Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (4): 837-843.doi: 10.12122/j.issn.1673-4254.2025.04.19
Yaqing YUE( ), Zhaoxia MU, Xibo WANG, Yan LIU(
), Zhaoxia MU, Xibo WANG, Yan LIU( )
)
Received:2024-10-05
Online:2025-04-20
Published:2025-04-28
Contact:
Yan LIU
E-mail:649745448@qq.com;liuyan496@126.com
Yaqing YUE, Zhaoxia MU, Xibo WANG, Yan LIU. Aurora-A overexpression promotes cervical cancer cell invasion and metastasis by activating the NF-κBp65/ARPC4 signaling axis[J]. Journal of Southern Medical University, 2025, 45(4): 837-843.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.04.19
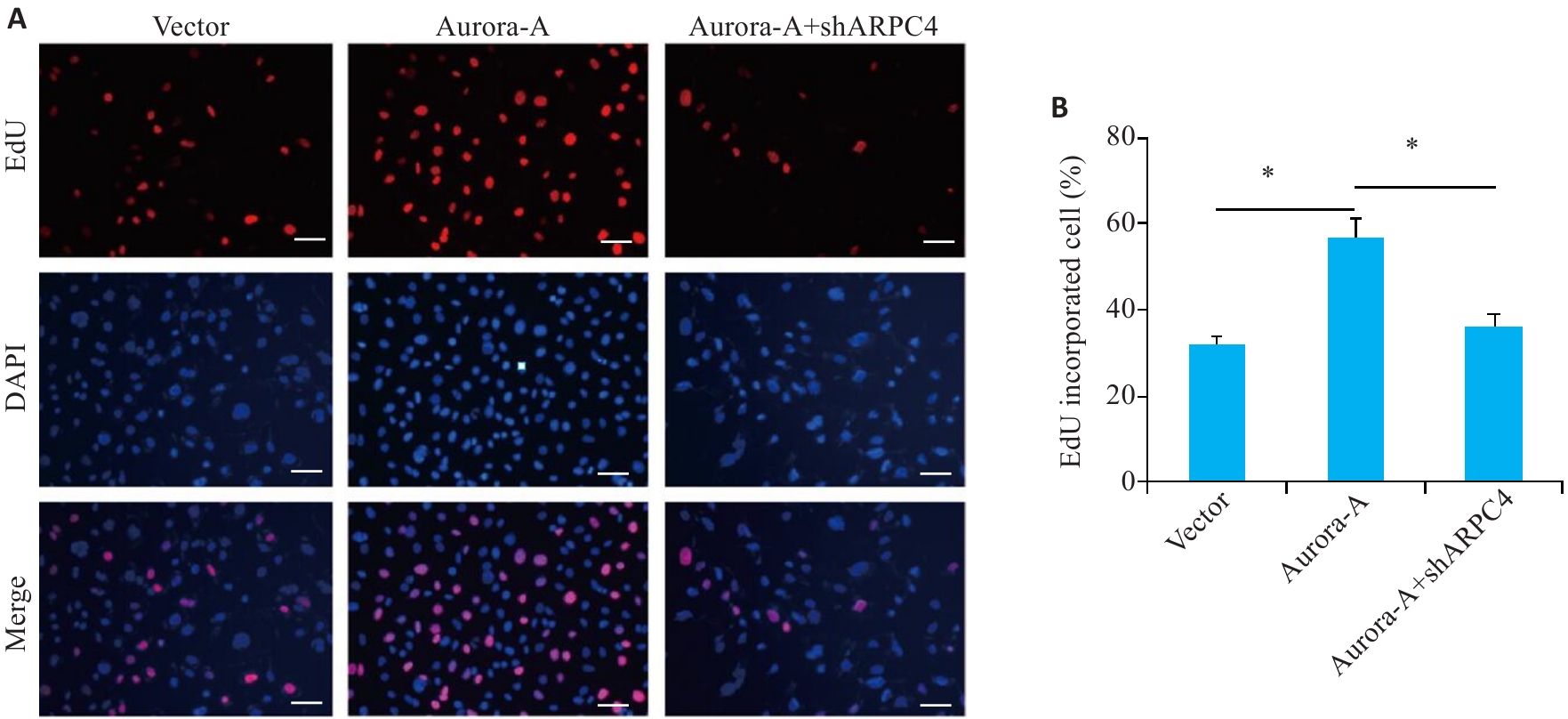
Fig.1 ARPC4 knockdown antagonizes Aurora-A overexpression-induced enhancement of HeLa cell proliferation. A: EDU immunofluorescence staining for detecting cell proliferation in each group (scale bar=200 μm). B: Statistical chart of cell proliferation. *P<0.05.
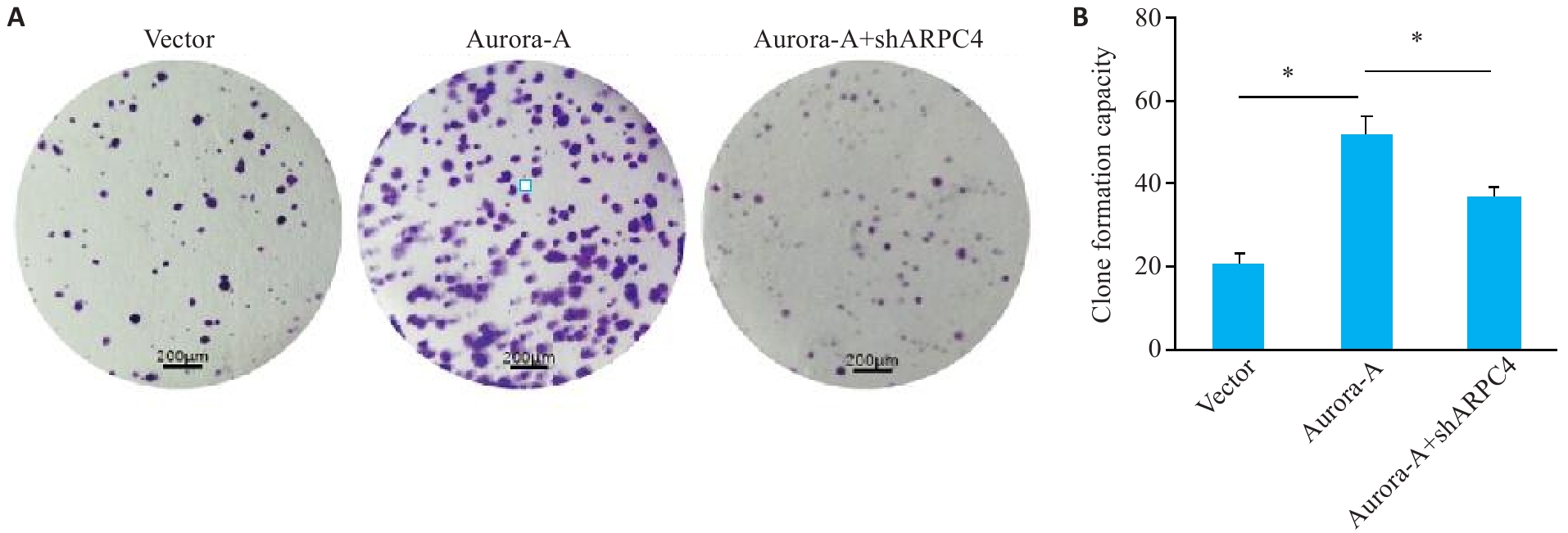
Fig.2 ARPC4 knockdown antagonizes the effect of Aurora-A overexpression for promoting cell colony formation in HeLa cells. A: Colony formation in each group (crystal violet staining, scale bar=200 μm). B: Statistical chart of colony formation. *P<0.05 .
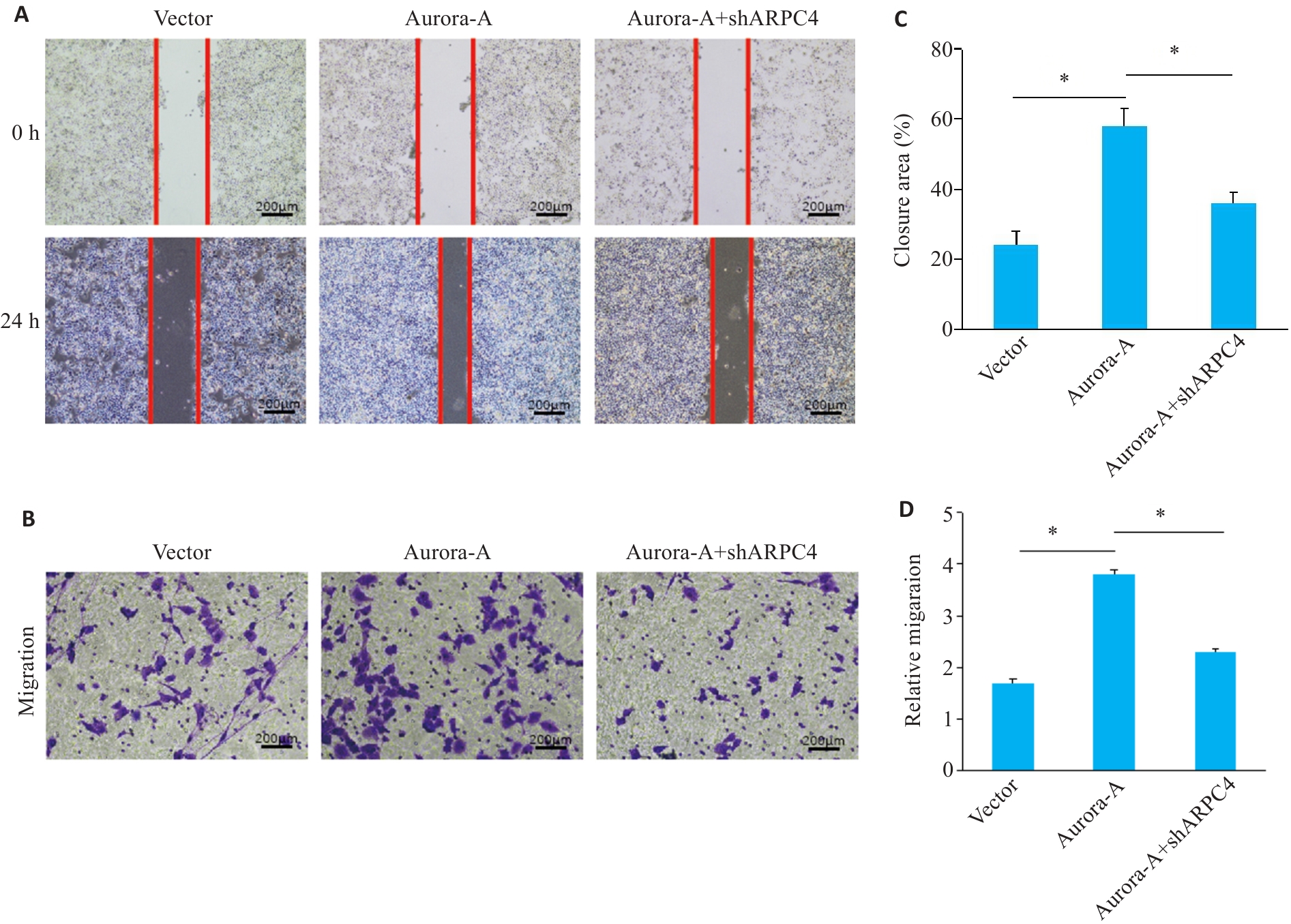
Fig.3 ARPC4 knockdown antagonizes Aurora-A overexpression-induced enhancement of cell migration. A: Scratch assay for assessing migration ability of HeLa cells in each group (scale bar=200 μm). B: Transwell assay for assessing cell migration in each group (Crystal violet staining, scale bar=200 μm). C: Statistical chart of scratch assay in each group; D: Statistical chart of Transwell assay for each group. *P<0.05.
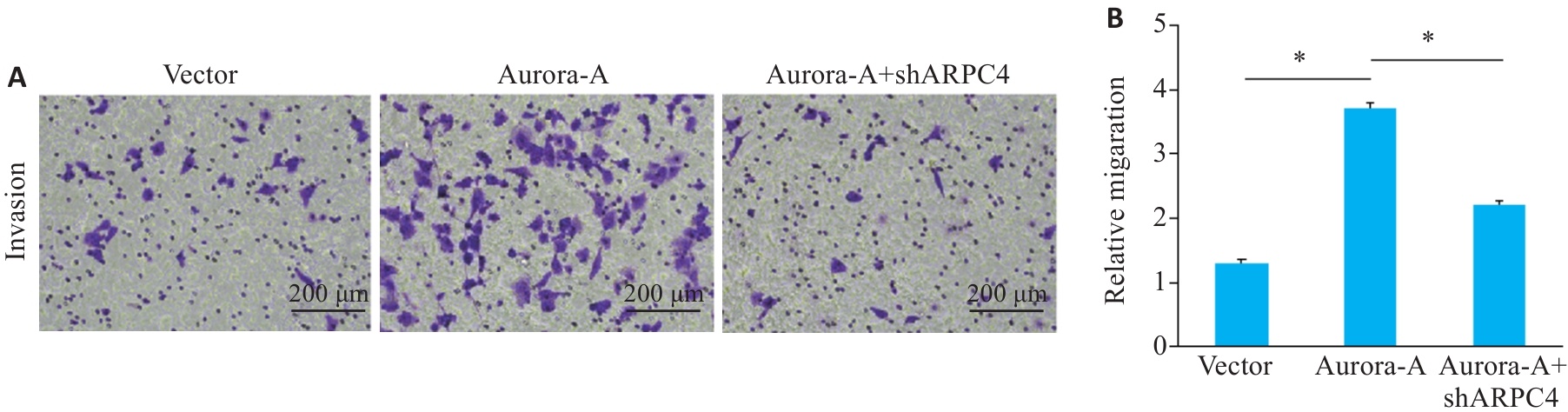
Fig.4 ARPC4 knockdown antagonizes the effect of Aurora-A overexpression for promoting cell invasion. A: Crystal violet staining for observing cell invasion in each group (scale bar=200 μm); B: Statistical chart of the invasive ability of each group. *P<0.05.
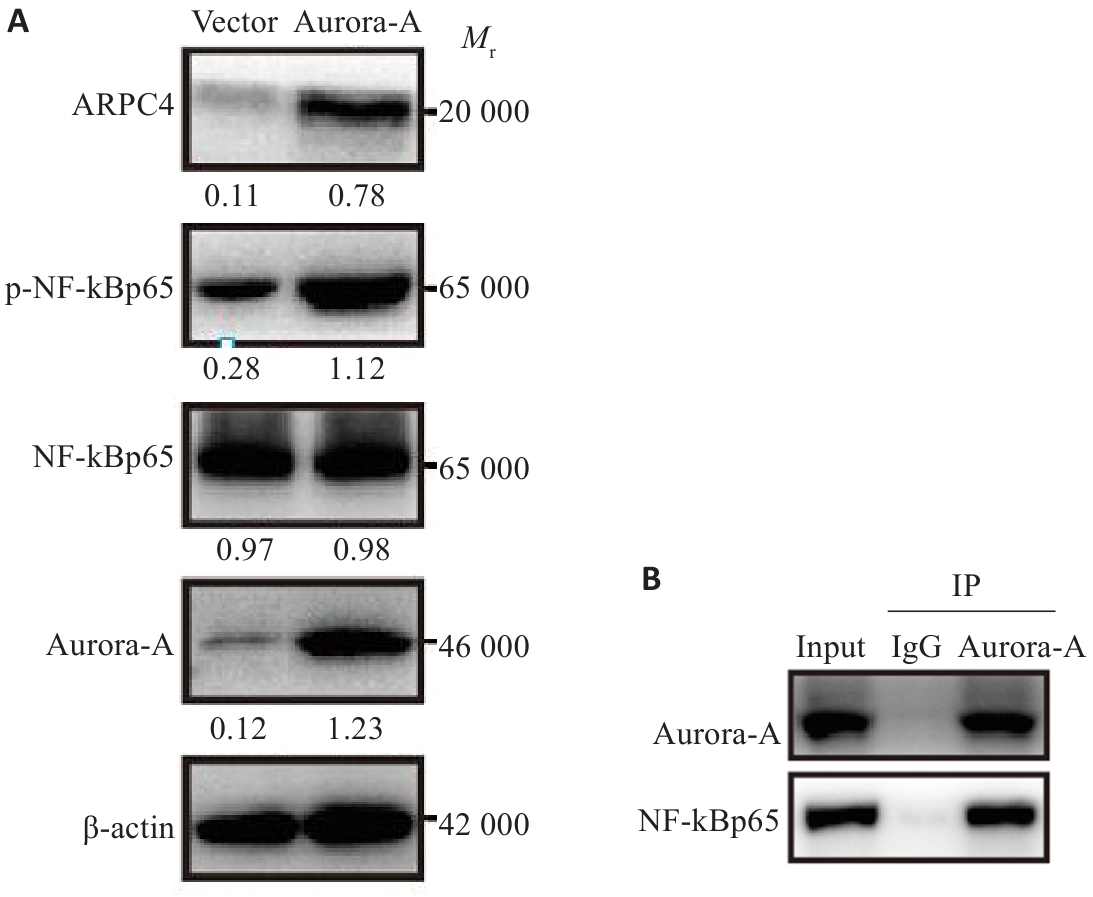
Fig.6 Effect of Aurora-A overexpression on NF-κBp65-ARPC4 signaling pathway in HeLa cells. A: Western blotting for detecting NF-κBp65-ARPC4 signaling pathway proteins in HeLa cells. B: Co-immunoprecipitation result showing interaction between Aurora-A and NF-κBp65.
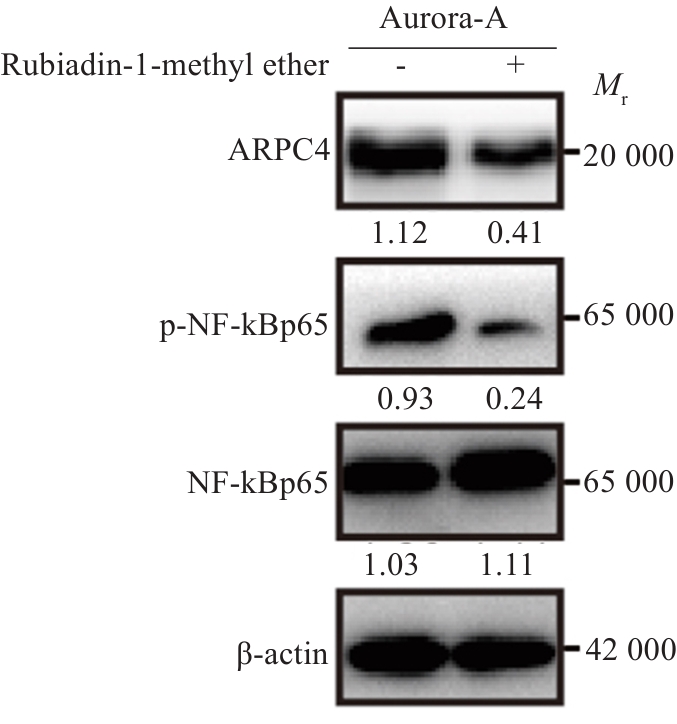
Fig.7 Aurora-A upregulates ARPC4 expression by activating the NF‑κBp65 signaling pathway. The changes in ARPC4, NF‑κBp65, and p-NF‑κBp65 expressions were detected using Western blotting.
| 1 | Ma Z, Zou XX, Yan ZH, et al. Preliminary analysis of cervical cancer immunotherapy[J]. Am J Clin Oncol, 2022, 45(11): 486-90. |
| 2 | Bejar FG, Oaknin A, Williamson C, et al. Novel therapies in gynecologic cancer[J]. Am Soc Clin Oncol Educ Book, 2022, 42: 1-17. |
| 3 | Kumar L, Harish P, Malik PS, et al. Chemotherapy and targeted therapy in the management of cervical cancer[J]. Curr Probl Cancer, 2018, 42(2): 120-8. |
| 4 | Su XJ, Wang SY, Huo YX, et al. Short interfering RNA-mediated silencing of actin-related protein 2/3 complex subunit 4 inhibits the migration of SW620 human colorectal cancer cells[J]. Oncol Lett, 2018, 15(3): 2847-54. |
| 5 | Yokotsuka M, Iwaya K, Saito T, et al. Overexpression of HER2 signaling to WAVE2-Arp2/3 complex activates MMP-independent migration in breast cancer[J]. Breast Cancer Res Treat, 2011, 126(2): 311-8. |
| 6 | Moriya Y, Nohata N, Kinoshita T, et al. Tumor suppressive microRNA-133a regulates novel molecular networks in lung squamous cell carcinoma[J]. J Hum Genet, 2012, 57(1): 38-45. |
| 7 | Kishore AH, Vedamurthy BM, Mantelingu K, et al. Specific small-molecule activator of aurora kinase A induces autophosphorylation in a cell-free system[J]. J Med Chem, 2008, 51(4): 792-7. |
| 8 | Coumar MS, Chu CY, Lin CW, et al. Fast-forwarding hit to lead: aurora and epidermal growth factor receptor kinase inhibitor lead identification[J]. J Med Chem, 2010, 53(13): 4980-8. |
| 9 | Borisa AC, Bhatt HG. A comprehensive review on aurora kinase: small molecule inhibitors and clinical trial studies[J]. Eur J Med Chem, 2017, 140: 1-19. |
| 10 | Lin XR, Xiang XS, Hao LP, et al. The role of Aurora-a in human cancers and future therapeutics[J]. Am J Cancer Res, 2020, 10(9): 2705-29. |
| 11 | Cheng AX, Zhang P, Wang B, et al. Aurora-a mediated phosphorylation of LDHB promotes glycolysis and tumor progression by relieving the substrate-inhibition effect[J]. Nat Commun, 2019, 10(1): 5566. |
| 12 | Sun HZ, Wang HS, Wang X, et al. Aurora-A/SOX8/FOXK1 signaling axis promotes chemoresistance via suppression of cell senescence and induction of glucose metabolism in ovarian cancer organoids and cells[J]. Theranostics, 2020, 10(15): 6928-45. |
| 13 | Zhi JT, Hu LF, Qian YY, et al. Targeting Aurora-a inhibits tumor progression and sensitizes thyroid carcinoma to Sorafenib by decreasing PFKFB3-mediated glycolysis[J]. Cell Death Dis, 2023, 14(3): 224. |
| 14 | Park SI, Lin CP, Ren N, et al. Inhibition of aurora A kinase in combination with chemotherapy induces synthetic lethality and overcomes chemoresistance in myc-overexpressing lymphoma[J]. Target Oncol, 2019, 14(5): 563-75. |
| 15 | Sun HZ, Wang Y, Wang ZL, et al. Aurora-a controls cancer cell radio- and chemoresistance via ATM/Chk2-mediated DNA repair networks[J]. Biochim Biophys Acta, 2014, 1843(5): 934-44. |
| 16 | Wang XB, Huang J, Liu FL, et al. Aurora A kinase inhibition compromises its antitumor efficacy by elevating PD-L1 expression[J]. J Clin Invest, 2023, 133(9): e161929. |
| 17 | Sun SL, Zhou W, Li XX, et al. Nuclear Aurora kinase A triggers programmed death-ligand 1-mediated immune suppression by activating MYC transcription in triple-negative breast cancer[J]. Cancer Commun, 2021, 41(9): 851-66. |
| 18 | Damodaran AP, Vaufrey L, Gavard O, et al. Aurora A kinase is a priori ty pharmaceutical target for the treatment of cancers[J]. Trends Pharmacol Sci, 2017, 38(8): 687-700. |
| 19 | 王恺越, 周怀君. Aurora A激酶与妇科肿瘤[J]. 国际肿瘤学杂志, 2014, 41(2): 117-20. |
| 20 | Zhang K, Wang T, Zhou H, et al. A novel aurora-a inhibitor (MLN8237) synergistically enhances the antitumor activity of sorafenib in hepatocellular carcinoma[J]. Mol Ther Nucleic Acids, 2018, 13: 176-88. |
| 21 | Ding YH, Zhou ZW, Ha CF, et al. Alisertib, an Aurora kinase A inhibitor, induces apoptosis and autophagy but inhibits epithelial to mesenchymal transition in human epithelial ovarian cancer cells[J]. Drug Des Devel Ther, 2015, 9: 425-64. |
| 22 | Bavetsias V, Linardopoulos S. Aurora kinase inhibitors: current status and outlook[J]. Front Oncol, 2015, 5: 278. |
| 23 | O’Connor OA, Özcan M, Jacobsen ED, et al. Randomized phase III study of alisertib or investigator's choice (selected single agent) in patients with relapsed or refractory peripheral T-cell lymphoma[J]. J Clin Oncol, 2019, 37(8): 613-23. |
| 24 | Kanamori S, Kajihara I, Kanazawa-Yamada S, et al. Expression of aurora kinase A expression in dermatofibrosarcoma protuberans[J]. J Dermatol, 2018, 45(4): 507-8. |
| 25 | Lykkesfeldt AE, Iversen BR, Jensen MB, et al. Aurora kinase A as a possible marker for endocrine resistance in early estrogen receptor positive breast cancer[J]. Acta Oncol, 2018, 57(1): 67-73. |
| 26 | Guo MJ, Lu SC, Huang HM, et al. Increased AURKA promotes cell proliferation and predicts poor prognosis in bladder cancer[J]. BMC Syst Biol, 2018, 12(): 118. |
| 27 | 陈远健. Aurora-A激酶的作用及其在结肠癌发生发展中的研究进展[J]. 医学理论与实践, 2023, 36(13): 2190-2, 2181. |
| 28 | Chiu SC, Chen KC, Hsia JY, et al. Overexpression of Aurora-a bypasses cytokinesis through phosphorylation of suppressed in lung cancer[J]. Am J Physiol Cell Physiol, 2019, 317(3): C600-12. |
| 29 | 左彤彤, 周卫萍. 神经母细胞瘤的分子生物学特性和靶向药物临床研究进展[J]. 中国肿瘤临床, 2021, 48(8): 426-31. |
| 30 | Wang ZH, Ma Z, Cao JP. Effects of repeated aurora-a siRNA transfection on Cilia generation and proliferation of SK-MES-1 or A549 cells[J]. Cancer Biother Radiopharm, 2018, 33(3): 110-7. |
| 31 | Heo SK, Noh EK, Jeong YK, et al. Radotinib inhibits mitosis entry in acute myeloid leukemia cells via suppression of Aurora kinase A expression[J]. Tumour Biol, 2019, 41(5): 1010428319848612. |
| 32 | Farmer H, McCabe N, Lord CJ, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy[J]. Nature, 2005, 434(7035): 917-21. |
| 33 | Sankaran S, Crone DE, Palazzo RE, et al. Aurora-a kinase regulates breast cancer associated gene 1 inhibition of centrosome-dependent microtubule nucleation[J]. Cancer Res, 2007, 67(23): 11186-94. |
| 34 | 许文兵. 子宫颈上皮内瘤变和子宫颈鳞癌中ARPC2/3蛋白的表达及意义[J]. 吉林医学, 2013, 34(32): 6674-5. |
| 35 | 董 洁, 胡观丽, 况 蕾, 等. 宫颈鳞癌组织中TPX2和Aurora-A蛋白的表达水平及预后意义[J]. 安徽医药, 2019, 23(10): 2018-21. |
| 36 | 张 鹏. 激酶Aurora A调控肿瘤代谢与氧化应激的机制探究[D]. 合肥: 中国科学技术大学, 2020. |
| 37 | 瞿根义. ARPC4调控细胞骨架对膀胱癌侵袭转移的作用和机制研究[D]. 福州: 福建医科大学, 2017. |
| [1] | Shunjie QING, Zhiyong SHEN. High expression of hexokinase 2 promotes proliferation, migration and invasion of colorectal cancer cells by activating the JAK/STAT pathway and regulating tumor immune microenvironment [J]. Journal of Southern Medical University, 2025, 45(3): 542-553. |
| [2] | Qingqing HUANG, Wenjing ZHANG, Xiaofeng ZHANG, Lian WANG, Xue SONG, Zhijun GENG, Lugen ZUO, Yueyue WANG, Jing LI, Jianguo HU. High MYO1B expression promotes proliferation, migration and invasion of gastric cancer cells and is associated with poor patient prognosis [J]. Journal of Southern Medical University, 2025, 45(3): 622-631. |
| [3] | Jinhua ZOU, Hui WANG, Dongyan ZHANG. SLC1A5 overexpression accelerates progression of hepatocellular carcinoma by promoting M2 polarization of macrophages [J]. Journal of Southern Medical University, 2025, 45(2): 269-284. |
| [4] | Yu BIN, Ziwen LI, Suwei ZUO, Sinuo SUN, Min LI, Jiayin SONG, Xu LIN, Gang XUE, Jingfang WU. High expression of apolipoprotein C1 promotes proliferation and inhibits apoptosis of papillary thyroid carcinoma cells by activating the JAK2/STAT3 signaling pathway [J]. Journal of Southern Medical University, 2025, 45(2): 359-370. |
| [5] | Zhoufang CAO, Yuan WANG, Mengna WANG, Yue SUN, Feifei LIU. LINC00837/miR-671-5p/SERPINE2 functional axis promotes pathological processes of fibroblast-like synovial cells in rheumatoid arthritis [J]. Journal of Southern Medical University, 2025, 45(2): 371-378. |
| [6] | Xiaohua CHEN, Hui LU, Ziliang WANG, Lian WANG, Yongsheng XIA, Zhijun GENG, Xiaofeng ZHANG, Xue SONG, Yueyue WANG, Jing LI, Jianguo HU, Lugen ZUO. Role of Abelson interactor 2 in progression and prognosis of gastric cancer and its regulatory mechanisms [J]. Journal of Southern Medical University, 2024, 44(9): 1653-1661. |
| [7] | Liangjun XUE, Qiuyu TAN, Jingwen XU, Lu FENG, Wenjin LI, Liang YAN, Yulei LI. MiR-6838-5p overexpression inhibits proliferation of breast cancer MCF-7 cells by downregulating DDR1 expression [J]. Journal of Southern Medical University, 2024, 44(9): 1677-1684. |
| [8] | Kai JI, Guanyu YU, Leqi ZHOU, Tianshuai ZHANG, Qianlong LING, Wenjiang MAN, Bing ZHU, Wei ZHANG. HNRNPA1 gene is highly expressed in colorectal cancer: its prognostic implications and potential as a therapeutic target [J]. Journal of Southern Medical University, 2024, 44(9): 1685-1695. |
| [9] | Yidan PANG, Ya LIU, Siai CHEN, Jinglei ZHANG, Jin ZENG, Yuanming PAN, Juan AN. Biological role of SPAG5 in the malignant proliferation of gastric cancer cells [J]. Journal of Southern Medical University, 2024, 44(8): 1497-1507. |
| [10] | Xiaofan CONG, Teng CHEN, Shuo LI, Yuanyuan WANG, Longyun ZHOU, Xiaolong LI, Pei ZHANG, Xiaojin SUN, Surong ZHAO. Dihydroartemisinin enhances sensitivity of nasopharyngeal carcinoma HNE1/DDP cells to cisplatin-induced apoptosis by promoting ROS production [J]. Journal of Southern Medical University, 2024, 44(8): 1553-1560. |
| [11] | Wenran HU, Rong FU. Trans-YOLOv5: a YOLOv5-based prior transformer network model for automated detection of abnormal cells or clumps in cervical cytology images [J]. Journal of Southern Medical University, 2024, 44(7): 1217-1226. |
| [12] | Mengdong ZHENG, Yan LIU, Jiaojiao LIU, Qiaozhen KANG, Ting WANG. Effect of deletion of protein 4.1R on proliferation, apoptosis and glycolysis of hepatocyte HL-7702 cells [J]. Journal of Southern Medical University, 2024, 44(7): 1355-1360. |
| [13] | Huaxing HE, Lulin LIU, Yingyin LIU, Nachuan CHEN, Suxia SUN. Sodium butyrate and sorafenib synergistically inhibit hepatocellular carcinoma cells possibly by inducing ferroptosis through inhibiting YAP [J]. Journal of Southern Medical University, 2024, 44(7): 1425-1430. |
| [14] | Jincun FANG, Liwei LIU, Junhao LIN, Fengsheng CHEN. Overexpression of CDHR2 inhibits proliferation of breast cancer cells by inhibiting the PI3K/Akt pathway [J]. Journal of Southern Medical University, 2024, 44(6): 1117-1125. |
| [15] | Yongsheng XIA, Lian WANG, Xiaohua CHEN, Yulu ZHANG, Aofei SUN, Deli CHEN. TSR2 overexpression inhibits proliferation and invasion of gastric cancer cells by downregulating the PI3K/AKT signaling pathway [J]. Journal of Southern Medical University, 2024, 44(5): 913-919. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||