Journal of Southern Medical University ›› 2024, Vol. 44 ›› Issue (7): 1407-1415.doi: 10.12122/j.issn.1673-4254.2024.07.21
Shenhao PAN1,2( ), Yankun LI1,2, Zhewei WU1,2, Yuling MAO1, Chunyan WANG1(
), Yankun LI1,2, Zhewei WU1,2, Yuling MAO1, Chunyan WANG1( )
)
Received:2024-05-15
Online:2024-07-20
Published:2024-07-25
Contact:
Chunyan WANG
E-mail:psh@stu.gzhmu.edu.cn;wangchunyan@zju.edu.cn
Supported by:Shenhao PAN, Yankun LI, Zhewei WU, Yuling MAO, Chunyan WANG. Establishment of a predictive nomogram for clinical pregnancy rate in patients with endometriosis undergoing fresh embryo transfer[J]. Journal of Southern Medical University, 2024, 44(7): 1407-1415.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2024.07.21
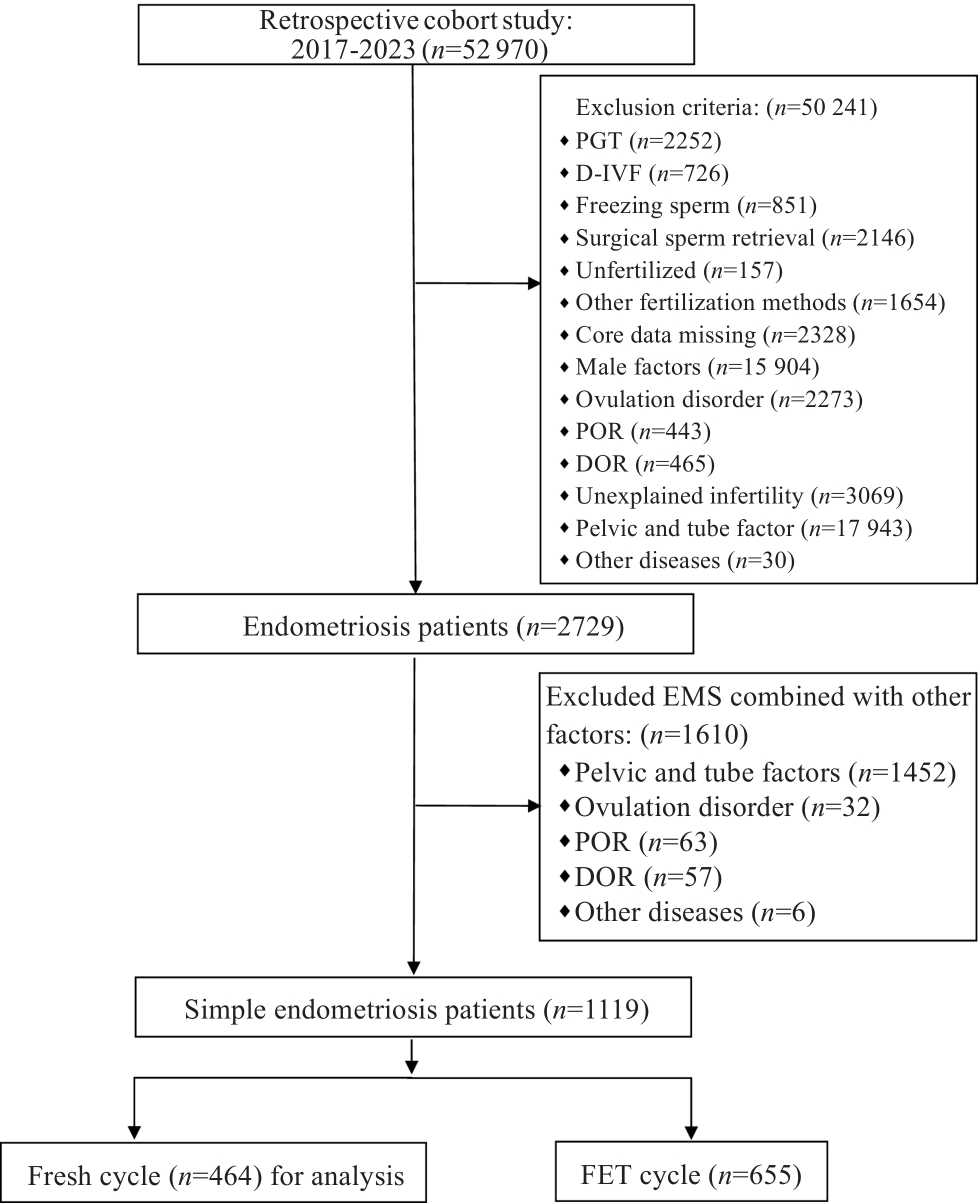
Fig 1 Flowchart of subject selection. Sample size (n) is indicated in each category. PGT: Preimplantation genetic testing; D-IVF: Sperm donation-in vitro fertilization; DOR: Diminished ovarian reserve; POR: Poor ovarian response; FET: Frozen embryo transfer.
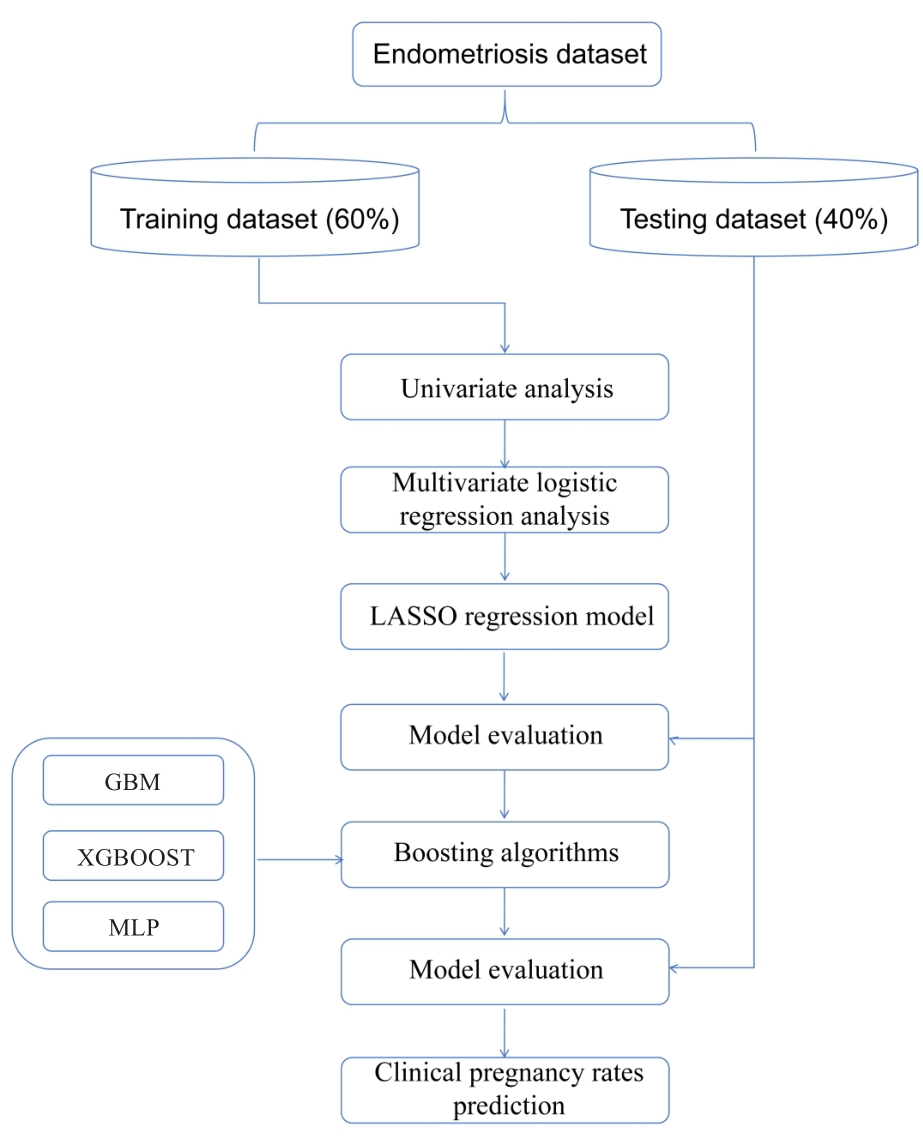
Fig.2 Proposed methodology for research work. LightGBM: Light gradient boosting machine; XGBoost: Extreme Gradient Boosting; MLP: Multi-Layer Perceptron.
| Variables | Pregnancy (n=254) | Unpregnancy (n=210) | t/χ² | P |
|---|---|---|---|---|
| Age (year) | 32.19±3.58 | 33.70±4.43 | -4.008 | <0.001 |
| BMI(kg/m2) | 21.22±3.00 | 21.66±2.87 | -1.596 | 0.111 |
| AMH (ng/mL) | 3.19±2.23 | 2.81±2.10 | 1.872 | 0.062 |
| Infertility time in years | 4.00±2.55 | 4.35±2.81 | -1.358 | 0.175 |
| Type of subfertility | 0.345 | 0.571 | ||
| Primary infertility | 102 | 90 | ||
| Secondary infertility | 152 | 120 | ||
| FSH (U/L) | 5.92±2.44 | 6.54±3.06 | -2.447 | 0.015 |
| LH (U/L) | 4.35±5.80 | 3.70±2.93 | 1.554 | 0.121 |
| P (nmol/L) | 1.69±6.80 | 1.61±5.55 | 0.137 | 0.891 |
| PRL (ng/mL) | 17.24±8.85 | 16.31±8.87 | 1.124 | 0.262 |
| T (nmol/L) | 0.98±0.46 | 1.00±0.41 | -0.611 | 0.541 |
| E2 (pg/mL) | 220.95±365.46 | 179.90±196.84 | 1.540 | 0.124 |
| Dates of Gn Duration | 11.14±2.28 | 10.78±2.38 | 1.650 | 0.100 |
| Total Gn (IU) | 2356.74±1166.58 | 2423.30±1018.86 | -0.652 | 0.515 |
| Gn initation dose | 190.25±60.69 | 211.22±67.40 | -3.526 | <0.001 |
| E2 on HCG day (pg/mL) | 8062.67±3937.74 | 7527.33±4201.39 | 1.414 | 0.158 |
| P on HCG day (nmol/L) | 2.04±0.94 | 2.20±1.01 | -1.714 | 0.087 |
| Follicles≥14 mm on HCG day | 6.45±4.32 | 5.80±4.19 | 1.633 | 0.103 |
| Endometrium thickness on HCG day (mm) | 11.46±2.22 | 11.10±2.42 | 1.665 | 0.097 |
| Oocytes retrieved | 9.09±3.92 | 8.19±4.31 | 2.366 | 0.018 |
| ART Cycles | 1.33±0.68 | 1.55±1.07 | -2.607 | 0.010 |
| Fertilization rate (%) | 83.58±17.52 | 81.50±20.29 | 1.174 | 0.241 |
| Normal Fertilization rate (%) | 59.92±23.11 | 60.99±23.67 | -0.492 | 0.623 |
| degeneration rate(%) | 2.97±8.24 | 3.24±1.43 | -0.252 | 0.801 |
| Cleavage rate (%) | 98.59±5.00 | 97.45±10.38 | 1.495 | 0.136 |
| Usable embryos rate (%) | 56.53±26.37 | 53.74±26.88 | 1.127 | 0.260 |
| High quality day 3 embyo (%) | 28.43±26.93 | 24.61±30.07 | 1.442 | 0.150 |
| Blastulation rate (%) | 33.08±33.81 | 31.50±33.41 | 0.506 | 0.613 |
| Number of frozen embryos | 2.08±2.05 | 1.58±1.91 | 2.716 | 0.007 |
| Embryo transfer (n) | 1.65±0.48 | 1.48±0.50 | 3.700 | <0.001 |
Tab.1 Univariate analysis of factors affecting clinical pregnancy
| Variables | Pregnancy (n=254) | Unpregnancy (n=210) | t/χ² | P |
|---|---|---|---|---|
| Age (year) | 32.19±3.58 | 33.70±4.43 | -4.008 | <0.001 |
| BMI(kg/m2) | 21.22±3.00 | 21.66±2.87 | -1.596 | 0.111 |
| AMH (ng/mL) | 3.19±2.23 | 2.81±2.10 | 1.872 | 0.062 |
| Infertility time in years | 4.00±2.55 | 4.35±2.81 | -1.358 | 0.175 |
| Type of subfertility | 0.345 | 0.571 | ||
| Primary infertility | 102 | 90 | ||
| Secondary infertility | 152 | 120 | ||
| FSH (U/L) | 5.92±2.44 | 6.54±3.06 | -2.447 | 0.015 |
| LH (U/L) | 4.35±5.80 | 3.70±2.93 | 1.554 | 0.121 |
| P (nmol/L) | 1.69±6.80 | 1.61±5.55 | 0.137 | 0.891 |
| PRL (ng/mL) | 17.24±8.85 | 16.31±8.87 | 1.124 | 0.262 |
| T (nmol/L) | 0.98±0.46 | 1.00±0.41 | -0.611 | 0.541 |
| E2 (pg/mL) | 220.95±365.46 | 179.90±196.84 | 1.540 | 0.124 |
| Dates of Gn Duration | 11.14±2.28 | 10.78±2.38 | 1.650 | 0.100 |
| Total Gn (IU) | 2356.74±1166.58 | 2423.30±1018.86 | -0.652 | 0.515 |
| Gn initation dose | 190.25±60.69 | 211.22±67.40 | -3.526 | <0.001 |
| E2 on HCG day (pg/mL) | 8062.67±3937.74 | 7527.33±4201.39 | 1.414 | 0.158 |
| P on HCG day (nmol/L) | 2.04±0.94 | 2.20±1.01 | -1.714 | 0.087 |
| Follicles≥14 mm on HCG day | 6.45±4.32 | 5.80±4.19 | 1.633 | 0.103 |
| Endometrium thickness on HCG day (mm) | 11.46±2.22 | 11.10±2.42 | 1.665 | 0.097 |
| Oocytes retrieved | 9.09±3.92 | 8.19±4.31 | 2.366 | 0.018 |
| ART Cycles | 1.33±0.68 | 1.55±1.07 | -2.607 | 0.010 |
| Fertilization rate (%) | 83.58±17.52 | 81.50±20.29 | 1.174 | 0.241 |
| Normal Fertilization rate (%) | 59.92±23.11 | 60.99±23.67 | -0.492 | 0.623 |
| degeneration rate(%) | 2.97±8.24 | 3.24±1.43 | -0.252 | 0.801 |
| Cleavage rate (%) | 98.59±5.00 | 97.45±10.38 | 1.495 | 0.136 |
| Usable embryos rate (%) | 56.53±26.37 | 53.74±26.88 | 1.127 | 0.260 |
| High quality day 3 embyo (%) | 28.43±26.93 | 24.61±30.07 | 1.442 | 0.150 |
| Blastulation rate (%) | 33.08±33.81 | 31.50±33.41 | 0.506 | 0.613 |
| Number of frozen embryos | 2.08±2.05 | 1.58±1.91 | 2.716 | 0.007 |
| Embryo transfer (n) | 1.65±0.48 | 1.48±0.50 | 3.700 | <0.001 |
| Variables | B | χ² | P | OR | 95% CI |
|---|---|---|---|---|---|
| Age (year) | -0.075 | 7.990 | 0.005 | 0.928 | 0.881-0.977 |
| Gn initation dose | -0.003 | 4.495 | 0.034 | 0.997 | 0.993-1.000 |
| ART Cycles | -0.247 | 4.207 | 0.040 | 0.781 | 0.617-0.989 |
| Embryo transfer (n) | 0.838 | 17.492 | <0.001 | 2.311 | 1.561-3.422 |
Tab.2 Multivariate logistic regression analysis of key clinical features affecting pregnancy outcomes
| Variables | B | χ² | P | OR | 95% CI |
|---|---|---|---|---|---|
| Age (year) | -0.075 | 7.990 | 0.005 | 0.928 | 0.881-0.977 |
| Gn initation dose | -0.003 | 4.495 | 0.034 | 0.997 | 0.993-1.000 |
| ART Cycles | -0.247 | 4.207 | 0.040 | 0.781 | 0.617-0.989 |
| Embryo transfer (n) | 0.838 | 17.492 | <0.001 | 2.311 | 1.561-3.422 |
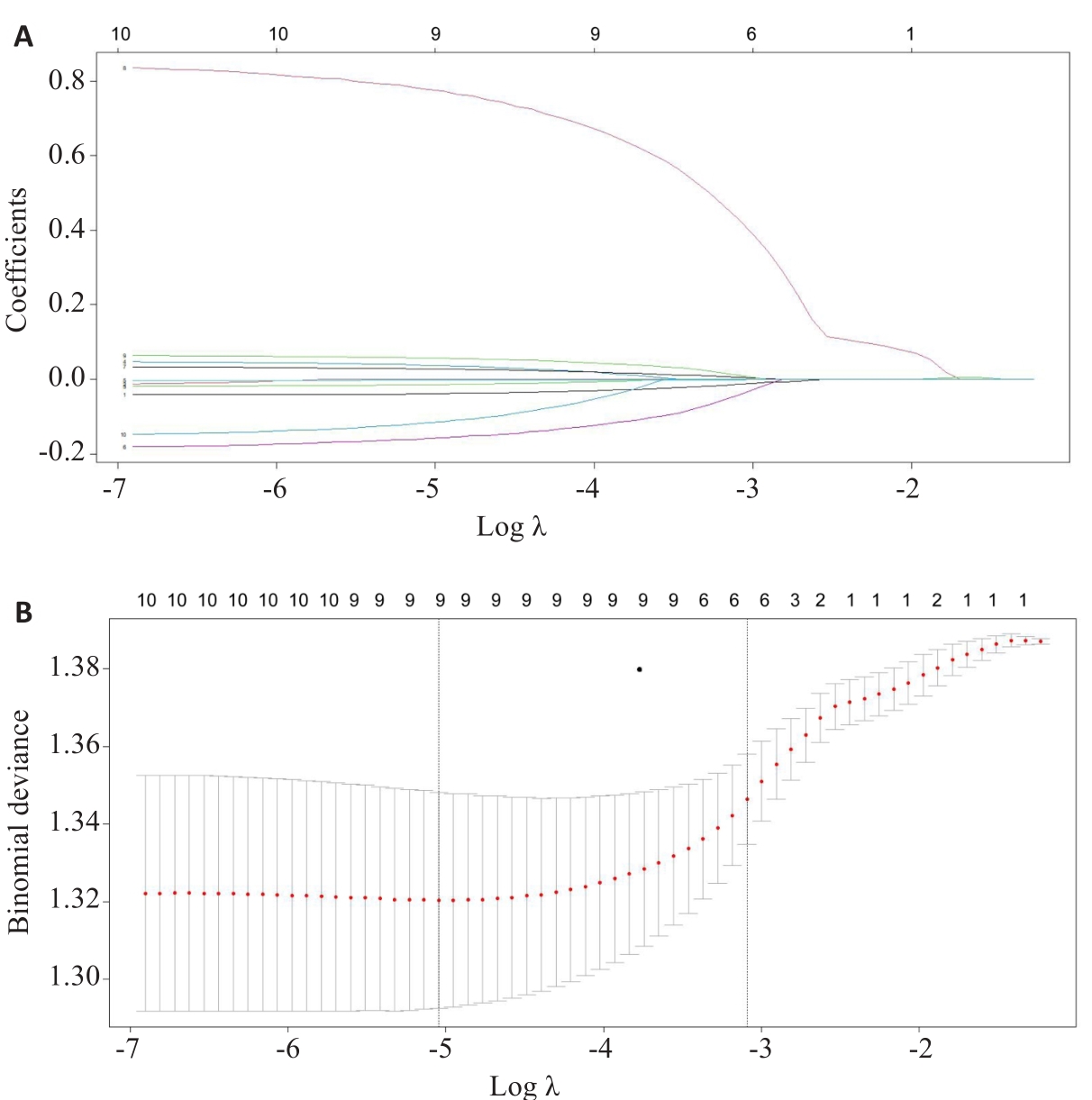
Fig.3 LASSO regression model. A: Coefficient distribution chart by lasso regression. Each curve represents a coefficient, and the x-axis represents the regularization penalty parameter. As λ changes, a coefficient that becomes non-zero enters the LASSO regression model. B: Ten-fold cross-validation diagram. The red dotted vertical line crosses over the optimal log λ. The two dotted lines represent one standard deviation from the minimum value, with 1se as the criterion (λ=0.006438551).
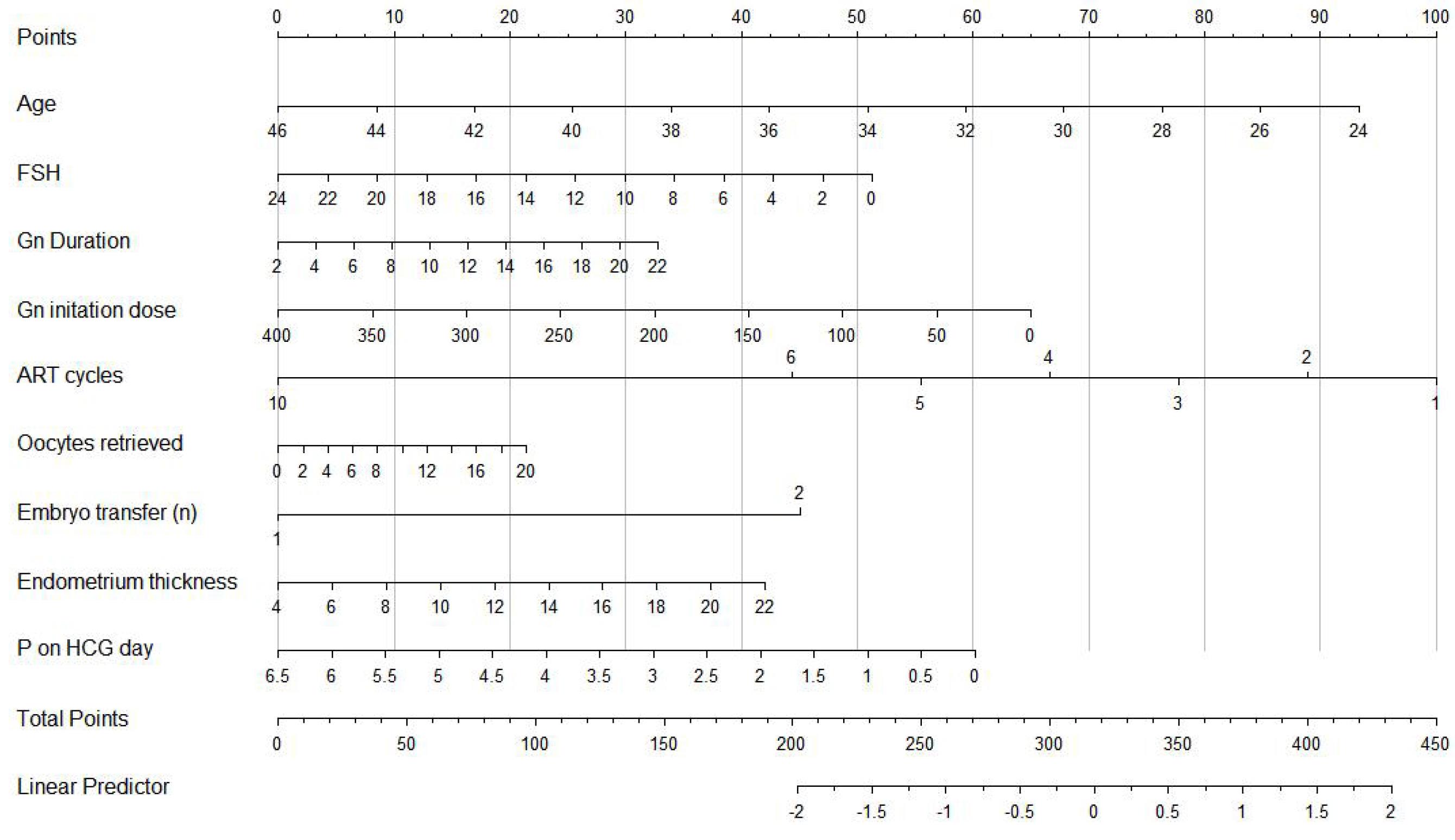
Fig.4 Nomogram of the prediction model for clinical pregnancy in endometriosis patients undergoing fresh embryo transfer. The nomogram is applied by drawing a perpendicular line from each risk factor's corresponding axis to intersect with the "Points" top line, followed by calculation of the total score as the sum of points for all risk factors, drawing a descending line from the "Total points" axis to intercept with the lower line, and determination of the probability of clinical pregnancy.
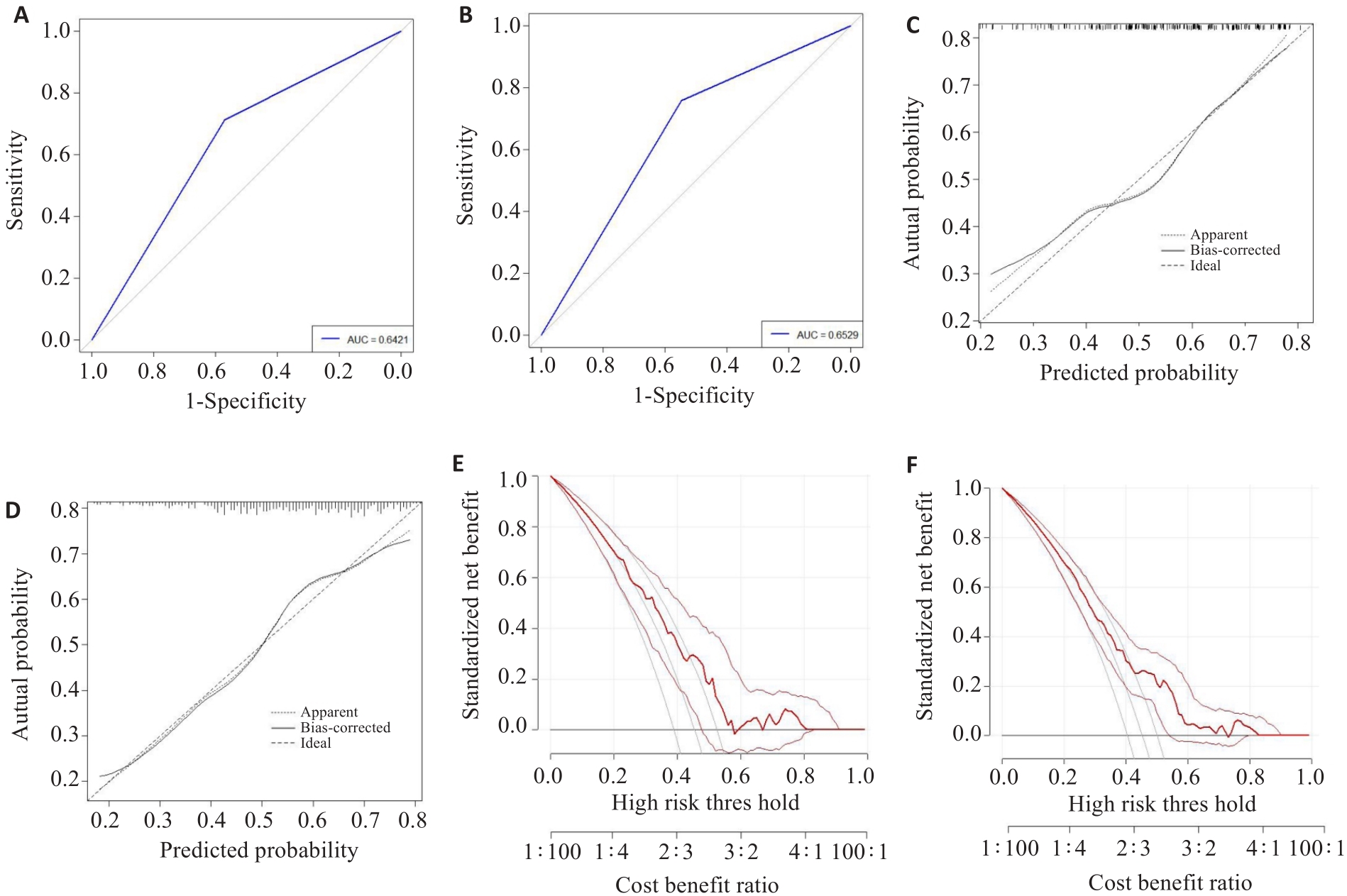
Fig.5 Validation of accuracy and discrimination of the nomogram model. A, B: ROC for training and validation cohorts. C, D: Calibration curves for evaluating calibration of the model: The horizontal axis is the predicted probability provided by this model, and the vertical axis is the observed incidence of pregnancy failure. The ideal line with 45° slope represents a perfect prediction (the predicted probability equals the observed probability; E, F: Decision curve of the prediction model.
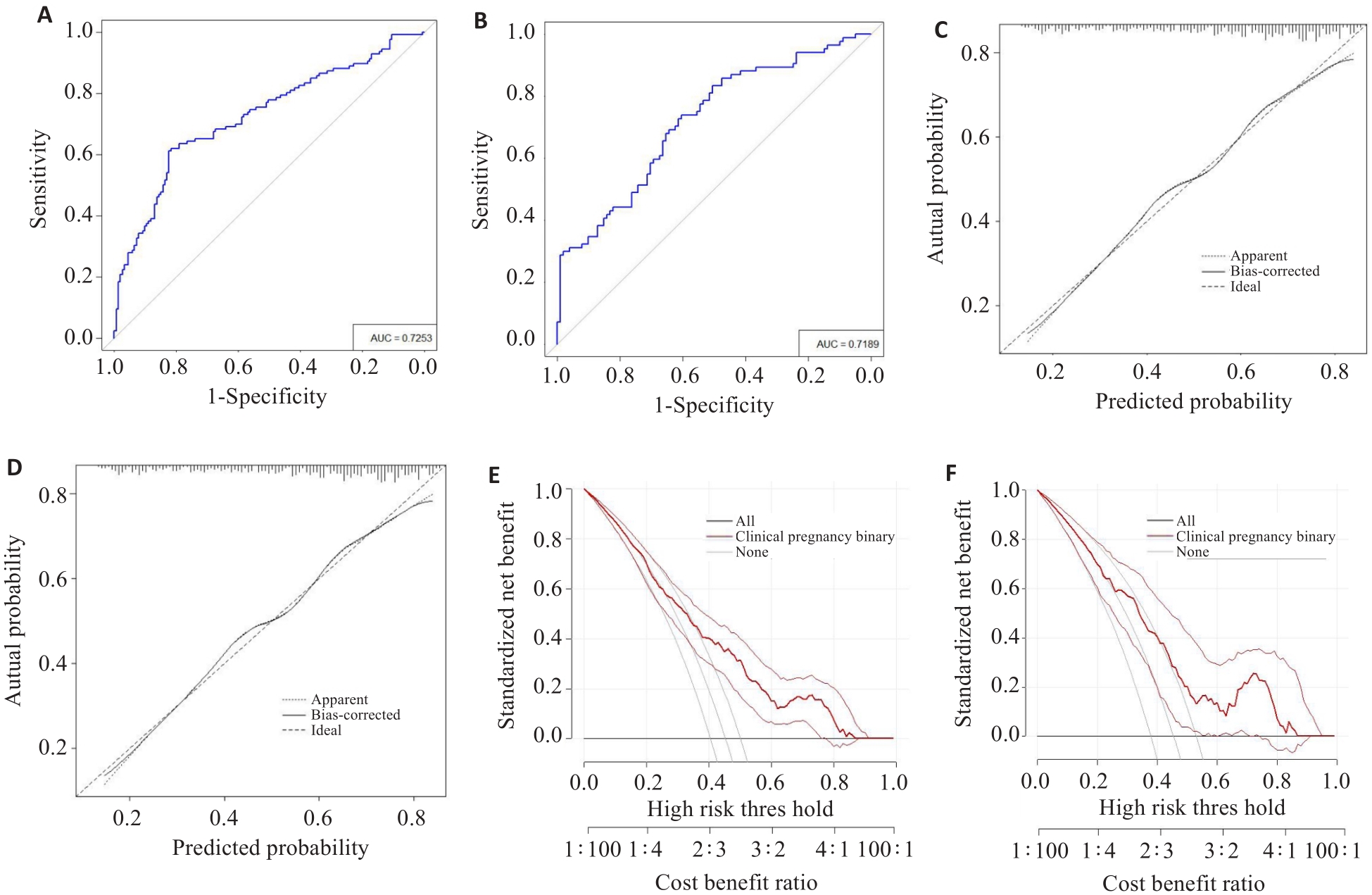
Fig.6 Ensemble learning improves the performance of the predictive models. A, B: ROC for training and validation cohorts; C, D: Calibration curves for evaluating calibration of the training and validation cohorts. E, F: Decision curve of the training and validation cohorts.
| 1 | Saunders PTK, Horne AW. Endometriosis: Etiology, pathobiology, and therapeutic prospects[J]. Cell, 2021, 184(11): 2807-24. |
| 2 | Taylor HS, Kotlyar AM, Flores VA. Endometriosis is a chronic systemic disease: clinical challenges and novel innovations[J]. Lancet, 2021, 397(10276): 839-52. |
| 3 | Simoens S, Dunselman G, Dirksen C, et al. The burden of endometriosis: costs and quality of life of women with endometriosis and treated in referral centres[J]. Hum Reprod, 2012, 27(5): 1292-9. |
| 4 | Ata B, Somigliana E. Endometriosis, staging, infertility and assisted reproductive technology: time for a rethink[J]. Reprod Biomed Online, 2024, 49(1): 103943. |
| 5 | Pais AS, Almeida-Santos T. Recent insights explaining susceptibility to endometriosis-From genetics to environment[J]. WIREs Mech Dis, 2023, 15(6): e1624. |
| 6 | Huang Y, Wang Z, Li B, et al. Loss of KLF15 impairs endometrial receptivity by inhibiting EMT in endometriosis[J]. J Endocrinol, 2024, 261(2): e230319. |
| 7 | Melado L, Ata B. Chapter 11. Endometriosis-related complications in women undergoing in-vitro fertilization[J]. Best Pract Res Clin Obstet Gynaecol, 2024, 93: 102456. |
| 8 | Bourdon M, Peigné M, Maignien C, et al. Impact of endometriosis surgery on in vitro fertilization/intracytoplasmic sperm injection outcomes: a systematic review and meta-analysis[J]. Reprod Sci, 2024, 31(6): 1431-55. |
| 9 | Ozer G, Akca A, Yuksel B, et al. Prediction of risk factors for first trimester pregnancy loss in frozen-thawed good-quality embryo transfer cycles using machine learning algorithms[J]. J Assist Reprod Genet, 2023, 40(2): 279-88. |
| 10 | Gao H, Liu DE, Li YM, et al. Early prediction of live birth for assisted reproductive technology patients: a convenient and practical prediction model[J]. Sci Rep, 2021, 11: 331. |
| 11 | Huang FP, Zhang HL, Xie X, et al. A model for pregnancy rates after IVF-ET in patients with infertility and endometriosis[J]. Eur Rev Med Pharmacol Sci, 2022, 26(19): 7188-94. |
| 12 | Ballester M, Oppenheimer A, Mathieu d' Argent E, et al. Nomogram to predict pregnancy rate after ICSI-IVF cycle in patients with endometriosis[J]. Hum Reprod, 2012, 27(2): 451-6. |
| 13 | Kordus RJ, LaVoie HA. Granulosa cell biomarkers to predict pregnancy in ART: pieces to solve the puzzle[J]. Reproduction, 2017, 153(2): R69-83. |
| 14 | Jin H, Shen X, Song W, et al. The development of nomograms to predict blastulation rate following cycles of in vitro fertilization in patients with tubal factor infertility, polycystic ovary syndrome, or endometriosis[J]. Front Endocrinol: Lausanne, 2021, 12: 751373. |
| 15 | Zhu S, Liao X, Jiang W, et al. Development and validation of a nomogram model for predicting clinical pregnancy in endometriosis patients undergoing fresh embryo transfer[J]. BMC Pregnancy Childbirth, 2023, 23(1): 764. |
| 16 | Riley RD, Ensor J, Snell KIE, et al. Calculating the sample size required for developing a clinical prediction model[J]. BMJ, 2020: m441. |
| 17 | Diakiw SM, Hall JMM, VerMilyea MD, et al. Development of an artificial intelligence model for predicting the likelihood of human embryo euploidy based on blastocyst images from multiple imaging systems during IVF[J]. Hum Reprod, 2022, 37(8): 1746-59. |
| 18 | Majumdar G, Majumdar A, Verma IC, et al. Relationship between morphology, euploidy and implantation potential of cleavage and blastocyst stage embryos[J]. J Hum Reprod Sci, 2017, 10(1): 49-57. |
| 19 | Lin XN, Wei ML, Tong XM, et al. Outcome of in vitro fertilization in endometriosis-associated infertility: a 5-year database cohort study[J]. Chin Med J: Engl, 2012, 125(15): 2688-93. |
| 20 | de Ziegler D, Pirtea P, Carbonnel M, et al. Assisted reproduction in endometriosis[J]. Best Pract Res Clin Endocrinol Metab, 2019, 33(1): 47-59. |
| 21 | Härkki P, Tiitinen A, Ylikorkala O. Endometriosis and assisted reproduction techniques[J]. Ann N Y Acad Sci, 2010, 1205: 207-13. |
| 22 | Osmanlıoğlu Ş, Berker B, Aslan B, et al. Presence of endometrioma does not impair embryo quality and assisted reproductive technology (ART) cycle outcome in diminished ovarian reserve (DOR) patients[J]. Reprod Sci, 2023, 30(5): 1540-7. |
| 23 | Barbosa MA, Teixeira DM, Navarro PA, et al. Impact of endometriosis and its staging on assisted reproduction outcome: systematic review and meta-analysis[J]. Ultrasound Obstet Gynecol, 2014, 44(3): 261-78. |
| 24 | Bourdon M, Dahan Y, Maignien C, et al. Influence of endometrioma size on ART outcomes[J]. Reprod Biomed Online, 2022, 45(6): 1237-46. |
| 25 | Wang XZ, Li WS, Chen XM, et al. Is the long-acting gonadotropin-releasing hormone agonist longprotocol better for patients with endometriosis undergoing IVF[J]? Int J Gynecol Obstet, 2023, 162(1): 325-32. |
| 26 | Hernández A, Sanz A, Spagnolo E, et al. Impact of ovarian endometrioma and surgery on reproductive outcomes: a single-center Spanish cohort study[J]. Biomedicines, 2023, 11(3): 844. |
| 27 | Hong IS. Endometrial stem/progenitor cells: properties, origins, and functions[J]. Genes Dis, 2023, 10(3): 931-47. |
| 28 | Labarta E, Martínez-Conejero JA, Alamá P, et al. Endometrial receptivity is affected in women with high circulating progesterone levels at the end of the follicular phase: a functional genomics analysis[J]. Hum Reprod, 2011, 26(7): 1813-25. |
| 29 | Ganie SM, Pramanik PKD, Bashir Malik M, et al. An ensemble learning approach for diabetes prediction using boosting techniques[J]. Front Genet, 2023, 14: 1252159. |
| [1] | Caiyu SHEN, Shuai WANG, Ruiying ZHOU, Yuhe WANG, Qin GAO, Xingzhi CHEN, Shu YANG. Prediction of risk of in-hospital death in patients with chronic heart failure complicated by lung infections using interpretable machine learning [J]. Journal of Southern Medical University, 2024, 44(6): 1141-1148. |
| [2] | LIU Yunze, LI Chengrun, GUO Juntang, LIU Yang. A clinical-radiomics nomogram for differentiating focal organizing pneumonia and lung adenocarcinoma [J]. Journal of Southern Medical University, 2024, 44(2): 397-404. |
| [3] | ZHANG Benlong, LU Yixun, LI Li, GAO Yunhe, LIANG Wenquan, XI Hongqing, WANG Xinxin, ZHANG Kecheng, CHEN Lin. Establishment and validation of a nomogram for predicting prognosis of gastric neuroendocrine neoplasms based on data from 490 cases in a single center [J]. Journal of Southern Medical University, 2023, 43(2): 183-190. |
| [4] | ZHANG Haoxuan, LU Jin, JIANG Chengyi, FANG Meifang. Construction and evaluation of an artificial intelligence-based risk prediction model for death in patients with nasopharyngeal cancer [J]. Journal of Southern Medical University, 2023, 43(2): 271-279. |
| [5] | KONG Dexian, SONG Liping, XIANG Yang. Construction of a prognostic nomogram combining PET/CT metabolic parameters and blood inflammatory markers for non-small cell lung cancer treated with first-line chemotherapy [J]. Journal of Southern Medical University, 2023, 43(12): 2139-2144. |
| [6] | LIU Zhaojun, ZHOU Xiaoli. A nomogram based on systemic inflammation markers can predict adverse outcomes in patients with heart failure [J]. Journal of Southern Medical University, 2022, 42(8): 1149-1158. |
| [7] | LUO Chao, WANG Gaoming, HU Liwen, QIANG Yong, ZHENG Chao, SHEN Yi. Development and validation of a prognostic model based on SEER data for patients with esophageal carcinoma after esophagectomy [J]. Journal of Southern Medical University, 2022, 42(6): 794-804. |
| [8] | MENG Lingfei, ZHU Xueyan, YANG Liming, LI Xinyang, CHENG Siyu, GUO Shizheng, ZHUANG Xiaohua, ZOU Hongbin, CUI Wenpeng. Development and validation of a prediction model for treatment failure in peritoneal dialysis-associated peritonitis patients: a multicenter study [J]. Journal of Southern Medical University, 2022, 42(4): 546-553. |
| [9] | ZHAO Chenling, DONG Ting, SUN Lunyan, HU Huibing, WANG Qiong, TIAN Liwei, JIANG Zhangsheng. Establishment and validation of a predictive nomogram for liver fibrosis in patients with Wilson disease and abnormal lipid metabolism [J]. Journal of Southern Medical University, 2022, 42(11): 1720-1725. |
| [10] | CAI Hong, LIU Mian, LIN Miaoling, LI Hong, SHEN Lang, QUAN Song. Lowered expression of CCN5 in endometriotic tissues promotes proliferation, migration and invasion of endometrial stromal cells [J]. Journal of Southern Medical University, 2022, 42(1): 86-92. |
| [11] | LIU Jin, YANG Yanling, YAN Ke, ZHU Cairong, JIANG Min. Development and validation of nomograms for predicting stroke recurrence after first-episode ischemic stroke [J]. Journal of Southern Medical University, 2022, 42(1): 130-136. |
| [12] | NIE Weizhe, LI Shuting, Krina T. Zondervan, Christian M. Becker, GUO Yinan, ZONG Lili. Analysis of the factors contributing to endometriosis in China and UK [J]. Journal of Southern Medical University, 2022, 42(1): 137-142. |
| [13] | ZHANG Haijie, YIN Fu, CHEN Menglin, QI Anqi, YANG Liyang, CUI Weiwei, YANG Shanshan, WEN Ge. Predicting postoperative recurrence of stage I-III renal clear cell carcinoma based on preoperative CT radiomics feature nomogram [J]. Journal of Southern Medical University, 2021, 41(9): 1358-1365. |
| [14] | . Factors affecting survival prognosis of advanced gastric cancer and establishment of a nomogram predictive model [J]. Journal of Southern Medical University, 2021, 41(4): 621-627. |
| [15] | . Mechanism of Ziyin recipe for treatment of ovulatory infertility: a network pharmacology-based study and clinical observations [J]. Journal of Southern Medical University, 2021, 41(3): 319-328. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||