南方医科大学学报 ›› 2026, Vol. 46 ›› Issue (1): 200-207.doi: 10.12122/j.issn.1673-4254.2026.01.22
孙送送1,2( ), 陶泉1,2, 赵凯旋3, 胡秋根4, 冯衍秋1,2,4(
), 陶泉1,2, 赵凯旋3, 胡秋根4, 冯衍秋1,2,4( )
)
收稿日期:2025-07-20
出版日期:2026-01-20
发布日期:2026-01-16
通讯作者:
冯衍秋
E-mail:sunsongsong02@163.com;foree@163.com
作者简介:孙送送,在读硕士研究生,E-mail: sunsongsong02@163.com
基金资助:
Songsong SUN1,2( ), Quan TAO1,2, Kaixuan ZHAO3, Qiugen HU4, Yanqiu FENG1,2,4(
), Quan TAO1,2, Kaixuan ZHAO3, Qiugen HU4, Yanqiu FENG1,2,4( )
)
Received:2025-07-20
Online:2026-01-20
Published:2026-01-16
Contact:
Yanqiu FENG
E-mail:sunsongsong02@163.com;foree@163.com
Supported by:摘要:
目的 通过高时间分辨率动态T2*加权平面回波成像(T2*W-EPI)监测大鼠肾脏在阶跃氧刺激下的氧合水平变化。 方法 对SD大鼠(n=10)施加2 min高氧(100% O2)-10 min低氧(10% O2)-10 min高氧(100% O2)的阶跃氧刺激,在9.4 T小动物磁共振扫描仪上连续采集多回波梯度回波序列(mGRE)及梯度回波-平面回波成像(EPI)序列的肾脏动态MRI数据,2种序列的时间分辨率分别为9 s、1 s。对大鼠肾脏不同感兴趣区域(ROI)的动态时间序列曲线建立二阶阶跃响应模型,并定量得到阶跃响应模型参数,包括时间延迟∆t、自然频率
孙送送, 陶泉, 赵凯旋, 胡秋根, 冯衍秋. 基于大鼠肾脏阶跃氧刺激的高时间分辨率动态T2*W成像研究[J]. 南方医科大学学报, 2026, 46(1): 200-207.
Songsong SUN, Quan TAO, Kaixuan ZHAO, Qiugen HU, Yanqiu FENG. A high temporal resolution dynamic T2*W imaging study based on step oxygen stimulation of rat kidneys[J]. Journal of Southern Medical University, 2026, 46(1): 200-207.
| MR scan sequence | RARE | mGRE | FID-EPI |
|---|---|---|---|
| TE (ms) | 45 | 2-33.05 (∆TE=2.07) | 8.458 |
| TR (ms) | 3500 | 40.553 | 1000 |
| FA (°) | - | 15 | 60 |
| FOV (mm2) | 55×55 | 55×55 | 55×55 |
| Matrix size | 110×110 | 110×110 | 110×110 |
| Slice thickness (mm) | 1 | 1 | 1 |
| Resolution (mm2) | 0.5×0.5 | 0.5×0.5 | 0.5×0.5 |
| Averages | 2 | 1 | 1 |
| Rare factor | 16 | - | - |
| Bandwidth (kHz) | - | - | 666.7 |
| Scan time (s) | 42 | 9 | 1 |
表1 各序列具体的MR扫描参数
Tab.1 MR scan parameters for each sequence
| MR scan sequence | RARE | mGRE | FID-EPI |
|---|---|---|---|
| TE (ms) | 45 | 2-33.05 (∆TE=2.07) | 8.458 |
| TR (ms) | 3500 | 40.553 | 1000 |
| FA (°) | - | 15 | 60 |
| FOV (mm2) | 55×55 | 55×55 | 55×55 |
| Matrix size | 110×110 | 110×110 | 110×110 |
| Slice thickness (mm) | 1 | 1 | 1 |
| Resolution (mm2) | 0.5×0.5 | 0.5×0.5 | 0.5×0.5 |
| Averages | 2 | 1 | 1 |
| Rare factor | 16 | - | - |
| Bandwidth (kHz) | - | - | 666.7 |
| Scan time (s) | 42 | 9 | 1 |
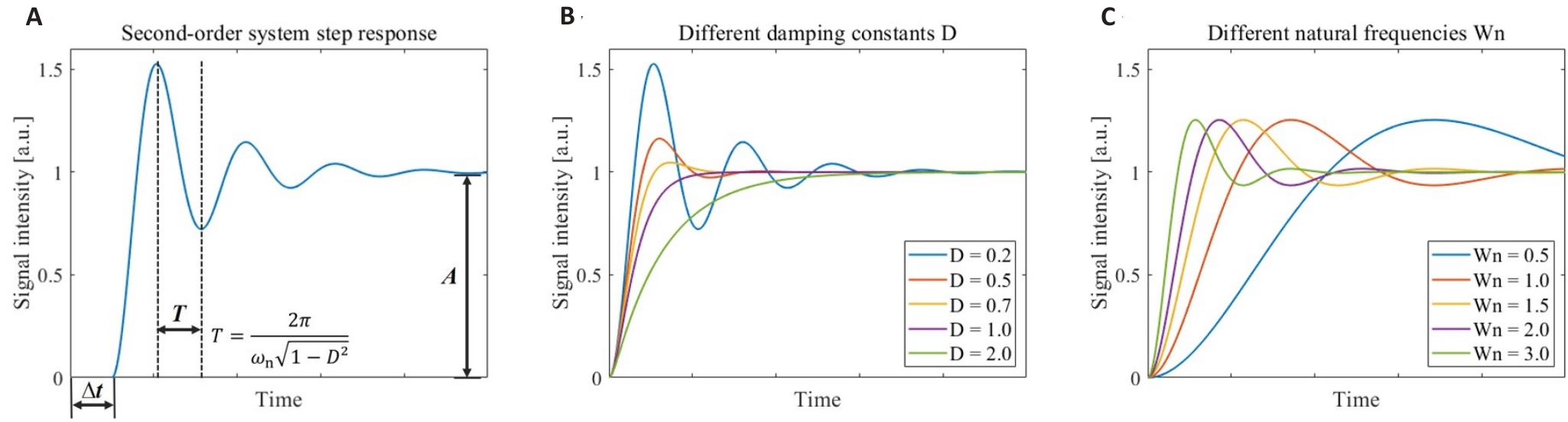
图1 二阶连续时间系统的阶跃响应模型
Fig.1 Step response models for the second-order continuous-time system. A: Step response of the second-order system and the significance of its model parameters. B: Step response of the second-order system corresponding to different damping constants D. C: Step response of the second-order system corresponding to different natural frequencies ωn.
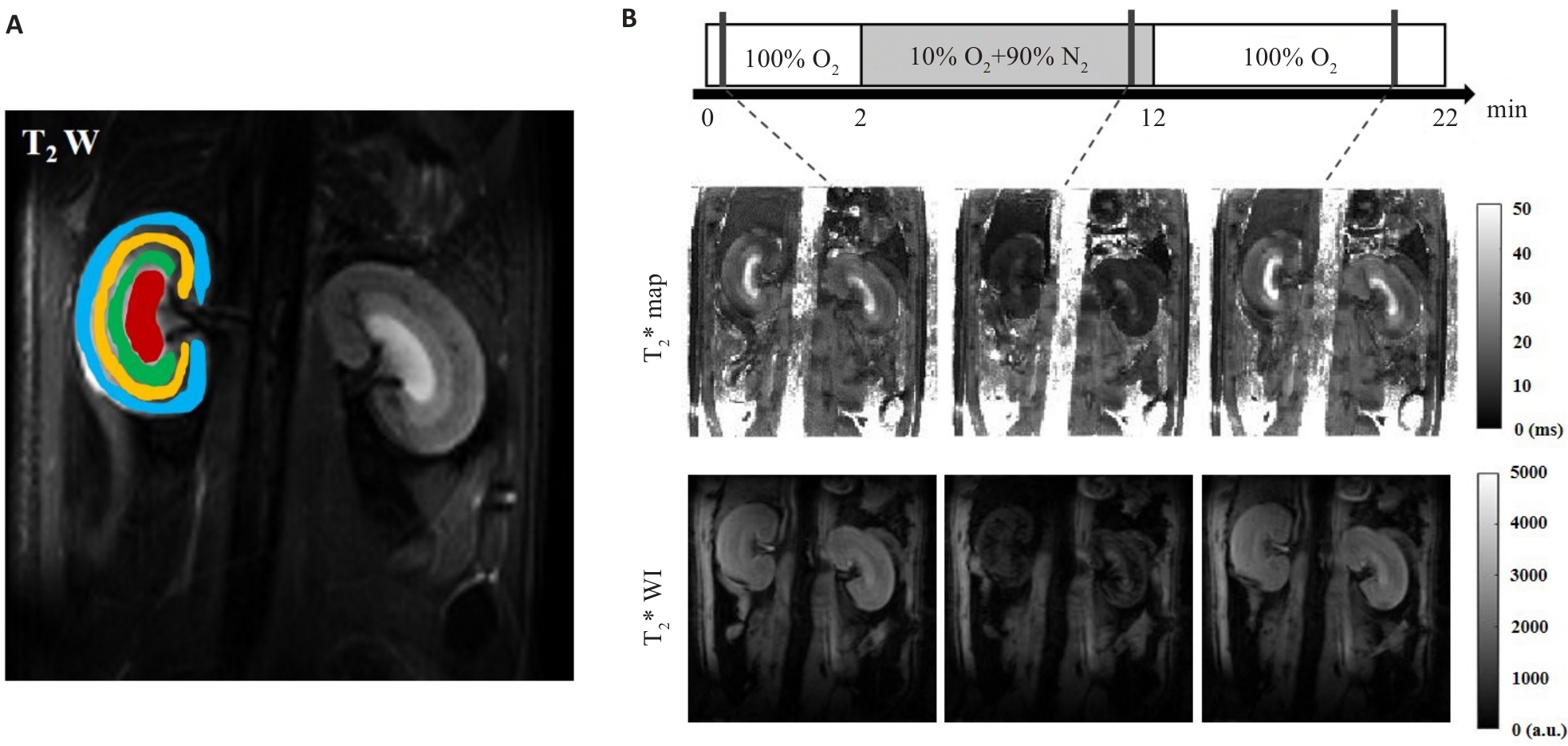
图3 在大鼠肾脏T2WI上勾画ROI(CO蓝色, OSOM黄色, ISOM绿色, IM红色)以及气体刺激时序图和在气体刺激各阶段对应的T2*map和T2*WI
Fig.3 Placement of ROIs on T2WI obtained from MRI (A) and gas challenge protocol, T2*map and T2*WI acquired at each stage of gas challenge (B). ROI placement 4 anatomical layers of kidney-CO (blue), OSOM (yellow), ISOM (green), and IM (red) were used.
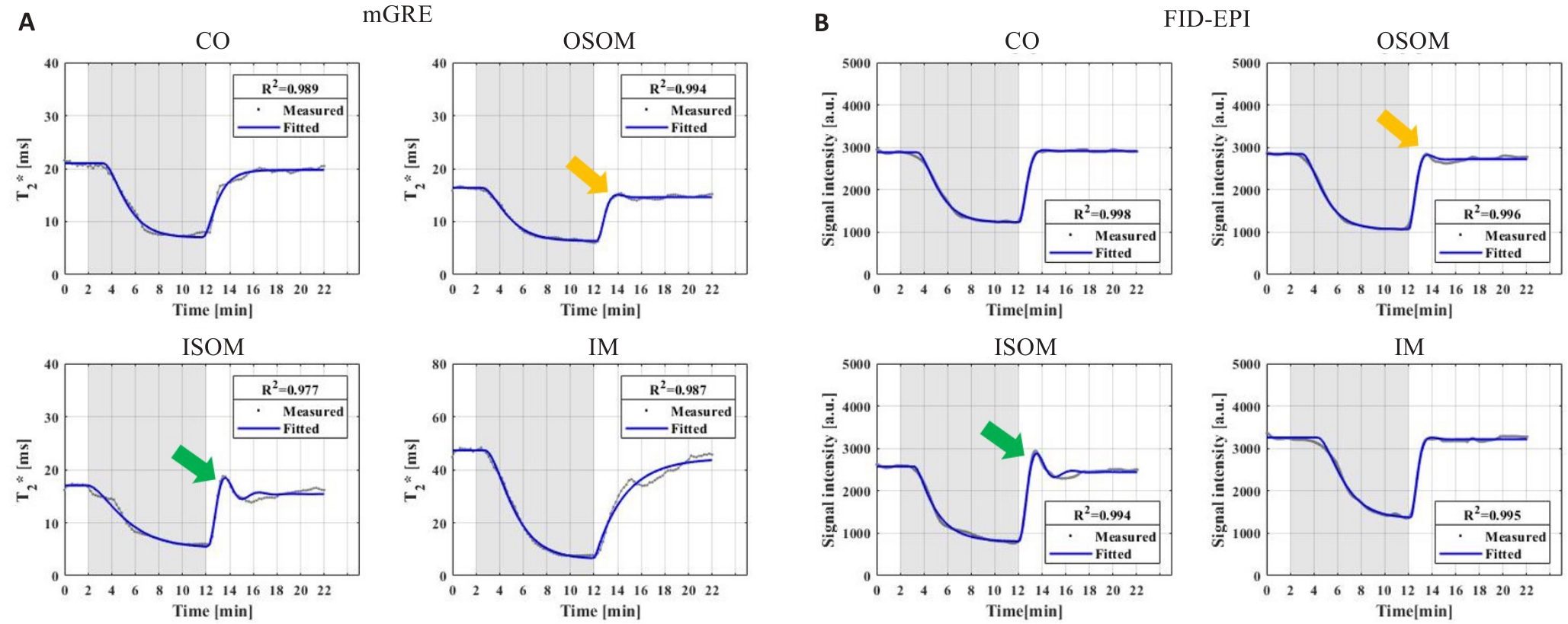
图4 大鼠肾脏CO, OSOM, ISOM及IM的动态时间序列曲线
Fig.4 Dynamic T2* sequence curves (A) and dynamic T2*W signal sequence curves (B) in renal CO, OSOM, ISOM and IM of the same rat. The yellow and green arrows represent the overshoot phenomena of OSOM and ISOM, respectively.
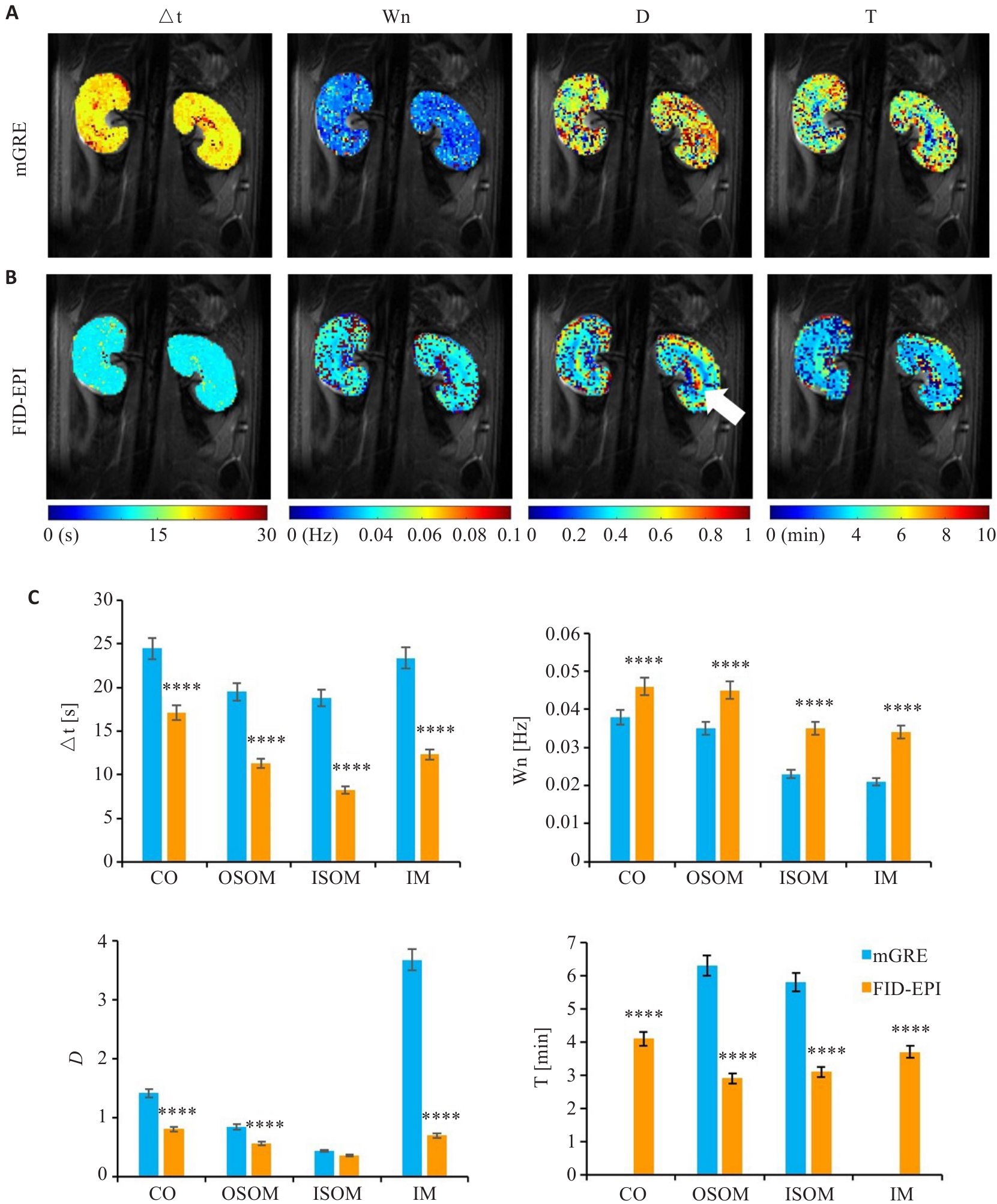
图5 mGRE和FID-EPI序列的动态数据的模型参数分析
Fig.5 Model parameter analysis of dynamic data of mGRE and FID-EPI sequences. A: Model parameter maps of mGRE. B: Model parameter maps of FID-EPI. C: Comparison of model parameters. ****P<0.0001 vs mGRE.
| [1] | Preuss HG. Basics of renal anatomy and physiology[J]. Clin Lab Med, 1993, 13(1): 1-11. doi:10.1016/s0272-2712(18)30456-6 |
| [2] | Bane O, Seeliger E, Cox E, et al. Renal MRI: from nephron to NMR signal[J]. J Magn Reson Imaging, 2023, 58(6): 1660-79. doi:10.1002/jmri.28828 |
| [3] | Levassort H, Essig M. The kidney, its anatomy and main functions[J]. Soins Gerontol, 2024, 29(165): 10-20. doi:10.1016/j.sger.2023.12.003 |
| [4] | Brezis M, Rosen S, Silva P, et al. Renal ischemia: a new perspective[J]. Kidney Int, 1984, 26(4): 375-83. doi:10.1038/ki.1984.185 |
| [5] | Brezis M, Rosen S. Hypoxia of the renal medulla: its implications for disease[J]. N Engl J Med, 1995, 332(10): 647-55. doi:10.1056/nejm199503093321006 |
| [6] | Hirakawa Y, Tanaka T, Nangaku M. Renal hypoxia in CKD; pathophysiology and detecting methods[J]. Front Physiol, 2017, 8: 99. doi:10.3389/fphys.2017.00099 |
| [7] | Gueutin V, Deray G, Isnard-Bagnis C. Renal physiology [J]. Bull Cancer, 2012, 99(3): 237-49. doi:10.1684/bdc.2011.1482 |
| [8] | Franzin R, Stasi A, Fiorentino M, et al. Renal delivery of pharmacologic agents during machine perfusion to prevent ischaemia-reperfusion injury: from murine model to clinical trials[J]. Front Immunol, 2021, 12: 673562. doi:10.3389/fimmu.2021.673562 |
| [9] | Shu S, Wang Y, Zheng M, et al. Hypoxia and hypoxia-inducible factors in kidney injury and repair[J]. Cells, 2019, 8(3): E207. doi:10.3390/cells8030207 |
| [10] | Cantow K, Evans RG, Grosenick D, et al. Quantitative assessment of renal perfusion and oxygenation by invasive probes: basic concepts[J]. Methods Mol Biol, 2021, 2216: 89-107. doi:10.1007/978-1-0716-0978-1_6 |
| [11] | Cantow K, Ladwig-Wiegard M, Flemming B, et al. Monitoring renal hemodynamics and oxygenation by invasive probes: experimental protocol[J]. Methods Mol Biol, 2021, 2216: 327-47. doi:10.1007/978-1-0716-0978-1_19 |
| [12] | Yeh TH, Tu KC, Wang HY, et al. From acute to chronic: unraveling the pathophysiological mechanisms of the progression from acute kidney injury to acute kidney disease to chronic kidney disease[J]. Int J Mol Sci, 2024, 25(3): 1755. doi:10.3390/ijms25031755 |
| [13] | Niendorf T, Gladytz T, Cantow K, et al. Magnetic resonance imaging of renal oxygenation[J]. Nat Rev Nephrol, 2025, 21(7): 483-502. doi:10.1038/s41581-025-00956-z |
| [14] | Ogawa S, Lee TM, Nayak AS, et al. Oxygenation-sensitive contrast in magnetic resonance image of rodent brain at high magnetic fields[J]. Magn Reson Med, 1990, 14(1): 68-78. doi:10.1002/mrm.1910140108 |
| [15] | Prasad PV, Edelman RR, Epstein FH. Noninvasive evaluation of intrarenal oxygenation with BOLD MRI[J]. Circulation, 1996, 94(12): 3271-5. doi:10.1161/01.cir.94.12.3271 |
| [16] | 杨桂香, 梅颖洁, 吕 健, 等. 血氧水平依赖磁共振成像评估急性马兜铃酸肾病大鼠肾脏氧合水平变化 [J]. 南方医科大学学报, 2019, 39(5): 528. |
| [17] | Pohlmann A, Hentschel J, Fechner M, et al. High temporal resolution parametric MRI monitoring of the initial ischemia/reperfusion phase in experimental acute kidney injury[J]. PLoS One, 2013, 8(2): e57411. doi:10.1371/journal.pone.0057411 |
| [18] | Zhao K, Pohlmann A, Feng Q, et al. Physiological system analysis of the kidney by high-temporal-resolution T2 monitoring of an oxygen-ation step response[J]. Magn Reson Med, 2021, 85(1): 334-45. doi:10.1002/mrm.28399 |
| [19] | Priatna A, Epstein FH, Spokes K, et al. Evaluation of changes in intrarenal oxygenation in rats using multiple gradient-recalled echo (mGRE) sequence[J]. J Magn Reson Imaging, 1999, 9(6): 842-6. doi:10.1002/(sici)1522-2586(199906)9:6<842::aid-jmri12>3.3.co;2-m |
| [20] | Markl M, Leupold J. Gradient echo imaging[J]. Magnetic Resonance Imaging, 2012, 35(6): 1274-89. doi:10.1002/jmri.23638 |
| [21] | Stehling MK, Turner R, Mansfield P. Echo-planar imaging: magnetic resonance imaging in a fraction of a second[J]. Science, 1991, 254(5028): 43-50. doi:10.1126/science.1925560 |
| [22] | Mansfield SP. EPI - in the beginning[J]. J Magn Reson, 2011, 213(2): 532. doi:10.1016/j.jmr.2011.08.017 |
| [23] | Jin N, da Silveira JS, Jolly MP, et al. Free-breathing myocardial T2* mapping using GRE-EPI and automatic non-rigid motion correction[J]. J Cardiovasc Magn Reson, 2015, 17: 113. doi:10.1186/1532-429x-17-s1-w8 |
| [24] | Kundu P, Inati SJ, Evans JW, et al. Differentiating BOLD and non-BOLD signals in fMRI time series using multi-echo EPI[J]. NeuroImage, 2012, 60(3): 1759-70. doi:10.1016/j.neuroimage.2011.12.028 |
| [25] | Wronski T, Seeliger E, Persson PB, et al. The step response: a method to characterize mechanisms of renal blood flow auto-regulation[J]. Am J Physiol Renal Physiol, 2003, 285(4): F758-64. doi:10.1152/ajprenal.00420.2002 |
| [26] | Boss A, Martirosian P, Jehs MC, et al. Influence of oxygen and carbogen breathing on renal oxygenation measured by T2*-weighted imaging at 3.0 T[J]. NMR Biomed, 2009, 22(6): 638-45. doi:10.1002/nbm.1378 |
| [27] | Seeliger E, Wronski T, Ladwig M, et al. The renin-angiotensin system and the third mechanism of renal blood flow autoregulation[J]. Am J Physiol Renal Physiol, 2009, 296(6): F1334-45. doi:10.1152/ajprenal.90476.2008 |
| [28] | Edwards A, Kurtcuoglu V. Renal blood flow and oxygenation[J]. Pflügers Arch Eur J Physiol, 2022, 474(8): 759-70. doi:10.1007/s00424-022-02690-y |
| [29] | Gloviczki ML, Glockner J, Gomez SI, et al. Comparison of 1.5 and 3 T BOLD MR to study oxygenation of kidney cortex and medulla in human renovascular disease[J]. Invest Radiol, 2009, 44(9): 566-71. doi:10.1097/rli.0b013e3181b4c1e8 |
| [30] | Pohlmann A, Arakelyan K, Hentschel J, et al. Detailing the relation between renal T2* and renal tissue PO2 using an integrated approach of parametric magnetic resonance imaging and invasive physiological measurements[J]. Invest Radiol, 2014, 49(8): 547-60. doi:10.1097/rli.0000000000000054 |
| [31] | Ganesh T, Estrada M, Duffin J, et al. T2* and T1 assessment of abdominal tissue response to graded hypoxia and hypercapnia using a controlled gas mixing circuit for small animals[J]. J Magn Reson Imaging, 2016, 44(2): 305-16. doi:10.1002/jmri.25169 |
| [32] | Gardiner BS, Smith DW, O' Connor PM, et al. A mathematical model of diffusional shunting of oxygen from arteries to veins in the kidney[J]. Am J Physiol Renal Physiol, 2011, 300(6): F1339-52. doi:10.1152/ajprenal.00544.2010 |
| [33] | Donati OF, Nanz D, Serra AL, et al. Quantitative BOLD response of the renal medulla to hyperoxic challenge at 1.5 T and 3.0 T[J]. NMR Biomed, 2012, 25(10): 1133-8. doi:10.1002/nbm.2781 |
| [34] | Evans RG, Smith DW, Lee CJ, et al. What makes the kidney susceptible to hypoxia[J]? Anat Rec: Hoboken, 2020, 303(10): 2544-52. doi:10.1002/ar.24260 |
| [35] | Wang R, Lin Z, Yang X, et al. Noninvasive evaluation of renal hypoxia by multiparametric functional MRI in early diabetic kidney disease[J]. J Magn Reson Imaging, 2022, 55(2): 518-27. doi:10.1002/jmri.27814 |
| [36] | Li ZL, Liu BC. Hypoxia and renal tubulointerstitial fibrosis[J]. Adv Exp Med Biol, 2019, 1165: 467-85. doi:10.1007/978-981-13-8871-2_23 |
| [37] | Crislip GR, Patel B, Mohamed R, et al. Ultrasound measurement of change in kidney volume is a sensitive indicator of severity of renal parenchymal injury[J]. Am J Physiol Renal Physiol, 2020, 319(3): F447-57. doi:10.1152/ajprenal.00221.2020 |
| [38] | Jufar AH, Lankadeva YR, May CN, et al. Renal and cerebral hypoxia and inflammation during cardiopulmonary bypass[J]. Compr Physiol, 2021, 12(1): 2799-834. doi:10.1002/j.2040-4603.2022.tb00202.x |
| [39] | Arnoux G, Serre J, Verissimo T, et al. The preferential injury of outer renal medulla after ischemia-reperfusion relies on high oxidative metabolism [J]. bioRxiv, 2024: 2024.09. 12.612245. |
| [40] | Sgouralis I, Evans RG, Layton AT. Renal medullary and urinary oxygen tension during cardiopulmonary bypass in the rat[J]. Math Med Biol, 2017, 34(3): 313-33. |
| [41] | 游 勇, 陈 丽. 呼吸衰竭的相关研究 [J]. 临床医学进展, 2025, 15(4): 2024-30. |
| [42] | Kim N, Voicu L, Hare GM, et al. Response of the renal inner medulla to hypoxia: possible defense mechanisms[J]. Nephron Physiol, 2012, 121(1/2): 1-7. doi:10.1159/000345516 |
| [43] | Lee CJ, Gardiner BS, Evans RG, et al. Analysis of the critical determinants of renal medullary oxygenation[J]. Am J Physiol Renal Physiol, 2019, 317(6): F1483-502. doi:10.1152/ajprenal.00315.2019 |
| [44] | Selby NM, Francis ST. Assessment of acute kidney injury using MRI[J]. J Magn Reson Imaging, 2025, 61(1): 25-41. doi:10.1002/jmri.29281 |
| [45] | 叶常红, 杨燕玲. 七氟烷与异氟烷吸入麻醉对肝肾功能影响的比较 [J]. 中国基层医药, 2012, 19(10): 1560-1. |
| [46] | Evans RG, Goddard D, Eppel GA, et al. Factors that render the kidney susceptible to tissue hypoxia in hypoxemia[J]. Am J Physiol Regul Integr Comp Physiol, 2011, 300(4): R931-40. doi:10.1152/ajpregu.00552.2010 |
| [1] | 呼琴, 金华. 清肾颗粒通过调控miR-23b及Nrf2通路改善慢性肾脏病湿热证患者的肾功能:基于网络药理学和临床试验[J]. 南方医科大学学报, 2025, 45(9): 1867-1879. |
| [2] | 刘炎忠, 朱润, 李玉柱, 马鑫, 麦海星. 术中肾脏集合系统受损是肾部分切除术后同侧上尿路结石发病的危险因素:一项1∶2匹配病例对照研究[J]. 南方医科大学学报, 2025, 45(9): 1880-1888. |
| [3] | 马倩倩, 牛钰琪, 左铭钰, 李鑫, 符竣轲, 王瑾瑾. 鬼箭羽通过抑制AGEs-RAGE信号转导通路改善晚期糖基化终末产物诱导的小鼠肾足细胞损伤[J]. 南方医科大学学报, 2025, 45(9): 1938-1945. |
| [4] | 马思雨, 陈美庆, 吴天宇, 赵文红. 膳食亚麻木酚素通过调控Bcl2/Bax/caspase3信号轴通道改善大鼠母体反式脂肪酸暴露所导致的子代肾损伤[J]. 南方医科大学学报, 2025, 45(12): 2658-2666. |
| [5] | 刘本菊, 王业磊, 任海文, 欧丽雯, 邓轩, 黄梦欣, 吴鑫, 龚权. 3-甲基腺嘌呤通过抑制AKT信号减轻糖尿病小鼠的早期肾损伤[J]. 南方医科大学学报, 2024, 44(7): 1236-1242. |
| [6] | 周凤敏, 郭艳菊, 陈 宁. 运动诱导的Irisin表达改善2型糖尿病大鼠的肾脏损伤[J]. 南方医科大学学报, 2024, 44(4): 675-681. |
| [7] | 罗冠峰, 刘华熙, 谢 钡, 邓伊健, 谢鹏辉, 赵晓山, 孙晓敏. 肾病III号方治疗慢性肾脏病大鼠肾脏纤维化的作用机制:基于网络药理学和分子对接技术[J]. 南方医科大学学报, 2023, 43(6): 924-934. |
| [8] | 郝雨薇, 高 升, 张潇月, 崔梦秋, 丁效蕙, 王 鹤, 杨大为, 叶慧义, 王海屹. 透明细胞癌可能性评分v1.0和v2.0的应用价值对比[J]. 南方医科大学学报, 2023, 43(5): 800-806. |
| [9] | 邓钰莹, 陈华锋, 李功辉, 陈立桁, 傅 强. 慢性肾脏病对肌钙蛋白诊断急性心肌梗死准确性的影响[J]. 南方医科大学学报, 2023, 43(2): 300-307. |
| [10] | 万 璐, 钱宇池, 倪文静, 卢宇欣, 李 巍, 潘 艳, 陈卫东. 利格列汀通过激活AMPK/PGC-1α/TFAM通路改善糖尿病肾脏疾病线粒体生物合成[J]. 南方医科大学学报, 2023, 43(12): 2053-2060. |
| [11] | 魏 敏, 陈乃洁, 李璟怡, 刘 丹, 沈双宏, 王 丰, 吴润华, 陈 沁. 慢性间歇性低氧大鼠肾组织差异蛋白的定量分析:基于TMT-PRM技术[J]. 南方医科大学学报, 2023, 43(11): 1857-1864. |
| [12] | 邢 磊, 邢文文, 郭宏敏. 龙杞方治疗糖尿病肾脏病的作用机制:基于网络药理学和大鼠验证实验[J]. 南方医科大学学报, 2022, 42(2): 171-180. |
| [13] | 梁小芳, 杨 越, 徐帅帅, 刘 映, 褚晗玉, 唐 艳, 杨 飞. 微囊藻毒素-LR长期低剂量暴露诱导小鼠肾脏结构和功能损伤:基于激活PI3K/AKT信号通路[J]. 南方医科大学学报, 2022, 42(10): 1486-1494. |
| [14] | 许晓双, 汤旭磊, 车红霞, 关聪会, 赵 楠, 傅松波, 刘丽娟, 叶 月, 郭梦然, 闵 行, 甄东户. 高甘油三酯-葡萄糖乘积指数是慢性肾脏病发生的独立危险因素:基于3439例40~75岁人群的前瞻性队列研究[J]. 南方医科大学学报, 2021, 41(11): 1600-1608. |
| [15] | 陆 静, 白志勋, 匡晓燕, 李 玲. 高盐刺激可诱导巨噬细胞极化从而促进肾脏成纤维细胞的增及表型转化[J]. 南方医科大学学报, 2020, 40(10): 1472-1479. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||