin Cancer Res, 2021, 40(1): 13. |
| 40 | Zhang GF, Zheng G, Zhang HP, et al. MUC1 induces the accumulation of Foxp3+ Treg cells in the tumor microenvironment to promote the growth and metastasis of cholangiocarcinoma through the EGFR/PI3K/Akt signaling pathway[J]. Int Immunopharmacol, 2023, 118: 110091. |
| 41 | Yang SC, Liu Y, Li MY, et al. FOXP3 promotes tumor growth and metastasis by activating Wnt/β-catenin signaling pathway and EMT in non-small cell lung cancer[J]. Mol Cancer, 2017, 16(1): 124. |
| 42 | Feng X, Xu ES. Alectinib and lorlatinib function by modulating EMT-related proteins and MMPs in NSCLC metastasis[J]. Bosn J Basic Med Sci, 2021, 21(3): 331-8. |
| 43 | Emery S, Fieux S, Vidal B, et al. Preclinical validation of [(18)F]2FNQ1P as a specific PET radiotracer of 5-HT(6) receptors in rat, pig, non-human primate and human brain tissue[J]. Nucl Med Biol, 2020, 82/83: 57-63. |
| 44 | Kessenbrock K, Plaks V, Werb Z. Matrix metalloproteinases: regulators of the tumor microenvironment[J]. Cell, 2010, 141(1): 52-67. |
| 45 | Scheau C, Badarau I A, Costache R, et al. The Role of Matrix Metalloproteinases in the Epithelial-Mesenchymal Transition of Hepatocellular Carcinoma [J]. Analytical Cellular Pathology, 2019, 2019: 1-10. |
| 46 | Scheau C, Badarau IA, Costache R, et al. The role of matrix metalloproteinases in the epithelial-mesenchymal transition of hepatocellular carcinoma[J]. Anal Cell Pathol, 2019, 2019: 9423907. |
| 47 | Rashid ZA, Bardaweel SK. Novel matrix metalloproteinase-9 (MMP-9) inhibitors in cancer treatment[J]. Int J Mol Sci, 2023, 24(15): 12133. |
| 48 | Miao Y, Bi XY, Zhao M, et al. Acetylcholine inhibits tumor necrosis factor α activated endoplasmic reticulum apoptotic pathway via EGFR-PI3K signaling in cardiomyocytes[J]. J Cell Physiol, 2015, 230(4): 767-74. |
| 49 | Tang M, Deng HD, Zheng KL, et al. Ginsenoside 3β‑O-Glc-DM (C3DM) suppressed glioma tumor growth by downregulating the EGFR/PI3K/AKT/mTOR signaling pathway and modulating the tumor microenvironment[J]. Toxicol Appl Pharmacol, 2023, 460: 116378. |
| 50 | Shirley M, Keam SJ. Aumolertinib: a review in non-small cell lung cancer[J]. Drugs, 2022, 82(5): 577-84. |
| 51 | He JY, Huang ZR, Han LZ, et al. Mechanisms and management of 3rd-generation EGFR-TKI resistance in advanced non-small cell lung cancer (Review)[J]. Int J Oncol, 2021, 59(5): 90. |
| 52 | Qu QH, Jiang SZ, Li XY. LncRNA TBX5-AS1 regulates the tumor progression through the PI3K/AKT pathway in non-small cell lung cancer[J]. Onco Targets Ther, 2020, 13: 7949-61. |
| 53 | Zhang D, Deng T, Yuan W, et al. Glaucocalyxin A induces apoptosis of non-small cell lung carcinoma cells by inhibiting the PI3K/Akt/GSK3β pathway[J]. Clin Exp Pharmacol Physiol, 2022, 49(8): 797-804. |
| 54 | Zhou J, Peng Y, Gao YC, et al. Targeting DNAJC19 overcomes tumor growth and lung metastasis in NSCLC by regulating PI3K/AKT signaling[J]. Cancer Cell Int, 2021, 21(1): 338. |
| 55 | Cao SY, Li LF, Li J, et al. MiR-1299 impedes the progression of non-small-cell lung cancer through EGFR/PI3K/AKT signaling pathway[J]. Onco Targets Ther, 2020, 13: 7493-502. |
| 56 | Yang F, Zheng YF, Luo Q, et al. Knockdown of NCAPD3 inhibits the tumorigenesis of non-small cell lung cancer by regulation of the PI3K/Akt pathway[J]. BMC Cancer, 2024, 24(1): 408. |
| 57 | Guan JK, Borenäs M, Xiong JF, et al. IGF1R contributes to cell proliferation in ALK-mutated neuroblastoma with preference for activating the PI3K-AKT signaling pathway[J]. Cancers, 2023, 15(17): 4252. |
| 58 | Bang J, Jun M, Lee S, et al. Targeting EGFR/PI3K/AKT/mTOR signaling in hepatocellular carcinoma[J]. Pharmaceutics, 2023, 15(8): 2130. |
| 59 | Shi C, Zhang C, Fu ZW, et al. Antitumor activity of aumolertinib, a third-generation EGFR tyrosine kinase inhibitor, in non-small-cell lung cancer harboring uncommon EGFR mutations[J]. Acta Pharm Sin B, 2023, 13(6): 2613-27. |
| 60 | Liu YL, Li F, Wang QY, et al. Anlotinib inhibits growth of human esophageal cancer TE-1 cells by negative regulating PI3K/Akt signaling pathway[J]. Discov Oncol, 2024, 15(1): 134. |
| 61 | Lu YF, Lin J, Duan M, et al. Anlotinib suppresses oral squamous cell carcinoma growth and metastasis by targeting the RAS protein to inhibit the PI3K/akt signalling pathway[J]. Anal Cell Pathol, 2021, 2021: 5228713. |
| 62 | Chen QL, Lai Q, Jiang YL, et al. Anlotinib exerts potent antileukemic activities in Ph chromosome negative and positive B-cell acute lymphoblastic leukemia via perturbation of PI3K/AKT/mTOR pathway[J]. Transl Oncol, 2022, 25: 101516. |
| [1] | 常笑语, 张瀚文, 曹红亭, 侯玲, 孟鑫, 陶虹, 罗彦, 李光华. 热应激对大鼠胸主动脉内皮细胞生物钟基因 Bmal1和细胞周期蛋白表达水平的影响[J]. 南方医科大学学报, 2025, 45(7): 1353-1362. |
| [2] | 何丽君, 陈晓菲, 闫陈昕, 师林. 扶正化积汤治疗非小细胞肺癌的分子机制:基于网络药理学及体外实验验证[J]. 南方医科大学学报, 2025, 45(6): 1143-1152. |
| [3] | 李嘉豪, 冼瑞婷, 李荣. 下调ACADM介导的脂毒性抑制雌激素受体阳性乳腺癌细胞的侵袭与转移[J]. 南方医科大学学报, 2025, 45(6): 1163-1173. |
| [4] | 杨毓甲, 杨丽芳, 吴雅玲, 段兆达, 于春泽, 吴春云, 于建云, 杨力. 大麻二酚经PERK-eIF2α-ATF4-CHOP通路减轻多重脑震荡大鼠的神经元内质网应激和凋亡[J]. 南方医科大学学报, 2025, 45(6): 1240-1250. |
| [5] | 李丹丹, 楚佳鑫, 闫妍, 徐文隽, 朱行春, 孙韵, 丁浩峰, 任丽, 朱博. 姜黄素通过下调HIF-1α通路抑制非小细胞肺癌脂质代谢[J]. 南方医科大学学报, 2025, 45(5): 1039-1046. |
| [6] | 陈悦, 肖林雨, 任侣, 宋雪, 李静, 胡建国. 水晶兰苷通过抑制PI3K/AKT信号通路减少神经元凋亡改善脊髓损伤后小鼠的运动功能[J]. 南方医科大学学报, 2025, 45(4): 774-784. |
| [7] | 储菲, 陈孝华, 宋博文, 杨晶晶, 左芦根. 苏荠宁黄酮通过抑制PI3K/AKT信号通路拮抗肠上皮细胞凋亡改善小鼠实验性结肠炎[J]. 南方医科大学学报, 2025, 45(4): 819-828. |
| [8] | 张毅, 沈昱, 万志强, 陶嵩, 柳亚魁, 王栓虎. CDKN3高表达促进胃癌细胞的迁移和侵袭:基于调控p53/NF-κB信号通路和抑制胃癌细胞凋亡[J]. 南方医科大学学报, 2025, 45(4): 853-861. |
| [9] | 陈镝, 吕莹, 郭怡欣, 张怡荣, 王蕊璇, 周小若, 陈雨欣, 武晓慧. 双氢青蒿素可显著增强阿霉素诱导的三阴性乳腺癌细胞凋亡:基于负向调控STAT3/HIF-1α通路[J]. 南方医科大学学报, 2025, 45(2): 254-260. |
| [10] | 宾禹, 李子雯, 左素微, 孙思诺, 李敏, 宋佳茵, 林旭, 薛刚, 吴靖芳. 载脂蛋白C1高表达通过激活JAK2/STAT3信号通路促进甲状腺乳头状癌细胞的增殖并抑制凋亡[J]. 南方医科大学学报, 2025, 45(2): 359-370. |
| [11] | 钟娜, 王会杰, 赵文英, 孙珍贵, 耿彪. 高表达RNF7增强非小细胞肺癌细胞的PD-1耐药:基于活化NF-kB通路促进CXCL1表达和髓源性抑制细胞的募集[J]. 南方医科大学学报, 2024, 44(9): 1704-1711. |
| [12] | 刘硕, 李静, 吴兴旺. Swertiamarin通过抑制肠上皮细胞细胞凋亡改善TNBS诱导的实验性结肠炎[J]. 南方医科大学学报, 2024, 44(8): 1545-1552. |
| [13] | 从小凡, 陈腾, 李硕, 王媛媛, 周龙云, 李小龙, 张配, 孙小锦, 赵素容. 双氢青蒿素通过促进活性氧的产生增强鼻咽癌细胞对顺铂诱导凋亡的敏感性[J]. 南方医科大学学报, 2024, 44(8): 1553-1560. |
| [14] | 肖林雨, 段婷, 夏勇生, 陈悦, 孙洋, 许轶博, 徐磊, 闫兴洲, 胡建国. 蒙花苷通过抑制TLR4/NF-κB通路抑制小鼠脊髓损伤后小胶质细胞活化介导的神经炎症和神经元凋亡[J]. 南方医科大学学报, 2024, 44(8): 1589-1598. |
| [15] | 陶怀祥, 骆金光, 闻志远, 虞亘明, 苏萧, 王鑫玮, 关翰, 陈志军. STING高表达通过调控TLR4/NF-κB/NLRP3通路和影响炎症与凋亡水平促进小鼠肾脏缺血再灌注损伤[J]. 南方医科大学学报, 2024, 44(7): 1345-1354. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||