Journal of Southern Medical University ›› 2024, Vol. 44 ›› Issue (12): 2375-2381.doi: 10.12122/j.issn.1673-4254.2024.12.13
Jiaxin JIN1( ), Pengzhen MA2, Eryu WANG1, Yingzhen XIE1(
), Pengzhen MA2, Eryu WANG1, Yingzhen XIE1( )
)
Received:2024-07-30
Online:2024-12-20
Published:2024-12-26
Contact:
Yingzhen XIE
E-mail:614522903@qq.com;xyz_3191@aliyun.com
Jiaxin JIN, Pengzhen MA, Eryu WANG, Yingzhen XIE. Risk factors of recurrence of acute ischemic stroke and construction of a nomogram model for predicting the recurrence risk based on Lasso Regression[J]. Journal of Southern Medical University, 2024, 44(12): 2375-2381.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2024.12.13
| Characteristics | Recurrence group (n=28) | Non-recurrence group (n=156) | t/χ2 /Z | P |
|---|---|---|---|---|
| Gender(n) | 0.000 | 0.992 | ||
| Male | 19 | 106 | ||
| Female | 9 | 50 | ||
| Age>65 years [n (%)] | 22 (78.6%) | 72 (46.2%) | 9.984 | 0.002 |
| Smoking [n (%)] | 12 (42.9%) | 78 (50.0%) | 0.485 | 0.486 |
| Alcohol abuse [n (%)] | 7 (25.0%) | 65 (41.7%) | 2.769 | 0.096 |
| Stroke [n (%)] | 7 (25.0%) | 42 (26.9%) | 0.045 | 0.832 |
| HBP [n (%)] | 19 (67.9%) | 116 (74.4%) | 0.514 | 0.474 |
| DM [n (%)] | 20 (71.4%) | 71 (45.5%) | 6.378 | 0.012 |
| CHD [n (%)] | 14 (50.0%) | 51 (32.7%) | 3.113 | 0.078 |
| Arrhythmia [n (%)] | 10 (35.7%) | 26 (16.7%) | 5.473 | 0.019 |
| Hyperlipemia [n (%)] | 11 (39.3%) | 87 (55.8%) | 2.591 | 0.107 |
| Hyperuricemia [n (%)] | 7 (25.0%) | 36 (23.1%) | 0.049 | 0.825 |
| Atherosclerosis [n (%)] | 21 (75.0%) | 134 (85.9%) | 2.123 | 0.161 |
| Constipation after stroke [n (%)] | 15 (53.6%) | 38 (24.4%) | 9.825 | 0.002 |
| Anxiety state [n (%)] | 8 (28.6%) | 22 (14.1%) | 3.642 | 0.090 |
| Family history of stroke [n (%)] | 7 (25.0%) | 41 (26.3%) | 0.020 | 0.887 |
| Family history of HBP [n (%)] | 11 (39.3%) | 44 (28.2%) | 1.391 | 0.238 |
| Family history of CHD [n (%)] | 4 (14.3%) | 19 (12.2%) | 0.096 | 0.756 |
| NIHSS (Mean±SD) | 4.18±4.68 | 3.31±3.25 | -0.726 | 0.468 |
| CISS [n (%)] | ||||
| LAA | 11 (39.3%) | 60 (38.5%) | 2.478 | 0.479 |
| CS | 3 (10.7%) | 7 (4.5%) | ||
| PAD | 12 (42.9%) | 82 (52.6%) | ||
| UE | 2 (7.1%) | 7 (4.5%) | ||
| WBC (×109/L, Mean±SD) | 8.03±3.72 | 7.41±2.14 | -0.528 | 0.597 |
| NE (×109/L, Mean±SD) | 5.84±3.39 | 5.07±1.89 | -1.152 | 0.249 |
| LY (×109/L, Mean±SD) | 1.57±0.78 | 1.71±0.66 | -1.372 | 0.170 |
| CRP (mg/L, Mean±SD) | 8.66±24.46 | 2.02±4.59 | -0.596 | 0.551 |
| NLR (Mean±SD) | 4.51±3.58 | 3.39±1.93 | -2.104 | 0.035 |
| PNR (Mean±SD) | 43.36±16.23 | 50.62±21.05 | -1.534 | 0.125 |
| SII (Mean±SD) | 1094.18±1207.77 | 778.59±508.24 | -1.303 | 0.193 |
| TyG (Mean±SD) | 1.77±0.77 | 1.61±0.73 | -1.403 | 0.161 |
| FBG>7.5 (mmol/L) | 16 (57.1%) | 39 (25%) | 11.704 | <0.001 |
| UREA (mmol/L, Mean±SD) | 6.20±1.97 | 5.19±1.62 | -2.848 | 0.044 |
| Cr (μmol/L, Mean±SD) | 78.50±23.32 | 67.50±15.50 | -2.198 | 0.028 |
| ALP (U/L, Mean±SD) | 85.90±24.46 | 78.93±21.82 | -1.486 | 0.137 |
| TC (mmol/L, Mean±SD) | 4.39±1.25 | 4.49±1.04 | -0.450 | 0.653 |
| TG (mmol/L, Mean±SD) | 1.52±0.69 | 1.80±1.10 | -0.698 | 0.485 |
| HDL-C (mmol/L, Mean±SD) | 1.05±0.21 | 1.07±0.26 | -0.245 | 0.807 |
| LDL-C (mmol/L, Mean±SD) | 2.69±0.94 | 2.73±0.78 | -0.219 | 0.827 |
| Hcy (μmol/L, Mean±SD) | 15.18±7.20 | 17.91±14.06 | -0.511 | 0.610 |
| HbA1c (%, Mean±SD) | 7.35±1.61 | 6.70±1.38 | -2.090 | 0.037 |
| APTT (S, Mean±SD) | 30.45±2.20 | 30.02±4.59 | -1.725 | 0.085 |
| FIB (g/L, Mean±SD) | 3.40±0.64 | 3.47±4.40 | -2.048 | 0.041 |
| TT (S, Mean±SD) | 15.24±1.26 | 15.23±6.38 | -2.265 | 0.023 |
| D-D (μg/L, Mean±SD) | 206.64±226.89 | 166.19±278.68 | -1.883 | 0.060 |
Tab.1 Comparison of general data between recurrence group and non-recurrence group
| Characteristics | Recurrence group (n=28) | Non-recurrence group (n=156) | t/χ2 /Z | P |
|---|---|---|---|---|
| Gender(n) | 0.000 | 0.992 | ||
| Male | 19 | 106 | ||
| Female | 9 | 50 | ||
| Age>65 years [n (%)] | 22 (78.6%) | 72 (46.2%) | 9.984 | 0.002 |
| Smoking [n (%)] | 12 (42.9%) | 78 (50.0%) | 0.485 | 0.486 |
| Alcohol abuse [n (%)] | 7 (25.0%) | 65 (41.7%) | 2.769 | 0.096 |
| Stroke [n (%)] | 7 (25.0%) | 42 (26.9%) | 0.045 | 0.832 |
| HBP [n (%)] | 19 (67.9%) | 116 (74.4%) | 0.514 | 0.474 |
| DM [n (%)] | 20 (71.4%) | 71 (45.5%) | 6.378 | 0.012 |
| CHD [n (%)] | 14 (50.0%) | 51 (32.7%) | 3.113 | 0.078 |
| Arrhythmia [n (%)] | 10 (35.7%) | 26 (16.7%) | 5.473 | 0.019 |
| Hyperlipemia [n (%)] | 11 (39.3%) | 87 (55.8%) | 2.591 | 0.107 |
| Hyperuricemia [n (%)] | 7 (25.0%) | 36 (23.1%) | 0.049 | 0.825 |
| Atherosclerosis [n (%)] | 21 (75.0%) | 134 (85.9%) | 2.123 | 0.161 |
| Constipation after stroke [n (%)] | 15 (53.6%) | 38 (24.4%) | 9.825 | 0.002 |
| Anxiety state [n (%)] | 8 (28.6%) | 22 (14.1%) | 3.642 | 0.090 |
| Family history of stroke [n (%)] | 7 (25.0%) | 41 (26.3%) | 0.020 | 0.887 |
| Family history of HBP [n (%)] | 11 (39.3%) | 44 (28.2%) | 1.391 | 0.238 |
| Family history of CHD [n (%)] | 4 (14.3%) | 19 (12.2%) | 0.096 | 0.756 |
| NIHSS (Mean±SD) | 4.18±4.68 | 3.31±3.25 | -0.726 | 0.468 |
| CISS [n (%)] | ||||
| LAA | 11 (39.3%) | 60 (38.5%) | 2.478 | 0.479 |
| CS | 3 (10.7%) | 7 (4.5%) | ||
| PAD | 12 (42.9%) | 82 (52.6%) | ||
| UE | 2 (7.1%) | 7 (4.5%) | ||
| WBC (×109/L, Mean±SD) | 8.03±3.72 | 7.41±2.14 | -0.528 | 0.597 |
| NE (×109/L, Mean±SD) | 5.84±3.39 | 5.07±1.89 | -1.152 | 0.249 |
| LY (×109/L, Mean±SD) | 1.57±0.78 | 1.71±0.66 | -1.372 | 0.170 |
| CRP (mg/L, Mean±SD) | 8.66±24.46 | 2.02±4.59 | -0.596 | 0.551 |
| NLR (Mean±SD) | 4.51±3.58 | 3.39±1.93 | -2.104 | 0.035 |
| PNR (Mean±SD) | 43.36±16.23 | 50.62±21.05 | -1.534 | 0.125 |
| SII (Mean±SD) | 1094.18±1207.77 | 778.59±508.24 | -1.303 | 0.193 |
| TyG (Mean±SD) | 1.77±0.77 | 1.61±0.73 | -1.403 | 0.161 |
| FBG>7.5 (mmol/L) | 16 (57.1%) | 39 (25%) | 11.704 | <0.001 |
| UREA (mmol/L, Mean±SD) | 6.20±1.97 | 5.19±1.62 | -2.848 | 0.044 |
| Cr (μmol/L, Mean±SD) | 78.50±23.32 | 67.50±15.50 | -2.198 | 0.028 |
| ALP (U/L, Mean±SD) | 85.90±24.46 | 78.93±21.82 | -1.486 | 0.137 |
| TC (mmol/L, Mean±SD) | 4.39±1.25 | 4.49±1.04 | -0.450 | 0.653 |
| TG (mmol/L, Mean±SD) | 1.52±0.69 | 1.80±1.10 | -0.698 | 0.485 |
| HDL-C (mmol/L, Mean±SD) | 1.05±0.21 | 1.07±0.26 | -0.245 | 0.807 |
| LDL-C (mmol/L, Mean±SD) | 2.69±0.94 | 2.73±0.78 | -0.219 | 0.827 |
| Hcy (μmol/L, Mean±SD) | 15.18±7.20 | 17.91±14.06 | -0.511 | 0.610 |
| HbA1c (%, Mean±SD) | 7.35±1.61 | 6.70±1.38 | -2.090 | 0.037 |
| APTT (S, Mean±SD) | 30.45±2.20 | 30.02±4.59 | -1.725 | 0.085 |
| FIB (g/L, Mean±SD) | 3.40±0.64 | 3.47±4.40 | -2.048 | 0.041 |
| TT (S, Mean±SD) | 15.24±1.26 | 15.23±6.38 | -2.265 | 0.023 |
| D-D (μg/L, Mean±SD) | 206.64±226.89 | 166.19±278.68 | -1.883 | 0.060 |
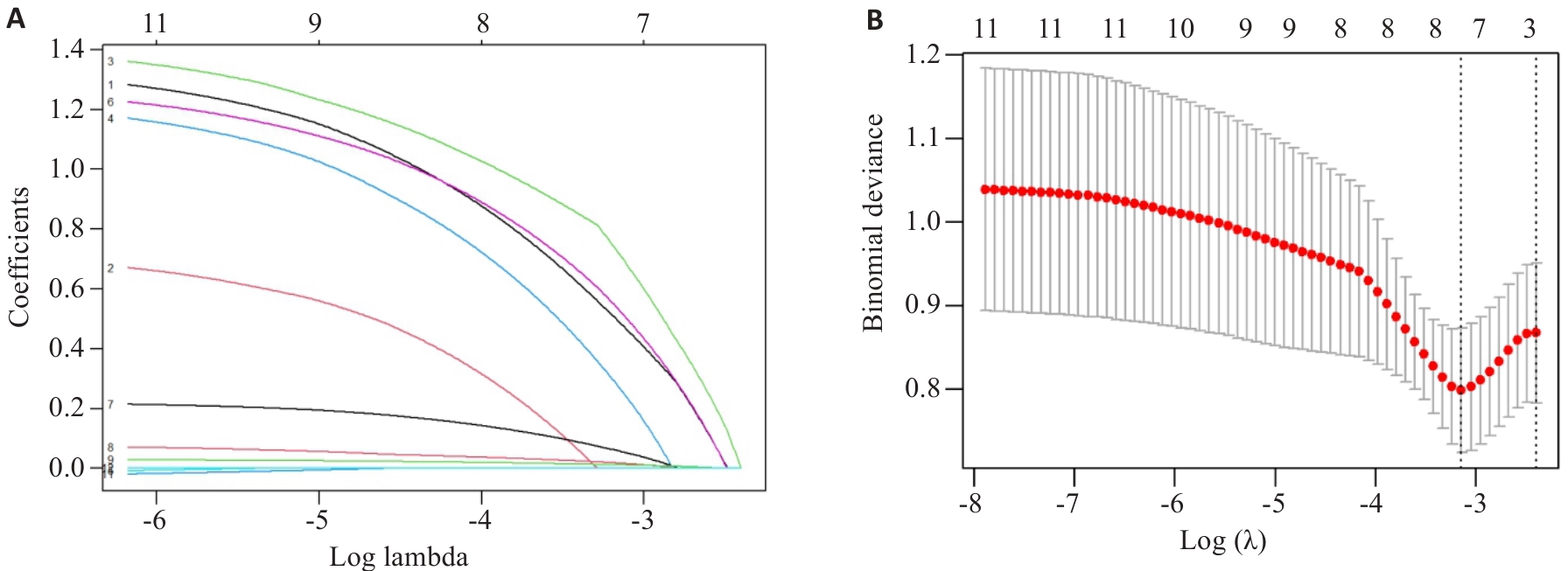
Fig.1 Clinical feature selection using Lasso regression. A: Lasso coefficients for 11 clinical features. B: Ten-fold cross-validation of the Lasso regression model.
| Variate | β | SE | Wald χ2 | OR (95% CI) | P |
|---|---|---|---|---|---|
| Age>65 years | 1.374 | 0.571 | 5.790 | 3.951 (1.290-12.098) | 0.016 |
| Arrhythmia | 1.208 | 0.568 | 4.526 | 3.348 (1.100-10.194) | 0.033 |
| Constipation after stroke | 1.325 | 0.504 | 6.913 | 3.762 (1.401-10.101) | 0.009 |
| NLR | 0.219 | 0.088 | 6.186 | 1.244 (1.047-1.479) | 0.013 |
| FBG>7.5 | 1.851 | 0.533 | 12.069 | 1.035 (1.008-1.063) | <0.001 |
| Cr | 0.034 | 0.014 | 6.374 | 6.366 (2.241-18.088) | 0.012 |
Tab.2 Multivariate Logistic regression analysis of the factors affecting recurrence in acute ischemic stroke patients
| Variate | β | SE | Wald χ2 | OR (95% CI) | P |
|---|---|---|---|---|---|
| Age>65 years | 1.374 | 0.571 | 5.790 | 3.951 (1.290-12.098) | 0.016 |
| Arrhythmia | 1.208 | 0.568 | 4.526 | 3.348 (1.100-10.194) | 0.033 |
| Constipation after stroke | 1.325 | 0.504 | 6.913 | 3.762 (1.401-10.101) | 0.009 |
| NLR | 0.219 | 0.088 | 6.186 | 1.244 (1.047-1.479) | 0.013 |
| FBG>7.5 | 1.851 | 0.533 | 12.069 | 1.035 (1.008-1.063) | <0.001 |
| Cr | 0.034 | 0.014 | 6.374 | 6.366 (2.241-18.088) | 0.012 |
| 1 | 《中国脑卒中防治报告》编写组. 《中国脑卒中防治报告2019》概要[J]. 中国脑血管病杂志, 2020, 17(5): 272-81. |
| 2 | 《中国脑卒中防治报告》编写组, 王陇德. 《中国脑卒中防治报告2021》概要[J]. 中国脑血管病杂志, 2023, 20(11): 783-92, 封3. |
| 3 | Modrego PJ, Pina MA, Fraj MM, et al. Type, causes, and prognosis of stroke recurrence in the province of Teruel, Spain. A 5-year analysis[J]. Neurol Sci, 2000, 21(6): 355-60. |
| 4 | Hardie K, Hankey GJ, Jamrozik K, et al. Ten-year risk of first recurrent stroke and disability after first-ever stroke in the Perth Community Stroke Study[J]. Stroke, 2004, 35(3): 731-5. |
| 5 | Hankey GJ. Secondary stroke prevention[J]. Lancet Neurol, 2014, 13(2): 178-94. |
| 6 | Mao C, Li MF. Stroke recurrence as a challenge for countries[J]. JAMA Netw Open, 2022, 5(6): e2219698. |
| 7 | 谷鸿秋, 杨凯璇, 姜英玉, 等. 缺血性卒中患者卒中复发风险预测模型研究进展及展望[J]. 中国卒中杂志, 2023, 18(7): 731-9. |
| 8 | 王桂倩, 谢雁鸣, 易丹辉, 等. 基于体质的缺血性中风病复发风险评估模型建立研究[J]. 中华中医药杂志, 2019, 34(10): 4860-6. |
| 9 | Zhuo YY, Wu JM, Qu YM, et al. Comparison of Prediction Models based on Risk Factors and Retinal Characteristics Associated with Recurrence One Year after Ischemic Stroke[J]. J Stroke Cerebrovasc Dis, 2020, 29(4): 104581. |
| 10 | 刘岚予, 贾晓静. 缺血性脑卒中90d复发预测模型的构建[J]. 北华大学学报: 自然科学版, 2021, 22(6): 779-83. |
| 11 | Pezzini A, Grassi M, Lodigiani C, et al. Predictors of long-term recurrent vascular events after ischemic stroke at young age: the Italian Project on Stroke in Young Adults[J]. Circulation, 2014, 129(16): 1668-76. |
| 12 | 安雅臣, 程 焱, 王玉浔, 等. 缺血性脑卒中3年复发危险因素的Cox回归分析及预测模型的构建[J].中华行为医学与脑科学杂志, 2017, 26(6):544-8. |
| 13 | 蔺雪梅, 王 芳, 王 静, 等. 西安地区卒中患者1年卒中复发预测模型的构建[J]. 中国卒中杂志, 2020, 15(1): 33-9. |
| 14 | Yuan K, Chen JJ, Xu PF, et al. A nomogram for predicting stroke recurrence among young adults[J]. Stroke, 2020, 51(6): 1865-7. |
| 15 | 刘 瑾, 杨燕玲, 严 可, 等. 列线图可预测首发缺血性脑卒中患者的复发[J]. 南方医科大学学报, 2022, 42(1): 130-6. |
| 16 | 周娟娟, 王翠琴, 朱胜康, 等. 缺血性脑卒中复发的影响因素及其预测模型构建: 基于五年的随访数据[J]. 实用心脑肺血管病杂志, 2022, 30(2): 13-7. |
| 17 | 陈思玎, 姜英玉, 王春娟, 等. 缺血性卒中患者院内复发风险预测模型开发与验证研究[J]. 中国卒中杂志, 2023, 18(12): 1397-404. |
| 18 | 莫秋红, 丁晓波, 张岩波, 等. 随机森林和决策树模型在轻型缺血性脑卒中患者复发预测中的应用分析[J]. 神经疾病与精神卫生, 2024, 24(2): 77-82. |
| 19 | Wu CX, Xu ZR, Wang QZ, et al. Development, validation, and visualization of a novel nomogram to predict stroke risk in patients[J]. Front Aging Neurosci, 2023, 15: 1200810. |
| 20 | Tang M, Gao J, Ma NE, et al. Radiomics nomogram for predicting stroke recurrence in symptomatic intracranial atherosclerotic stenosis[J]. Front Neurosci, 2022, 16: 851353. |
| 21 | Drossman DA. The functional gastrointestinal disorders and the Rome III process[J]. Gastroenterology, 2006, 130(5): 1377-90. |
| 22 | Zhou MG, Wang HD, Zeng XY, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017[J]. Lancet, 2019, 394(10204): 1145-58. |
| 23 | Kamouchi M, Kumagai N, Okada Y, et al. Risk score for predicting recurrence in patients with ischemic stroke: the Fukuoka stroke risk score for Japanese[J]. Cerebrovasc Dis, 2012, 34(5/6): 351-7. |
| 24 | Diener HC, Ringleb PA, Savi P. Clopidogrel for the secondary prevention of stroke[J]. Expert Opin Pharmacother, 2005, 6(5): 755-64. |
| 25 | 肖正华, 卢 晨, 项蒙蒙, 等. 中国心房颤动诊疗指南的质量评价[J]. 中国循证医学杂志, 2019, 19(2): 199-204. |
| 26 | Vinther KH, Tveskov C, Möller S, et al. Excessive premature atrial complexes and the risk of recurrent stroke or death in an ischemic stroke population[J]. J Stroke Cerebrovasc Dis, 2017, 26(6): 1163-70. |
| 27 | O’Neal WT, Howard VJ, Kleindorfer D, et al. Interrelationship between electrocardiographic left ventricular hypertrophy, QT prolongation, and ischaemic stroke: the REasons for Geographic and Racial Differences in Stroke Study[J]. Europace, 2016, 18(5): 767-72. |
| 28 | Dahlin AA, Parsons CC, Barengo NC, et al. Association of ventricular arrhythmia and in-hospital mortality in stroke patients in Florida: a nonconcurrent prospective study[J]. Medicine, 2017, 96(28): e7403. |
| 29 | Marinheiro R, Parreira L, Amador P, et al. Excessive atrial ectopic activity as an independent risk factor for ischemic stroke[J]. Int J Cardiol, 2017, 249: 226-30. |
| 30 | Li JX, Yuan MG, Liu YF, et al. Incidence of constipation in stroke patients: a systematic review and meta-analysis[J]. Medicine, 2017, 96(25): e7225. |
| 31 | Su YJ, Zhang XY, Zeng JS, et al. New-onset constipation at acute stage after first stroke: incidence, risk factors, and impact on the stroke outcome[J]. Stroke, 2009, 40(4): 1304-9. |
| 32 | Ley RE, Turnbaugh PJ, Klein S, et al. Microbial ecology: human gut microbes associated with obesity[J]. Nature, 2006, 444(7122):1022-9. |
| 33 | Wang ZN, Klipfell E, Bennett BJ, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease[J]. Nature, 2011, 472(7341): 57-63. |
| 34 | Org E, Mehrabian M, Lusis AJ. Unraveling the environmental and genetic interactions inatherosclerosis: central role of the gut microbiota[J]. Atherosclerosis, 2015, 241(2): 387-99. |
| 35 | Sundbøll J, Szépligeti SK, Adelborg K, et al. Constipation and risk of cardiovascular diseases: a Danish population-based matched cohort study[J]. BMJ Open, 2020, 10(9): e037080. |
| 36 | Fu Y, Liu Q, Anrather J, et al. Immune interventions in stroke[J]. Nat Rev Neurol, 2015, 11(9):524-35. |
| 37 | An CR, Shi YJ, Li PY, et al. Molecular dialogs between the ischemic brain and the peripheral immune system: dualistic roles in injury and repair[J]. Prog Neurobiol, 2014, 115: 6-24. |
| 38 | Haeusler KG, Schmidt WU, Föhring F, et al. Cellular immunodepression preceding infectious complications after acute ischemic stroke in humans[J]. Cerebrovasc Dis, 2008, 25(1/2): 50-8. |
| 39 | 刘子嘉. 中性粒细胞/淋巴细胞比值与进展性缺血性卒中的相关性研究[D]. 长春: 吉林大学, 2023. |
| 40 | 何 妮, 黄 攀, 刘 梦, 等. 全身炎症反应指数与急性缺血性脑卒中患者早期神经功能恶化及预后的相关性研究[J]. 华西医学, 2024, 39(4): 580-7. |
| 41 | 张 威, 李静杰, 王海峰, 等. NLR在急性缺血性脑卒中患者早期神经功能损伤、预后及复发风险评估中的价值[J].浙江医学,2024,46(07):728-32, 751. |
| 42 | 刘 洁, 陈 璐, 黄小雨, 等. 中性粒细胞/淋巴细胞与脑梗死复发的关系[J]. 医学研究杂志, 2020, 49(6): 61-5. |
| 43 | 吴一帆. 基于机器学习的MRI放射组学急性缺血性脑卒中复发预测模型研究[D]. 江西:南昌大学, 2023. |
| 44 | 高希法, 彭明洋, 任 军, 等. 基于DWI图像的急性脑卒中病灶自动分割及复发风险预测研究[J]. 临床神经病学杂志, 2024, 37(3): 161-5. |
| 45 | 王 玥, 侯晓雯, 陈会生, 等. 基于颅内斑块影像组学联合传统标志物预测缺血性脑卒中复发风险[J]. 磁共振成像, 2023, 14(8): 1-9. |
| 46 | 刘 敬. ESRS联合CISS分型对脑梗死复发的预测价值研究[D]. 大连: 大连医科大学, 2017. |
| 47 | Clare F, Walter M, Charles DA, et al. Risk and secondary prevention of stroke recurrence[J]. Stroke, 2020, 51(8):2435-44. |
| [1] | Shenhao PAN, Yankun LI, Zhewei WU, Yuling MAO, Chunyan WANG. Establishment of a predictive nomogram for clinical pregnancy rate in patients with endometriosis undergoing fresh embryo transfer [J]. Journal of Southern Medical University, 2024, 44(7): 1407-1415. |
| [2] | Caiyu SHEN, Shuai WANG, Ruiying ZHOU, Yuhe WANG, Qin GAO, Xingzhi CHEN, Shu YANG. Prediction of risk of in-hospital death in patients with chronic heart failure complicated by lung infections using interpretable machine learning [J]. Journal of Southern Medical University, 2024, 44(6): 1141-1148. |
| [3] | LUO Xiao, CHENG Yi, WU Cheng, HE Jia. An interpretable machine learning-based prediction model for risk of death for patients with ischemic stroke in intensive care unit [J]. Journal of Southern Medical University, 2023, 43(7): 1241-1247. |
| [4] | HE Shuning, ZHANG Jiahao, YANG Ruonan, YUAN Ping. Spatial distribution of cognitive dysfunction and its risk factors in Chinese population aged 45 years and above [J]. Journal of Southern Medical University, 2023, 43(4): 611-619. |
| [5] | QIN Yue, LIU Rongping, ZHANG Xiaonan, ZHANG Wan, REN Chen, WU Dehua. A single-center, retrospective analysis of relapse and progression patterns of primary central nervous system lymphoma: can whole brain radiotherapy be replaced? [J]. Journal of Southern Medical University, 2023, 43(4): 499-506. |
| [6] | LIANG Libing, CHEN Jingjuan, ZHANG Chengguo, WANG Yukai, LUO Baigui, ZHOU Tianen, WANG Xiaofeng. Serum lipoprotein-associated phospholipase A2 level is positively correlated with the recurrence risk of acute ischemic cerebral infarction in hypertensive patients [J]. Journal of Southern Medical University, 2023, 43(2): 317-322. |
| [7] | ZHANG Haoxuan, LU Jin, JIANG Chengyi, FANG Meifang. Construction and evaluation of an artificial intelligence-based risk prediction model for death in patients with nasopharyngeal cancer [J]. Journal of Southern Medical University, 2023, 43(2): 271-279. |
| [8] | ZHANG Ling, LI Jun, YANG Ming, ZHANG Qiong, WU Xiuying, WANG Qingxia. Investigation of medical humanistic practice ability of nurses and factors affecting their practices: a questionnaire-based analysis of 1196 cases in a general hospital in Hunan Province [J]. Journal of Southern Medical University, 2023, 43(1): 139-144. |
| [9] | ZHANG Panyang, HE Mingmin, ZENG Yuanyuan, CAI Xiongwei. Identification of key molecules in miRNA-mRNA regulatory network associated with high-grade serous ovarian cancer recurrence using bioinformatic analysis [J]. Journal of Southern Medical University, 2023, 43(1): 8-16. |
| [10] | MENG Lingfei, ZHU Xueyan, YANG Liming, LI Xinyang, CHENG Siyu, GUO Shizheng, ZHUANG Xiaohua, ZOU Hongbin, CUI Wenpeng. Development and validation of a prediction model for treatment failure in peritoneal dialysis-associated peritonitis patients: a multicenter study [J]. Journal of Southern Medical University, 2022, 42(4): 546-553. |
| [11] | SU Xiaofeng, HAN Jiming, GAO Yinghui, FAN Li, HE Zijun, ZHAO Zhe, LIN Junlin, GUO Jingjing, CHEN Kaibing, GAOYan, LIU lin. A long-term ischemic stroke risk score model in patients aged 60 years and older with obstructive sleep apnea: a multicenter prospective cohort study [J]. Journal of Southern Medical University, 2022, 42(3): 338-346. |
| [12] | LIU Jin, YANG Yanling, YAN Ke, ZHU Cairong, JIANG Min. Development and validation of nomograms for predicting stroke recurrence after first-episode ischemic stroke [J]. Journal of Southern Medical University, 2022, 42(1): 130-136. |
| [13] | ZHANG Haijie, YIN Fu, CHEN Menglin, QI Anqi, YANG Liyang, CUI Weiwei, YANG Shanshan, WEN Ge. Predicting postoperative recurrence of stage I-III renal clear cell carcinoma based on preoperative CT radiomics feature nomogram [J]. Journal of Southern Medical University, 2021, 41(9): 1358-1365. |
| [14] | LIN Yidie, ZHANG Baiyang, HU Meijing, XU Minghan, QIN Chengjie, ZHU Cairong. Causal relationship between physical exercise and risk of ischemic stroke recurrence based on the potential outcome theory [J]. Journal of Southern Medical University, 2021, 41(8): 1191-1197. |
| [15] | . Relapse of ankylosing spondylitis and its predictors after withdrawal of tumor necrosis factor-α inhibitors: a 52-week follow-up study [J]. Journal of Southern Medical University, 2021, 41(5): 633-639. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||