Journal of Southern Medical University ›› 2024, Vol. 44 ›› Issue (6): 1141-1148.doi: 10.12122/j.issn.1673-4254.2024.06.15
Caiyu SHEN1( ), Shuai WANG2, Ruiying ZHOU1, Yuhe WANG3, Qin GAO4, Xingzhi CHEN4, Shu YANG1(
), Shuai WANG2, Ruiying ZHOU1, Yuhe WANG3, Qin GAO4, Xingzhi CHEN4, Shu YANG1( )
)
Received:2024-01-15
Online:2024-06-20
Published:2024-07-01
Contact:
Shu YANG
E-mail:1224911076@qq.com;yangshu@bbmc.edu.cn
Supported by:Caiyu SHEN, Shuai WANG, Ruiying ZHOU, Yuhe WANG, Qin GAO, Xingzhi CHEN, Shu YANG. Prediction of risk of in-hospital death in patients with chronic heart failure complicated by lung infections using interpretable machine learning[J]. Journal of Southern Medical University, 2024, 44(6): 1141-1148.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2024.06.15
| Troponin T (ng/mL) | 0.7 (0.08, 0.53) | 0.64 (0.08, 0.52) | 0.88 (0.07, 0.62) | 0.834 |
| NT-proBNP (pg/mL) | 13207 (6192, 18491) | 12 852 (5555, 17906) | 14703 (8280, 20015) | <0.001 |
| PaO2 (mmHg) | 108 (71.0, 123.0) | 110 (71.2, 126.0) | 100 (69.0, 116.0) | 0.386 |
| PaCO2 (mmHg) | 43.6 (38.0, 47.0) | 43.6 (38.7, 47.0) | 43.4 (36.0, 48.0) | 0.069 |
| Lactate min (mmol/L) | 1.6 (1.0, 1.8) | 1.5 (1.0, 1.8) | 1.9 (1.1, 2.1) | <0.001 |
| Lactate max (mmol/L) | 2.8 (1.5, 3.3) | 2.6 (1.4, 3.0) | 3.4 (1.6, 4.1) | <0.001 |
| Bicarbonate min (mEq/L) | 25.9 (19.0, 26.0) | 23.0 (19.0, 26.0) | 21.3 (18.3, 25.0) | <0.001 |
| Bicarbonate max (mEq/L) | 25.7 (22.0, 29.0) | 26.1 (22.0, 29.0) | 25.0 (21.0, 28.0) | <0.001 |
| Urine output (mL) | 1759 (905, 2295) | 1848 (994, 2395) | 1382 (584, 1885) | <0.001 |
| Cerebrovascular disease [n(%)] | 221 (15.6) | 157 (13.7) | 64 (23.6) | <0.001 |
| Mild liver disease [n(%)] | 136 (9.6) | 97 (8.4) | 39 (14.4) | 0.003 |
| Myocardial infarct [n(%)] | 423 (29.9) | 338 (29.5) | 85 (31.4) | 0.556 |
| Peripheral vascular disease [n(%)] | 258 (18.2) | 210 (18.4) | 48 (17.7) | 0.805 |
| Dementia [n(%)] | 73 (5.2) | 58 (5.1) | 15 (5.5) | 0.756 |
| Chronic Pulmonary Disease [n(%)] | 608 (43.0) | 498 (43.5) | 110 (40.6) | 0.379 |
| Rheumatic disease [n(%)] | 69 (4.9) | 53 (4.6) | 16 (5.9) | 0.382 |
| Peptic ulcer disease [n(%)] | 38 (2.7) | 32 (2.8) | 6 (2.2) | 0.593 |
| Diabetes without cc [n(%)] | 448 (31.7) | 366 (32.0) | 82 (30.3) | 0.581 |
| Diabetes with cc [n(%)] | 276 (19.5) | 229 (20.0) | 47 (17.3) | 0.318 |
| Paraplegia [n(%)] | 66 (4.7) | 46 (4.0) | 20 (7.4) | 0.018 |
| Renal disease [n(%)] | 583 (41.2) | 456 (39.9) | 127 (46.9) | 0.035 |
| Metastatic solid tumor [n(%)] | 17 (1.2) | 9 (0.8) | 8 (0.3) | 0.003 |
| Aids [n(%)] | 12 (0.08) | 12 (0.1) | 0 | 0.090 |
| SOFA score | 6.9 (4.0, 9.0) | 6.3 (3.0, 9.0) | 9.2 (6.0, 12) | <0.001 |
| SAPSII score | 42.0 (32.0, 50.0) | 40.2 (31.0, 48.0) | 49.4 (40.0, 58.0) | <0.001 |
| GCS min score | 11.1 (8.0, 15.0) | 11.7 (9.0, 15.0) | 8.3 (3.0, 13.0) | <0.001 |
| Diuretic [n(%)] | 487 (34.4) | 388 (33.9) | 99 (36.5) | 0.415 |
| ACEI [n(%)] | 42 (0.03) | 32 (0.03) | 10 (0.036) | 0.436 |
Tab.1 Baseline patient characteristics [M (Q1, Q3)]
| Troponin T (ng/mL) | 0.7 (0.08, 0.53) | 0.64 (0.08, 0.52) | 0.88 (0.07, 0.62) | 0.834 |
| NT-proBNP (pg/mL) | 13207 (6192, 18491) | 12 852 (5555, 17906) | 14703 (8280, 20015) | <0.001 |
| PaO2 (mmHg) | 108 (71.0, 123.0) | 110 (71.2, 126.0) | 100 (69.0, 116.0) | 0.386 |
| PaCO2 (mmHg) | 43.6 (38.0, 47.0) | 43.6 (38.7, 47.0) | 43.4 (36.0, 48.0) | 0.069 |
| Lactate min (mmol/L) | 1.6 (1.0, 1.8) | 1.5 (1.0, 1.8) | 1.9 (1.1, 2.1) | <0.001 |
| Lactate max (mmol/L) | 2.8 (1.5, 3.3) | 2.6 (1.4, 3.0) | 3.4 (1.6, 4.1) | <0.001 |
| Bicarbonate min (mEq/L) | 25.9 (19.0, 26.0) | 23.0 (19.0, 26.0) | 21.3 (18.3, 25.0) | <0.001 |
| Bicarbonate max (mEq/L) | 25.7 (22.0, 29.0) | 26.1 (22.0, 29.0) | 25.0 (21.0, 28.0) | <0.001 |
| Urine output (mL) | 1759 (905, 2295) | 1848 (994, 2395) | 1382 (584, 1885) | <0.001 |
| Cerebrovascular disease [n(%)] | 221 (15.6) | 157 (13.7) | 64 (23.6) | <0.001 |
| Mild liver disease [n(%)] | 136 (9.6) | 97 (8.4) | 39 (14.4) | 0.003 |
| Myocardial infarct [n(%)] | 423 (29.9) | 338 (29.5) | 85 (31.4) | 0.556 |
| Peripheral vascular disease [n(%)] | 258 (18.2) | 210 (18.4) | 48 (17.7) | 0.805 |
| Dementia [n(%)] | 73 (5.2) | 58 (5.1) | 15 (5.5) | 0.756 |
| Chronic Pulmonary Disease [n(%)] | 608 (43.0) | 498 (43.5) | 110 (40.6) | 0.379 |
| Rheumatic disease [n(%)] | 69 (4.9) | 53 (4.6) | 16 (5.9) | 0.382 |
| Peptic ulcer disease [n(%)] | 38 (2.7) | 32 (2.8) | 6 (2.2) | 0.593 |
| Diabetes without cc [n(%)] | 448 (31.7) | 366 (32.0) | 82 (30.3) | 0.581 |
| Diabetes with cc [n(%)] | 276 (19.5) | 229 (20.0) | 47 (17.3) | 0.318 |
| Paraplegia [n(%)] | 66 (4.7) | 46 (4.0) | 20 (7.4) | 0.018 |
| Renal disease [n(%)] | 583 (41.2) | 456 (39.9) | 127 (46.9) | 0.035 |
| Metastatic solid tumor [n(%)] | 17 (1.2) | 9 (0.8) | 8 (0.3) | 0.003 |
| Aids [n(%)] | 12 (0.08) | 12 (0.1) | 0 | 0.090 |
| SOFA score | 6.9 (4.0, 9.0) | 6.3 (3.0, 9.0) | 9.2 (6.0, 12) | <0.001 |
| SAPSII score | 42.0 (32.0, 50.0) | 40.2 (31.0, 48.0) | 49.4 (40.0, 58.0) | <0.001 |
| GCS min score | 11.1 (8.0, 15.0) | 11.7 (9.0, 15.0) | 8.3 (3.0, 13.0) | <0.001 |
| Diuretic [n(%)] | 487 (34.4) | 388 (33.9) | 99 (36.5) | 0.415 |
| ACEI [n(%)] | 42 (0.03) | 32 (0.03) | 10 (0.036) | 0.436 |
| Trait | Coefficient |
|---|---|
| Age | 0.000264 |
| Heart rate | 0.001311 |
| Systolic blood pressure | -0.000002 |
| Resp rate | 0.000995 |
| Temperature | -0.032731 |
| Peripheral vascular disease | -0.004364 |
| Cerebrovascular disease | 0.034564 |
| Peptic ulcer disease | -0.027540 |
| Mild liver disease | 0.001324 |
| Diabetes with cc | -0.000665 |
| Metastatic solid tumor | 0.202496 |
| Aids | -0.020164 |
| SOFA | 0.004093 |
| SAPS II | 0.000876 |
| GCS min | -0.017186 |
| Weight | -0.000768 |
| White blood cell | 0.008654 |
| Platelet | -0.000094 |
| Blood urea nitrogen | 0.001737 |
| PaO2 | 0.000110 |
| PaCO2 | -0.000313 |
| Lactate min | 0.033445 |
| Urine output | -0.000008 |
| Diuretic | 0.011216 |
Tab.2 Characterization coefficients of the selected features
| Trait | Coefficient |
|---|---|
| Age | 0.000264 |
| Heart rate | 0.001311 |
| Systolic blood pressure | -0.000002 |
| Resp rate | 0.000995 |
| Temperature | -0.032731 |
| Peripheral vascular disease | -0.004364 |
| Cerebrovascular disease | 0.034564 |
| Peptic ulcer disease | -0.027540 |
| Mild liver disease | 0.001324 |
| Diabetes with cc | -0.000665 |
| Metastatic solid tumor | 0.202496 |
| Aids | -0.020164 |
| SOFA | 0.004093 |
| SAPS II | 0.000876 |
| GCS min | -0.017186 |
| Weight | -0.000768 |
| White blood cell | 0.008654 |
| Platelet | -0.000094 |
| Blood urea nitrogen | 0.001737 |
| PaO2 | 0.000110 |
| PaCO2 | -0.000313 |
| Lactate min | 0.033445 |
| Urine output | -0.000008 |
| Diuretic | 0.011216 |
| Mode | Accuracy | Precision | F1-score | AUC | AUC (95 %CI) |
|---|---|---|---|---|---|
| LR1 | 0.816 | 0.832 | 0.893 | 0.773 | (0.788, 0.839) |
| AdaBoost1 | 0.841 | 0.861 | 0.906 | 0.767 | (0.688, 0.803) |
| XGBoost1 | 0.845 | 0.855 | 0.909 | 0.829 | (0.785, 0.866) |
| LightGBM1 | 0.837 | 0.854 | 0.904 | 0.836 | (0.697, 0.869) |
| LR2 | 0.805 | 0.808 | 0.891 | 0.757 | (0.686, 0.786) |
| AdaBoost2 | 0.751 | 0.836 | 0.848 | 0.763 | (0.605, 0.779) |
| XGBoost2 | 0.811 | 0.842 | 0.889 | 0.810 | (0.709, 0.829) |
| LightGBM2 | 0.805 | 0.832 | 0.887 | 0.818 | (0.740, 0.846) |
| LR3 | 0.791 | 0.807 | 0.880 | 0.826 | (0.790, 0.841) |
| AdaBoost3 | 0.809 | 0.829 | 0.888 | 0.787 | (0.724, 0.848) |
| XGBoost3 | 0.835 | 0.840 | 0.904 | 0.846 | (0.788, 0.862) |
| LightGBM3 | 0.826 | 0.832 | 0.899 | 0.830 | (0.742, 0.860) |
Tab.3 Comparison of the performance of the 4 models using the 3 dataset
| Mode | Accuracy | Precision | F1-score | AUC | AUC (95 %CI) |
|---|---|---|---|---|---|
| LR1 | 0.816 | 0.832 | 0.893 | 0.773 | (0.788, 0.839) |
| AdaBoost1 | 0.841 | 0.861 | 0.906 | 0.767 | (0.688, 0.803) |
| XGBoost1 | 0.845 | 0.855 | 0.909 | 0.829 | (0.785, 0.866) |
| LightGBM1 | 0.837 | 0.854 | 0.904 | 0.836 | (0.697, 0.869) |
| LR2 | 0.805 | 0.808 | 0.891 | 0.757 | (0.686, 0.786) |
| AdaBoost2 | 0.751 | 0.836 | 0.848 | 0.763 | (0.605, 0.779) |
| XGBoost2 | 0.811 | 0.842 | 0.889 | 0.810 | (0.709, 0.829) |
| LightGBM2 | 0.805 | 0.832 | 0.887 | 0.818 | (0.740, 0.846) |
| LR3 | 0.791 | 0.807 | 0.880 | 0.826 | (0.790, 0.841) |
| AdaBoost3 | 0.809 | 0.829 | 0.888 | 0.787 | (0.724, 0.848) |
| XGBoost3 | 0.835 | 0.840 | 0.904 | 0.846 | (0.788, 0.862) |
| LightGBM3 | 0.826 | 0.832 | 0.899 | 0.830 | (0.742, 0.860) |
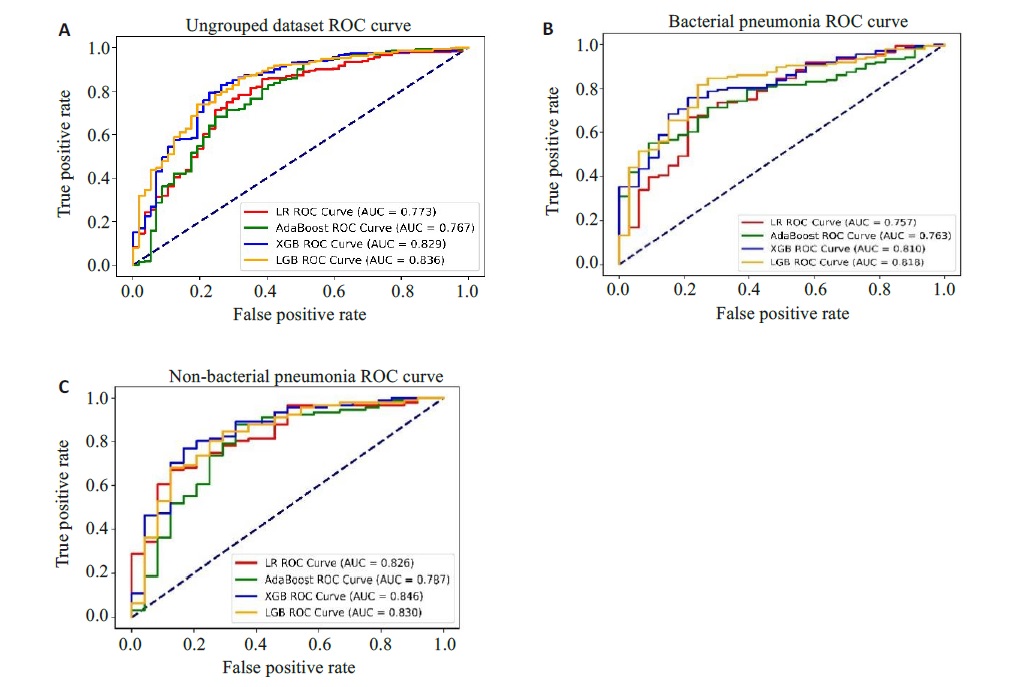
Fig.4 ROC curves of the patients before and after grouping. A: Ungrouped dataset ROC. B: ROC for bacterial pneumonia dataset. C: ROC for non-bacterial pneumonia dataset.
| Mode | Accuracy | Precision | F1-score | AUC | AUC (95% CI) |
|---|---|---|---|---|---|
| LR1 | 0.833 | 0.840 | 0.908 | 0.674 | (0.652, 0.697) |
| AdaBoost1 | 0.815 | 0.856 | 0.894 | 0.746 | (0.639, 0.788) |
| XGBoost1 | 0.827 | 0.851 | 0.903 | 0.691 | (0.654, 0.720) |
| LightGBM 1 | 0.829 | 0.845 | 0.904 | 0.737 | (0.647, 0.770) |
| LR2 | 0.742 | 0.772 | 0.846 | 0.664 | (0.567, 0.753) |
| AdaBoost2 | 0.710 | 0.784 | 0.816 | 0.675 | (0.549, 0.780) |
| XGBoost2 | 0.774 | 0.800 | 0.863 | 0.725 | (0.577, 0.782) |
| LightGBM 2 | 0.772 | 0.801 | 0.862 | 0.699 | (0.569, 0.786) |
Tab.4 Comparison of model performance for patients with bacterial pneumonia and non-bacterial pneumonia from eICU-CRD
| Mode | Accuracy | Precision | F1-score | AUC | AUC (95% CI) |
|---|---|---|---|---|---|
| LR1 | 0.833 | 0.840 | 0.908 | 0.674 | (0.652, 0.697) |
| AdaBoost1 | 0.815 | 0.856 | 0.894 | 0.746 | (0.639, 0.788) |
| XGBoost1 | 0.827 | 0.851 | 0.903 | 0.691 | (0.654, 0.720) |
| LightGBM 1 | 0.829 | 0.845 | 0.904 | 0.737 | (0.647, 0.770) |
| LR2 | 0.742 | 0.772 | 0.846 | 0.664 | (0.567, 0.753) |
| AdaBoost2 | 0.710 | 0.784 | 0.816 | 0.675 | (0.549, 0.780) |
| XGBoost2 | 0.774 | 0.800 | 0.863 | 0.725 | (0.577, 0.782) |
| LightGBM 2 | 0.772 | 0.801 | 0.862 | 0.699 | (0.569, 0.786) |
| 1 | 肖小菊, 黎励文. 《心力衰竭的通用定义和分类》解读[J]. 中国胸心血管外科临床杂志, 2021, 28(10): 1140-4. DOI: 10.7507/1007-4848.202106044 |
| 2 | 马丽媛, 王增武, 樊 静, 等. 《中国心血管健康与疾病报告2022》要点解读[J]. 中国全科医学, 2023, 26(32): 3975-94. DOI: 10.12114/j.issn.1007-9572.2023.0408 |
| 3 | Shen L, Jhund PS, Anand IS, et al. Incidence and outcomes of pneumonia in patients with heart failure[J]. J Am Coll Cardiol, 2021, 77(16): 1961-73. |
| 4 | Bo XW, Zhang YH, Liu Y, et al. Performance of the heart failure risk scores in predicting 1year mortality and short-term readmission of patients[J]. ESC Heart Fail, 2023, 10(1): 502-17. |
| 5 | Wang B, Li YX, Tian Y, et al. Novel pneumonia score based on a machine learning model for predicting mortality in pneumonia patients on admission to the intensive care unit[J]. Respir Med, 2023, 217: 107363. |
| 6 | Theunissen M, Browning J. Putting explainable AI in context: institutional explanations for medical AI[J]. Ethics Inf Technol, 2022, 24(2): 23-9. |
| 7 | Saqr M. Is GDPR failing? a tale of the many challenges in interpretations, applications, and enforcement[J]. Int J Health Sci, 2022, 16(5): 1-2. |
| 8 | 陈珂锐, 孟小峰. 机器学习的可解释性[J]. 计算机研究与发展, 2020, 57(9): 1971-86. DOI: 10.7544/issn1000-1239.2020.20190456 |
| 9 | Rogers P, Wang D, Lu ZY. Medical information mart for intensive care: a foundation for the fusion of artificial intelligence and real-world data[J]. Front Artif Intell, 2021, 4: 691626-35. |
| 10 | Pollard TJ, Johnson AEW, Raffa JD, et al. The eICU Collaborative Research Database, a freely available multi-center database for critical care research[J]. Sci Data, 2018, 5: 180178-83. |
| 11 | Chen YN, Chen H, Lu XD, et al. Automatic ICD-10 coding: deep semantic matching based on analogical reasoning[J]. Heliyon, 2023, 9(4): e15570-6. |
| 12 | 于翠香, 王西艳. 《中国成人医院获得性肺炎与呼吸机相关性肺炎诊断和治疗指南(2018年版)》解读[J]. 中国医刊, 2021, 56(9): 951-3. DOI: 10.3969/j.issn.1008-1070.2021.09.008 |
| 13 | 卓于迪, 朱陵群, 张立山, 等. 套索回归模型在中医临床研究数据的统计应用与R语言实践[J]. 世界中医药, 2023, 18(7): 1033-8. DOI: 10.3969/j.issn.1673-7202.2023.07.023 |
| 14 | 杨 柳, 王 钰. 泛化误差的各种交叉验证估计方法综述[J]. 计算机应用研究, 2015, 32(5): 1287-90, 1297. DOI: 10.3969/j.issn.1001-3695.2015.05.002 |
| 15 | Lynam AL, Dennis JM, Owen KR, et al. Logistic regression has similar performance to optimised machine learning algorithms in a clinical setting: application to the discrimination between type 1 and type 2 diabetes in young adults[J]. Diagn Progn Res, 2020, 4: 6-12. |
| 16 | Amendolara A, Pfister D, Settelmayer M, et al. An overview of machine learning applications in sports injury prediction[J]. Cureus, 2023, 15(9): e46170-8. |
| 17 | Chen RC, Caraka RE, Arnita NE, et al. An end to end of scalable tree boosting system[J]. Sylwan, 2020, 165(1): 1-11. |
| 18 | Li XQ, Xiong XY, Liang ZA, et al. A machine learning diagnostic model for Pneumocystis jirovecii pneumonia in patients with severe pneumonia[J]. Intern Emerg Med, 2023, 18(6): 1741-9. |
| 19 | Xu CG, Li HX, Yang JP, et al. Interpretable prediction of 3-year all-cause mortality in patients with chronic heart failure based on machine learning[J]. BMC Med Inform Decis Mak, 2023, 23(1): 267-79. |
| 20 | Petch J, Di S, Nelson W. Opening the black box: the promise and limitations of explainable machine learning in cardiology[J]. Can J Cardiol, 2022, 38(2): 204-13. |
| 21 | Cho YR, Kang M. Interpretable machine learning in bioinformatics[J]. Methods, 2020, 179: 1-2. |
| 22 | Ma MW, Liu RY, Wen CJ, et al. Predicting the molecular subtype of breast cancer and identifying interpretable imaging features using machine learning algorithms[J]. Eur Radiol, 2022, 32(3): 1652-62. |
| 23 | 鲍利改, 董 谦. 慢性心力衰竭合并肺部感染患者MIP-2、MMP-9、D-D、miR-21表达及与病原菌类型、心肌功能的关联性研究[J]. 临床误诊误治, 2022, 35(3): 78-83. DOI: 10.3969/j.issn.1002-3429.2022.03.018 |
| 24 | Mancini D, Gibson GT. Impact of pneumonia in HeartFailurePatients[J]. J Am Coll Cardiol, 2021, 77(16): 1974-6. |
| 25 | Chen ZJ, Li TM, Guo S, et al. Machine learning-based in-hospital mortality risk prediction tool for intensive care unit patients with heart failure[J]. Front Cardiovasc Med, 2023, 10: 1119699. |
| 26 | Chiotos K, Tamma PD, Gerber JS. Antibiotic stewardship in the intensive care unit: challenges and opportunities[J]. Infect Control Hosp Epidemiol, 2019, 40(6): 693-8. |
| 27 | Bifarin OO. Interpretable machine learning with tree-based shapley additive explanations: application to metabolomics datasets for binary classification[J]. PLoS One, 2023, 18(5): e0284315. |
| 28 | Chen JM, Li Y, Liu P, et al. A nomogram to predict the in-hospital mortality of patients with congestive heart failure and chronic kidney disease[J]. ESC Heart Fail, 2022, 9(5): 3167-76. |
| 29 | Aryee EK, Ozkan B, Ndumele CE. Heart failure and obesity: the latest pandemic[J]. Prog Cardiovasc Dis, 2023, 78: 43-8. |
| 30 | 孟广蕊, 纪志芳, 田 勇. 老年心力衰竭合并肺部感染病原菌分布及血清CRP、PCT水平变化[J]. 中国病原生物学杂志, 2023, 18(7): 821-4, 829. |
| [1] | Lili CHEN, Tianyu WU, Ming ZHANG, Zixia DING, Yan ZHANG, Yiqing YANG, Jiaqian ZHENG, Xiaonan ZHANG. Identification of potential biomarkers and immunoregulatory mechanisms of rheumatoid arthritis based on multichip co-analysis of GEO database [J]. Journal of Southern Medical University, 2024, 44(6): 1098-1108. |
| [2] | Zhiwei ZUO, Qingliang MENG, Jiakang CUI, Kelei GUO, Hua BIAN. An artificial neural network diagnostic model for scleroderma and immune cell infiltration analysis based on mitochondria-associated genes [J]. Journal of Southern Medical University, 2024, 44(5): 920-929. |
| [3] | HE Huishan, GUO Erjia, MENG Wenyi, WANG Yu, WANG Wen, HE Wenle, WU Yuankui, YANG Wei. Predicting cerebral glioma enhancement pattern using a machine learning-based magnetic resonance imaging radiomics model [J]. Journal of Southern Medical University, 2024, 44(1): 194-200. |
| [4] | LUO Xiao, CHENG Yi, WU Cheng, HE Jia. An interpretable machine learning-based prediction model for risk of death for patients with ischemic stroke in intensive care unit [J]. Journal of Southern Medical University, 2023, 43(7): 1241-1247. |
| [5] | GAO Kaiji, WANG Yihao, CAO Haikun, JIA Jianguang. Efficacy of machine learning models versus Cox regression model for predicting prognosis of esophagogastric junction adenocarcinoma [J]. Journal of Southern Medical University, 2023, 43(6): 952-963. |
| [6] | ZENG Pengguihang, TANG Xiuxiao, WU Tingqin, TIAN Qi, LI Mangmang, DING Junjun. Identification of potential regulatory genes for embryonic stem cell self-renewal and pluripotency by random forest [J]. Journal of Southern Medical University, 2021, 41(8): 1234-1242. |
| [7] | . Establishment of naive Bayes classifier-based risk prediction model for chemotherapy-induced nausea and vomiting [J]. Journal of Southern Medical University, 2021, 41(4): 607-612. |
| [8] | . Application of artificial intelligence for detection and classification of colon polyps [J]. Journal of Southern Medical University, 2021, 41(2): 310-312. |
| [9] | CHEN Yonfeng, LI Xiaorong, LAI Weiwei, ZHU Feiyu, TAN Xin, XIAN Wei, KANG Pinfang, WANG Hongju. RIP1/RIP3-MLKL signaling pathway correlates with occurrence, progression and prognosis of chronic heart failure [J]. Journal of Southern Medical University, 2021, 41(10): 1534-1539. |
| [10] | . Inhibition of CD96 enhances interferon-γ secretion by natural killer cells to alleviate lung injury in mice with pulmonary Chlamydia muridarum infection [J]. Journal of Southern Medical University, 2020, 40(07): 930-935. |
| [11] | Relationship between circadian rhythm related brain dysfunction and bipolar disorder. [J]. Journal of Southern Medical University, 2020, 40(06): 822-827. |
| [12] | . Deep learning network-based recognition and localization of diatom images against complex background [J]. Journal of Southern Medical University, 2020, 40(02): 183-189. |
| [13] | . A machine learning model using gut microbiome data for predicting changes of trimethylamine-N-oxide in healthy volunteers after choline consumption [J]. Journal of Southern Medical University, 2017, 37(03): 290-. |
| [14] | . Correlation between left ventricular mass index and NADPH oxidase p22phox in patients with non-valvular chronic heart failure [J]. Journal of Southern Medical University, 2013, 33(01): 142-. |
| [15] | SHEN Qian-bo, XU Ding-li, LIN Sheng, LAI Wen-yan Department of Cardiology, Nanfang Hospital, Southern Medical University, Guangzhou 510515, China. Sleep-disordered breathing and left ventricular remodeling in patients with chronic heart failure [J]. Journal of Southern Medical University, 2006, 26(04): 486-489. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||