Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (1): 118-125.doi: 10.12122/j.issn.1673-4254.2025.01.15
Previous Articles Next Articles
Qing SHI( ), Suye RAN, Lingyu SONG, Hong YANG, Wenjuan WANG, Hanlin LIU, Qi LIU(
), Suye RAN, Lingyu SONG, Hong YANG, Wenjuan WANG, Hanlin LIU, Qi LIU( )
)
Received:2024-09-09
Online:2025-01-20
Published:2025-01-20
Contact:
Qi LIU
E-mail:1090720176@ qq.com;gyqiliu6071@ sina.com
Qing SHI, Suye RAN, Lingyu SONG, Hong YANG, Wenjuan WANG, Hanlin LIU, Qi LIU. NLRP6 overexpression improves nonalcoholic fatty liver disease by promoting lipid oxidation and decomposition in hepatocytes through the AMPK/CPT1A/PGC1A pathway[J]. Journal of Southern Medical University, 2025, 45(1): 118-125.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.01.15
| Gene | Forward primer | Reverse primer |
|---|---|---|
| Homo CD36 | ACGCTGAGGACAACACAGTCT | GCCACAGCCAGATTGAGAAC |
| Homo FATP1 | ACGCGATATACCAGGAGCTG | ATCTTGAAGGTGCCTGTGGT |
| Homo PPARG | CATAAAGTCCTTCCCGCTGA | TCTGTGATCTCCTGCACAGC |
| Homo SREBF1 | GCTGTTGGTGCTCGTCTCCTTG | GCTTGCGATGCCTCCAGAAGTAC |
| Homo FASN | GTCCACCAGCAACATCAGC | GTTCTCCAGCAAGCCATCTC |
| Homo CPT1A | GCACATCGTCGTGTACCATC | AATAGGCCTGACGACACCTG |
| Homo PGC1A | GAAGCAGACAAGACCGGTGA | AATAGGCCTGACGACACCTG |
| Homo MTTP | CTTCCTGGCCTTCATTCAGC | AGCAGAGGTGACAGCATCCA |
| Homo GAPDH | CTCCTCCTGTTCGACAGTCAGC | CCCAATACGACCAAATCCGTT |
| Homo NLRP6 | GGAGTTGCTGTACTGCCTGT | CCTCAGAAAGGTCTCGGCAG |
| Mus NLRP6 | CGGGACGAGAGGAAGGCAGAG | CACACGATCCAGCACACGAAGG |
| Mus β-actin | TCATCACTATTGGCAACGAGC | AACAGTCCGCCTAGAAGCAC |
Tab.1 Primers for RT-qPCR
| Gene | Forward primer | Reverse primer |
|---|---|---|
| Homo CD36 | ACGCTGAGGACAACACAGTCT | GCCACAGCCAGATTGAGAAC |
| Homo FATP1 | ACGCGATATACCAGGAGCTG | ATCTTGAAGGTGCCTGTGGT |
| Homo PPARG | CATAAAGTCCTTCCCGCTGA | TCTGTGATCTCCTGCACAGC |
| Homo SREBF1 | GCTGTTGGTGCTCGTCTCCTTG | GCTTGCGATGCCTCCAGAAGTAC |
| Homo FASN | GTCCACCAGCAACATCAGC | GTTCTCCAGCAAGCCATCTC |
| Homo CPT1A | GCACATCGTCGTGTACCATC | AATAGGCCTGACGACACCTG |
| Homo PGC1A | GAAGCAGACAAGACCGGTGA | AATAGGCCTGACGACACCTG |
| Homo MTTP | CTTCCTGGCCTTCATTCAGC | AGCAGAGGTGACAGCATCCA |
| Homo GAPDH | CTCCTCCTGTTCGACAGTCAGC | CCCAATACGACCAAATCCGTT |
| Homo NLRP6 | GGAGTTGCTGTACTGCCTGT | CCTCAGAAAGGTCTCGGCAG |
| Mus NLRP6 | CGGGACGAGAGGAAGGCAGAG | CACACGATCCAGCACACGAAGG |
| Mus β-actin | TCATCACTATTGGCAACGAGC | AACAGTCCGCCTAGAAGCAC |
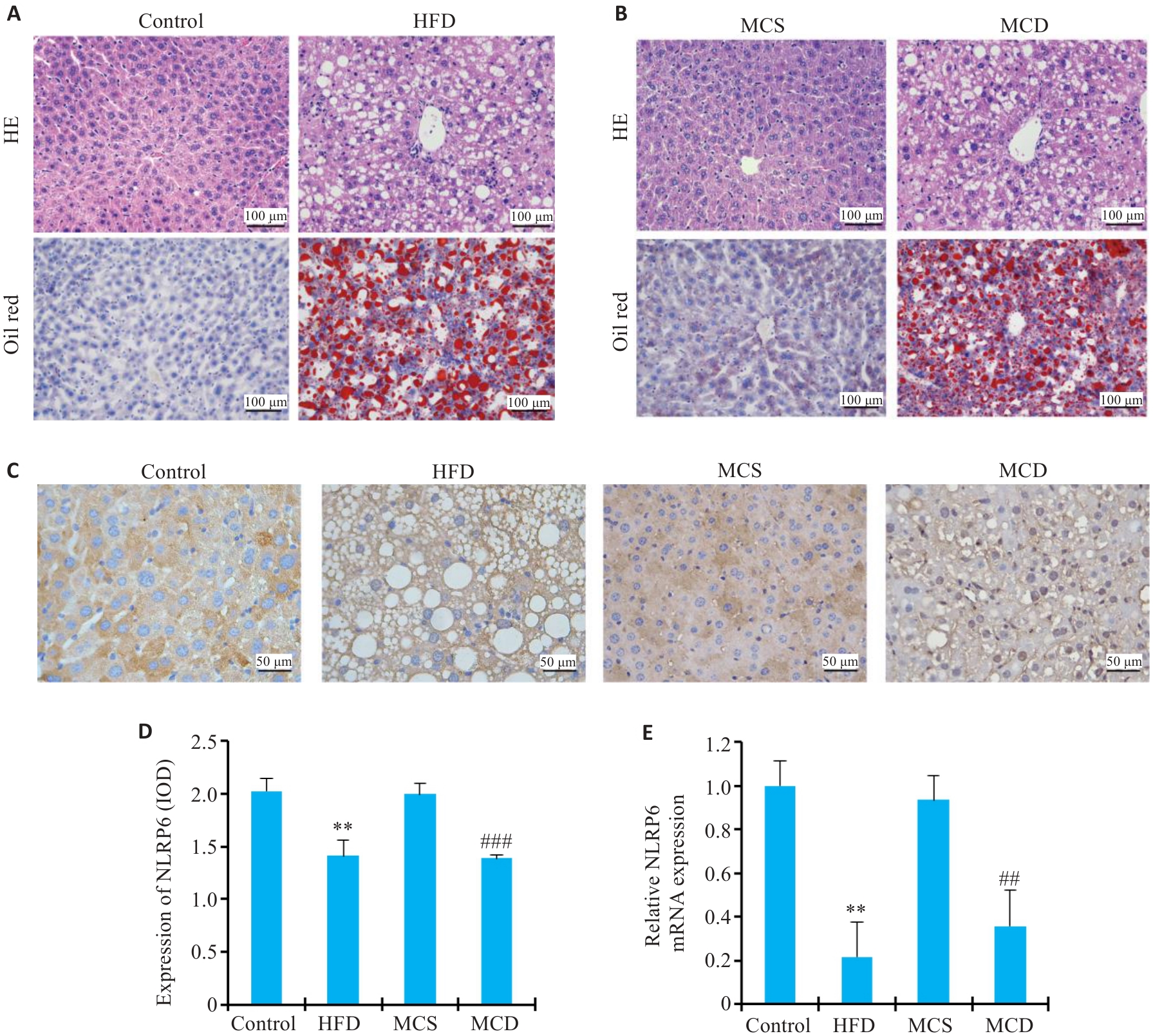
Fig. 1 NLRP6 expression is decreased in the liver of mouse models of NAFLD. A, B: HE and oil red O staining for detecting lipid deposition in the liver. C, D: NLRP6 immunohistochemical staining of the liver of NAFLD mice (**P<0.01 vs Control, ## #P<0.001 vs control MCS). E: NLRP6 mRNA expression level in the liver of NAFLD mice (**P<0.01 vs Control, ##P<0.01 vs MCS).
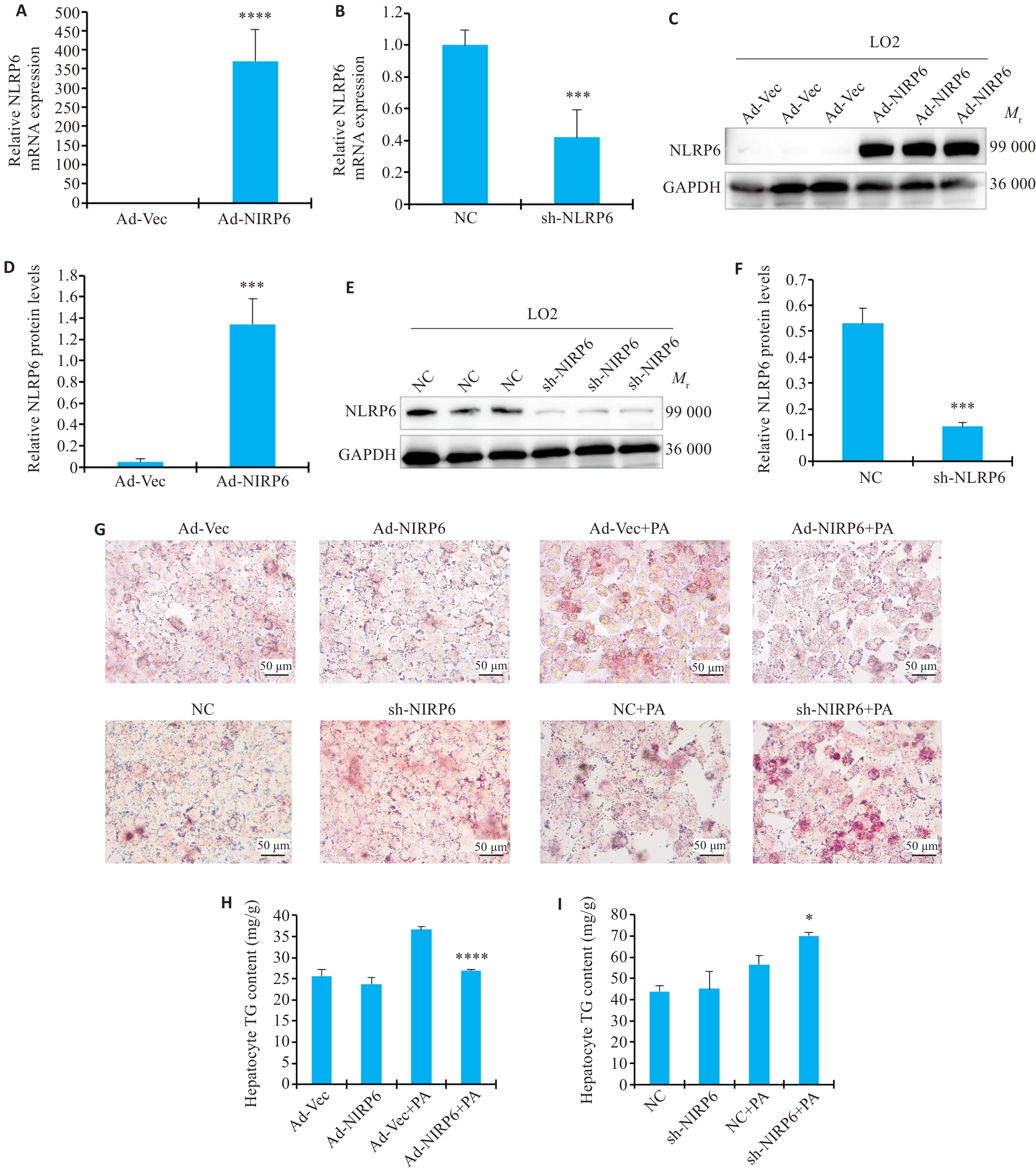
Fig.2 Effect of NLRP6 on lipid deposition in cultured hepatocytes A: Relative NLRP6 mRNA levels in NLRP6-overexpressing hepatocytes (****P<0.0001). B: Relative NLRP6 mRNA levels in hepatocytes with NLRP6 knockdown (***P<0.001). C, D: Relative NLRP6 protein levels in NLRP6-overexpressing hepatocytes (***P<0.001). E, F: Relative NLRP6 protein levels in hepatocytes with NLRP6 knockdown (***P<0.001). G: oil red O staining of hepatocytes with NLRP6 overexpression or knockdown. H: TG content in NLRP6-overexpressing hepatocytes (****P<0.0001 vs Ad-Vec+PA group ). I: TG content in hepatocytes with NLRP6 knockdown (*P<0.05 vs NC+PA group).
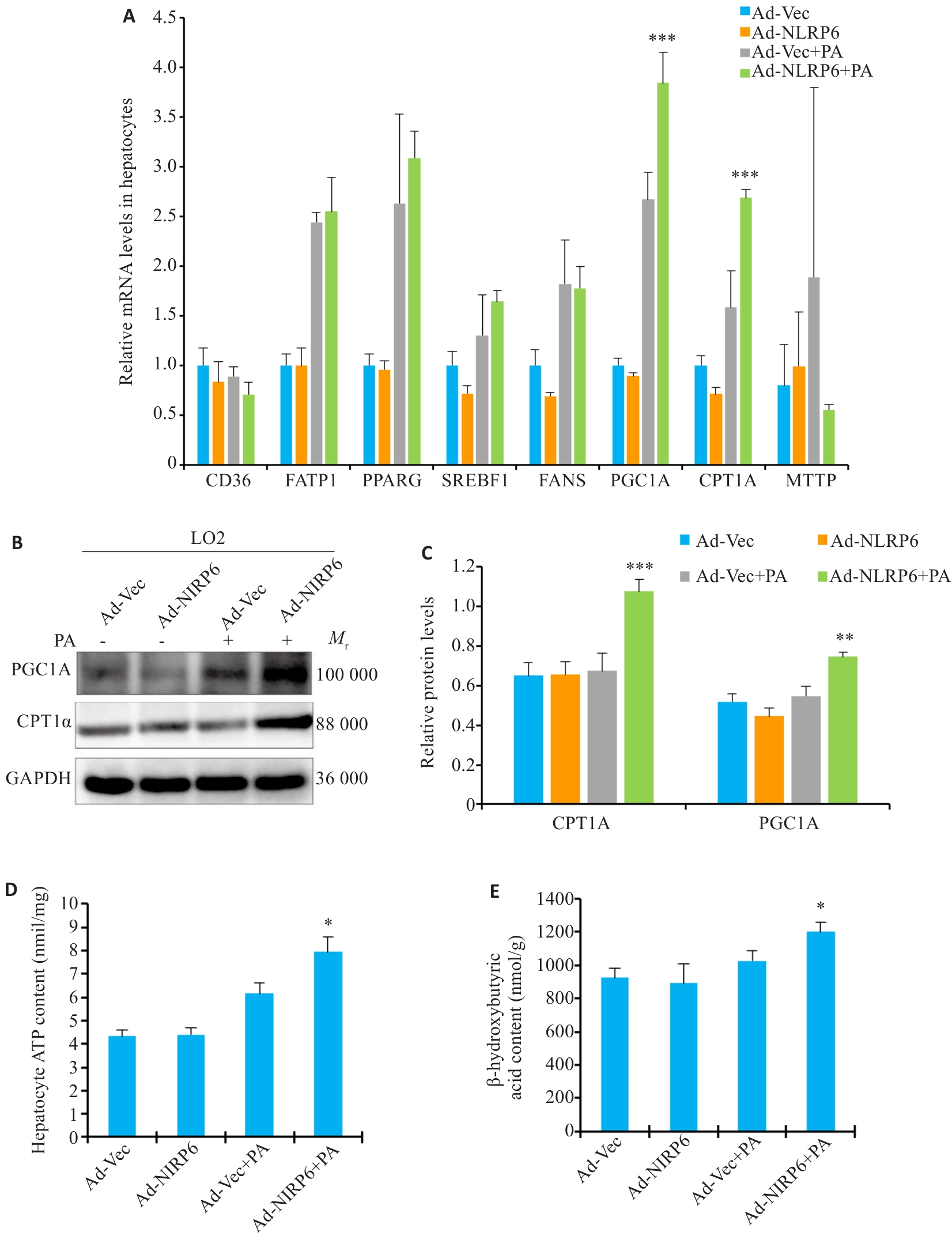
Fig.3 Effect of NLRP6 on lipid oxidation and decomposition in hepatocytes A: mRNA expression levels of lipid metabolism-related genes in PA-treated liver cells overexpressing NLRP6 (***P<0.001 vs Ad-Vec+PA group). B, C: Western blotting of CPT1A and PGC1A in NLRP6-overexpressing hepatocytes (**P<0.01, ***P<0.001 vs Ad-Vec+PA group). D: ATP content in NLRP6-overexpressing hepatocytes (*P<0.05 vs Ad-Vec+PA group). E: β-hydroxybutyrate content in NLRP6-overexpressing hepatocytes (*P<0.05 vs Ad-Vec+PA group).
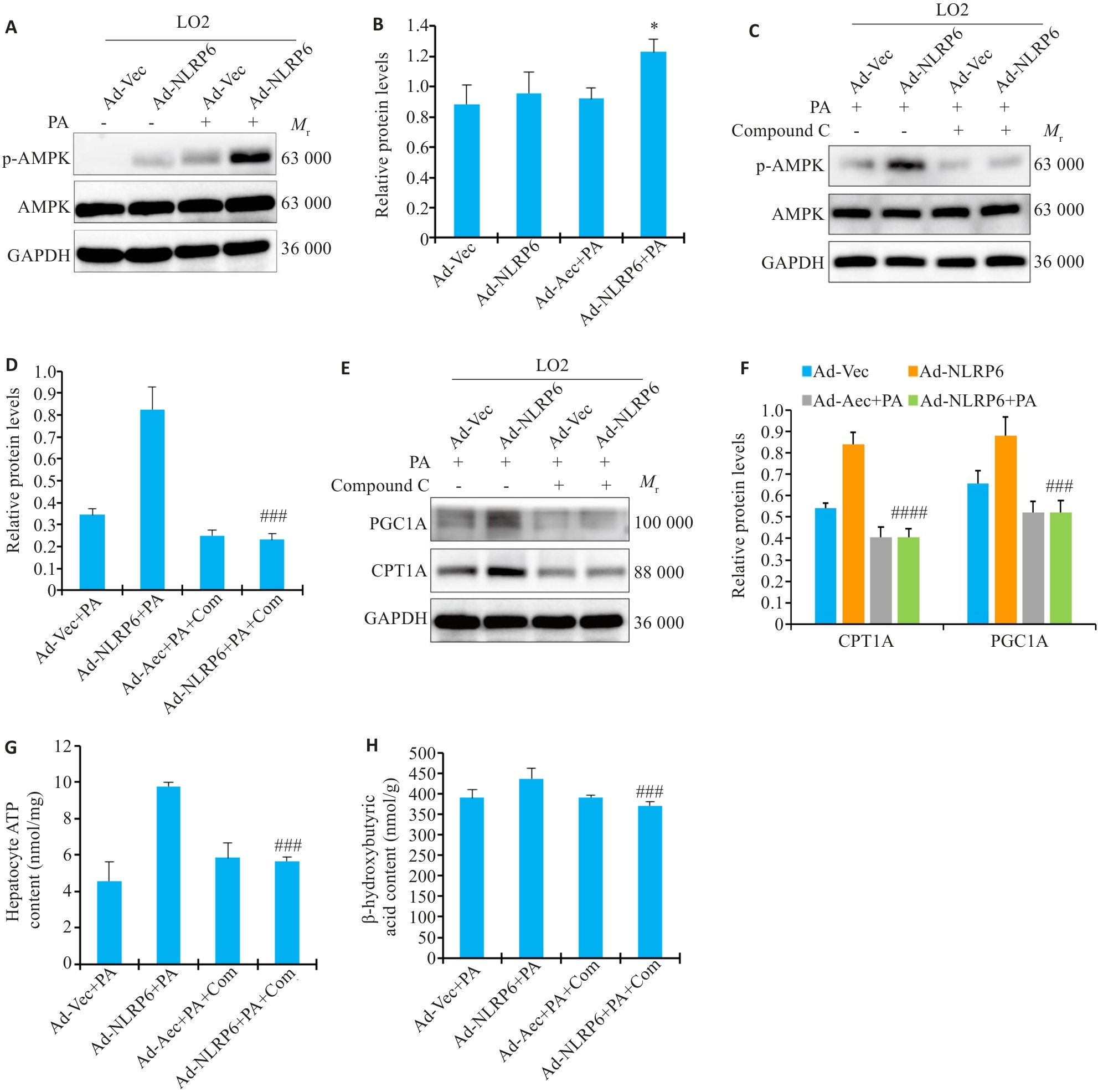
Fig.4 Effect of NLRP6 on AMPK pathway in hepatocytes. A, B: Western blotting for p-AMPK in NLRP6-overexpressing hepatocytes (*P<0.05 vs Ad-Vec+PA ). C, D: Western blotting for p-AMPK in NLRP6-overexpressing hepatocytes treated with AMPK inhibitor ( ###P<0.001 vs Ad-NLRP6+PA). E, F: Western blotting for CPT1A and PGC1A in NLRP6-overexpressing hepatocytes treated with AMPK inhibitor (###P<0.001, ####P<0.0001 vs Ad-NLRP6+PA). G: ATP content in NLRP6-overexpressing hepatocytes treated with AMPK inhibitor (###P<0.001 vs Ad-NLRP6+PA). H: β‑hydroxybutyrate content in NLRP6-overexpressing hepatocytes treated with AMPK inhibitor (###P<0.001 vs Ad-NLRP6+PA) .
| 1 | Powell EE, Wong VW, Rinella M. Non-alcoholic fatty liver disease[J]. Lancet, 2021, 397(10290): 2212-24. |
| 2 | Younossi ZM. Non-alcoholic fatty liver disease-A global public health perspective[J]. J Hepatol, 2019, 70(3): 531-44. |
| 3 | Sanyal AJ, van Natta ML, Clark J, et al. Prospective study of outcomes in adults with nonalcoholic fatty liver disease[J]. N Engl J Med, 2021, 385(17): 1559-69. |
| 4 | Rong L, Zou JY, Ran W, et al. Advancements in the treatment of non-alcoholic fatty liver disease (NAFLD)[J]. Front Endocrinol, 2023, 13: 1087260. |
| 5 | Li RZ, Zhu S. NLRP6 inflammasome[J]. Mol Aspects Med, 2020, 76: 100859. |
| 6 | Zheng DP, Kern L, Elinav E. The NLRP6 inflammasome[J]. Immunology, 2021, 162(3): 281-9. |
| 7 | Tao Q, Xu DY, Jia KX, et al. NLRP6 serves as a negative regulator of neutrophil recruitment and function during Streptococcus pneumoniae infection[J]. Front Microbiol, 2022, 13: 898559. |
| 8 | Mukherjee S, Kumar R, Tsakem Lenou E, et al. Deubiquitination of NLRP6 inflammasome by Cyld critically regulates intestinal inflammation[J]. Nat Immunol, 2020, 21(6): 626-35. |
| 9 | Huang CY, Liu QH, Tang Q, et al. Hepatocyte-specific deletion of Nlrp6 in mice exacerbates the development of non-alcoholic steatohepatitis[J]. Free Radic Biol Med, 2021, 169: 110-21. |
| 10 | Frietze KK, Brown AM, Das D, et al. Lipotoxicity reduces DDX58/Rig-1 expression and activity leading to impaired autophagy and cell death[J]. Autophagy, 2022, 18(1): 142-60. |
| 11 | Schneider KM, Mohs A, Gui WF, et al. Imbalanced gut microbiota fuels hepatocellular carcinoma development by shaping the hepatic inflammatory microenvironment[J]. Nat Commun, 2022, 13(1): 3964. |
| 12 | Badmus OO, Hillhouse SA, Anderson CD, et al. Molecular mechanisms of metabolic associated fatty liver disease (MAFLD): functional analysis of lipid metabolism pathways[J]. Clin Sci, 2022, 136(18): 1347-66. |
| 13 | Yki-Järvinen H, Luukkonen PK, Hodson L, et al. Dietary carbohydrates and fats in nonalcoholic fatty liver disease[J]. Nat Rev Gastroenterol Hepatol, 2021, 18(11): 770-86. |
| 14 | Machado MV, Diehl AM. Pathogenesis of nonalcoholic steatohepatitis[J]. Gastroenterology, 2016, 150(8): 1769-77. |
| 15 | Ipsen DH, Lykkesfeldt J, Tveden-Nyborg P. Molecular mechanisms of hepatic lipid accumulation in non-alcoholic fatty liver disease[J]. Cell Mol Life Sci, 2018, 75(18): 3313-27. |
| 16 | Yamamoto T, Takabatake Y, Minami S, et al. Eicosapentaenoic acid attenuates renal lipotoxicity by restoring autophagic flux[J]. Autophagy, 2021, 17(7): 1700-13. |
| 17 | Li K, Gao L, Zhou S, et al. Erythropoietin promotes energy metabolism to improve LPS-induced injury in HK-2 cells via SIRT1/PGC1-α pathway[J]. Mol Cell Biochem, 2023, 478(3): 651-63. |
| 18 | Helsley RN, Park SH, Vekaria HJ, et al. Ketohexokinase-C regulates global protein acetylation to decrease carnitine palmitoyltransferase 1a-mediated fatty acid oxidation[J]. J Hepatol, 2023, 79(1): 25-42. |
| 19 | Sun W, Nie T, Li K, et al. Hepatic CPT1A facilitates liver-adipose cross-talk via induction of FGF21 in mice[J]. Diabetes, 2021: db210363. |
| 20 | Schlaepfer IR, Joshi M. CPT1A-mediated fat oxidation, mechanisms, and therapeutic potential[J]. Endocrinology, 2020, 161(2): bqz046. |
| 21 | Qian L, Zhu Y, Deng C, et al. Peroxisome proliferator-activated receptor gamma coactivator-1 (PGC-1) family in physiological and pathophysiological process and diseases[J]. Signal Transduct Target Ther, 2024,9(1):50. |
| 22 | Trefts E, Shaw RJ. AMPK: restoring metabolic homeostasis over space and time[J]. Mol Cell, 2021, 81(18): 3677-90. |
| 23 | Diniz TA, de Lima Junior EA, Teixeira AA, et al. Aerobic training improves NAFLD markers and insulin resistance through AMPK-PPAR-α signaling in obese mice[J]. Life Sci, 2021, 266: 118868. |
| 24 | Herzig S, Shaw RJ. AMPK: guardian of metabolism and mitochondrial homeostasis[J]. Nat Rev Mol Cell Biol, 2018, 19(2): 121-35. |
| 25 | Lin SC, Hardie DG. AMPK: sensing glucose as well as cellular energy status[J]. Cell Metab, 2018, 27(2): 299-313. |
| 26 | Steinberg GR, Hardie DG. New insights into activation and function of the AMPK[J]. Nat Rev Mol Cell Biol, 2023, 24(4): 255-72. |
| 27 | Nakamura MT, Yudell BE, Loor JJ. Regulation of energy metabolism by long-chain fatty acids[J]. Prog Lipid Res, 2014, 53: 124-44. |
| 28 | Fang CQ, Pan JH, Qu N, et al. The AMPK pathway in fatty liver disease[J]. Front Physiol, 2022, 13: 970292. |
| 29 | Turkieh A, Caubère C, Barutaut M, et al. Apolipoprotein O is mitochondrial and promotes lipotoxicity in heart[J]. J Clin Investig, 2014, 124(5): 2277-86. |
| 30 | Bai DS, Du JY, Bu XM, et al. ALDOA maintains NLRP3 inflammasome activation by controlling AMPK activation[J]. Autophagy, 2022, 18(7): 1673-93. |
| 31 | He YT, Xu K, Wang Y, et al. AMPK as a potential pharmacological target for alleviating LPS-induced acute lung injury partly via NLRC4 inflammasome pathway inhibition[J]. Exp Gerontol, 2019, 125: 110661. |
| [1] | Lu ZHANG, Huanzhang DING, Haoran XU, Ke CHEN, Bowen XU, Qinjun YANG, Di WU, Jiabing TONG, Zegeng LI. Shenqi Buzhong Formula ameliorates mitochondrial dysfunction in a rat model of chronic obstructive pulmonary disease by activating the AMPK/SIRT1/PGC-1α pathway [J]. Journal of Southern Medical University, 2025, 45(5): 969-976. |
| [2] | Jing XIAO, Ying LI, Min FANG, Hong GONG, Wen LI, Chunyan ZHANG, Fangyao CHEN, Yan ZHANG, Tuo HAN. Triglyceride-glucose index in non-obese individuals: its association with and predictive value for non-alcoholic fatty liver disease [J]. Journal of Southern Medical University, 2024, 44(7): 1266-1271. |
| [3] | ZHOU Fengmin, GUO Yanju, CHEN Ning. Exercise promotes irisin expression to ameliorate renal injury in type 2 diabetic rats [J]. Journal of Southern Medical University, 2024, 44(4): 675-681. |
| [4] | SHAO Shan, BAI Weichao, ZHOU Pengcheng, LUO Minna, ZHAO Xinhan, LEI Jianjun. Metformin suppresses hypoxia-inducible factor-1α expression in cancer-associated fibroblasts to block tumor-stromal cross-talk in breast cancer [J]. Journal of Southern Medical University, 2024, 44(3): 428-436. |
| [5] | XIAO Hongmin, HAN Baosong, GUO Jiacheng, WU Chao, WU Jingyi. HTD4010 attenuates myocardial injury in mice with septic cardiomyopathy by promoting autophagy via the AMPK/mTOR signaling pathway [J]. Journal of Southern Medical University, 2024, 44(3): 507-514. |
| [6] | CHEN Guodong, LUO Suxin. Colchicine alleviates myocardial ischemia-reperfusion injury in mice by activating AMPK [J]. Journal of Southern Medical University, 2024, 44(2): 226-235. |
| [7] | Yunfei LI, Lijun PANG, Longwu SHU, Ming LI, Chuanbing HUANG. Qihuang Jianpi Zishen Granules improves thrombocytopenia in mice with systemic lupus erythematosus by suppressing platelet autophagy via the Ca2+/CaMKK2/AMPK/mTOR signaling pathway [J]. Journal of Southern Medical University, 2024, 44(12): 2327-2334. |
| [8] | Yonghua LI, Xinran XI, Meng ZHANG, Xun WU, Xianghai WANG. High expression of LINC00467 promotes proliferation and metastasis of lung adenocarcinoma cells by suppressing autophagy via inhibiting the AMPK/mTOR pathway [J]. Journal of Southern Medical University, 2024, 44(10): 1898-1909. |
| [9] | Cuiyuan HUANG, Yunping SUN, Wenqiang LI, Li LIU, Wei WANG, Jing ZHANG. Nlrp6 overexpression inhibits lipid synthesis to suppress proliferation of hepatocellular carcinoma cells by regulating the AMPK-Srebp1c axis [J]. Journal of Southern Medical University, 2024, 44(10): 1910-1917. |
| [10] | KONG Xiang, ZHANG Teng, ZHANG Yan, GAO Linxi, WANG Wen, WANG Mengyan, WANG Guodong, LÜ Kun. Overexpression of lncRNA HEM2M alleviates liver injury in mice with non-alcoholic fatty liver disease [J]. Journal of Southern Medical University, 2024, 44(1): 1-8. |
| [11] | DENG Guanghui, JIA Hui, LI Yunjia, LI Junjie, WU Chaofeng, SHI Hao, QIN Mengchen, ZHAO Jiamin, LIU Chang, LIAO Yuxin, GAO Lei. Erchen Decoction improves iron homeostasis in mice with non-alcoholic fatty liver disease by regulating iron transport capacity in the spleen [J]. Journal of Southern Medical University, 2023, 43(8): 1287-1296. |
| [12] | MA Jinmiao, XU Zhibing, ZHU Jie, LIU Yingqing, WANG Qingqing, XI Xixiang, ZHANG Lifen, HUANG Jing, XIAO Lingling. Fuyu Decoction improves ventricular remodeling in rats with heart failure by inhibiting AMPK/mTOR pathway-mediated autophagy [J]. Journal of Southern Medical University, 2023, 43(3): 466-473. |
| [13] | CHEN Xing, WANG Kaiwan, CHU Dehai, ZHU Yu, ZHANG Wenbing, CAO Huiping, XIE Wenyu, LU Chuanhao, LI Xia. Forsythiaside B inhibits cerebral ischemia/reperfusion-induced oxidative stress injury in mice via the AMPK/DAF-16/FOXO3 pathway [J]. Journal of Southern Medical University, 2023, 43(2): 199-205. |
| [14] | WAN Lu, QIAN Yuchi, NI Wenjing, LU Yuxin, LI Wei, PAN Yan, CHEN Weidong. Linagliptin improves diabetic kidney disease in rats by promoting mitochondrial biogenesis through the AMPK/PGC-1α/TFAM pathway [J]. Journal of Southern Medical University, 2023, 43(12): 2053-2060. |
| [15] | WEI Jia, YANG Qiang, LIN Lin, ZHU Canzhan, WEI Jin. Metformin mitigates doxorubicin-induced cardiotoxicity via the AMPK pathway [J]. Journal of Southern Medical University, 2023, 43(10): 1682-1688. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||