Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (12): 2616-2627.doi: 10.12122/j.issn.1673-4254.2025.12.09
Mengyao YUAN1,2( ), Xianghan RUAN1,2, Yang LI1, Ting ZHANG1, Chunxiang HAO1, Hao LI1, Jingsheng LOU1, Jiangbei CAO1, Yanhong LIU1, Weidong MI1(
), Xianghan RUAN1,2, Yang LI1, Ting ZHANG1, Chunxiang HAO1, Hao LI1, Jingsheng LOU1, Jiangbei CAO1, Yanhong LIU1, Weidong MI1( ), Xiaoying ZHANG1(
), Xiaoying ZHANG1( )
)
Received:2025-07-15
Online:2025-12-20
Published:2025-12-22
Contact:
Weidong MI, Xiaoying ZHANG
E-mail:yuanmengyaoup@126.com;wwdd1962@163.com;zxystudy@163.com
Mengyao YUAN, Xianghan RUAN, Yang LI, Ting ZHANG, Chunxiang HAO, Hao LI, Jingsheng LOU, Jiangbei CAO, Yanhong LIU, Weidong MI, Xiaoying ZHANG. Preoperative serum magnesium as a biomarker for predicting delirium following non-cardiac surgery in elderly patients: a retrospective cohort study[J]. Journal of Southern Medical University, 2025, 45(12): 2616-2627.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.12.09
| Characteristics | Overall | Preoperative serum magnesium levels (mmol/L) | P | ||||
|---|---|---|---|---|---|---|---|
Quintile 1 (0.36-0.82) | Quintile 2 (0.82-0.87) | Quintile 3 (0.87-0.90) | Quintile 4 (0.90-0.94) | Quintile 5 (0.94-1.44) | |||
| Case (n) | 12 876 | 2322 | 2781 | 2278 | 2641 | 2854 | |
| sMg (mmol/L, Mean±SD) | 0.88±0.08 | 0.76±0.05 | 0.84±0.01 | 0.88±0.01 | 0.91±0.01 | 0.98±0.04 | <0.001 |
| Demographics | |||||||
| Age (year, median [IQR]) | 70 (67, 75) | 71 (67, 77) | 70 (67, 75) | 71 (67, 75) | 70 (67, 75) | 70 (67, 75) | <0.001 |
| Male | 6110 (47.5%) | 1125 (48.4%) | 1296 (46.6%) | 1092 (47.9%) | 1268 (48.0%) | 1329 (46.6%) | 0.529 |
| BMI (kg/m2, Mean±SD) | 24.6±3.9 | 24.2±4.1 | 24.8±4.0 | 24.8±3.9 | 24.7±3.8 | 24.5±3.8 | <0.001 |
| Comorbidities | |||||||
| Diabetes mellitus | 3373 (26.2%) | 855 (36.8%) | 786 (28.3%) | 553 (24.3%) | 584 (22.1%) | 595 (20.8%) | <0.001 |
| Cancer | 5158 (40.1%) | 901 (38.8%) | 1006 (36.2%) | 904 (39.7%) | 1101 (41.7%) | 1246 (43.7%) | <0.001 |
| Renal insufficiency | 309 (2.4%) | 69 (3.0%) | 64 (2.3%) | 41 (1.8%) | 50 (1.9%) | 85 (3.0%) | 0.008 |
| Liver cirrhosis | 389 (3.0%) | 80 (3.4%) | 93 (3.3%) | 61 (2.7%) | 73 (2.8%) | 82 (2.9%) | 0.387 |
| Laboratory measurements | |||||||
| CRP [mg/L (median, IQR)] | 0.43 (0.10, 1.59) | 0.77 (0.19, 3.00) | 0.42 (0.10, 1.59) | 0.37 (0.10, 1.24) | 0.37 (0.10, 1.18) | 0.42 (0.11, 1.40) | <0.001 |
| SCr (μmol/L, Mean±SD) | 75.35±42.48 | 73.41±35.74 | 72.05±27.39 | 73.89±32.44 | 74.35±33.44 | 82.33±66.83 | <0.001 |
| TBil (μmol/L, Mean±SD) | 20.77±41.85 | 24.88±48.79 | 20.81±43.62 | 18.81±35.98 | 19.17±36.62 | 20.45±42.65 | <0.001 |
| ALT (U/L, Mean±SD) | 25.99±50.93 | 31.59±93.86 | 25.15±45.43 | 24.49±32.40 | 24.49±27.41 | 24.82±31.02 | <0.001 |
| Albumin (g/L, Mean±SD) | 38.32±4.43 | 36.31±4.85 | 38.02±4.28 | 38.67±4.00 | 38.98±4.09 | 39.37±4.29 | <0.001 |
| sCa (mmol/L, Mean±SD) | 2.24±0.13 | 2.21±0.17 | 2.23±0.13 | 2.24±0.12 | 2.25±0.12 | 2.25±0.12 | <0.001 |
| Surgery-related factors | |||||||
| Emergency surgery | 1298 (5.9%) | 447 (11.2%) | 252 (5.2%) | 164 (4.3%) | 187 (4.1%) | 248 (5.1%) | <0.001 |
| Surgery specialty | <0.001 | ||||||
Otorhinolaryngology-head &neck, plastic,or abdominal wallsurgery | 1104 (8.6%) | 129 (5.6%) | 223 (8.0%) | 196 (8.6%) | 264 (10.0%) | 292 (10.2%) | |
| Obstetrics/gynecology | 80 (0.6%) | 21 (0.9%) | 21 (0.8%) | 11 (0.5%) | 12 (0.5%) | 15 (0.5%) | |
| Urology | 260 (2.0%) | 38 (1.6%) | 57 (2.0%) | 49 (2.2%) | 46 (1.7%) | 70 (2.5%) | |
| Hepatobiliary/pancreatic/ gastrointestinal | 4081 (31.7%) | 798 (34.4%) | 761 (27.4%) | 664 (29.1%) | 864 (32.7%) | 994 (34.8%) | |
| Vascular | 431 (3.3%) | 73 (3.1%) | 97 (3.5%) | 77 (3.4%) | 87 (3.3%) | 97 (3.4%) | |
| Orthopedic | 5940 (46.1%) | 1030 (44.4%) | 1417 (51.0%) | 1093 (48.0%) | 1193 (45.2%) | 1207 (42.3%) | |
| Endoscopic | 739 (5.7%) | 196 (8.4%) | 153 (5.5%) | 139 (6.1%) | 123 (4.7%) | 128 (4.5%) | |
| Thoracic | 241 (1.9%) | 37 (1.6%) | 52 (1.9%) | 49 (2.2%) | 52 (2.0%) | 51 (1.8%) | |
| Surgery duration (h, median [IQR]) | 2.08 (1.42, 3.17) | 2.04 (1.42, 3.08) | 2.05 (1.42, 3.08) | 2.08 (1.42, 3.17) | 2.08 (1.42, 3.25) | 2.17 (1.45, 3.25) | 0.445 |
| Outcome | |||||||
| POD | 685 (5.3%) | 218 (9.4%) | 146 (5.2%) | 111 (4.9%) | 99 (3.7%) | 111 (3.9%) | <0.001 |
Tab.1 Baseline characteristics of the patients stratified by preoperative serum magnesium level quintiles
| Characteristics | Overall | Preoperative serum magnesium levels (mmol/L) | P | ||||
|---|---|---|---|---|---|---|---|
Quintile 1 (0.36-0.82) | Quintile 2 (0.82-0.87) | Quintile 3 (0.87-0.90) | Quintile 4 (0.90-0.94) | Quintile 5 (0.94-1.44) | |||
| Case (n) | 12 876 | 2322 | 2781 | 2278 | 2641 | 2854 | |
| sMg (mmol/L, Mean±SD) | 0.88±0.08 | 0.76±0.05 | 0.84±0.01 | 0.88±0.01 | 0.91±0.01 | 0.98±0.04 | <0.001 |
| Demographics | |||||||
| Age (year, median [IQR]) | 70 (67, 75) | 71 (67, 77) | 70 (67, 75) | 71 (67, 75) | 70 (67, 75) | 70 (67, 75) | <0.001 |
| Male | 6110 (47.5%) | 1125 (48.4%) | 1296 (46.6%) | 1092 (47.9%) | 1268 (48.0%) | 1329 (46.6%) | 0.529 |
| BMI (kg/m2, Mean±SD) | 24.6±3.9 | 24.2±4.1 | 24.8±4.0 | 24.8±3.9 | 24.7±3.8 | 24.5±3.8 | <0.001 |
| Comorbidities | |||||||
| Diabetes mellitus | 3373 (26.2%) | 855 (36.8%) | 786 (28.3%) | 553 (24.3%) | 584 (22.1%) | 595 (20.8%) | <0.001 |
| Cancer | 5158 (40.1%) | 901 (38.8%) | 1006 (36.2%) | 904 (39.7%) | 1101 (41.7%) | 1246 (43.7%) | <0.001 |
| Renal insufficiency | 309 (2.4%) | 69 (3.0%) | 64 (2.3%) | 41 (1.8%) | 50 (1.9%) | 85 (3.0%) | 0.008 |
| Liver cirrhosis | 389 (3.0%) | 80 (3.4%) | 93 (3.3%) | 61 (2.7%) | 73 (2.8%) | 82 (2.9%) | 0.387 |
| Laboratory measurements | |||||||
| CRP [mg/L (median, IQR)] | 0.43 (0.10, 1.59) | 0.77 (0.19, 3.00) | 0.42 (0.10, 1.59) | 0.37 (0.10, 1.24) | 0.37 (0.10, 1.18) | 0.42 (0.11, 1.40) | <0.001 |
| SCr (μmol/L, Mean±SD) | 75.35±42.48 | 73.41±35.74 | 72.05±27.39 | 73.89±32.44 | 74.35±33.44 | 82.33±66.83 | <0.001 |
| TBil (μmol/L, Mean±SD) | 20.77±41.85 | 24.88±48.79 | 20.81±43.62 | 18.81±35.98 | 19.17±36.62 | 20.45±42.65 | <0.001 |
| ALT (U/L, Mean±SD) | 25.99±50.93 | 31.59±93.86 | 25.15±45.43 | 24.49±32.40 | 24.49±27.41 | 24.82±31.02 | <0.001 |
| Albumin (g/L, Mean±SD) | 38.32±4.43 | 36.31±4.85 | 38.02±4.28 | 38.67±4.00 | 38.98±4.09 | 39.37±4.29 | <0.001 |
| sCa (mmol/L, Mean±SD) | 2.24±0.13 | 2.21±0.17 | 2.23±0.13 | 2.24±0.12 | 2.25±0.12 | 2.25±0.12 | <0.001 |
| Surgery-related factors | |||||||
| Emergency surgery | 1298 (5.9%) | 447 (11.2%) | 252 (5.2%) | 164 (4.3%) | 187 (4.1%) | 248 (5.1%) | <0.001 |
| Surgery specialty | <0.001 | ||||||
Otorhinolaryngology-head &neck, plastic,or abdominal wallsurgery | 1104 (8.6%) | 129 (5.6%) | 223 (8.0%) | 196 (8.6%) | 264 (10.0%) | 292 (10.2%) | |
| Obstetrics/gynecology | 80 (0.6%) | 21 (0.9%) | 21 (0.8%) | 11 (0.5%) | 12 (0.5%) | 15 (0.5%) | |
| Urology | 260 (2.0%) | 38 (1.6%) | 57 (2.0%) | 49 (2.2%) | 46 (1.7%) | 70 (2.5%) | |
| Hepatobiliary/pancreatic/ gastrointestinal | 4081 (31.7%) | 798 (34.4%) | 761 (27.4%) | 664 (29.1%) | 864 (32.7%) | 994 (34.8%) | |
| Vascular | 431 (3.3%) | 73 (3.1%) | 97 (3.5%) | 77 (3.4%) | 87 (3.3%) | 97 (3.4%) | |
| Orthopedic | 5940 (46.1%) | 1030 (44.4%) | 1417 (51.0%) | 1093 (48.0%) | 1193 (45.2%) | 1207 (42.3%) | |
| Endoscopic | 739 (5.7%) | 196 (8.4%) | 153 (5.5%) | 139 (6.1%) | 123 (4.7%) | 128 (4.5%) | |
| Thoracic | 241 (1.9%) | 37 (1.6%) | 52 (1.9%) | 49 (2.2%) | 52 (2.0%) | 51 (1.8%) | |
| Surgery duration (h, median [IQR]) | 2.08 (1.42, 3.17) | 2.04 (1.42, 3.08) | 2.05 (1.42, 3.08) | 2.08 (1.42, 3.17) | 2.08 (1.42, 3.25) | 2.17 (1.45, 3.25) | 0.445 |
| Outcome | |||||||
| POD | 685 (5.3%) | 218 (9.4%) | 146 (5.2%) | 111 (4.9%) | 99 (3.7%) | 111 (3.9%) | <0.001 |
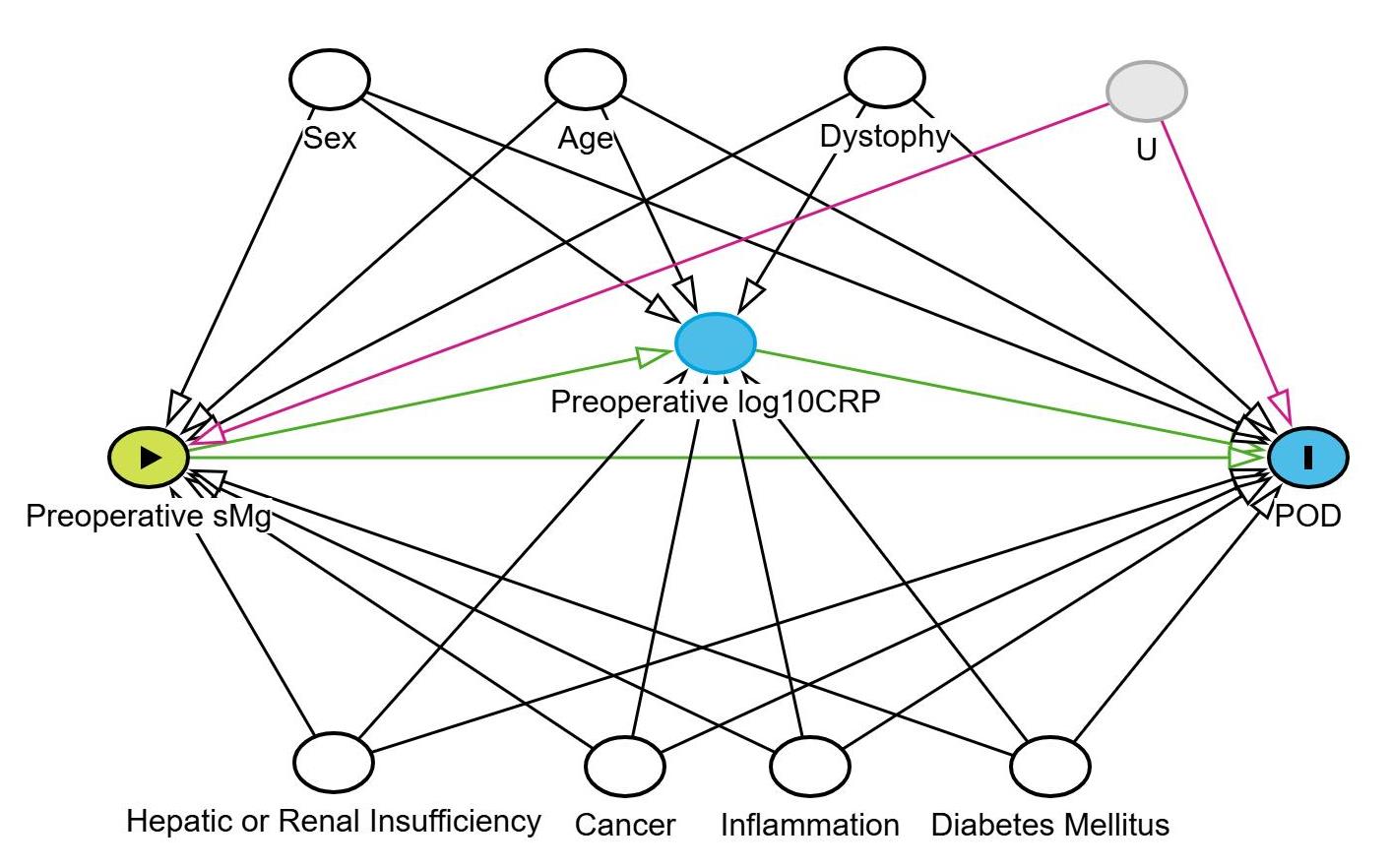
Fig.2 Directed acyclic graph showing associations among the covariates, primary exposure, and the outcome. White circles denote ancestors of both the exposure and outcome that have been controlled as confounders, blue circles represent the outcome and its causal direct determinants, green circle symbolizes the exposure variable, and the gray circle denotes variables that are unobserved. The causal relationships are depicted by green lines, and gray lines illustrate the paths of bias that have been accounted for. Conversely, pink lines highlight the biasing paths that remain unadjusted due to latent variables. OR: Odds ratio; CI: Confidence interval; U: Unmeasured confounders.
| Variables | Events [n (%)] | Model 1a | Model 2b | Model 3c | |||
|---|---|---|---|---|---|---|---|
| (P trend=0.004) | (P trend=0.054) | (P trend=0.036) | |||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | ||
| Continuous | |||||||
| Standardized sMg | 685 (5.3%) | 0.71 (0.66, 0.76) | <0.001 | 0.83 (0.77, 0.89) | <0.001 | 0.84 (0.78, 0.90) | <0.001 |
| Categoricale | |||||||
| Quintile 1 | 218 (9.4%) | 2.66 (2.09, 3.41) | <0.001 | 1.81 (1.41, 2.35) | <0.001 | 1.77 (1.37, 2.29) | <0.001 |
| Quintile 2 | 146 (5.2%) | 1.42 (1.10, 1.85) | 0.008 | 1.26 (0.97, 1.65) | 0.091 | 1.25 (0.96, 1.64) | 0.097 |
| Quintile 3 | 111 (4.9%) | 1.32 (1.00, 1.74) | 0.052 | 1.27 (0.96, 1.68) | 0.096 | 1.27 (0.96, 1.69) | 0.096 |
| Quintile 4 | 99 (3.7%) | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Quintile 5 | 111 (3.9%) | 1.04 (0.79, 1.37) | 0.786 | 1.06 (0.80, 1.40) | 0.708 | 1.01 (0.76, 1.34) | 0.941 |
Tab.2 Association between preoperative sMg levels and POD risk in univariate and multivariable logistic regression models
| Variables | Events [n (%)] | Model 1a | Model 2b | Model 3c | |||
|---|---|---|---|---|---|---|---|
| (P trend=0.004) | (P trend=0.054) | (P trend=0.036) | |||||
| OR (95% CI) | P | OR (95% CI) | P | OR (95% CI) | P | ||
| Continuous | |||||||
| Standardized sMg | 685 (5.3%) | 0.71 (0.66, 0.76) | <0.001 | 0.83 (0.77, 0.89) | <0.001 | 0.84 (0.78, 0.90) | <0.001 |
| Categoricale | |||||||
| Quintile 1 | 218 (9.4%) | 2.66 (2.09, 3.41) | <0.001 | 1.81 (1.41, 2.35) | <0.001 | 1.77 (1.37, 2.29) | <0.001 |
| Quintile 2 | 146 (5.2%) | 1.42 (1.10, 1.85) | 0.008 | 1.26 (0.97, 1.65) | 0.091 | 1.25 (0.96, 1.64) | 0.097 |
| Quintile 3 | 111 (4.9%) | 1.32 (1.00, 1.74) | 0.052 | 1.27 (0.96, 1.68) | 0.096 | 1.27 (0.96, 1.69) | 0.096 |
| Quintile 4 | 99 (3.7%) | 1 (reference) | 1 (reference) | 1 (reference) | |||
| Quintile 5 | 111 (3.9%) | 1.04 (0.79, 1.37) | 0.786 | 1.06 (0.80, 1.40) | 0.708 | 1.01 (0.76, 1.34) | 0.941 |
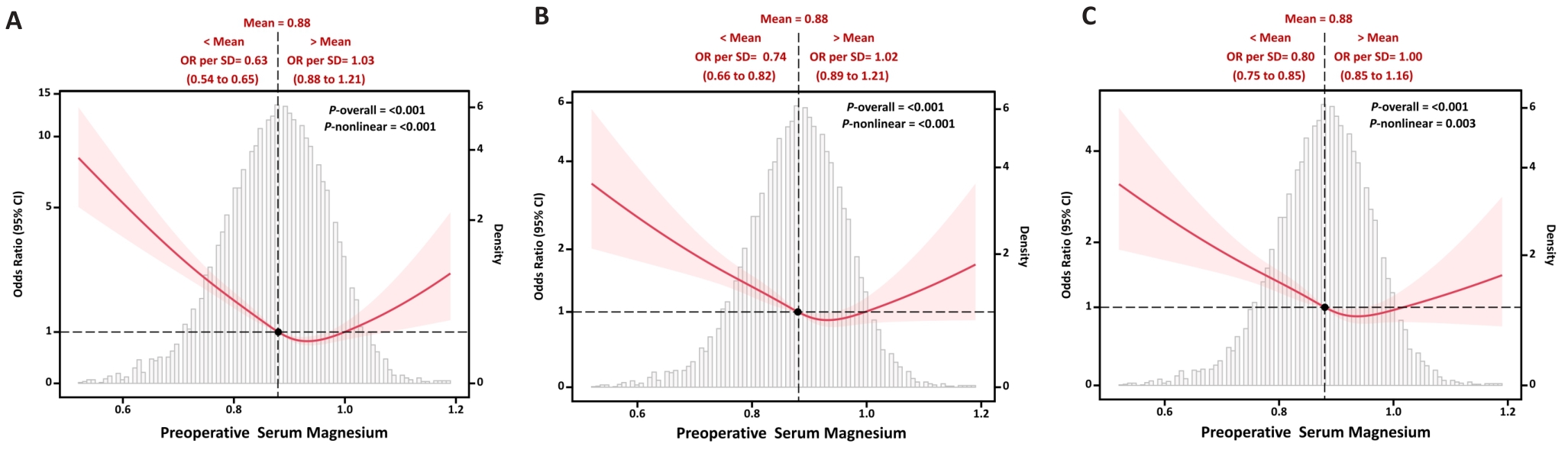
Fig.3 Association between preoperative sMg levels and POD risk on continuous scales. A: Model 1 (unadjusted model). B: Model 2 (multivariable model adjusted for age, sex, BMI, albumin, TBil, ALT, diabetes mellitus, cancer and renal insufficiency). C: Model 3 (multivariable model additionally adjusted for CRP levels as a potential mediator). ORs are indicated by blue solid lines and 95% CIs by light blue dotted lines. Reference lines for no association are indicated by the blackdotted lines at an OR of 1.0. Density plots are presented by gray shadow area to show the fraction of the population with different levels of sMg. sMg level corresponding to the OR equal to 1 (reference value) is shown by dark spot.
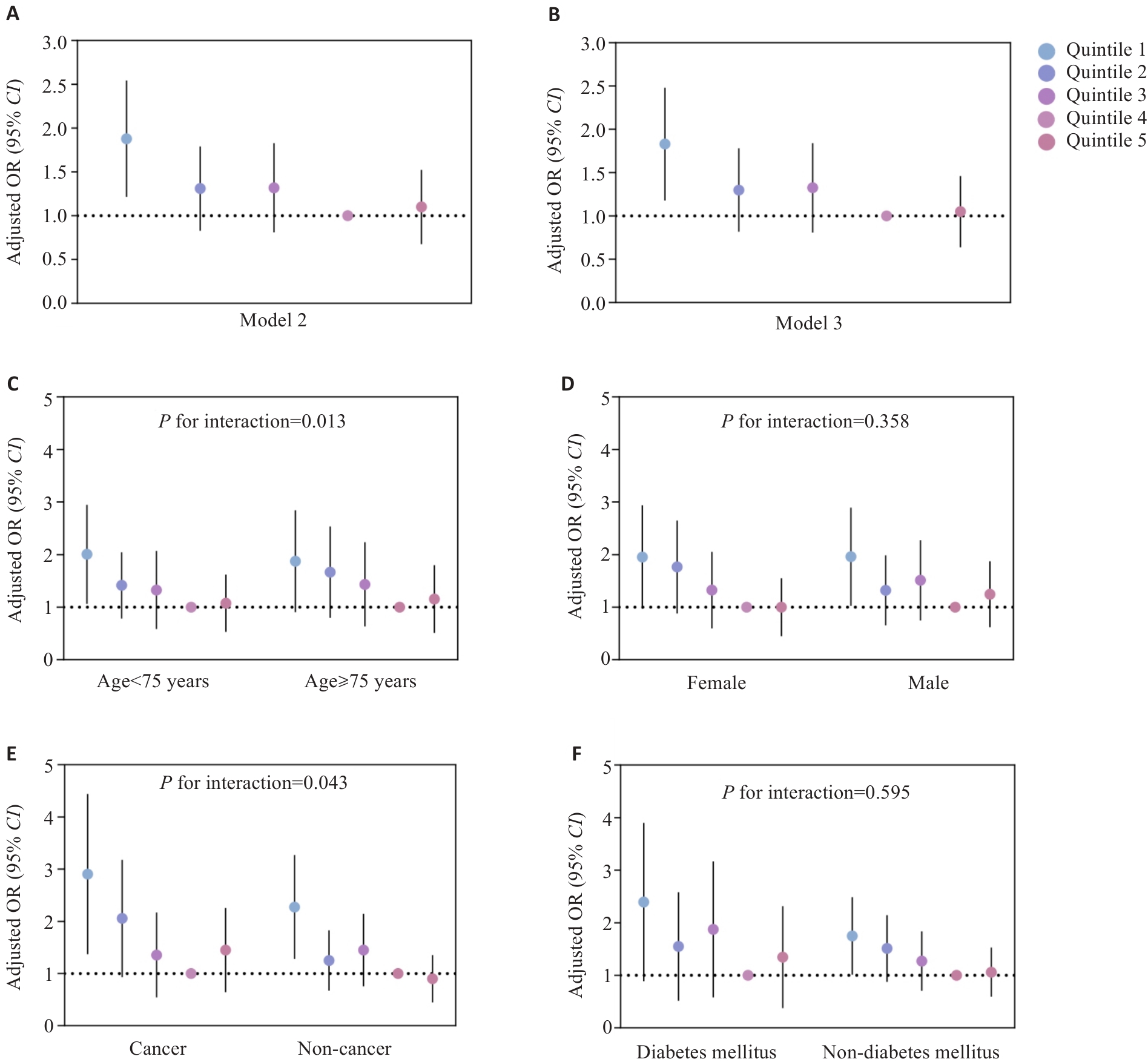
Fig.4 Association between preoperative sMg levels and POD risk based on quintile analyses. Forest plots show associations in the overall population (A, B) and subgroups (C-F). Subgroup analyses were adjusted as in model 2.
| Subgroup | OR (95% CI) of serum magnesium quintiles | P for trend | P for interaction | ||||
|---|---|---|---|---|---|---|---|
| Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | |||
| Age (year) | 0.013 | ||||||
| <75 (n=9169) | 1.88 (1.34, 2.67) | 1.30 (0.91, 1.86) | 1.27 (0.87, 1.85) | 1 (reference) | 1.01 (0.69, 1.46) | 0.018 | |
| ≥75 (n=3707) | 1.73 (1.19, 2.56) | 1.54 (1.05, 2.28) | 1.32 (0.87, 2.00) | 1 (reference) | 1.06 (0.70, 1.61) | 0.138 | |
| Gender | 0.358 | ||||||
| Male (n=6110) | 1.84 (1.30, 2.62) | 1.23 (0.85, 1.79) | 1.40 (0.97, 2.05) | 1 (reference) | 1.16 (0.80, 1.69) | 0.150 | |
| Female (n=6766) | 1.81 (1.26, 2.65) | 1.64 (1.14, 2.39) | 1.22 (0.81, 1.84) | 1 (reference) | 0.92 (0.61, 1.39) | 0.011 | |
| Diabetes mellitus | 0.595 | ||||||
| No (n=9503) | 1.67 (1.23, 2.27) | 1.44 (1.06, 1.96) | 1.20 (0.87, 1.67) | 1 (reference) | 1.01 (0.73, 1.39) | 0.023 | |
| Yes (n=3373) | 2.15 (1.33, 3.46) | 1.35 (0.82, 2.28) | 1.62 (0.96, 2.79) | 1 (reference) | 1.15 (0.66, 2.03) | 0.166 | |
| Cancer | 0.043 | ||||||
| No (n=7718) | 2.15 (1.57, 2.98) | 1.18 (0.84, 1.66) | 1.36 (0.96, 1.94) | 1 (reference) | 0.84 (0.58, 1.22) | 0.025 | |
| Yes (n=5158) | 2.67 (1.82, 3.99) | 1.88 (1.26, 2.85) | 1.23 (0.78, 1.93) | 1 (reference) | 1.33 (0.88, 2.02) | 0.076 | |
Tab.3 Associations between preoperative sMg levels and POD risk based on quintile analysis
| Subgroup | OR (95% CI) of serum magnesium quintiles | P for trend | P for interaction | ||||
|---|---|---|---|---|---|---|---|
| Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | |||
| Age (year) | 0.013 | ||||||
| <75 (n=9169) | 1.88 (1.34, 2.67) | 1.30 (0.91, 1.86) | 1.27 (0.87, 1.85) | 1 (reference) | 1.01 (0.69, 1.46) | 0.018 | |
| ≥75 (n=3707) | 1.73 (1.19, 2.56) | 1.54 (1.05, 2.28) | 1.32 (0.87, 2.00) | 1 (reference) | 1.06 (0.70, 1.61) | 0.138 | |
| Gender | 0.358 | ||||||
| Male (n=6110) | 1.84 (1.30, 2.62) | 1.23 (0.85, 1.79) | 1.40 (0.97, 2.05) | 1 (reference) | 1.16 (0.80, 1.69) | 0.150 | |
| Female (n=6766) | 1.81 (1.26, 2.65) | 1.64 (1.14, 2.39) | 1.22 (0.81, 1.84) | 1 (reference) | 0.92 (0.61, 1.39) | 0.011 | |
| Diabetes mellitus | 0.595 | ||||||
| No (n=9503) | 1.67 (1.23, 2.27) | 1.44 (1.06, 1.96) | 1.20 (0.87, 1.67) | 1 (reference) | 1.01 (0.73, 1.39) | 0.023 | |
| Yes (n=3373) | 2.15 (1.33, 3.46) | 1.35 (0.82, 2.28) | 1.62 (0.96, 2.79) | 1 (reference) | 1.15 (0.66, 2.03) | 0.166 | |
| Cancer | 0.043 | ||||||
| No (n=7718) | 2.15 (1.57, 2.98) | 1.18 (0.84, 1.66) | 1.36 (0.96, 1.94) | 1 (reference) | 0.84 (0.58, 1.22) | 0.025 | |
| Yes (n=5158) | 2.67 (1.82, 3.99) | 1.88 (1.26, 2.85) | 1.23 (0.78, 1.93) | 1 (reference) | 1.33 (0.88, 2.02) | 0.076 | |
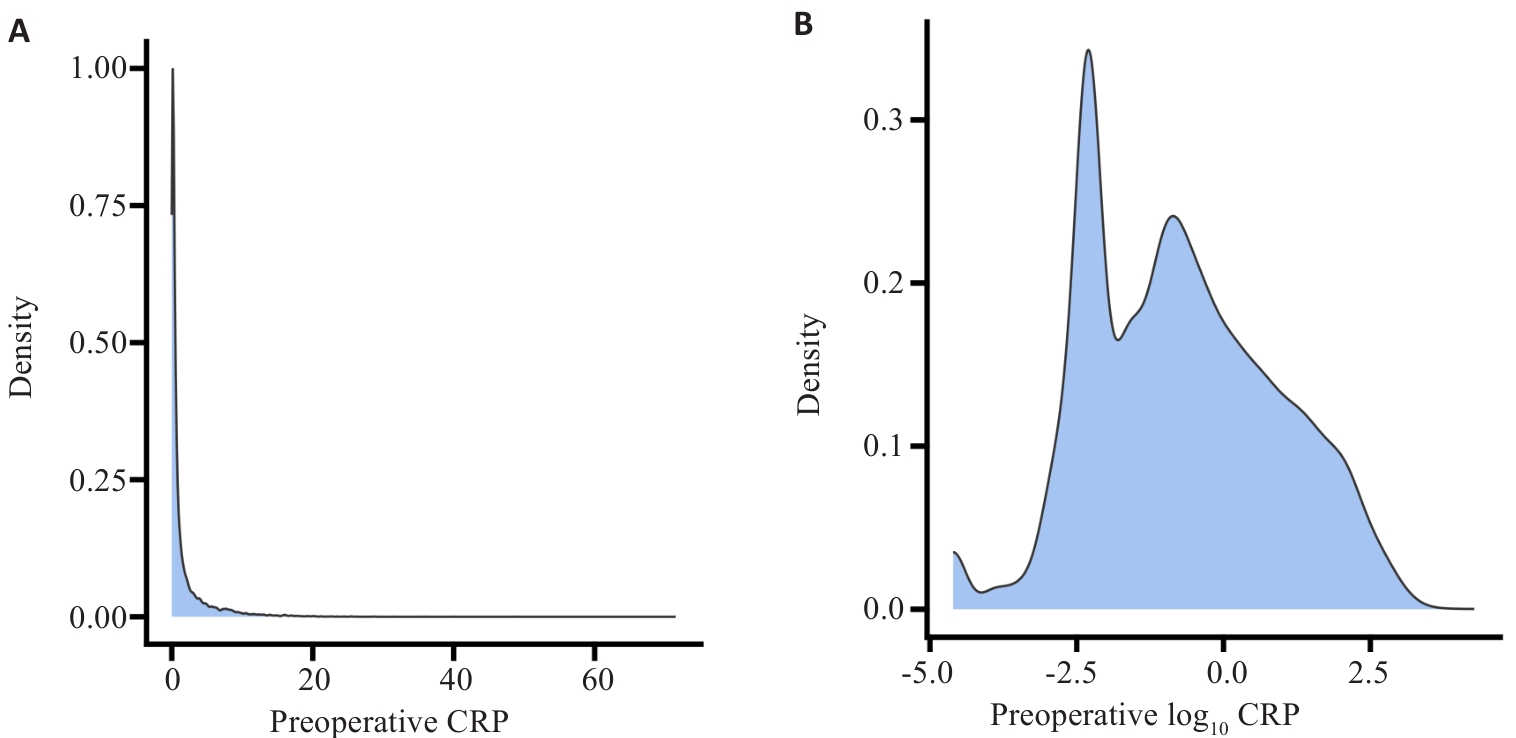
Fig.5 Distribution of CRP levels before and after logarithmic transformation. A: Histogram of the distribution of preoperative CRP levels. B: Histogram of the distribution of preoperative log10 CRP levels.
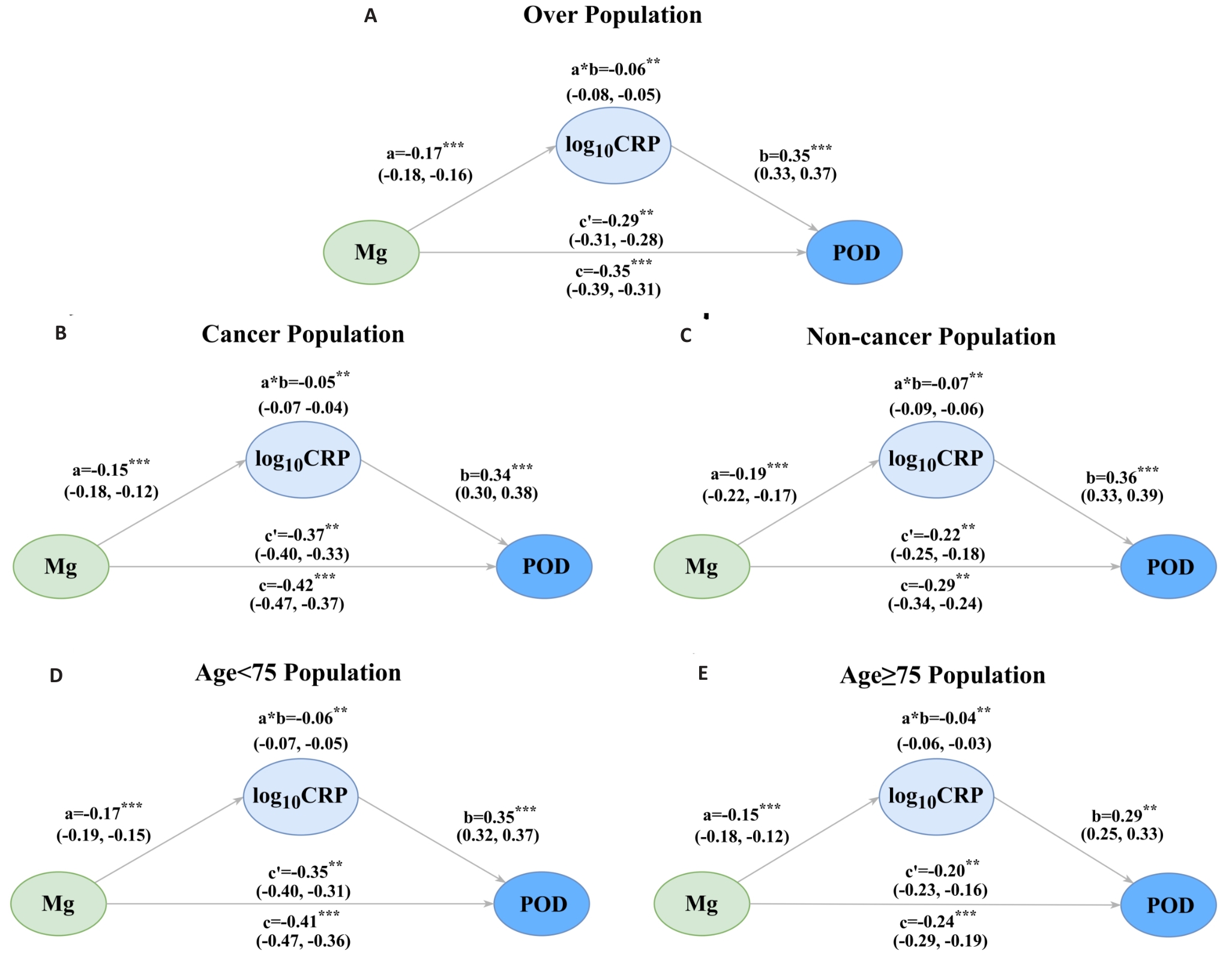
Fig.6 Mediation analyses of the associations between preoperative serum magnesium levels and POD risk through log10CRP levels. Mediation analyses were conducted in the overall population (A) and in key subgroups, including cancer (B), non-cancer (C), age <75 years (D), and age ≥75 years (E) Mediation groups. Subgroup analyses were adjusted as in model 2. a=the effects of sMg on log10 CRP; b=the effects of log10 CRP on POD Risk. a*b: the indirect effect; c: the total effect; c': the direct effect. **P<0.01,***P<0.001.
Pathways sMg→log10 CRP→POD | c | P | c' | P | a*b | P | a | P | b | P | |ab/c| |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | -0.35 | <0.001 | -0.29 | <0.001 | -0.06 | 0.007 | -0.17 | <0.001 | 0.35 | <0.001 | 17.14% |
| Age (year) | |||||||||||
| <75 | -0.41 | <0.001 | -0.35 | 0.006 | -0.06 | <0.001 | -0.17 | <0.001 | 0.35 | <0.001 | 14.63% |
| ≥75 | -0.24 | 0.005 | -0.20 | 0.008 | -0.04 | 0.006 | -0.25 | 0.005 | 0.29 | <0.001 | 16.67% |
| Cancer | |||||||||||
| Absent | -0.29 | 0.015 | -0.22 | 0.003 | -0.07 | 0.008 | -0.19 | <0.001 | 0.36 | <0.001 | 24.14% |
| Present | -0.42 | <0.001 | -0.37 | <0.001 | -0.05 | 0.010 | -0.17 | <0.001 | 0.35 | <0.001 | 11.90% |
Tab.4 Mediation analysis in the overall population and subgroups
Pathways sMg→log10 CRP→POD | c | P | c' | P | a*b | P | a | P | b | P | |ab/c| |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | -0.35 | <0.001 | -0.29 | <0.001 | -0.06 | 0.007 | -0.17 | <0.001 | 0.35 | <0.001 | 17.14% |
| Age (year) | |||||||||||
| <75 | -0.41 | <0.001 | -0.35 | 0.006 | -0.06 | <0.001 | -0.17 | <0.001 | 0.35 | <0.001 | 14.63% |
| ≥75 | -0.24 | 0.005 | -0.20 | 0.008 | -0.04 | 0.006 | -0.25 | 0.005 | 0.29 | <0.001 | 16.67% |
| Cancer | |||||||||||
| Absent | -0.29 | 0.015 | -0.22 | 0.003 | -0.07 | 0.008 | -0.19 | <0.001 | 0.36 | <0.001 | 24.14% |
| Present | -0.42 | <0.001 | -0.37 | <0.001 | -0.05 | 0.010 | -0.17 | <0.001 | 0.35 | <0.001 | 11.90% |
| Analysis | OR (95% CI) | P for trend | ||||
|---|---|---|---|---|---|---|
Quintile 1 (0.36-0.82) | Quintile 2 (0.82-0.87) | Quintile 3 (0.87-0.90) | Quintile 4 (0.90-0.94) | Quintile 5 (0.94-1.44) | ||
| Primary analysis | 1.81 (1.41, 2.35) | 1.26 (0.97, 1.65) | 1.27 (0.96, 1.68) | 1 (reference) | 1.06 (0.80, 1.40) | 0.054 |
| Sensitivity analysis | ||||||
Additional adjustment for major intraoperative factorsa (n=12 876) | 1.89 (1.47, 2.45) | 1.26 (0.97, 1.65) | 1.30 (0.98, 1.72) | 1 (reference) | 1.05 (0.80, 1.40) | 0.175 |
Excluding patients with confounders missing (n=12 570) | 1.79 (1.37, 2.29) | 1.25 (0.96, 1.64) | 1.29 (0.96,1.69) | 1 (reference) | 1.03 (0.75,1.32) | 0.188 |
| Excluding patients with dystrophy (n=12 246) | 1.81 (1.39, 2.37) | 1.28 (0.97, 1.69) | 1.29 (0.97, 1.73) | 1 (reference) | 1.04 (0.78, 1.40) | 0.240 |
Excluding patients with inflammation, hepatic or renal insufficiency (n=12 156) | 1.92 (1.48, 2.52) | 1.30 (0.99, 1.72) | 1.26 (0.93, 1.69) | 1 (reference) | 1.04 (0.77, 1.40) | 0.124 |
Tab.5 Sensitivity analysis for associations between preoperative serum magnesium levels and POD risk
| Analysis | OR (95% CI) | P for trend | ||||
|---|---|---|---|---|---|---|
Quintile 1 (0.36-0.82) | Quintile 2 (0.82-0.87) | Quintile 3 (0.87-0.90) | Quintile 4 (0.90-0.94) | Quintile 5 (0.94-1.44) | ||
| Primary analysis | 1.81 (1.41, 2.35) | 1.26 (0.97, 1.65) | 1.27 (0.96, 1.68) | 1 (reference) | 1.06 (0.80, 1.40) | 0.054 |
| Sensitivity analysis | ||||||
Additional adjustment for major intraoperative factorsa (n=12 876) | 1.89 (1.47, 2.45) | 1.26 (0.97, 1.65) | 1.30 (0.98, 1.72) | 1 (reference) | 1.05 (0.80, 1.40) | 0.175 |
Excluding patients with confounders missing (n=12 570) | 1.79 (1.37, 2.29) | 1.25 (0.96, 1.64) | 1.29 (0.96,1.69) | 1 (reference) | 1.03 (0.75,1.32) | 0.188 |
| Excluding patients with dystrophy (n=12 246) | 1.81 (1.39, 2.37) | 1.28 (0.97, 1.69) | 1.29 (0.97, 1.73) | 1 (reference) | 1.04 (0.78, 1.40) | 0.240 |
Excluding patients with inflammation, hepatic or renal insufficiency (n=12 156) | 1.92 (1.48, 2.52) | 1.30 (0.99, 1.72) | 1.26 (0.93, 1.69) | 1 (reference) | 1.04 (0.77, 1.40) | 0.124 |
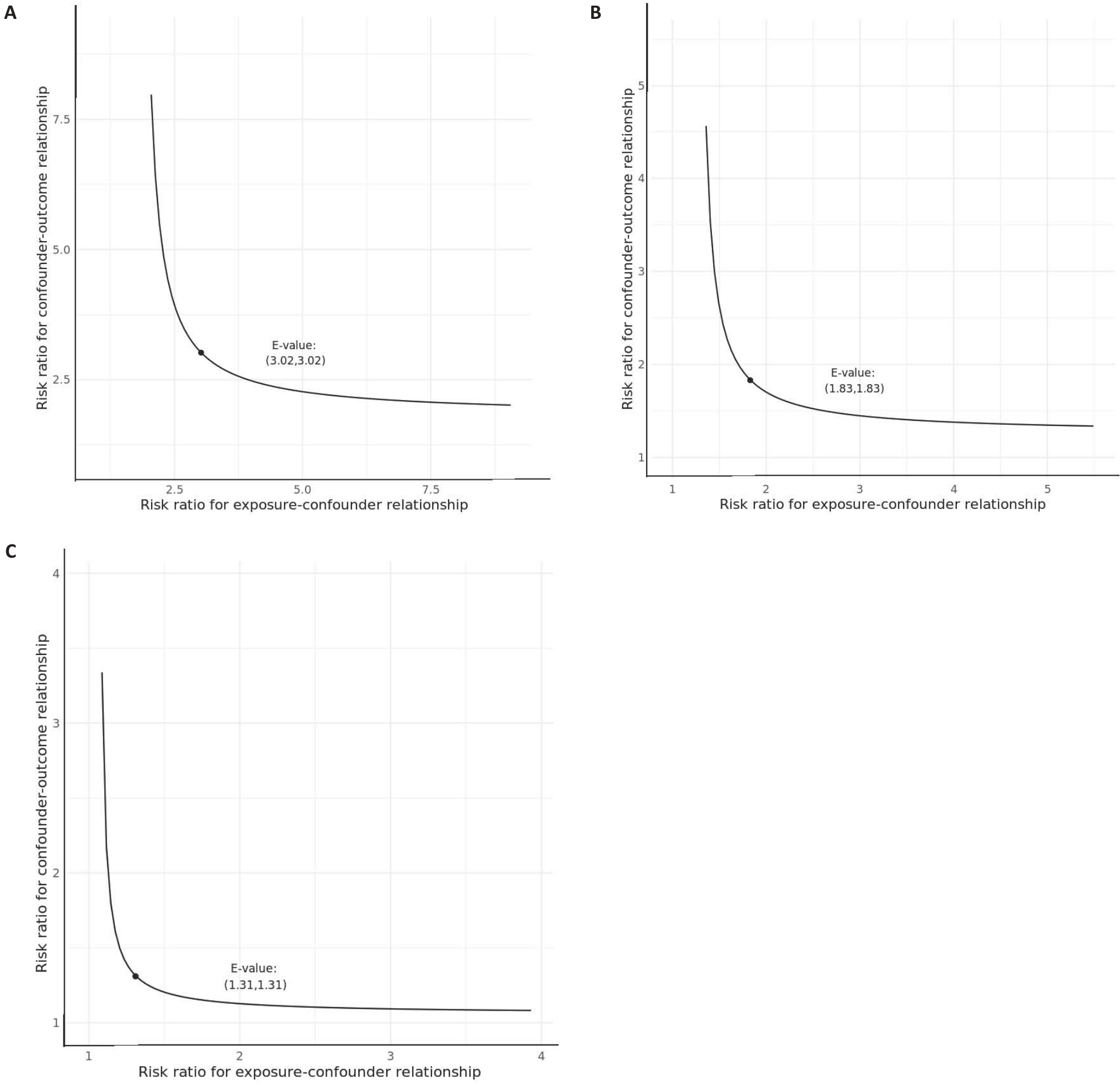
Fig. 7 Curves of the sensitivity analyses for unobserved confounders with E-value highlighted. A: E-value for quintile 1 point estimate: 3.02 and for confidence interval: 2.17. B: E-value for quintile 2 point estimate: 1.83 and for confidence interval: 1. C: E-value for quintile 5 point estimate:1.31 and for confidence interval: 1.
| [1] | Hughes CG, Boncyk CS, Culley DJ, et al. American society for enhanced recovery and perioperative quality initiative joint consensus statement on postoperative delirium prevention[J]. Anesth Analg, 2020, 130(6): 1572-90. doi:10.1213/ane.0000000000004641 |
| [2] | Oh ES, Fong TG, Hshieh TT, et al. Delirium in older persons: advances in diagnosis and treatment[J]. JAMA, 2017, 318(12): 1161-74. doi:10.1001/jama.2017.12067 |
| [3] | Yan E, Veitch M, Saripella A, et al. Association between postoperative delirium and adverse outcomes in older surgical patients: a systematic review and meta-analysis[J]. J Clin Anesth, 2023, 90: 111221. doi:10.1016/j.jclinane.2023.111221 |
| [4] | Jin Z, Hu J, Ma D. Postoperative delirium: perioperative assessment, risk reduction, and management[J]. Br J Anaesth, 2020, 125(4): 492-504. doi:10.1016/j.bja.2020.06.063 |
| [5] | Mattison MLP. Delirium[J]. Ann Intern Med, 2020, 173(7): ITC49-64. doi:10.7326/aitc202010060 |
| [6] | Maier JAM, Locatelli L, Fedele G, et al. Magnesium and the brain: a focus on neuroinflammation and neurodegeneration[J]. Int J Mol Sci, 2022, 24(1): 223. doi:10.3390/ijms24010223 |
| [7] | Kirkland AE, Sarlo GL, Holton KF. The role of magnesium in neurological disorders[J]. Nutrients, 2018, 10(6): E730. doi:10.3390/nu10060730 |
| [8] | Veronese N, Zurlo A, Solmi M, et al. Magnesium status in Alzheimer's disease: a systematic review[J]. Am J Alzheimers Dis Other Demen, 2016, 31(3): 208-13. doi:10.1177/1533317515602674 |
| [9] | Yamanaka R, Shindo Y, Oka K. Magnesium is a key player in neuronal maturation and neuropathology[J]. Int J Mol Sci, 2019, 20(14): E3439. doi:10.3390/ijms20143439 |
| [10] | Hynd MR, Scott HL, Dodd PR. Glutamate-mediated excitotoxicity and neurodegeneration in Alzheimer's disease[J]. Neurochem Int, 2004, 45(5): 583-95. doi:10.1016/j.neuint.2004.03.007 |
| [11] | Slutsky I, Sadeghpour S, Li B, et al. Enhancement of synaptic plasticity through chronically reduced Ca2+ flux during uncorrelated activity[J]. Neuron, 2004, 44(5): 835-49. doi:10.1016/j.neuron.2004.11.013 |
| [12] | Serita T, Miyahara M, Tanimizu T, et al. Dietary magnesium deficiency impairs hippocampus-dependent memories without changes in the spine density and morphology of hippocampal neurons in mice[J]. Brain Res Bull, 2019, 144: 149-57. doi:10.1016/j.brainresbull.2018.11.019 |
| [13] | Balmuș IM, Strungaru SA, Ciobica A, et al. Preliminary data on the interaction between some biometals and oxidative stress status in mild cognitive impairment and Alzheimer’s disease patients[J]. Oxid Med Cell Longev, 2017, 2017: 7156928. doi:10.1155/2017/7156928 |
| [14] | Kieboom BCT, Licher S, Wolters FJ, et al. Serum magnesium is associated with the risk of dementia[J]. Neurology, 2017, 89(16): 1716-22. doi:10.1212/wnl.0000000000004517 |
| [15] | Kim JY, Lee HJ, Lee HY, et al. The effects of hypomagnesemia on delirium in middle-aged and older adult patients admitted to medical intensive care units[J]. Acute Crit Care, 2022, 37(3): 407-14. doi:10.4266/acc.2022.00164 |
| [16] | Boccardi V, Ercolani S, Serra R, et al. Hypomagnesemia and incident delirium in hospitalized older persons[J]. Aging Clin Exp Res, 2023, 35(4): 847-53. doi:10.1007/s40520-023-02357-3 |
| [17] | Fathy W, Hussein M, Elanwar R, et al. Effect of intra-operative Magnesium sulphate on the occurrence of post-operative delirium and insomnia in patients undergoing lumbar fixation: a randomized controlled trial[J]. BMC Anesthesiol, 2024, 24(1): 289. doi:10.1186/s12871-024-02579-6 |
| [18] | Hassan WF, Tawfik MH, Nabil TM, et al. Could intraoperative magnesium sulphate protect against postoperative cognitive dysfunction[J]? Minerva Anestesiol, 2020, 86(8): 808-15. doi:10.23736/s0375-9393.20.14012-4 |
| [19] | Li W, Yu J, Liu Y, et al. Elevation of brain magnesium prevents synaptic loss and reverses cognitive deficits in Alzheimer’s disease mouse model[J]. Mol Brain, 2014, 7: 65. doi:10.1186/s13041-014-0065-y |
| [20] | Cederholm T, Bosaeus I, Barazzoni R, et al. Diagnostic criteria for malnutrition–an ESPEN consensus statement[J]. Clin Nutr, 2015, 34(3): 335-40. doi:10.1016/j.clnu.2015.03.001 |
| [21] | Zhang LM, Hornor MA, Robinson T, et al. Evaluation of postoperative functional health status decline among older adults[J]. JAMA Surg, 2020, 155(10): 950-8. doi:10.1001/jamasurg.2020.2853 |
| [22] | Kim EM, Li G, Kim M. Development of a risk score to predict postoperative delirium in patients with hip fracture[J]. Anesth Analg, 2020, 130(1): 79-86. doi:10.1213/ane.0000000000004386 |
| [23] | Saczynski JS, Kosar CM, Xu G, et al. A tale of two methods: chart and interview methods for identifying delirium[J]. J Am Geriatr Soc, 2014, 62(3): 518-24. doi:10.1111/jgs.12684 |
| [24] | Peduzzi P, Concato J, Kemper E, et al. A simulation study of the number of events per variable in logistic regression analysis[J]. J Clin Epidemiol, 1996, 49(12): 1373-9. doi:10.1016/s0895-4356(96)00236-3 |
| [25] | Zhang Q, Xiao S, Jiao X, et al. The triglyceride-glucose index is a predictor for cardiovascular and all-cause mortality in CVD patients with diabetes or pre-diabetes: evidence from NHANES 2001-2018[J]. Cardiovasc Diabetol, 2023, 22(1): 279. doi:10.1186/s12933-023-02030-z |
| [26] | Textor J, van der Zander B, Gilthorpe MS, et al. Robust causal inference using directed acyclic graphs: the R package ‘dagitty’[J]. Int J Epidemiol, 2016, 45(6): 1887-94. |
| [27] | Lindenauer PK, Stefan MS, Pekow PS, et al. Association between initiation of pulmonary rehabilitation after hospitalization for COPD and 1-year survival among medicare beneficiaries[J]. JAMA, 2020, 323(18): 1813-23. doi:10.1001/jama.2020.4437 |
| [28] | Hou H, Wang L, Fu T, et al. Magnesium acts as a second messenger in the regulation of NMDA receptor-mediated CREB signaling in neurons[J]. Mol Neurobiol, 2020, 57(6): 2539-50. doi:10.1007/s12035-020-01871-z |
| [29] | Rajani V, Sengar AS, Salter MW. Tripartite signalling by NMDA receptors[J]. Mol Brain, 2020, 13(1): 23. doi:10.1186/s13041-020-0563-z |
| [30] | Metwally E, Zhao GL, Zhang YQ. The calcium-dependent protease calpain in neuronal remodeling and neurodegeneration[J]. Trends Neurosci, 2021, 44(9): 741-52. doi:10.1016/j.tins.2021.07.003 |
| [31] | Collingridge GL. Long-term potentiation in the hippocampus: from magnesium to memory[J]. Neuroscience, 2025, 578: 126-31. doi:10.1016/j.neuroscience.2024.11.069 |
| [32] | Maridaki Z, Syrros G, Gianna Delichatsiou S, et al. Claudin-5 and occludin levels in patients with psychiatric disorders-A systematic review[J]. Brain Behav Immun, 2025, 123: 865-75. doi:10.1016/j.bbi.2024.11.006 |
| [33] | Jawa RS, Anillo S, Huntoon K, et al. Interleukin-6 in surgery, trauma, and critical care part II: clinical implications[J]. J Intensive Care Med, 2011, 26(2): 73-87. doi:10.1177/0885066610384188 |
| [34] | Zhu D, You J, Zhao N, et al. Magnesium regulates endothelial barrier functions through TRPM7, MagT1, and S1P1[J]. Adv Sci: Weinh, 2019, 6(18): 1901166. doi:10.1002/advs.201901166 |
| [35] | Esen F, Erdem T, Aktan D, et al. Effect of magnesium sulfate administration on blood-brain barrier in a rat model of intraperitoneal sepsis: a randomized controlled experimental study[J]. Crit Care, 2005, 9(1): R18-R23. doi:10.1186/cc3004 |
| [36] | Ben-David D, Livne E, Reznick AZ. The involvement of oxidants and NF-κB in cytokine-induced MMP-9 synthesis by bone marrow-derived osteoprogenitor cells[J]. Inflamm Res, 2012, 61(7): 673-88. doi:10.1007/s00011-012-0461-7 |
| [37] | Chiarini A, Gui L, Viviani C, et al. NLRP3 inflammasome's activation in acute and chronic brain diseases-an update on pathogenetic mechanisms and therapeutic perspectives with respect to other inflammasomes[J]. Biomedicines, 2023, 11(4): 999. doi:10.3390/biomedicines11040999 |
| [38] | Kelley N, Jeltema D, Duan Y, et al. The NLRP3 inflammasome: an overview of mechanisms of activation and regulation[J]. Int J Mol Sci, 2019, 20(13): E3328. doi:10.3390/ijms20133328 |
| [39] | Yang S, Gu C, Mandeville ET, et al. Anesthesia and surgery impair blood-brain barrier and cognitive function in mice[J]. Front Immunol, 2017, 8: 902. doi:10.3389/fimmu.2017.00902 |
| [40] | Ma G, Jiang X, Meng X, et al. Inhibition of NLRP3 inflammasome alleviates postoperative cognitive impairment by suppressing the HMGB-1/TLR4/NF‑κB pathway[J]. Neurochem Res, 2025, 50(3): 173. doi:10.1007/s11064-025-04416-9 |
| [41] | Perazella MA. Onco-nephrology: renal toxicities of chemothera-peutic agents[J]. Clin J Am Soc Nephrol, 2012, 7(10): 1713-21. doi:10.2215/cjn.02780312 |
| [42] | Kimura A, Kato K, Nakashima A, et al. Association between parathyroid hormone-related peptide levels and mortality in patients with malignancy[J]. Endocr Pract, 2024, 30(12): 1119-25. doi:10.1016/j.eprac.2024.09.003 |
| [43] | Javanmehr N, Saleki K, Alijanizadeh P, et al. Microglia dynamics in aging-related neurobehavioral and neuroinflammatory diseases[J]. J Neuroinflammation, 2022, 19(1): 273. doi:10.1186/s12974-022-02637-1 |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||