Journal of Southern Medical University ›› 2024, Vol. 44 ›› Issue (10): 1866-1873.doi: 10.12122/j.issn.1673-4254.2024.10.04
Xueyan XI( ), Ting DENG, Boyu DU(
), Ting DENG, Boyu DU( )
)
Received:2024-07-23
Online:2024-10-20
Published:2024-10-31
Contact:
Boyu DU
E-mail:xixueyan2001@126.com;du.boyu@hotmail.com
Supported by:Xueyan XI, Ting DENG, Boyu DU. Colorectal fibroblasts promote malignant phenotype of colorectal cancer cells by activating the ERK signaling pathway[J]. Journal of Southern Medical University, 2024, 44(10): 1866-1873.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2024.10.04
| Gene name | Primer sequences |
|---|---|
| CD29 | Up: 5'-TCCAACCTGATCCTGTGTCC-3' |
| Down: 5'-ACAATTCCAGCAACCACACC-3' | |
| CD44 | Up: 5'-GGCACCCGCTATGTCCAGAA-3' |
| Down: 5'-CCTCCTGAAGTGCTGCTCCT-3' | |
| CD166 | Up: 5'-GTCTGCTCTTCTGCCTCTTG-3' |
| Down: 5'-CGTCAAGTCGGCAAGGTATG-3' | |
| MYC | Up: 5'- CGTCTCCACACATCAGCACAA-3' |
| Down: 5'-TCTTGGCAGCAGGATAGTCCTT -3' | |
| EPCAM | Up: 5'-GGCTCTTTAAGGCCAAGCAG-3' |
| Down: 5'-CCAGTAGGTTCTCACTCGCT-3' | |
| GAPDH | Up:5'-AGCTCACTGGCATGGCCTTC-3' |
| Down: 5'-CGCCTGCTTCACCACCTTCT-3' |
Tab.1 Primer sequences for RT-PCR
| Gene name | Primer sequences |
|---|---|
| CD29 | Up: 5'-TCCAACCTGATCCTGTGTCC-3' |
| Down: 5'-ACAATTCCAGCAACCACACC-3' | |
| CD44 | Up: 5'-GGCACCCGCTATGTCCAGAA-3' |
| Down: 5'-CCTCCTGAAGTGCTGCTCCT-3' | |
| CD166 | Up: 5'-GTCTGCTCTTCTGCCTCTTG-3' |
| Down: 5'-CGTCAAGTCGGCAAGGTATG-3' | |
| MYC | Up: 5'- CGTCTCCACACATCAGCACAA-3' |
| Down: 5'-TCTTGGCAGCAGGATAGTCCTT -3' | |
| EPCAM | Up: 5'-GGCTCTTTAAGGCCAAGCAG-3' |
| Down: 5'-CCAGTAGGTTCTCACTCGCT-3' | |
| GAPDH | Up:5'-AGCTCACTGGCATGGCCTTC-3' |
| Down: 5'-CGCCTGCTTCACCACCTTCT-3' |
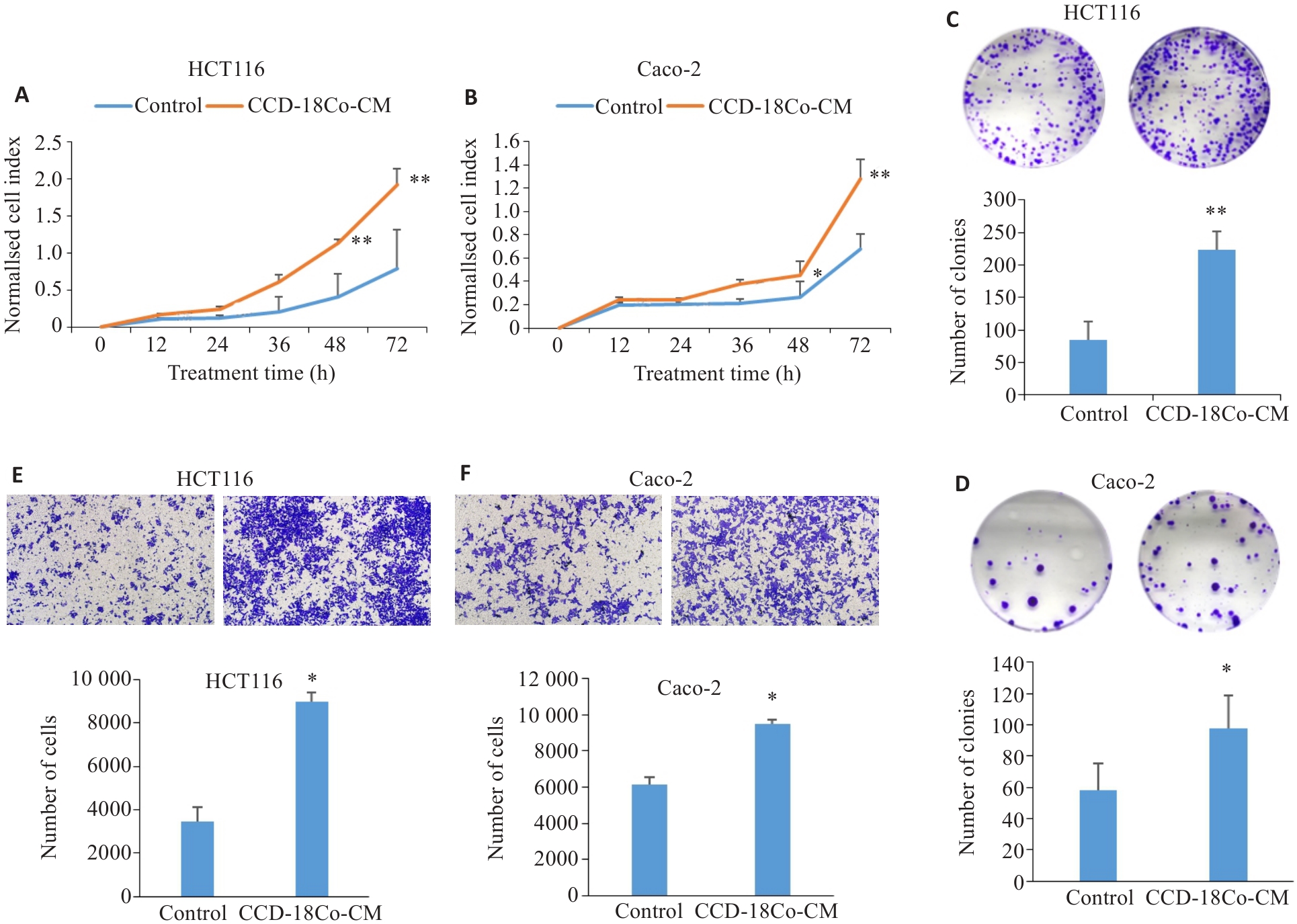
Fig.1 CCD-18Co-CM promotes proliferation (A, B), clone formation (C, D) and migration (E, F; original magnification: ×100) of CRC cells analyzed using real-time cellular analysis, colony forming assay and Transwell assay (Mean±SD, n=3). *P<0.05, **P<0. 01 vs control.
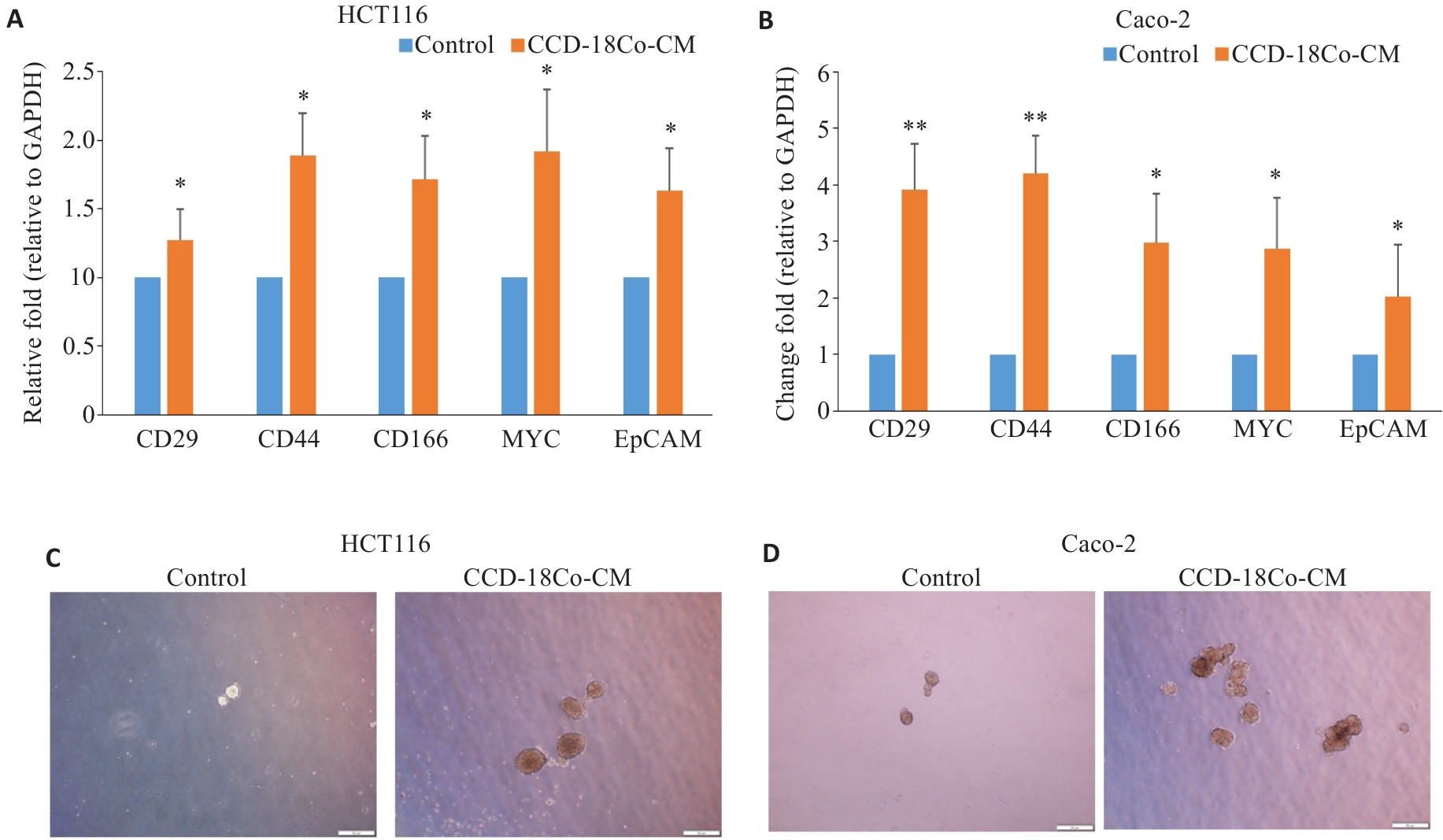
Fig.2 CCD-18Co-CM promotes stemness characteristics of CRC cells. A, B: Relative mRNA expression levels of CD29, CD44, CD166, MYC and EPCAM in HCT116 and Caco-2 cells after CCD-18Co-CM treatment detected by RT-qPCR (Mean±SD, n=3). C, D: Morphology of the tumor spheres formed by HCT116 and Caco-2 cells after CCD-18Co-CM treatment (Scale bar = 50 μm). *P<0.05, **P<0.01 vs control.
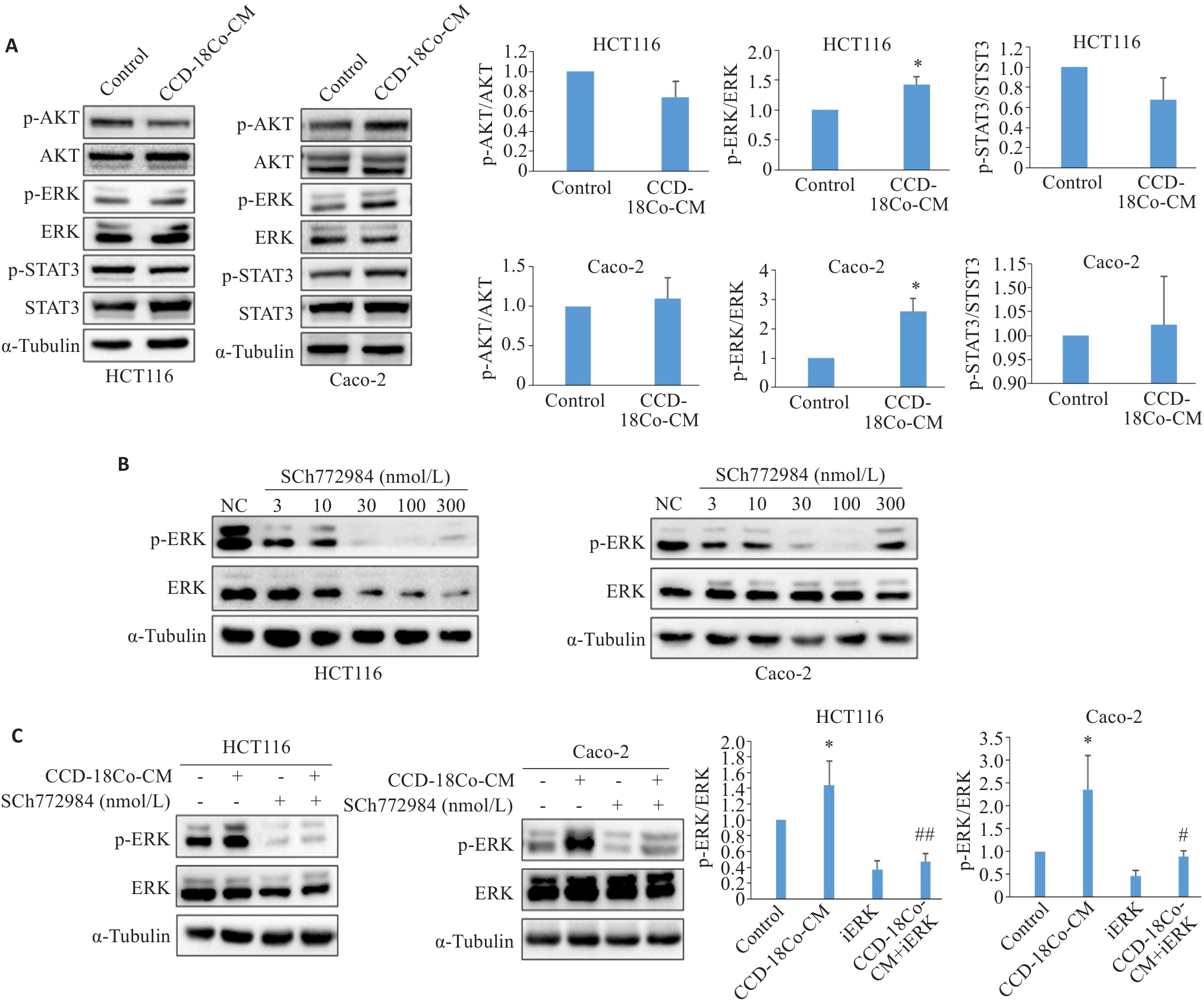
Fig.3 CCD-18Co-CM activates the ERK signaling pathway in CRC cells. A: Western blotting for detecting expression levels of STAT3, p-STAT3, AKT, p-AKT, ERK and p-ERK proteins in HCT116 and Caco-2 cells treated with CCD-18Co-CM. B: Western blotting for detecting expression levels of ERK and p-ERK in HCT116 and Caco-2 cells treated with different concentrations of SCH772984. C: Western blotting for detecting expression levels of ERK and p-ERK in HCT116 and Caco-2 cells after combined treatment with CCD-18Co-CM and 100 nmol/L SCH772984. Data are presented as Mean±SD (n=3). *P<0.05 vs control; #P<0.05, ##P<0.01 vs CCD-18Co-CM.
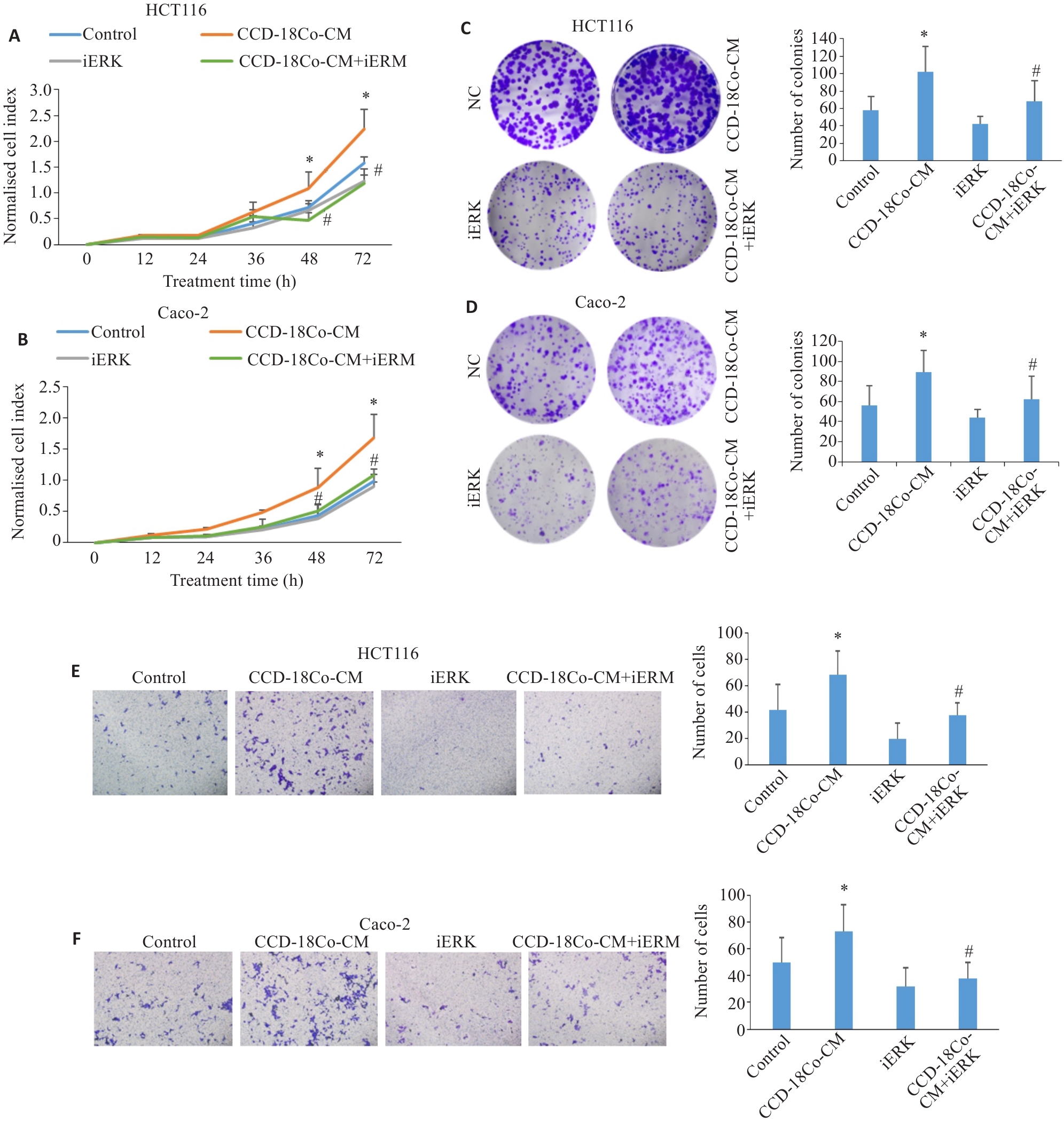
Fig.4 SCH772984 (iERK) inhibits CCD-18Co-CM-induced proliferation, clone formation, and migration of CRC cells. A, B: RTCA for assessing proliferation of HCT116 and Caco-2 cells treated with CCD-18Co-CM and iERK (100 nmol/L). C, D: Colony-forming assay of HCT116 and Caco-2 cells treated with CCD-18Co-CM and 100 nmol/L iERK (×100). E, F:Transwell assay of HCT116 and Caco-2 cells treated with CCD-18Co-CM and 100 nmol/L iERK (×100). Data are presented as Mean±SD (n=3). *P<0.05 vs control, #P<0.05 vs CCD-18Co-CM.
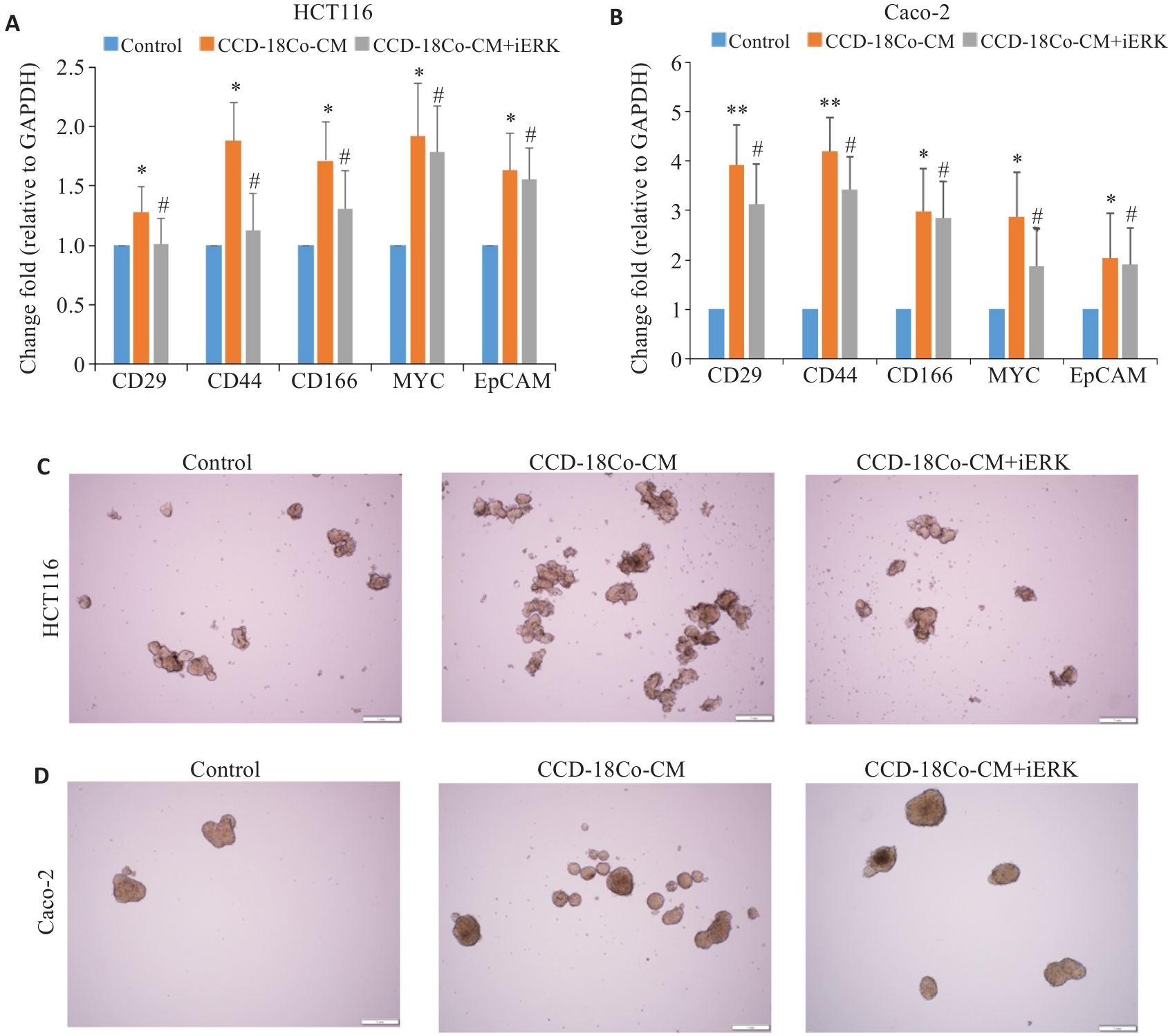
Fig.5 iERK decreases cancer stemness of CRC cells induced by CCD-18Co-CM. A, B: RT-qPCR for detecting mRNA expression levels of stemness-related genes in HCT116 and Caco-2 cells treated with CCD-18Co-CM and SCH772984 (Mean±SD, n=3). C, D: Morphology of tumor spheres formed by HCT116 and Caco-2 cells after CCD-18Co-CM and SCH772984 treatment (Scale bar=1 mm). *P<0.05, **P<0.01 vs control; #P<0.05 vs CCD-18Co-CM.
| 1 | Dyba T, Randi G, Bray F, et al. The European cancer burden in 2020: incidence and mortality estimates for 40 countries and 25 major cancers[J]. Eur J Cancer, 2021, 157: 308-47. |
| 2 | Arnold M, Sierra MS, Laversanne M, et al. Global patterns and trends in colorectal cancer incidence and mortality[J]. Gut, 2017, 66(4): 683-91. |
| 3 | Mao XQ, Xu J, Wang W, et al. Crosstalk between cancer-associated fibroblasts and immune cells in the tumor microenvironment: new findings and future perspectives[J]. Mol Cancer, 2021, 20(1): 131. |
| 4 | Bejarano L, Jordāo MJC, Joyce JA. Therapeutic targeting of the tumor microenvironment[J]. Cancer Discov, 2021, 11(4): 933-59. |
| 5 | Tiwari A, Trivedi R, Lin SY. Tumor microenvironment: barrier or opportunity towards effective cancer therapy[J]. J Biomed Sci, 2022, 29(1): 83. |
| 6 | Verginadis II, Avgousti H, Monslow J, et al. A stromal Integrated Stress Response activates perivascular cancer-associated fibroblasts to drive angiogenesis and tumour progression[J]. Nat Cell Biol, 2022, 24(6): 940-53. |
| 7 | Sahai E, Astsaturov I, Cukierman E, et al. A framework for advancing our understanding of cancer-associated fibroblasts[J]. Nat Rev Cancer, 2020, 20(3): 174-86. |
| 8 | Fang T, Lv HW, Lv GS, et al. Tumor-derived exosomal miR-1247-3p induces cancer-associated fibroblast activation to foster lung metastasis of liver cancer[J]. Nat Commun, 2018, 9(1): 191. |
| 9 | Chen MH, Gu YY, Zhang AL, et al. Biological effects and mechanisms of matrine and other constituents of Sophora flavescens in colorectal cancer[J]. Pharmacol Res, 2021, 171: 105778. |
| 10 | Rausio H, Cervera A, Heuser VD, et al. PIK3R1 fusion drives chemoresistance in ovarian cancer by activating ERK1/2 and inducing rod and ring-like structures[J]. Neoplasia, 2024, 51: 100987. |
| 11 | 邓 婷, 杜伯雨, 郗雪艳. 结直肠癌细胞通过激活成纤维细胞的ERK通路诱导癌症相关成纤维细胞的形成[J]. 南方医科大学学报, 2023, 43(6): 943-51. |
| 12 | Correa-Gallegos D, Jiang DS, Rinkevich Y. Fibroblasts as confederates of the immune system[J]. Immunol Rev, 2021, 302(1): 147-62. |
| 13 | Gong Z, Li Q, Shi JY, et al. Lung fibroblasts facilitate pre-metastatic niche formation by remodeling the local immune microenvironment[J]. Immunity, 2022, 55(8): 1483-500. e9. |
| 14 | Chen W, Chen YW, Su J, et al. CaMKII mediates TGFβ1-induced fibroblasts activation and its cross talk with colon cancer cells[J]. Dig Dis Sci, 2022, 67(1): 134-45. |
| 15 | Najafi M, Farhood B, Mortezaee K. Cancer stem cells (CSCs) in cancer progression and therapy[J]. J Cell Physiol, 2019, 234(6): 8381-95. |
| 16 | Angius A, Scanu AM, Arru C, et al. Portrait of cancer stem cells on colorectal cancer: molecular biomarkers, signaling pathways and miRNAome[J]. Int J Mol Sci, 2021, 22(4): 1603. |
| 17 | Ferrer-Mayorga G, Niell N, Cantero R, et al. Vitamin D and Wnt3A have additive and partially overlapping modulatory effects on gene expression and phenotype in human colon fibroblasts[J]. Sci Rep, 2019, 9(1): 8085. |
| 18 | Dias Carvalho P, Mendonça S, Martins F, et al. Modulation of fibroblast phenotype by colorectal cancer cell-secreted factors is mostly independent of oncogenic KRAS[J]. Cells, 2022, 11(16): 2490. |
| 19 | Hassametto A, Tanomrat R, Muangthong T, et al. Role of oxidative stress-dependent C/EBPβ expression on CAF transformation inducing HCT116 colorectal cancer cell progression; migration and invasion[J]. Asian Pac J Cancer Prev, 2023, 24(11): 3825-35. |
| 20 | Si GF, Li SY, Zheng Q, et al. MiR-1246 shuttling from fibroblasts promotes colorectal cancer cell migration[J]. Neoplasma, 2021, 68(2): 317-24. |
| 21 | Yoshida GJ. Regulation of heterogeneous cancer-associated fibroblasts: the molecular pathology of activated signaling pathways[J]. J Exp Clin Cancer Res, 2020, 39(1): 112. |
| 22 | Mhaidly R, Mechta-Grigoriou F. Role of cancer-associated fibroblast subpopulations in immune infiltration, as a new means of treatment in cancer[J]. Immunol Rev, 2021, 302(1): 259-72. |
| 23 | Widjaja AA, Chothani S, Viswanathan S, et al. IL11 stimulates IL33 expression and proinflammatory fibroblast activation across tissues[J]. Int J Mol Sci, 2022, 23(16): 8900. |
| 24 | Pein M, Insua-Rodríguez J, Hongu T, et al. Metastasis-initiating cells induce and exploit a fibroblast niche to fuel malignant colonization of the lungs[J]. Nat Commun, 2020, 11(1): 1494. |
| 25 | Takatsu F, Suzawa K, Tomida S, et al. Periostin secreted by cancer-associated fibroblasts promotes cancer progression and drug resistance in non-small cell lung cancer[J]. J Mol Med, 2023, 101(12): 1603-14. |
| 26 | Tian BQ, Chen XJ, Zhang HH, et al. Urokinase plasminogen activator secreted by cancer-associated fibroblasts induces tumor progression via PI3K/AKT and ERK signaling in esophageal squamous cell carcinoma[J]. Oncotarget, 2017, 8(26): 42300-13. |
| 27 | Liu L, Liu SC, Luo HJ, et al. GPR30-mediated HMGB1 upregulation in CAFs induces autophagy and tamoxifen resistance in ERα‑positive breast cancer cells[J]. Aging, 2021, 13(12): 16178-97. |
| 28 | Tayama H, Karasawa H, Yamamura A, et al. The association between ERK inhibitor sensitivity and molecular characteristics in colorectal cancer[J]. Biochem Biophys Res Commun, 2021, 560: 59-65. |
| 29 | Lin K, Zhao Y, Tang YQ, et al. Collagen I-induced VCAN/ERK signaling and PARP1/ZEB1-mediated metastasis facilitate OSBPL2 defect to promote colorectal cancer progression[J]. Cell Death Dis, 2024, 15(1): 85. |
| 30 | Liu W, Tang JT, Gao W, et al. PPP2R1B abolishes colorectal cancer liver metastasis and sensitizes Oxaliplatin by inhibiting MAPK/ERK signaling pathway[J]. Cancer Cell Int, 2024, 24(1): 90. |
| [1] | Kai JI, Guanyu YU, Leqi ZHOU, Tianshuai ZHANG, Qianlong LING, Wenjiang MAN, Bing ZHU, Wei ZHANG. HNRNPA1 gene is highly expressed in colorectal cancer: its prognostic implications and potential as a therapeutic target [J]. Journal of Southern Medical University, 2024, 44(9): 1685-1695. |
| [2] | Yinliang ZHANG, Zetan LUO, Rui ZHAO, Na ZHAO, Zhidong XU, Di AO, Guyi CONG, Xinyu LIU, Hailun ZHENG. Sanguinarine induces ferroptosis of colorectal cancer cells by upregulating STUB1 and downregulating GPX4 [J]. Journal of Southern Medical University, 2024, 44(8): 1537-1544. |
| [3] | Jinguang LUO, Huaixiang TAO, Zhiyuan WEN, Long CHEN, Hao HU, Han GUAN. Tumor-associated fibroblasts promotes proliferation and migration of prostate cancer cells by suppressing FBXL3 via upregulating hsa-miR-18b-5p [J]. Journal of Southern Medical University, 2024, 44(7): 1284-1296. |
| [4] | Heping LI, Gaohua LI, Xuehua ZHANG, Yanan WANG. Genetic drivers for inflammatory protein markers in colorectal cancer: a Mendelian randomization approach to clinical prognosis study [J]. Journal of Southern Medical University, 2024, 44(7): 1361-1370. |
| [5] | Nan WANG, Bin SHI, Xiaolan MAN, Weichao WU, Jia CAO. High expression of fragile X mental retardation protein inhibits ferroptosis of colorectal tumor cells by activating the RAS/MAPK signaling pathway [J]. Journal of Southern Medical University, 2024, 44(5): 885-893. |
| [6] | RONG Shengwei, LI Hongfang, WEI Yiran, FENG Zihang, GAN Lu, DENG Zhonghao, ZHAO Liang. Zinc finger protein-36 deficiency inhibits osteogenic differentiation of mouse bone marrow-derived mesenchymal stem cells and preosteoblasts by activating the ERK/MAPK pathway [J]. Journal of Southern Medical University, 2024, 44(4): 697-705. |
| [7] | WANG Zining, YANG Ming, LI Shuanglei, CHI Haitao, WANG Junhui, XIAO Cangsong. A transcriptomic analysis of correlation between mitochondrial function and energy metabolism remodeling in mice with myocardial fibrosis following myocardial infarction [J]. Journal of Southern Medical University, 2024, 44(4): 666-674. |
| [8] | SHAO Shan, BAI Weichao, ZHOU Pengcheng, LUO Minna, ZHAO Xinhan, LEI Jianjun. Metformin suppresses hypoxia-inducible factor-1α expression in cancer-associated fibroblasts to block tumor-stromal cross-talk in breast cancer [J]. Journal of Southern Medical University, 2024, 44(3): 428-436. |
| [9] | YAN Chang, LIU Shuang, SONG Qingzhi, HU Yibing. Metformin inhibits self-renewal of colorectal cancer stem cells by inhibiting mitochondrial oxidative phosphorylation [J]. Journal of Southern Medical University, 2023, 43(8): 1279-1286. |
| [10] | WEI Ke, SHI Jiwen, XIAO Yuhan, WANG Wenrui, YANG Qingling, CHEN Changjie. MiR-30e-5p overexpression promotes proliferation and migration of colorectal cancer cells by activating the CXCL12 axis via downregulating PTEN [J]. Journal of Southern Medical University, 2023, 43(7): 1081-1092. |
| [11] | ZHANG Xuefang, CHEN Yanhua, LI Zongheng, SHANG Jing, YUAN Zeting, DENG Wanli, LUO Ying, HAN Na, YIN Peihao, YIN Jun. Analysis of therapeutic mechanism of Liushen Wan against colitis-associated colorectal cancer based on network pharmacology and validation in mice [J]. Journal of Southern Medical University, 2023, 43(7): 1051-1062. |
| [12] | DENG Ting, DU Boyu, XI Xueyan. Colorectal cancer cells induce the formation of cancer-associated fibroblasts by activating the ERK signaling pathway in fibroblasts [J]. Journal of Southern Medical University, 2023, 43(6): 943-951. |
| [13] | MA Zhennan, ZHAO Xuefeng, ZHANG Xiaowei, XU Guangda, LIU Fuquan. DTX2 overexpression promotes migration and invasion of colorectal cancer cells through the Notch2/Akt axis [J]. Journal of Southern Medical University, 2023, 43(3): 340-348. |
| [14] | WANG Xuancheng, ZHU Yifan, ZHOU Hailin, HUANG Zongsheng, CHEN Hongwei, ZHANG Jiahao, YANG Shanyi, CHEN Guanghui, ZHANG Qisong. Integrated analysis of serum untargeted metabolomics and targeted bile acid metabolomics for identification of diagnostic biomarkers for colorectal cancer [J]. Journal of Southern Medical University, 2023, 43(3): 443-453. |
| [15] | YANG Pan, WANG Yuanyuan, GAO Qunwei, LIU Yang, WANG Yi, GUO Yu, LIU Changqing, LIU Gaofeng. Chemical reprogramming of human embryonic fibroblasts into neural progenitor cells in vitro [J]. Journal of Southern Medical University, 2023, 43(3): 360-367. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||