Journal of Southern Medical University ›› 2026, Vol. 46 ›› Issue (1): 23-33.doi: 10.12122/j.issn.1673-4254.2026.01.03
Previous Articles Next Articles
Bei ZHAO1( ), Zhengyi LÜ2(
), Zhengyi LÜ2( ), Dingru JI1, Shuxin TIAN1, Yuxin WU1, Xingzhen LI1, Jie ZHOU1, Jianqiao FANG1, Yi LIANG1(
), Dingru JI1, Shuxin TIAN1, Yuxin WU1, Xingzhen LI1, Jie ZHOU1, Jianqiao FANG1, Yi LIANG1( )
)
Received:2025-05-26
Online:2026-01-20
Published:2026-01-16
Contact:
Yi LIANG
E-mail:984722585@qq.com;aprilv_kuco@icloud.com;liangyiwww@126.com
Supported by:Bei ZHAO, Zhengyi LÜ, Dingru JI, Shuxin TIAN, Yuxin WU, Xingzhen LI, Jie ZHOU, Jianqiao FANG, Yi LIANG. Temporal changes of chronic postsurgical pain in mice: the regulatory role of CX3CL1 in the dorsal root ganglion[J]. Journal of Southern Medical University, 2026, 46(1): 23-33.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2026.01.03
| Gene | Sequence (5′-3′) |
|---|---|
| Cx3cl1 forward | CAGAGGAGCAGGCAGGACAG |
| Cx3cl1 reverse | CTTCAGAGCAGGAGAGACCCATC |
| Cxcl14 forward | TCCGGTCAGCATGAGGCTCC |
| Cxcl14 reverse | CACCCTATTCTTCGTAGACC |
| Ccr5 forward | GTTGTTTTGGAGAACGCCCC |
| Ccr5 reverse | CAACACTGCTCCGAAACTGC |
| Il7 forward | CTAGCAACTGGCAAGGAGGAC |
| Il7 reverse | CCTGTAAGTGGAAGCATGGC |
| β-actin forward | ACTGGAACGGTGAAGGTGAC |
| β-actin reverse | AGAGAAGTGGGGTGGCTTTT |
Tab.1 Primer sequences for RT-qPCR
| Gene | Sequence (5′-3′) |
|---|---|
| Cx3cl1 forward | CAGAGGAGCAGGCAGGACAG |
| Cx3cl1 reverse | CTTCAGAGCAGGAGAGACCCATC |
| Cxcl14 forward | TCCGGTCAGCATGAGGCTCC |
| Cxcl14 reverse | CACCCTATTCTTCGTAGACC |
| Ccr5 forward | GTTGTTTTGGAGAACGCCCC |
| Ccr5 reverse | CAACACTGCTCCGAAACTGC |
| Il7 forward | CTAGCAACTGGCAAGGAGGAC |
| Il7 reverse | CCTGTAAGTGGAAGCATGGC |
| β-actin forward | ACTGGAACGGTGAAGGTGAC |
| β-actin reverse | AGAGAAGTGGGGTGGCTTTT |
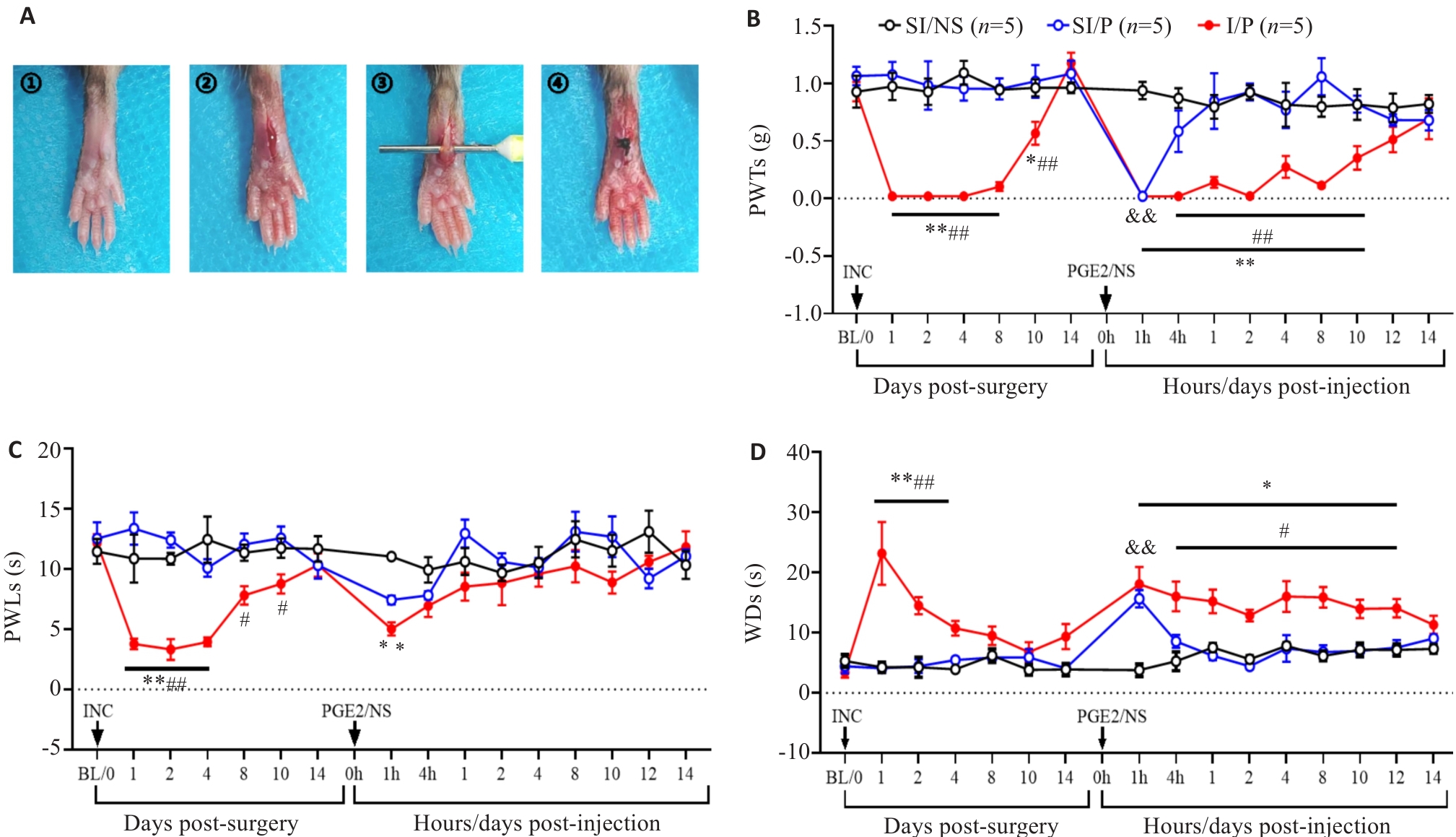
Fig.1 Temporal changes of pain-related behaviors in the mouse models of chronic postsurgical pain (CPSP). A: Schematic diagram of plantar incision for inducing CPSP in mice. B: Changes in mechanical paw withdrawal thresholds (PWTs) after plantar incision and after PGE2 injection in each group. C: Changes in thermal paw withdrawal latencies (PWLs) after plantar incision and after PGE2 injection in each group. D: Changes in cold withdrawal durations (WDs) of the mice after plantar incision and after PGE2 injection. INC: Incision. *P<0.05, **P<0.01 I/P vs SI/NS; #P<0.05, ##P<0.01 I/P vs SI/P; &&P<0.01 SI/P vs SI/NS.
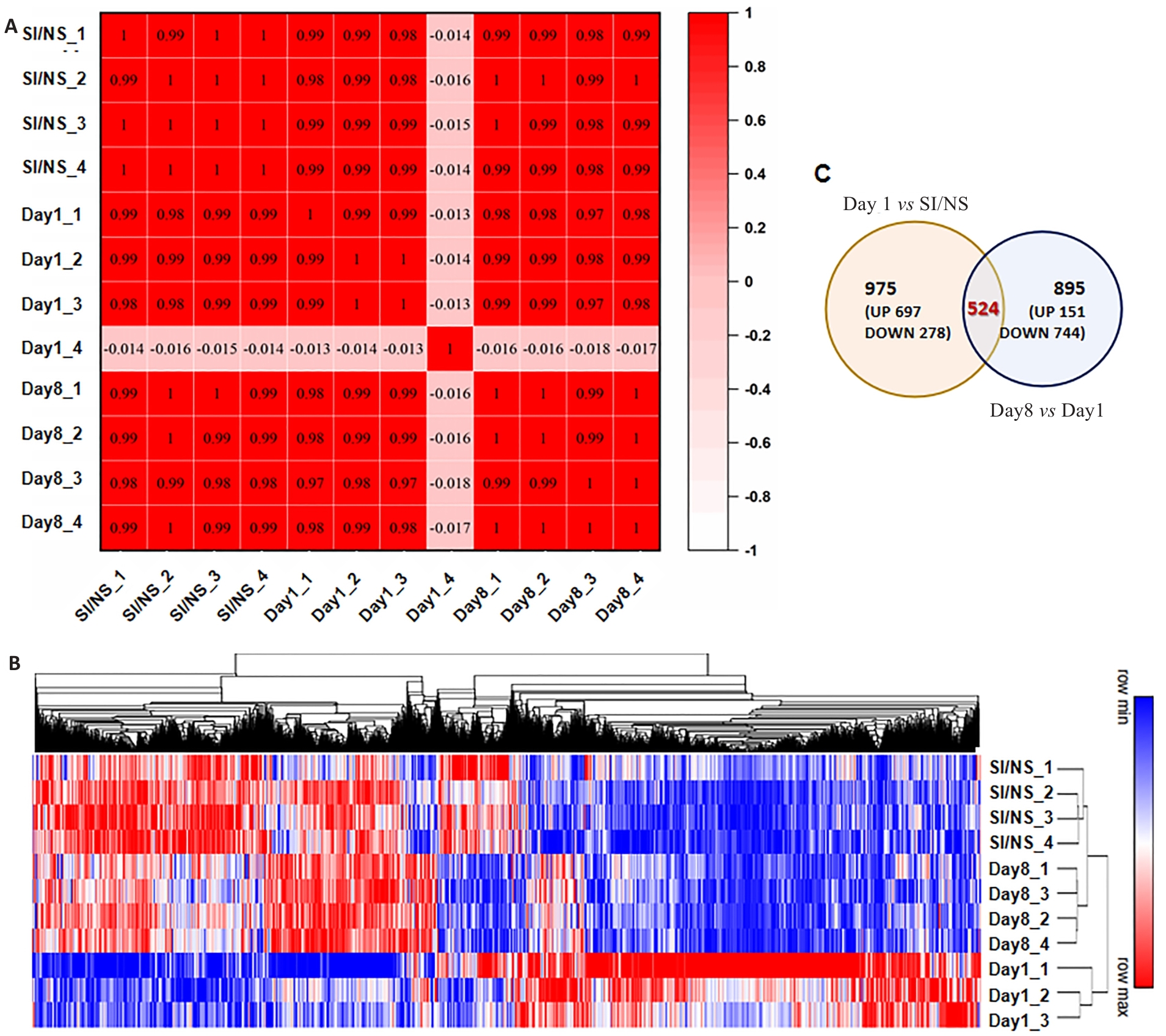
Fig.2 Gene expression profile in dorsal root ganglion (DRGs) of the mice with CPSP at different time points. A: Heat map of correlation coefficient of each sample (Numbers in the box are Pearson correlation coefficients between the corresponding two samples). B: Heat map and hierarchical clustering of differential gene expression in each sample (P<0.05 and |log2FC|>0.3 were the threshold criteria for differentially expressed genes). C: Venn diagram of DEGs between groups.
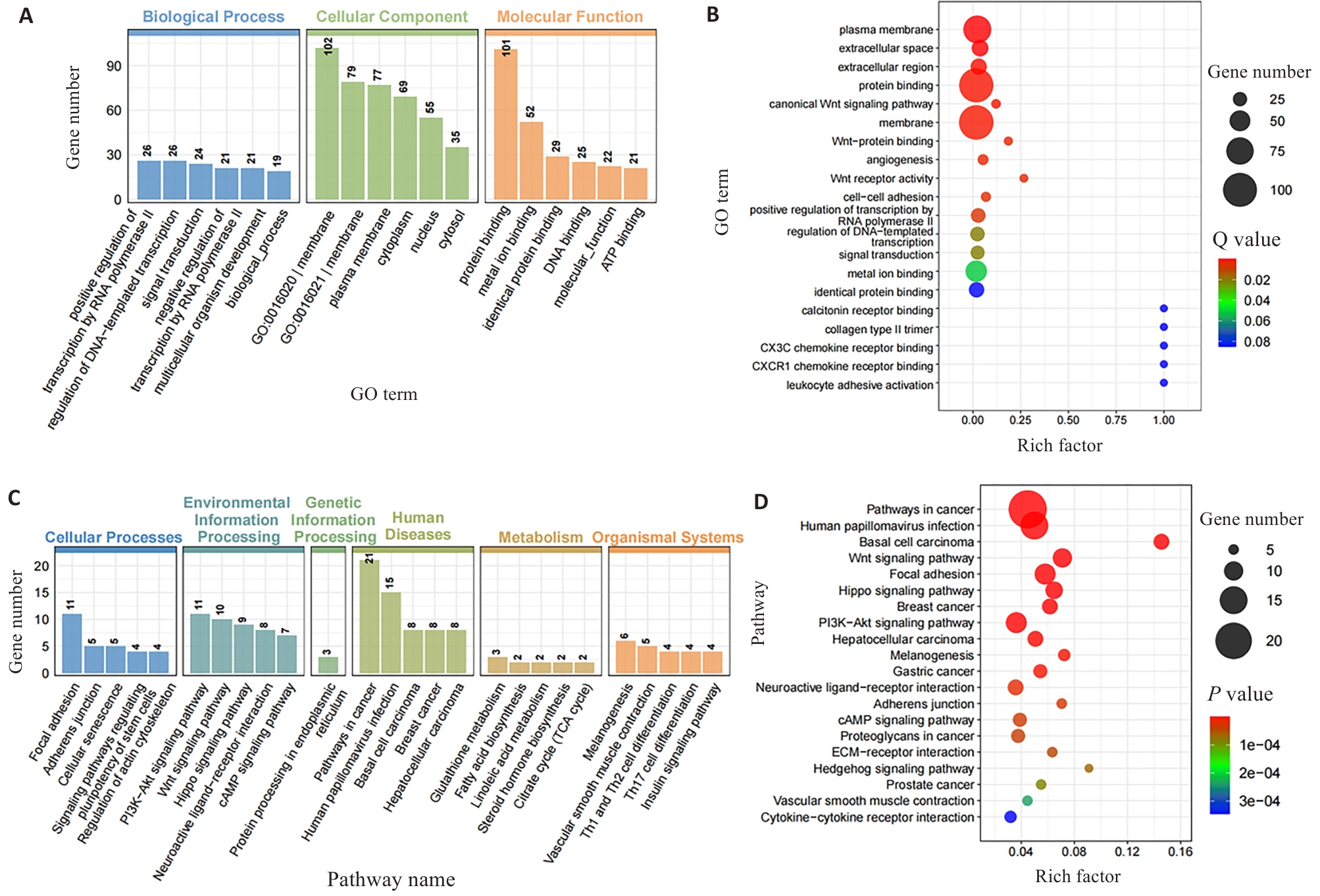
Fig.3 GO and KEGG enrichment analysis of differentially expressed genes at the intersection DEGs in CPSP mice. A: GO enrichment bar chart of the intersection DEGs between Day1vs. SI/NS and Day8 vs. Day1 (Ranked by the number of significantly enriched genes). B: GO enrichment scatter plot of intersection DEGs. C: KEGG enrichment bar chart of intersection DEGs. D: KEGG enrichment scatter plot of intersection DEGs.
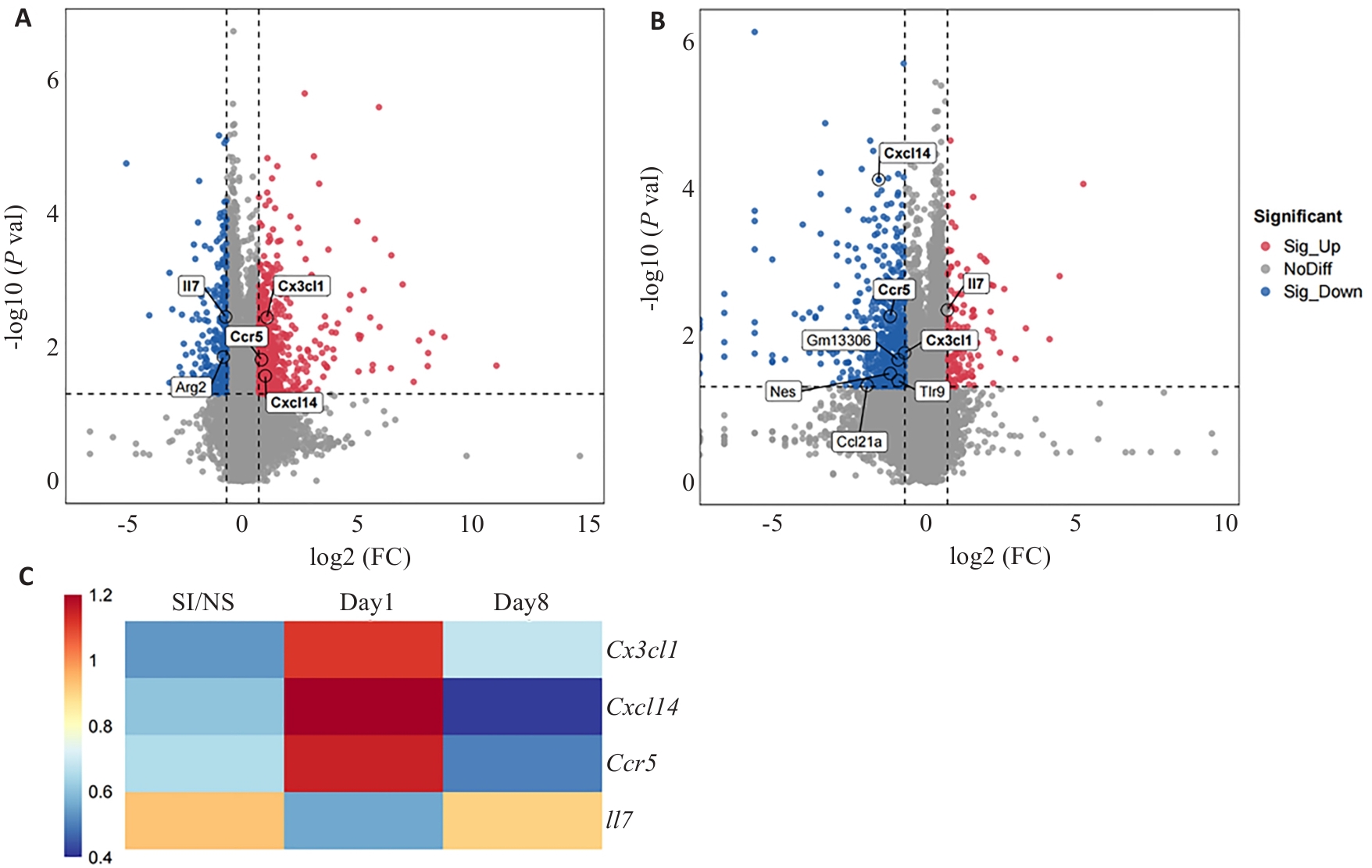
Fig.4 Expression of chemokine-related genes in DRGs of mice with CPSP at different time points. A: Volcano plot of differentially expressed genes in day 1 and SI/NS groups (Chemokine-related genes are marked). B: Volcano plot of differentially expressed genes in day 8 and day 1 groups. C: Table of differential genes associated with chemokines between the groups. All chemokine-related genes are extracted using GO terms.
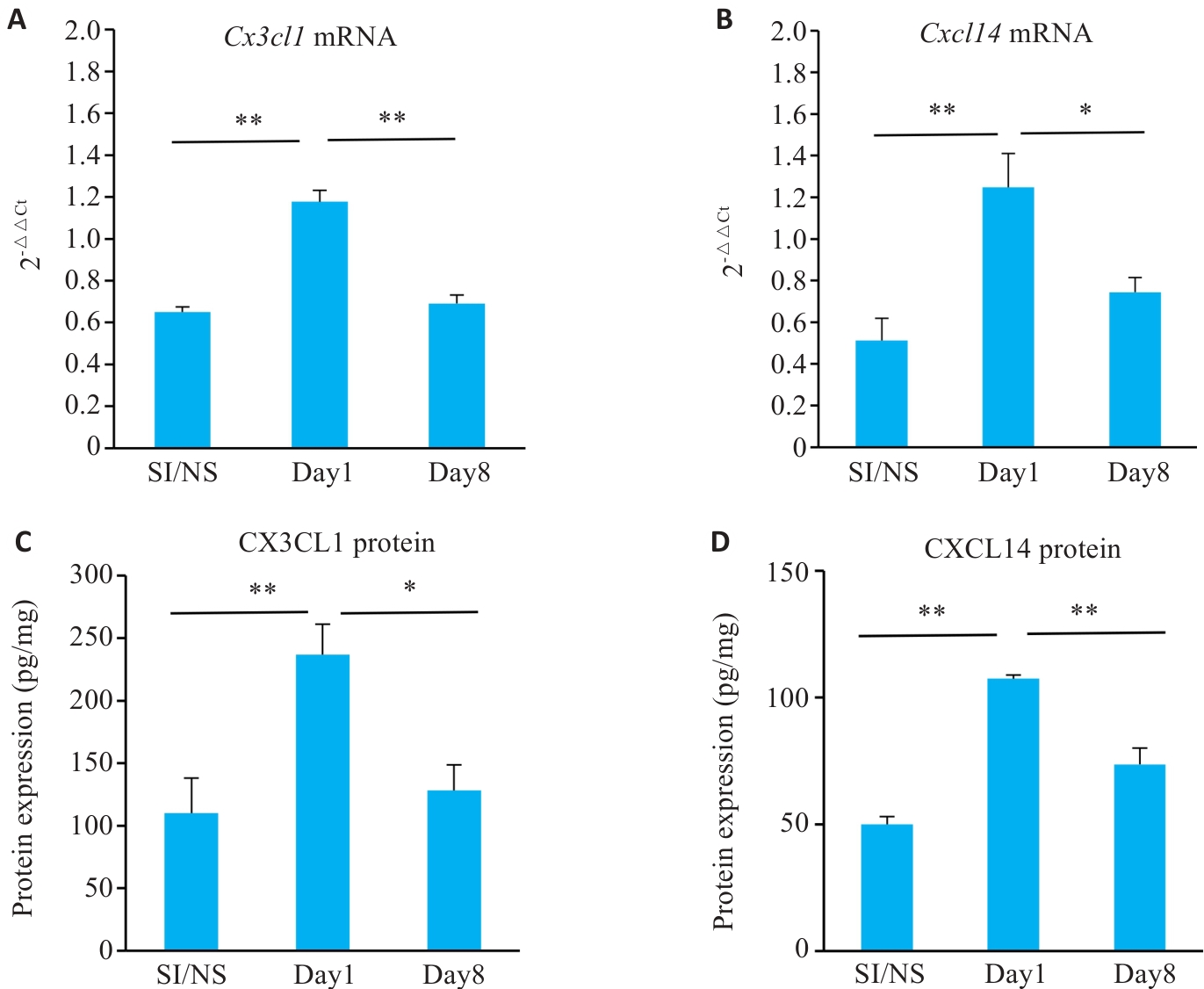
Fig.5 Gene and protein expression of Cx3c11 and Cxc114 in different stages of CPSP. A: Cx3cl1 mRNA expression levels in ipsilateral DRGs of the mice at each time point. B: Cxcl14 mRNA expression levels in ipsilateral DRGs of the mice at each time point. C: CX3CL1 protein expression in ipsilateral DRGs of the mice at each time point. D: CXCL14 protein expression in ipsilateral DRGs of the mice at each time point. *P<0.05, **P<0.01.
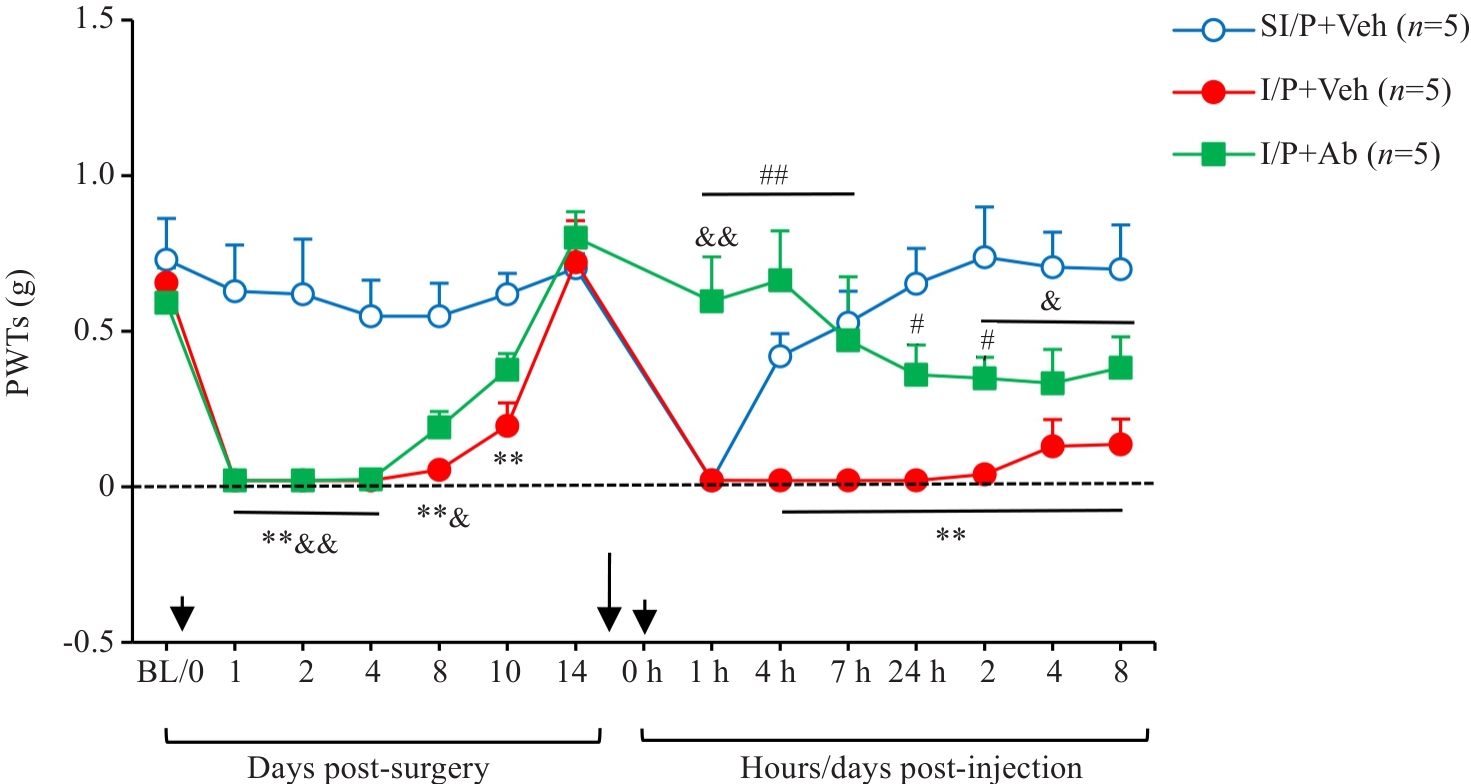
Fig.6 Intrathecal injection of CX3CL1 neutralizing antibody (5 µg/10 µL) 10 min prior to PGE2 injection significantly modulates mechanical PWTs in INC/PGE2 mice. **P<0.01 I/P+Veh vs SI/P+Veh group; #P<0.05, ##P<0.01 I/P+Ab vs I/P+Veh group; &P<0.05, &&P<0.01 I/P+Ab vs SI/P+Veh group. Ab: CX3CL1-neutralizing antibody; Veh: Vehicle, goat IgG control (1 µL/10 µL).
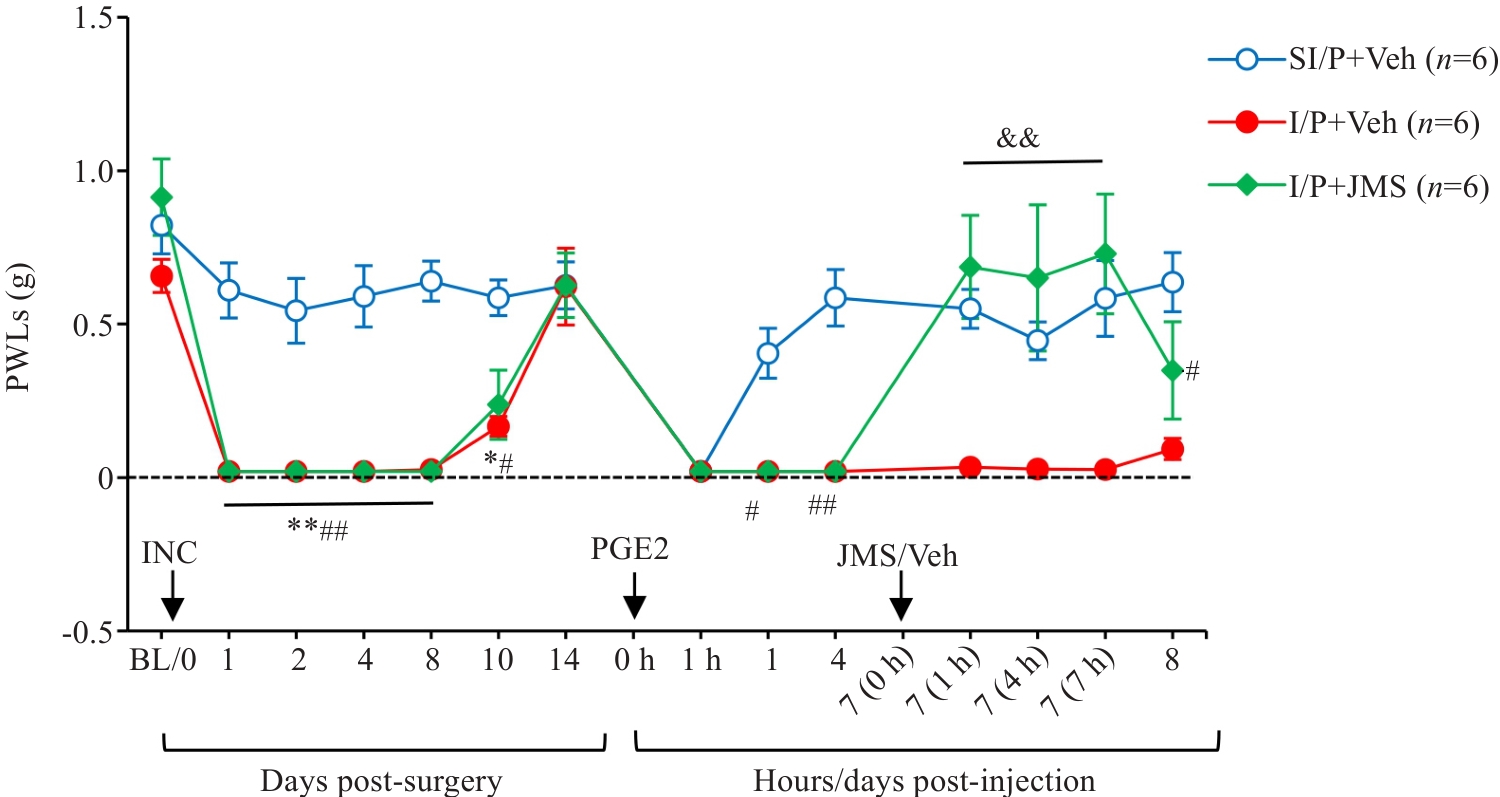
Fig.7 Effects of intrathecal injection of JMS17-2 (75 µg/10 µL), a selective CX3CR1 antagonist, on Day 7 post-PGE2 injection, on PWTs in CPSP mice. *P<0.05, **P<0.01 I/P+Veh vs SI/P+Veh; #P<0.05, ##P<0.01 I/P+JMS vs SI/P+Veh; &&P<0.01 I/P+JMS vs I/P+Veh. I/P: INC/PGE2; SI/P: Sham INC/PGE2; JMS: CX3CR1-selective antagonist JMS17-2; Veh: Corn oil vehicle.
| [1] | 冯 艺, 许军军, 林夏清, 等. 慢性术后或创伤后疼痛[J]. 中国疼痛医学杂志, 2021, 27(4): 241-5. |
| [2] | Fletcher D, Stamer UM, Pogatzki-Zahn E, et al. Chronic postsurgical pain in Europe: an observational study[J]. Eur J Anaesthesiol, 2015, 32(10): 725-34. doi:10.1097/eja.0000000000000319 |
| [3] | 金菊英, 彭丽桦, 杜洵松, 等. 手术后慢性疼痛的流行病学调查和危险因素分析[J]. 中国疼痛医学杂志, 2015, 21(7): 505-12. |
| [4] | 韩 琦, 冯 艺. 术后急、慢性疼痛危险因素研究进展[J]. 中国疼痛医学杂志, 2020, 26(11): 849-53. |
| [5] | Richebé P, Capdevila X, Rivat C. Persistent postsurgical pain: pathophysiology and preventative pharmacologic considerations[J]. Anesthesiology, 2018, 129(3): 590-607. doi:10.1097/aln.0000000000002238 |
| [6] | Inyang KE, Burton MD, Szabo-Pardi T, et al. Indirect AMP-activated protein kinase activators prevent incision-induced hyperalgesia and block hyperalgesic priming, whereas positive allosteric modulators block only priming in mice[J]. J Pharmacol Exp Ther, 2019, 371(1): 138-50. doi:10.1124/jpet.119.258400 |
| [7] | Pogatzki EM, Raja SN. A mouse model of incisional pain[J]. Anesthesiology, 2003, 99(4): 1023-7. doi:10.1097/00000542-200310000-00041 |
| [8] | Xu JJ, Gao P, Wu Y, et al. G protein-coupled estrogen receptor in the rostral ventromedial medulla contributes to the chronification of postoperative pain[J]. CNS Neurosci Ther, 2021, 27(11): 1313-26. doi:10.1111/cns.13704 |
| [9] | Kehlet H, Jensen TS, Woolf CJ. Persistent postsurgical pain: risk factors and prevention[J]. Lancet, 2006, 367(9522): 1618-25. doi:10.1016/s0140-6736(06)68700-x |
| [10] | Tillu DV, Melemedjian OK, Asiedu MN, et al. Resveratrol engages AMPK to attenuate ERK and mTOR signaling in sensory neurons and inhibits incision-induced acute and chronic pain[J]. Mol Pain, 2012, 8: 5. doi:10.1186/1744-8069-8-5 |
| [11] | 甄思佳, 赵 贝, 郑博习, 等. 背根神经节嘌呤受体亚型P2X3R介导小鼠术后急—慢痛转化[J]. 中国药理学通报, 2023, 39(7): 1282-8. |
| [12] | Baptista-de-Souza D, Tavares-Ferreira D, Megat S, et al. Sex differences in the role of atypical PKC within the basolateral nucleus of the amygdala in a mouse hyperalgesic priming model[J]. Neurobiol Pain, 2020, 8: 100049. doi:10.1016/j.ynpai.2020.100049 |
| [13] | Guo ZB, Tang L, Wang LP, et al. The analgesic effects of ulinastatin either as a single agent or in combination with sufentanil: a novel therapeutic potential for postoperative pain[J]. Eur J Pharmacol, 2021, 907: 174267. doi:10.1016/j.ejphar.2021.174267 |
| [14] | Pak DJ, Yong RJ, Kaye AD, et al. Chronification of pain: mechanisms, current understanding, and clinical implications[J]. Curr Pain Headache Rep, 2018, 22(2): 9. doi:10.1007/s11916-018-0666-8 |
| [15] | Li CS, Yang Y, Liu SF, et al. Stress induces pain transition by potentiation of AMPA receptor phosphorylation[J]. J Neurosci, 2014, 34(41): 13737-46. doi:10.1523/jneurosci.2130-14.2014 |
| [16] | Banik RK, Woo YC, Park SS, et al. Strain and sex influence on pain sensitivity after plantar incision in the mouse[J]. Anesthesiology, 2006, 105(6): 1246-53. doi:10.1097/00000542-200612000-00025 |
| [17] | Chaplan SR, Bach FW, Pogrel JW, et al. Quantitative assessment of tactile allodynia in the rat paw[J]. J Neurosci Methods, 1994, 53(1): 55-63. doi:10.1016/0165-0270(94)90144-9 |
| [18] | Hargreaves K, Dubner R, Brown F, et al. A new and sensitive method for measuring thermal nociception in cutaneous hyperalgesia[J]. Pain, 1988, 32(1): 77-88. doi:10.1016/0304-3959(88)90026-7 |
| [19] | Yoon C, Wook YY, Sik NH, et al. Behavioral signs of ongoing pain and cold allodynia in a rat model of neuropathic pain[J]. Pain, 1994, 59(3): 369-76. doi:10.1016/0304-3959(94)90023-x |
| [20] | 张晓光, 郄文斌, 屠伟峰, 等. 围术期目标导向全程镇痛管理中国专家共识(2021版)[J]. 中华疼痛学杂志, 2021, 17(2): 119-25. |
| [21] | Brennan TJ, Vandermeulen EP, Gebhart GF. Characterization of a rat model of incisional pain[J]. Pain, 1996, 64(3): 493-502. doi:10.1016/0304-3959(95)01441-1 |
| [22] | Reichling DB, Levine JD. Critical role of nociceptor plasticity in chronic pain[J]. Trends Neurosci, 2009, 32(12): 611-8. doi:10.1016/j.tins.2009.07.007 |
| [23] | Sun Y, Sahbaie P, Liang DY, et al. Epigenetic regulation of spinal CXCR2 signaling in incisional hypersensitivity in mice[J]. Anesthesiology, 2013, 119(5): 1198-208. doi:10.1097/aln.0b013e31829ce340 |
| [24] | Sahbaie P, Sun Y, Liang DY, et al. Curcumin treatment attenuates pain and enhances functional recovery after incision[J]. Anesth Analg, 2014, 118(6): 1336-44. doi:10.1213/ane.0000000000000189 |
| [25] | Matsuda M, Oh-Hashi K, Yokota I, et al. Acquired exchange protein directly activated by cyclic adenosine monophosphate activity induced by p38 mitogen-activated protein kinase in primary afferent neurons contributes to sustaining postincisional nociception[J]. Anesthesiology, 2017, 126(1): 150-62. doi:10.1097/aln.0000000000001401 |
| [26] | 胡海宇, 丁家威, 吴叶琪, 等. 电针对痛觉敏化大鼠背根神经节蛋白酶激活受体2的影响[J]. 针刺研究, 2018, 43(1): 14-9. |
| [27] | Jiang BC, Liu T, Gao YJ. Chemokines in chronic pain: cellular and molecular mechanisms and therapeutic potential[J]. Pharmacol Ther, 2020, 212: 107581. doi:10.1016/j.pharmthera.2020.107581 |
| [28] | Subbarayan MS, Joly-Amado A, Bickford PC, et al. CX3CL1/CX3CR1 signaling targets for the treatment of neurodegenerative diseases[J]. Pharmacol Ther, 2022, 231: 107989. doi:10.1016/j.pharmthera.2021.107989 |
| [29] | Holmes FE, Arnott N, Vanderplank P, et al. Intra-neural administration of fractalkine attenuates neuropathic pain-related behaviour[J]. J Neurochem, 2008, 106(2): 640-9. doi:10.1111/j.1471-4159.2008.05419.x |
| [30] | Bian C, Wang ZC, Yang JL, et al. Up-regulation of interleukin-23 induces persistent allodynia via CX3CL1 and interleukin-18 signaling in the rat spinal cord after tetanic sciatic stimulation[J]. Brain Behav Immun, 2014, 37: 220-30. doi:10.1016/j.bbi.2013.12.011 |
| [31] | Souza GR, Talbot J, Lotufo CM, et al. Fractalkine mediates inflammatory pain through activation of satellite glial cells[J]. Proc Natl Acad Sci USA, 2013, 110(27): 11193-8. doi:10.1073/pnas.1307445110 |
| [32] | Gowhari Shabgah A, Haleem Al-Qaim Z, Markov A, et al. Chemokine CXCL14; a double-edged sword in cancer development[J]. Int Immunopharmacol, 2021, 97: 107681. doi:10.1016/j.intimp.2021.107681 |
| [33] | Westrich JA, Vermeer DW, Colbert PL, et al. The multifarious roles of the chemokine CXCL14 in cancer progression and immune responses[J]. Mol Carcinog, 2020, 59(7): 794-806. doi:10.1002/mc.23188 |
| [34] | Liu M, Zhang SB, Luo YX, et al. NFATc2-dependent epigenetic upregulation of CXCL14 is involved in the development of neuropathic pain induced by paclitaxel[J]. J Neuroinflammation, 2020, 17(1): 310. doi:10.1186/s12974-020-01992-1 |
| [35] | Wang YY, Weng XL, Wang LY, et al. HIC1 deletion promotes breast cancer progression by activating tumor cell/fibroblast crosstalk[J]. J Clin Invest, 2018, 128(12): 5235-50. doi:10.1172/jci99974 |
| [36] | Witte A, Rohlfing AK, Dannenmann B, et al. The chemokine CXCL14 mediates platelet function and migration via direct interaction with CXCR4[J]. Cardiovasc Res, 2021, 117(3): 903-17. doi:10.1093/cvr/cvaa080 |
| [37] | Chang TM, Chiang YC, Lee CW, et al. CXCL14 promotes metastasis of non-small cell lung cancer through ACKR2-depended signaling pathway[J]. Int J Biol Sci, 2023, 19(5): 1455-70. doi:10.7150/ijbs.79438 |
| [38] | Xu YY, Deng CZ, Chen HM, et al. Osteosarcoma cells secrete CXCL14 that activates integrin α11β1 on fibroblasts to form a lung metastatic niche[J]. Cancer Res, 2024, 84(7): 994-1012. doi:10.1158/0008-5472.can-23-1307 |
| [39] | Lu Y, Jiang BC, Cao DL, et al. Chemokine CCL8 and its receptor CCR5 in the spinal cord are involved in visceral pain induced by experimental colitis in mice[J]. Brain Res Bull, 2017, 135: 170-8. doi:10.1016/j.brainresbull.2017.10.009 |
| [40] | Zhong SS, Liu FX, Giniatullin R, et al. Blockade of CCR5 suppresses paclitaxel-induced peripheral neuropathic pain caused by increased deoxycholic acid[J]. Cell Rep, 2023, 42(11): 113386. doi:10.1016/j.celrep.2023.113386 |
| [41] | Jonsjö MA, Olsson GL, Wicksell RK, et al. The role of low-grade inflammation in ME/CFS (Myalgic Encephalomyelitis/Chronic Fatigue Syndrome)-associations with symptoms[J]. Psychoneuro-endocrinology, 2020, 113: 104578. doi:10.1016/j.psyneuen.2019.104578 |
| [1] | WU Ruojie, LIU Rui, ZHANG Yisu, LI Xiaohong. Parecoxib sodium down-regulates CXCL8-CXCR1/2 to improve inflammatory microenvironment and promote patient recovery following laparoscopic radical resection of rectal cancer [J]. Journal of Southern Medical University, 2024, 44(2): 363-369. |
| [2] | LAN Yu, WANG Kaifeng, LAN Zhixian, ZHOU Heqi, SUN Jian. Dealcoholized red wine inhibits occurrence and progression of hepatocellular carcinoma possibly by inducing cell cycle arrest and apoptosis [J]. Journal of Southern Medical University, 2023, 43(8): 1297-1305. |
| [3] | . Di (2-ethylhexyl) phthalate-induced hypospadias in SD rats is related with Mafb expression: a transcriptome profiling-based study [J]. Journal of Southern Medical University, 2019, 39(04): 456-. |
| [4] | . Dexmedetomidine alleviates cognitive dysfunction induced by tibial fracture in rats [J]. Journal of Southern Medical University, 2019, 39(03): 292-. |
| [5] | . Role of stromal cell-derived factor-1 and CXC chemokine receptor 4 in corneal graft rejection in rats [J]. Journal of Southern Medical University, 2016, 36(12): 1677-. |
| [6] | . Expression of chemokine receptor CXCR7 in gastric cancer tissues and cell lines [J]. Journal of Southern Medical University, 2014, 34(12): 1780-. |
| [7] | . Oleanolic acid synergizes with cyclosporine A to prolong renal allograft survival in rats [J]. Journal of Southern Medical University, 2014, 34(06): 843-. |
| [8] | . Expression of chemokine CXCL14 in primary osteosarcoma and its association with prognosis [J]. Journal of Southern Medical University, 2013, 33(06): 798-. |
| [9] | ZHNA Jin-hong1,WANG Jian1,JIANG Shui-qing2,XIANG Gui-ju2 1Department of Etiology and Immunology,Medical College of Anhui University of Science and Technology,Huainan 232001,China;2Department of Infectious Diseases,Second Worker’s Hospital of Huainan,Huainan 232057,China. Expression of chemokine monokine induced by interferon-γ in patients with chronic hepatitis B [J]. Journal of Southern Medical University, 2006, 26(11): 1589-1592. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||