南方医科大学学报 ›› 2025, Vol. 45 ›› Issue (12): 2767-2776.doi: 10.12122/j.issn.1673-4254.2025.12.24
• • 上一篇
高世毅1( ), 韩子晨2,4(
), 韩子晨2,4( ), 曾强1, 程增为3, 王钧1, 康品方1, 王洪巨1, 李妙男1(
), 曾强1, 程增为3, 王钧1, 康品方1, 王洪巨1, 李妙男1( ), 胡司淦1(
), 胡司淦1( )
)
收稿日期:2025-06-22
出版日期:2025-12-20
发布日期:2025-12-22
通讯作者:
李妙男,胡司淦
E-mail:1933799781@qq.com;291979024@qq.com;13855265385@163.com;siganhu@126.com
作者简介:高世毅,在读硕士研究生,E-mail: 1933799781@qq.com基金资助:
Shiyi GAO1( ), Zichen HAN2,4(
), Zichen HAN2,4( ), Qiang ZENG1, Zengwei CHENG3, Jun WANG1, Pinfang KANG1, Hongju WANG1, Miaonan LI1(
), Qiang ZENG1, Zengwei CHENG3, Jun WANG1, Pinfang KANG1, Hongju WANG1, Miaonan LI1( ), Sigan HU1(
), Sigan HU1( )
)
Received:2025-06-22
Online:2025-12-20
Published:2025-12-22
Contact:
Miaonan LI, Sigan HU
E-mail:1933799781@qq.com;291979024@qq.com;13855265385@163.com;siganhu@126.com
摘要:
目的 通过联合评估冠状动脉大血管和微循环,全面预测ST段抬高型心肌梗死(STEMI)患者接受经皮冠状动脉介入治疗(PCI)治疗后发生不良心脑血管事件(MACCEs) 的风险。 方法 回顾性纳入来自两个医学中心的507例成功接受PCI的STEMI患者。基于受试者工作特征(ROC)曲线分析,确定基于血管的微血管阻力(AMR)预测MACCEs的最佳截断值为256.5 mmHg·s/m,结合既往文献确立的定量流量比(QFR)临界值0.80,采用2×2析因设计将患者分为4个亚组。第1组为心外膜血管功能正常且微循环功能良好组(QFR≥0.8且AMR<256.5,n=271,占53.5%);第2组为心外膜血管功能正常但微循环功能异常组(QFR≥0.8且AMR≥256.5,n=140,占27.6%);第3组为心外膜血管功能异常但微循环功能相对良好组(QFR<0.8且AMR<256.5,n=77,占15.2%);第4组为心外膜血管与微循环功能均异常组(QFR<0.8且AMR≥256.5,n=19,占3.7%)。主要临床结局为2年随访期间的心源性死亡或因心力衰竭再次入院的发生情况。 结果 在507例患者中,AMR≥256.5 mmHg·s/m的患者在PCI术后2年内发生MACCEs 的风险显著增加(P<0.001)。Kaplan-Meier生存分析表明,QFR<0.8且AMR≥256.5 mmHg·s/m的患者具有更差的生存率。多元线性回归分析显示,糖尿病(P<0.001)、高脂血症(P<0.001)、吸烟 (P<0.014)、系统性炎症反应指数(P<0.007)以及血小板与淋巴细胞比值(P<0.001)均与AMR水平升高独立相关。此外,限制性立方样条回归分析揭示了AMR与MACCEs发生风险之间的非线性关系(non-linear P<0.001),当AMR阈值达到259.45 mmHg·s/m时,MACCEs的发生风险显著增加。 结论 基于QFR与AMR的联合评估框架可有效预测STEMI患者急诊PCI术后发生MACCEs的风险。此外,AMR是PCI术后MACCEs的独立预测指标,其数值升高与MACCEs风险显著相关。
高世毅, 韩子晨, 曾强, 程增为, 王钧, 康品方, 王洪巨, 李妙男, 胡司淦. 冠状动脉微血管功能障碍的评估及其对ST段抬高型急性心肌梗死再灌注治疗的预测价值:基于QFR-AMR研究[J]. 南方医科大学学报, 2025, 45(12): 2767-2776.
Shiyi GAO, Zichen HAN, Qiang ZENG, Zengwei CHENG, Jun WANG, Pinfang KANG, Hongju WANG, Miaonan LI, Sigan HU. Evaluation of coronary microvascular dysfunction for assessing prognosis of ST-segment elevation acute myocardial infarction following reperfusion therapy: insights from QFR-AMR[J]. Journal of Southern Medical University, 2025, 45(12): 2767-2776.
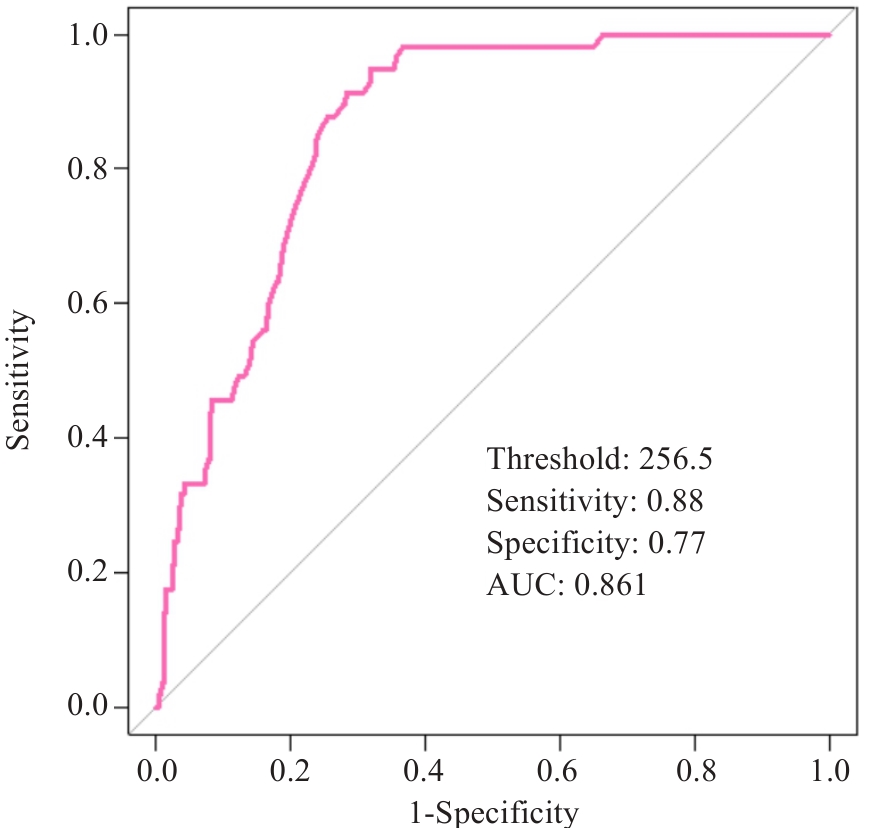
图1 STEMI患者PCI术后AMR的ROC曲线分析
Fig.1 ROC curve analysis of angio-based microvascular resistance (AMR) in patients with ST-segment elevation myocardial infarction (STEMI) after percutaneous coronary intervention (PCI). The curve illustrates the diagnostic efficacy of AMR for identifying major adverse cardiovascular and cerebrovascular events at the optimal cutoff value of 256.5 mmHg·s·m (sensitivity: 88%; specificity: 77%; AUC: 0.861).
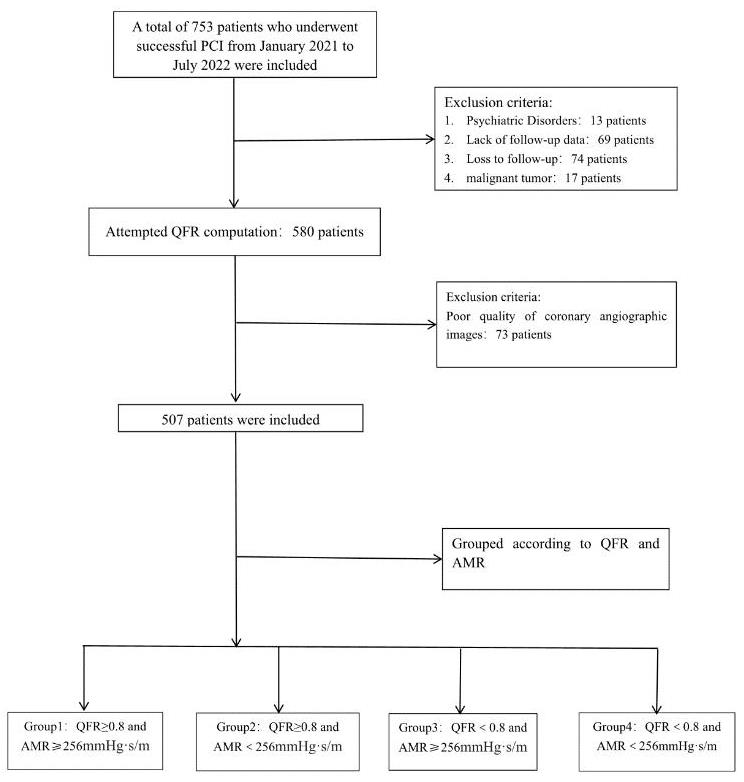
图2 患者筛选分组流程图
Fig.2 Patient screening flowchart. A total of 753 patients who underwent PCI were screened during the period from January 1, 2021, to July 1, 2022, and 507 patients included for further analysis. According to the QFR and AMR, the patients were categorized into 4 groups.
| Characteristics | QFR≥0.8 | P | QFR<0.8 | P | ||
|---|---|---|---|---|---|---|
| AMR≥256.5 mmHg·s/m (n=140, group 1) | AMR<256.5 mmHg·s/m (n=271, group 2) | AMR≥256.5 mmHg·s/m (n=19, group 3) | AMR<256.5 mmHg·s/m (n=77, group 4) | |||
| Study population | ||||||
| Age (year) | 69 (60, 77) | 60 (53, 72) | <0.001 | 69 (56, 76.00) | 67.00 (57, 78) | 0.873 |
| Male [n (%)] | 118 (84.3) | 201 (74.2) | 0.024 | 18 (94.7) | 53 (68.8) | 0.021 |
| Cardiovascular risk factors | ||||||
| Hypertension [n (%)] | 93 (66.4) | 160 (59.1) | 0.165 | 17 (89.5) | 54 (70.1) | 0.142 |
| Diabetes [n (%)] | 77 (55.0) | 95 (35.1) | <0.001 | 10 (52.6) | 24 (31.1) | 0.036 |
| Hyperlipemia [n (%)] | 98 (70.0) | 140 (51.7) | <0.001 | 18 (94.7) | 40 (51.9) | <0.001 |
| Stroke [n (%)] | 29 (20.7) | 45 (16.6) | 0.343 | 2 (10.5) | 12 (15.6) | 0.729 |
| Smoking [n (%)] | 103 (73.6) | 160 (59.0) | 0.005 | 12 (63.1) | 47 (61.0) | 0.875 |
| Previous CHD [n (%)] | 16 (11.4) | 46 (16.9) | 0.148 | 2 (10.5) | 11 (14.3) | 0.397 |
| Previous PCI [n (%)] | 10 (7.1) | 16 (5.9) | 0.671 | 0 (0) | 2 (2.6) | 0.682 |
| Pain-to-balloon time (min) | 246 (140.8, 362.5) | 219 (129.5, 387.0) | 0.110 | 489 (247.0, 690.0) | 454.0 (254.0, 900.0) | 0.457 |
| Laboratory index | ||||||
| cTnI (ng/L) | 1.1 (0.1, 8.7) | 0.6 (0.1, 7.6) | 0.443 | 12.6 (1.3, 36.6) | 9.4 (1.2, 27.9) | 0.608 |
| NT‐proBNP (pg/mL) | 241.0 (97.2, 1019.2) | 220.1 (70.7, 731.5) | 0.724 | 852.0 (407.1, 1600.0) | 356.0 (158.0, 1877.0) | 0.300 |
| Creatinine (μmol/L) | 69.0 (56.0, 82.0) | 66.0 (55.0, 79.0) | 0.232 | 69.0 (59.5, 85.0) | 69.0 (58.0, 86.0) | 0.835 |
| CK/CKMB | 7.4 (5.5, 9.6) | 7.3 (5.6, 9.5) | 0.755 | 6.1 (5.0, 8.2) | 8.2 (5.2, 9.9) | 0.124 |
| TC-C (mmol/L) | 4.7 (3.8, 5.4) | 4.7 (3.8, 5.6) | 0.472 | 4.3 (3.6, 4.7) | 4.4 (3.7, 5.2) | 0.561 |
| TG (mmol/L) | 1.6 (1.0, 2.3) | 1.5 (1.0, 2.2) | 0.339 | 1.2 (0.8, 1.8) | 1.2 (0.7, 1.9) | 0.846 |
| HDL-C (mmol/L) | 1.0 (0.9, 1.2) | 1.0 (0.8, 1.2) | 0.472 | 1.0 (0.9, 1.2) | 1.0 (0.8, 1.2) | 0.896 |
| LDL-C (mmol/L) | 2.6 (2.2, 3.3) | 2.7 (2.1, 3.4) | 0.508 | 2.6 (2.3, 3.0) | 2.6 (2.2, 3.1) | 0.935 |
| Inflammatory index | ||||||
| Neutrophil (109/L) | 6.2 (4.8, 7.2) | 6.0 (4.6, 7.4) | 0.728 | 6.3 (5.8, 8.3) | 7.1 (5.4, 9.2) | 0.306 |
| Monocyte (109/L) | 0.5 (0.3, 0.6) | 0.4 (0.3, 0.6) | 0.263 | 0.5 (0.4, 0.8) | 0.5 (0.4, 0.7) | 0.919 |
| Platelet (109/L) | 223.0 (187.2, 255.2) | 201.0 (164.0, 235.0) | 0.005 | 252.0 (240.5, 265.5) | 204.0 (155.0, 227.0) | 0.001 |
| Lymphocyte (109/L) | 1.6 (1.2, 2.0) | 1.9 (1.5, 2.4) | <0.001 | 1.4 (1.2, 2.3) | 2.4 (1.9, 2.6) | 0.051 |
| SII | 781.9 (651.9, 942.6) | 632.2 (466.0, 769.8) | <0.001 | 968.0 (773.6, 1466.5) | 591.3 (422.6, 812.3) | 0.002 |
| SIRI | 1.7 (1.1, 2.8) | 1.49 (0.9, 2.1) | 0.061 | 1.87 (1.1, 3.8) | 1.57 (1.0, 2.8) | 0.609 |
| PLR | 3.6 (2.9, 4.0) | 3.2 (2.3, 4.0) | 0.005 | 3.9 (2.9, 5.6) | 3.0 (2.2, 4.0) | 0.124 |
| NLR | 130.3 (105.4, 165.1) | 100.8 (74.9, 125.8) | <0.001 | 152.3 (99.1, 224.3) | 83.0 (64.4, 100.7) | <0.001 |
| Discharge medications | ||||||
| Aspirin [n (%)] | 134 (95.7) | 265 (97.7) | 0.306 | 14 (73.6) | 63 (96.9) | 0.468 |
| Ticagrelor [n (%)] | 80 (57.1) | 174 (64.2) | 0.381 | 11 (57.8) | 55 (84.6) | 0.286 |
| Clopidogrel [n (%)] | 52 (37.1) | 95 (35.0) | 0.511 | 3 (15.7) | 10 (15.3) | 0.702 |
| Statins [n (%)] | 133 (95.0) | 266 (98.1) | 1.000 | 14 (73.6) | 62 (95.3) | 0.572 |
| ACEI/ARB [n (%)] | 65 (46.4) | 139 (51.2) | 0.597 | 4 (21.0) | 20 (30.7) | 0.511 |
| Beta‐blocker [n (%)] | 107 (76.4) | 219 (80.8) | 0.788 | 10 (52.6) | 44 (67.6) | 0.488 |
| ARNi [n (%)] | 24 (17.1) | 57 (21.0) | 0.135 | 5 (26.3) | 24 (36.9) | 0.304 |
| SGLT2i [n (%)] | 1 (0.7) | 13 (4.8) | 0.041 | 1 (5.2) | 10 (15.3) | 0.392 |
| Spirolactone [n (%)] | 64 (45.7) | 102 (37.6) | 0.068 | 6 (31.5) | 22 (33.8) | 0.180 |
| Furosemide [n (%)] | 57 (40.7) | 92 (33.9) | 0.125 | 6 (31.5) | 19 (29.2) | 0.259 |
表1 基线资料
Tab.1 Baseline characteristics of the patients included
| Characteristics | QFR≥0.8 | P | QFR<0.8 | P | ||
|---|---|---|---|---|---|---|
| AMR≥256.5 mmHg·s/m (n=140, group 1) | AMR<256.5 mmHg·s/m (n=271, group 2) | AMR≥256.5 mmHg·s/m (n=19, group 3) | AMR<256.5 mmHg·s/m (n=77, group 4) | |||
| Study population | ||||||
| Age (year) | 69 (60, 77) | 60 (53, 72) | <0.001 | 69 (56, 76.00) | 67.00 (57, 78) | 0.873 |
| Male [n (%)] | 118 (84.3) | 201 (74.2) | 0.024 | 18 (94.7) | 53 (68.8) | 0.021 |
| Cardiovascular risk factors | ||||||
| Hypertension [n (%)] | 93 (66.4) | 160 (59.1) | 0.165 | 17 (89.5) | 54 (70.1) | 0.142 |
| Diabetes [n (%)] | 77 (55.0) | 95 (35.1) | <0.001 | 10 (52.6) | 24 (31.1) | 0.036 |
| Hyperlipemia [n (%)] | 98 (70.0) | 140 (51.7) | <0.001 | 18 (94.7) | 40 (51.9) | <0.001 |
| Stroke [n (%)] | 29 (20.7) | 45 (16.6) | 0.343 | 2 (10.5) | 12 (15.6) | 0.729 |
| Smoking [n (%)] | 103 (73.6) | 160 (59.0) | 0.005 | 12 (63.1) | 47 (61.0) | 0.875 |
| Previous CHD [n (%)] | 16 (11.4) | 46 (16.9) | 0.148 | 2 (10.5) | 11 (14.3) | 0.397 |
| Previous PCI [n (%)] | 10 (7.1) | 16 (5.9) | 0.671 | 0 (0) | 2 (2.6) | 0.682 |
| Pain-to-balloon time (min) | 246 (140.8, 362.5) | 219 (129.5, 387.0) | 0.110 | 489 (247.0, 690.0) | 454.0 (254.0, 900.0) | 0.457 |
| Laboratory index | ||||||
| cTnI (ng/L) | 1.1 (0.1, 8.7) | 0.6 (0.1, 7.6) | 0.443 | 12.6 (1.3, 36.6) | 9.4 (1.2, 27.9) | 0.608 |
| NT‐proBNP (pg/mL) | 241.0 (97.2, 1019.2) | 220.1 (70.7, 731.5) | 0.724 | 852.0 (407.1, 1600.0) | 356.0 (158.0, 1877.0) | 0.300 |
| Creatinine (μmol/L) | 69.0 (56.0, 82.0) | 66.0 (55.0, 79.0) | 0.232 | 69.0 (59.5, 85.0) | 69.0 (58.0, 86.0) | 0.835 |
| CK/CKMB | 7.4 (5.5, 9.6) | 7.3 (5.6, 9.5) | 0.755 | 6.1 (5.0, 8.2) | 8.2 (5.2, 9.9) | 0.124 |
| TC-C (mmol/L) | 4.7 (3.8, 5.4) | 4.7 (3.8, 5.6) | 0.472 | 4.3 (3.6, 4.7) | 4.4 (3.7, 5.2) | 0.561 |
| TG (mmol/L) | 1.6 (1.0, 2.3) | 1.5 (1.0, 2.2) | 0.339 | 1.2 (0.8, 1.8) | 1.2 (0.7, 1.9) | 0.846 |
| HDL-C (mmol/L) | 1.0 (0.9, 1.2) | 1.0 (0.8, 1.2) | 0.472 | 1.0 (0.9, 1.2) | 1.0 (0.8, 1.2) | 0.896 |
| LDL-C (mmol/L) | 2.6 (2.2, 3.3) | 2.7 (2.1, 3.4) | 0.508 | 2.6 (2.3, 3.0) | 2.6 (2.2, 3.1) | 0.935 |
| Inflammatory index | ||||||
| Neutrophil (109/L) | 6.2 (4.8, 7.2) | 6.0 (4.6, 7.4) | 0.728 | 6.3 (5.8, 8.3) | 7.1 (5.4, 9.2) | 0.306 |
| Monocyte (109/L) | 0.5 (0.3, 0.6) | 0.4 (0.3, 0.6) | 0.263 | 0.5 (0.4, 0.8) | 0.5 (0.4, 0.7) | 0.919 |
| Platelet (109/L) | 223.0 (187.2, 255.2) | 201.0 (164.0, 235.0) | 0.005 | 252.0 (240.5, 265.5) | 204.0 (155.0, 227.0) | 0.001 |
| Lymphocyte (109/L) | 1.6 (1.2, 2.0) | 1.9 (1.5, 2.4) | <0.001 | 1.4 (1.2, 2.3) | 2.4 (1.9, 2.6) | 0.051 |
| SII | 781.9 (651.9, 942.6) | 632.2 (466.0, 769.8) | <0.001 | 968.0 (773.6, 1466.5) | 591.3 (422.6, 812.3) | 0.002 |
| SIRI | 1.7 (1.1, 2.8) | 1.49 (0.9, 2.1) | 0.061 | 1.87 (1.1, 3.8) | 1.57 (1.0, 2.8) | 0.609 |
| PLR | 3.6 (2.9, 4.0) | 3.2 (2.3, 4.0) | 0.005 | 3.9 (2.9, 5.6) | 3.0 (2.2, 4.0) | 0.124 |
| NLR | 130.3 (105.4, 165.1) | 100.8 (74.9, 125.8) | <0.001 | 152.3 (99.1, 224.3) | 83.0 (64.4, 100.7) | <0.001 |
| Discharge medications | ||||||
| Aspirin [n (%)] | 134 (95.7) | 265 (97.7) | 0.306 | 14 (73.6) | 63 (96.9) | 0.468 |
| Ticagrelor [n (%)] | 80 (57.1) | 174 (64.2) | 0.381 | 11 (57.8) | 55 (84.6) | 0.286 |
| Clopidogrel [n (%)] | 52 (37.1) | 95 (35.0) | 0.511 | 3 (15.7) | 10 (15.3) | 0.702 |
| Statins [n (%)] | 133 (95.0) | 266 (98.1) | 1.000 | 14 (73.6) | 62 (95.3) | 0.572 |
| ACEI/ARB [n (%)] | 65 (46.4) | 139 (51.2) | 0.597 | 4 (21.0) | 20 (30.7) | 0.511 |
| Beta‐blocker [n (%)] | 107 (76.4) | 219 (80.8) | 0.788 | 10 (52.6) | 44 (67.6) | 0.488 |
| ARNi [n (%)] | 24 (17.1) | 57 (21.0) | 0.135 | 5 (26.3) | 24 (36.9) | 0.304 |
| SGLT2i [n (%)] | 1 (0.7) | 13 (4.8) | 0.041 | 1 (5.2) | 10 (15.3) | 0.392 |
| Spirolactone [n (%)] | 64 (45.7) | 102 (37.6) | 0.068 | 6 (31.5) | 22 (33.8) | 0.180 |
| Furosemide [n (%)] | 57 (40.7) | 92 (33.9) | 0.125 | 6 (31.5) | 19 (29.2) | 0.259 |
| Characteristics | QFR≥0.8 | P | QFR<0.8 | P | ||
|---|---|---|---|---|---|---|
| AMR≥256.5 mmHg·s/m (n=140, Group 1) | AMR<256.5 mmHg·s/m (n=271, Group 2) | AMR≥256.5 mmHg·s/m (n=19, Group 3) | AMR<256.5 mmHg·s/m (n=77, Group 4) | |||
| Infarct‐related artery | ||||||
| LAD [n (%)] | 65 (46.4) | 105 (38.7) | 0.408 | 13 (68.4) | 45 (58.4) | 0.744 |
| AMR | 269 (263, 302) | 220 (195, 235) | <0.001 | 297 [269, 329] | 199 (161, 225) | <0.001 |
| LCX [n (%)] | 81 (57.8) | 172 (63.4) | 0.473 | 3 (15.7) | 9 (11.6) | 0.833 |
| AMR | 296 (274, 310) | 227 (211, 242) | <0.001 | 257 [256, 260] | 195 (186, 233) | 0.182 |
| RCA [n (%)] | 59.0 (42.1) | 118.0 (43.5) | 0.987 | 3 (15.7) | 23 (29.8) | 0.679 |
| AMR | 272 (261, 303) | 221.5 (198, 239) | <0.001 | 306 [299, 327] | 194 (180, 215) | 0.220 |
| Multivessel disease | ||||||
| 1 [n (%)] | 65 (46.4) | 65 (23.9) | 0.013 | 7 (36.8) | 14 (18.1) | 0.689 |
| 2 [n (%)] | 24 (17.1) | 114 (42.0) | 0.040 | 7 (36.8) | 38 (49.3) | 0.844 |
| 3 [n (%)] | 51 (36.4) | 92 (33.9) | 0.908 | 5 (26.3) | 25 (32.4) | 0.689 |
| TIMI flow grade (inital) | ||||||
| 0 | 124 (88.5) | 229 (84.5) | 0.374 | 15 (78.9) | 46 (59.7) | 0.338 |
| 1 | 12 (8.5) | 32 (11.8) | 0.898 | 2 (10.5) | 24 (31.1) | 0.784 |
| 2 | 2 (1.4) | 4 (1.4) | 0.933 | 0 (0) | 7 (7.7) | 1.000 |
| 3 | 2 (1.4) | 6 (2.2) | 0.947 | 2 (10.5) | 1 (1.3) | 0.863 |
| TIMI flow grade (post) | 0.776 | 0.645 | ||||
| 0 | 0 | 0 | 0 | 0 | ||
| 1 | 0 | 0 | 0 | 0 | ||
| 2 | 0 | 0 | 0 | 0 | ||
| 3 | 140 (100) | 271 (100) | 19 (100) | 77 (100) | ||
| QFR | 0.94 (0.91, 0.97) | 0.94 (0.89, 0.97) | 0.382 | 0.74 (0.70, 0.77) | 0.74 (0.70, 0.77) | 0.885 |
| AMR (mmHg·s/m) | 274.00 (262.75, 308.00) | 221.00 (197.50, 238.00) | <0.001 | 293.00 (268.00, 327.00) | 195.00 (169.00, 225.00) | <0.001 |
| MACCEs [n (%)] | 26 (18.57) | 4 (1.48) | <0.001 | 14 (73.68) | 16 (20.78) | <0.001 |
| Non-culprit vessel | ||||||
| QFR | 0.90 (0.85, 0.96) | 0.85 (0.83,0.94) | 0.452 | 0.83 (0.81,0.91) | 0.88 (0.82, 0.94) | 0.521 |
| AMR (mmHg·s/m) | 232.00 (204.00, 241.00) | 227.00 (200.00, 239.00) | 0.326 | 239.00 (217.50, 249.00) | 225.00 (214.00, 234.00) | 0.428 |
表2 冠状动脉血管相关特征
Tab. 2 Characteristics related to coronary artery vessels in different groups of patients
| Characteristics | QFR≥0.8 | P | QFR<0.8 | P | ||
|---|---|---|---|---|---|---|
| AMR≥256.5 mmHg·s/m (n=140, Group 1) | AMR<256.5 mmHg·s/m (n=271, Group 2) | AMR≥256.5 mmHg·s/m (n=19, Group 3) | AMR<256.5 mmHg·s/m (n=77, Group 4) | |||
| Infarct‐related artery | ||||||
| LAD [n (%)] | 65 (46.4) | 105 (38.7) | 0.408 | 13 (68.4) | 45 (58.4) | 0.744 |
| AMR | 269 (263, 302) | 220 (195, 235) | <0.001 | 297 [269, 329] | 199 (161, 225) | <0.001 |
| LCX [n (%)] | 81 (57.8) | 172 (63.4) | 0.473 | 3 (15.7) | 9 (11.6) | 0.833 |
| AMR | 296 (274, 310) | 227 (211, 242) | <0.001 | 257 [256, 260] | 195 (186, 233) | 0.182 |
| RCA [n (%)] | 59.0 (42.1) | 118.0 (43.5) | 0.987 | 3 (15.7) | 23 (29.8) | 0.679 |
| AMR | 272 (261, 303) | 221.5 (198, 239) | <0.001 | 306 [299, 327] | 194 (180, 215) | 0.220 |
| Multivessel disease | ||||||
| 1 [n (%)] | 65 (46.4) | 65 (23.9) | 0.013 | 7 (36.8) | 14 (18.1) | 0.689 |
| 2 [n (%)] | 24 (17.1) | 114 (42.0) | 0.040 | 7 (36.8) | 38 (49.3) | 0.844 |
| 3 [n (%)] | 51 (36.4) | 92 (33.9) | 0.908 | 5 (26.3) | 25 (32.4) | 0.689 |
| TIMI flow grade (inital) | ||||||
| 0 | 124 (88.5) | 229 (84.5) | 0.374 | 15 (78.9) | 46 (59.7) | 0.338 |
| 1 | 12 (8.5) | 32 (11.8) | 0.898 | 2 (10.5) | 24 (31.1) | 0.784 |
| 2 | 2 (1.4) | 4 (1.4) | 0.933 | 0 (0) | 7 (7.7) | 1.000 |
| 3 | 2 (1.4) | 6 (2.2) | 0.947 | 2 (10.5) | 1 (1.3) | 0.863 |
| TIMI flow grade (post) | 0.776 | 0.645 | ||||
| 0 | 0 | 0 | 0 | 0 | ||
| 1 | 0 | 0 | 0 | 0 | ||
| 2 | 0 | 0 | 0 | 0 | ||
| 3 | 140 (100) | 271 (100) | 19 (100) | 77 (100) | ||
| QFR | 0.94 (0.91, 0.97) | 0.94 (0.89, 0.97) | 0.382 | 0.74 (0.70, 0.77) | 0.74 (0.70, 0.77) | 0.885 |
| AMR (mmHg·s/m) | 274.00 (262.75, 308.00) | 221.00 (197.50, 238.00) | <0.001 | 293.00 (268.00, 327.00) | 195.00 (169.00, 225.00) | <0.001 |
| MACCEs [n (%)] | 26 (18.57) | 4 (1.48) | <0.001 | 14 (73.68) | 16 (20.78) | <0.001 |
| Non-culprit vessel | ||||||
| QFR | 0.90 (0.85, 0.96) | 0.85 (0.83,0.94) | 0.452 | 0.83 (0.81,0.91) | 0.88 (0.82, 0.94) | 0.521 |
| AMR (mmHg·s/m) | 232.00 (204.00, 241.00) | 227.00 (200.00, 239.00) | 0.326 | 239.00 (217.50, 249.00) | 225.00 (214.00, 234.00) | 0.428 |
| Characteristics | Regression coefficient β | Standard error | t | P |
|---|---|---|---|---|
| Diabetes | 16.970 | 5.014 | 3.384 | <0.001 |
| Hyperlipemia | 15.071 | 4.531 | 3.326 | <0.001 |
| Smoking | 11.457 | 4.645 | 2.466 | 0.014 |
| SIRI | 5.677 | 2.081 | 2.728 | 0.007 |
| PLR | 0.261 | 0.064 | 4.072 | <0.001 |
表3 AMR的多元线性回归分析
Tab.3 Multivariate linear regression analysis of AMR of the patients
| Characteristics | Regression coefficient β | Standard error | t | P |
|---|---|---|---|---|
| Diabetes | 16.970 | 5.014 | 3.384 | <0.001 |
| Hyperlipemia | 15.071 | 4.531 | 3.326 | <0.001 |
| Smoking | 11.457 | 4.645 | 2.466 | 0.014 |
| SIRI | 5.677 | 2.081 | 2.728 | 0.007 |
| PLR | 0.261 | 0.064 | 4.072 | <0.001 |
| Characteristics | Total | Group1 | Group2 | Group3 | Group4 | P |
|---|---|---|---|---|---|---|
| Primary outcome | 60 (11.83%) | 26 (18.57%) | 4 (1.48%) | 14 (73.68%) | 16 (20.78%) | <0.001 |
| All-cause mortality | 24 (4.73%) | 9 (6.43%) | 2 (0.74%) | 6 (31.57%) | 7 (9.09%) | <0.001 |
| Cardiac failure | 36 (7.10%) | 17 (12.14%) | 2 (0.74%) | 8 (42.11%) | 9 (11.69%) | 0.005 |
| Any myocardial infarction | 7 (1.38%) | 3 (2.14%) | 0 (0.00%) | 2 (10.52%) | 2 (2.59%) | 0.438 |
| IRA myocardial infarction | 4 (0.79%) | 2 (1.43%) | 0 (0.00%) | 1 (5.26%) | 1 (1.29%) | 0.572 |
| Non-IRA myocardial infarction | 3 (0.59%) | 1 (0.71%) | 0 (0.00%) | 1 (5.26%) | 1 (1.29%) | 0.801 |
| Readmission for angina | 18 (3.55%) | 8 (5.71%) | 1 (0.37%) | 3 (15.78%) | 6 (7.79%) | 0.092 |
| Any revascularization | 10 (1.97%) | 4 (2.86%) | 0 (0.00%) | 2 (10.52%) | 4 (5.19%) | 0.221 |
| Stroke | 5 (0.98%) | 3 (2.14%) | 1 (0.37%) | 1 (5.26%) | 0 (0.00%) | 0.284 |
表4 不同组别的临床结果
Tab.4 Clinical outcomes across different groups of patients
| Characteristics | Total | Group1 | Group2 | Group3 | Group4 | P |
|---|---|---|---|---|---|---|
| Primary outcome | 60 (11.83%) | 26 (18.57%) | 4 (1.48%) | 14 (73.68%) | 16 (20.78%) | <0.001 |
| All-cause mortality | 24 (4.73%) | 9 (6.43%) | 2 (0.74%) | 6 (31.57%) | 7 (9.09%) | <0.001 |
| Cardiac failure | 36 (7.10%) | 17 (12.14%) | 2 (0.74%) | 8 (42.11%) | 9 (11.69%) | 0.005 |
| Any myocardial infarction | 7 (1.38%) | 3 (2.14%) | 0 (0.00%) | 2 (10.52%) | 2 (2.59%) | 0.438 |
| IRA myocardial infarction | 4 (0.79%) | 2 (1.43%) | 0 (0.00%) | 1 (5.26%) | 1 (1.29%) | 0.572 |
| Non-IRA myocardial infarction | 3 (0.59%) | 1 (0.71%) | 0 (0.00%) | 1 (5.26%) | 1 (1.29%) | 0.801 |
| Readmission for angina | 18 (3.55%) | 8 (5.71%) | 1 (0.37%) | 3 (15.78%) | 6 (7.79%) | 0.092 |
| Any revascularization | 10 (1.97%) | 4 (2.86%) | 0 (0.00%) | 2 (10.52%) | 4 (5.19%) | 0.221 |
| Stroke | 5 (0.98%) | 3 (2.14%) | 1 (0.37%) | 1 (5.26%) | 0 (0.00%) | 0.284 |
| Characteristics | HR (univariable) | P | HR (multivariable) | P |
|---|---|---|---|---|
| Age | 1.033 (1.010-1.056) | 0.045 | 1.043 (1.010-1.078) | 0.069 |
| Hypertension | 3.625 (1.486-6.085) | <0.001 | 3.412 (1.178-6.328) | 0.002 |
| Diabetes | 4.838 (2.645-8.849) | <0.001 | 2.948 (1.326-6.557) | 0.008 |
| Hyperlipemia | 5.408 (2.511-11.648) | 0.032 | 5.434 (2.121-13.923) | 0.079 |
| Smoking | 3.680 (1.767-7.664) | <0.001 | 3.021 (1.187-7.687) | 0.020 |
| Pain-to-balloon time | 1.458 (1.235-3.454) | 0.033 | 1.001 (0.701-1.012) | 0.041 |
| SIRI | 1.582 (1.335-1.874) | 0.065 | 1.665 (1.370-2.023) | 0.082 |
| AMR | 1.247 (1.185-3.583) | <0.001 | 1.145 (1.046-2.638) | <0.001 |
表5 MACCEs的独立预测因子
Tab.5 Independent predictors of MACCEs in patients with STEMI
| Characteristics | HR (univariable) | P | HR (multivariable) | P |
|---|---|---|---|---|
| Age | 1.033 (1.010-1.056) | 0.045 | 1.043 (1.010-1.078) | 0.069 |
| Hypertension | 3.625 (1.486-6.085) | <0.001 | 3.412 (1.178-6.328) | 0.002 |
| Diabetes | 4.838 (2.645-8.849) | <0.001 | 2.948 (1.326-6.557) | 0.008 |
| Hyperlipemia | 5.408 (2.511-11.648) | 0.032 | 5.434 (2.121-13.923) | 0.079 |
| Smoking | 3.680 (1.767-7.664) | <0.001 | 3.021 (1.187-7.687) | 0.020 |
| Pain-to-balloon time | 1.458 (1.235-3.454) | 0.033 | 1.001 (0.701-1.012) | 0.041 |
| SIRI | 1.582 (1.335-1.874) | 0.065 | 1.665 (1.370-2.023) | 0.082 |
| AMR | 1.247 (1.185-3.583) | <0.001 | 1.145 (1.046-2.638) | <0.001 |
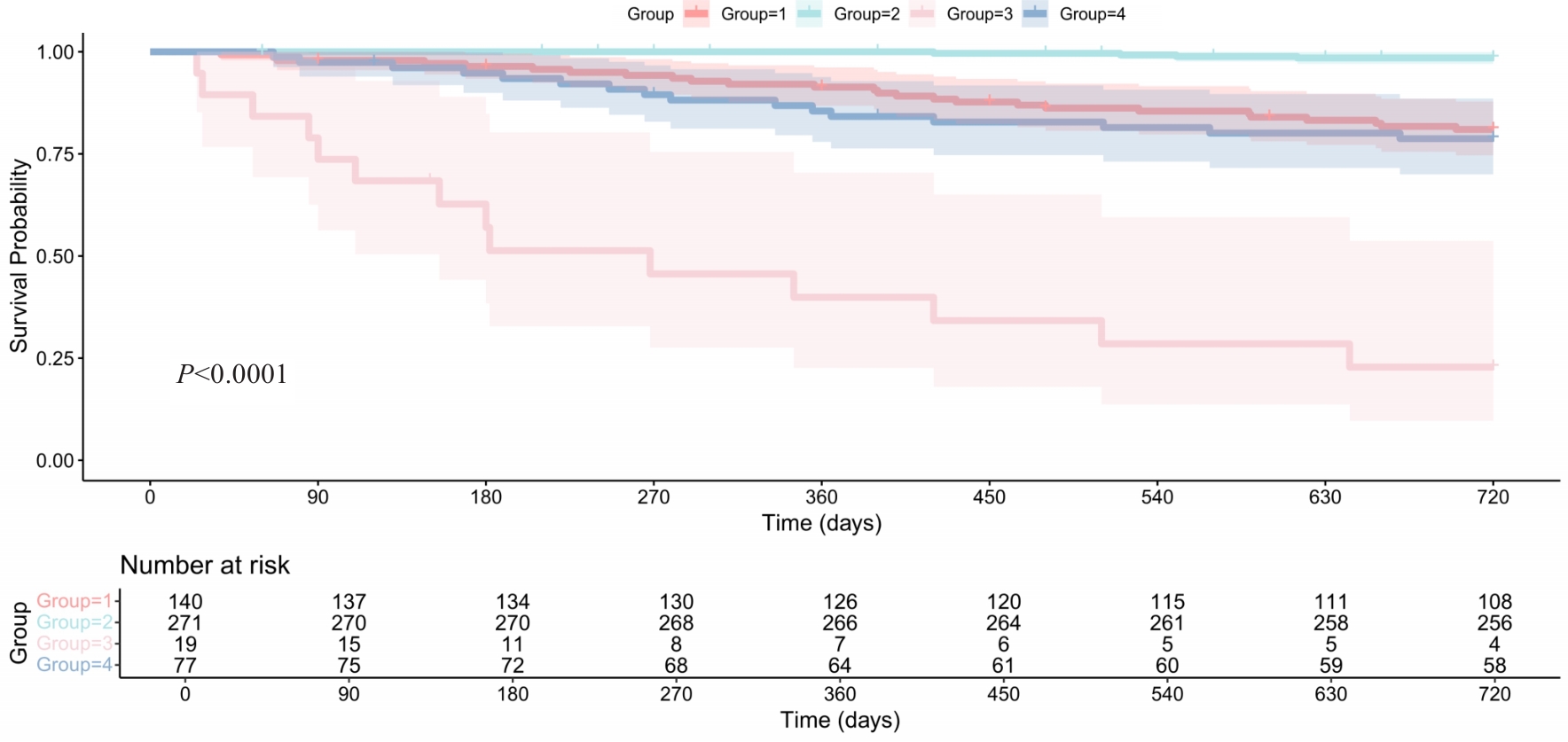
图4 根据QFR-AMR分层的Kaplan-Meier生存曲线
Fig.4 Kaplan-Meier survival curves of the primary outcome in patients with STEMI stratified by QFR-AMR. The survival outcomes vary significantly across the groups (P<0.0001).
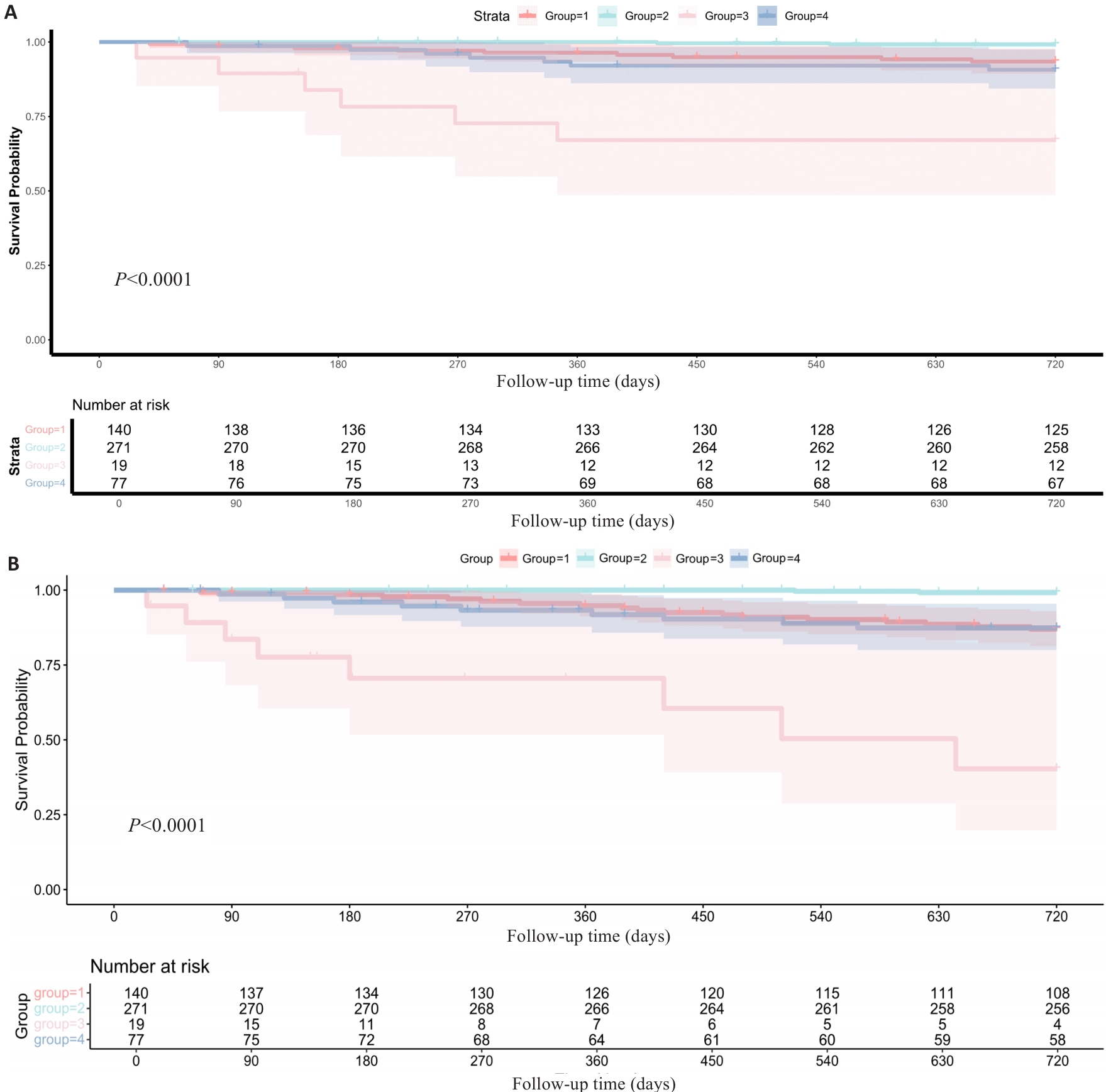
图6 根据AMR-QFR分组的全因死亡和心力衰竭结局的Kaplan-Meier生存曲线
Fig.6 Kaplan-Meier analyses reveal significant differences in all-cause mortality rates (A) and heart failure incidence (B) among the 4 groups stratified based on AMR-QFR.
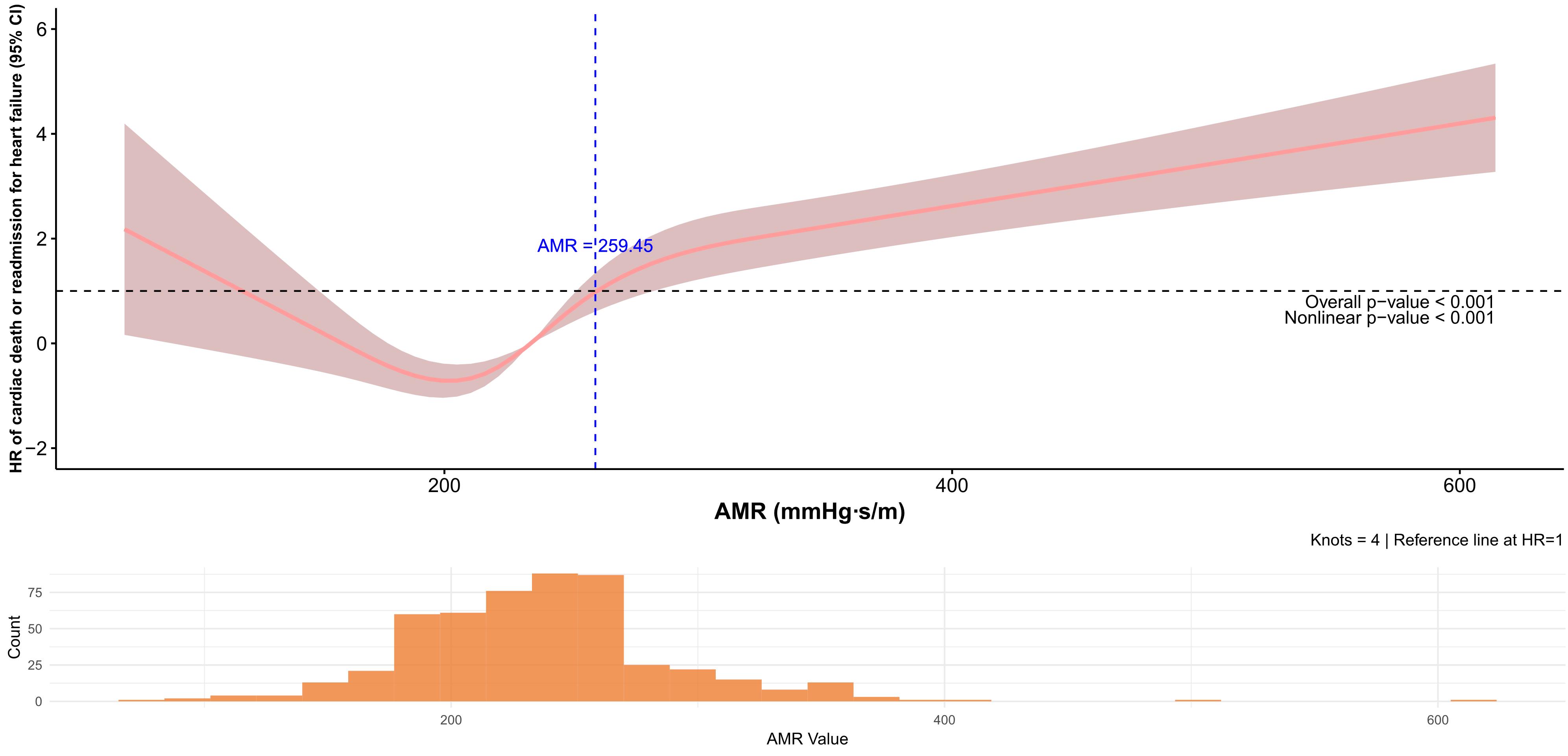
图7 限制三次样条分析
Fig.7 Relationships between MAR and the risk of cardiac death or readmission for heart failure according to the restricted cubic spline analysis.
| [1] | 胡司淦, 程增为, 李 敏, 等. 冠状动脉慢性完全闭塞病变侧支循环的建立与胰岛素抵抗的相关性[J]. 南方医科大学学报, 2024, 44(4): 780-6. |
| [2] | Li Y, Han YL. Interpretation of 2023 ESC Guidelines for the management of acute coronary syndromes[J]. Zhonghua Xin Xue Guan Bing Za Zhi, 2023, 51(12): 1263-7. |
| [3] | Milasinovic D, Nedeljkovic O, Maksimovic R, et al. Coronary microcirculation: the next frontier in the management of STEMI[J]. J Clin Med, 2023, 12(4): 1602. doi:10.3390/jcm12041602 |
| [4] | Rehan R, Virk S, Wong CCY, et al. Intracoronary thrombolysis in ST-elevation myocardial infarction: a systematic review and meta-analysis[J]. Heart, 2024, 110(15): 988-96. doi:10.1136/heartjnl-2024-324078 |
| [5] | Mignatti A, Echarte-Morales J, Sturla M, et al. State of the art of primary PCI: present and future[J]. J Clin Med, 2025, 14(2): 653. doi:10.3390/jcm14020653 |
| [6] | Kleinbongard P, Heusch G. A fresh look at coronary microembolization[J]. Nat Rev Cardiol, 2022, 19(4): 265-80. doi:10.1038/s41569-021-00632-2 |
| [7] | Sagris M, Theofilis P, Antonopoulos AS, et al. Inflammation in coronary microvascular dysfunction[J]. Int J Mol Sci, 2021, 22(24): 13471. doi:10.3390/ijms222413471 |
| [8] | Cui J, Liu W, Yan F, et al. Predictive value of cardiac magnetic resonance imaging for adverse left ventricular remodeling after acute ST-segment elevation myocardial infarction[J]. Nan Fang Yi Ke da Xue Xue Bao, 2024, 44(3): 553-62. |
| [9] | Travieso A, Jeronimo-Baza A, Faria D, et al. Invasive evaluation of coronary microvascular dysfunction[J]. J Nucl Cardiol, 2022, 29(5): 2474-86. doi:10.1007/s12350-022-02997-4 |
| [10] | Geng YY, Wu XT, Liu HP, et al. Index of microcirculatory resistance: state-of-the-art and potential applications in com-putational simulation of coronary artery disease[J]. J Zhejiang Univ SCIENCE B, 2022, 23(2): 123-40. doi:10.1631/jzus.b2100425 |
| [11] | Wang D, Li X, Feng W, et al. Diagnostic and prognostic value of angiography-derived index of microvascular resistance: a systematic review and meta-analysis[J]. Front Cardiovasc Med, 2024, 11: 1360648. doi:10.3389/fcvm.2024.1360648 |
| [12] | Zhan J, Zhong L, Wu J. Assessment and treatment for coronary microvascular dysfunction by contrast enhanced ultrasound[J]. Front Cardiovasc Med, 2022, 9: 899099. doi:10.3389/fcvm.2022.899099 |
| [13] | Biscaglia S, Verardi FM, Tebaldi M, et al. QFR-based virtual PCI or conventional angiography to guide PCI the AQVA trial[J]. JACC Cardiovasc Interv, 2023, 16(7): 783-94. doi:10.1016/j.jcin.2022.10.054 |
| [14] | Xu B, Tu SX, Qiao SB, et al. Diagnostic accuracy of angiography-based quantitative flow ratio measurements for online assessment of coronary stenosis[J]. J Am Coll Cardiol, 2017, 70(25): 3077-87. doi:10.1016/j.jacc.2017.10.035 |
| [15] | Rao SV, O’Donoghue ML, Ruel M, et al. Correction to: 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American college of cardiology/American heart association joint committee on clinical practice guidelines[J]. Circulation, 2025, 151(25): e1098. |
| [16] | Byrne R, Coughlan JJ, Rossello X, et al. The ‘10 commandments’ for the 2023 ESC Guidelines for the management of acute coronary syndromes[J]. Eur Heart J, 2024, 45(14): 1193-5. doi:10.1093/eurheartj/ehad863 |
| [17] | McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure[J]. Eur Heart J, 2021, 42(36): 3599-726. |
| [18] | Xia Y, Xia C, Wu L, et al. Systemic immune inflammation index (SII), system inflammation response index (SIRI) and risk of all-cause mortality and cardiovascular mortality: a 20-year follow-up cohort study of 42, 875 US adults[J]. J Clin Med, 2023, 12(3): 1128. doi:10.3390/jcm12031128 |
| [19] | Jo YS, Moon H, Park K. Different microcirculation response between culprit and non-culprit vessels in patients with acute coronary syndrome[J]. J Am Heart Assoc, 2020, 9(10): e015507. doi:10.1161/jaha.119.015507 |
| [20] | Sokratous S, Mitsis A, Khattab E, et al. Coronary microvascular disease early after myocardial infarction: diagnostic approach and prognostic value-a narrative review[J]. Biomedicines, 2025, 13(6): 1289. doi:10.3390/biomedicines13061289 |
| [21] | Heusch G. Coronary blood flow in heart failure: cause, consequence and bystander[J]. Basic Res Cardiol, 2022, 117(1): 1. doi:10.1007/s00395-022-00909-8 |
| [22] | Yang DR, Wang MY, Zhang CL, et al. Endothelial dysfunction in vascular complications of diabetes: a comprehensive review of mechanisms and implications[J]. Front Endocrinol: Lausanne, 2024, 15: 1359255. doi:10.3389/fendo.2024.1359255 |
| [23] | Islam K, Islam R, Nguyen I, et al. Diabetes mellitus and associated vascular disease: pathogenesis, complications, and evolving treatments[J]. Adv Ther, 2025, 42(6): 2659-78. doi:10.1007/s12325-025-03185-9 |
| [24] | Goligorsky MS. Vascular endothelium in diabetes[J]. Am J Physiol Renal Physiol, 2017, 312(2): F266-75. doi:10.1152/ajprenal.00473.2016 |
| [25] | Galos G, Rabai M, Szabo R, et al. The influence of triglyceride and low-density-lipoprotein target levels on microcirculation: Is there a difference[J]? Heliyon, 2024, 10(6): e27954. doi:10.1016/j.heliyon.2024.e27954 |
| [26] | Qin P, Ho FK, Celis-Morales CA, et al. Association between systemic inflammation biomarkers and incident cardiovascular disease in 423, 701 individuals: evidence from the UK biobank cohort[J]. Cardiovasc Diabetol, 2025, 24(1): 162. doi:10.1186/s12933-025-02721-9 |
| [27] | Xu SW, Ilyas I, Little PJ, et al. Endothelial dysfunction in atherosclerotic cardiovascular diseases and beyond: from mechanism to pharmacotherapies[J]. Pharmacol Rev, 2021, 73(3): 924-67. doi:10.1124/pharmrev.120.000096 |
| [28] | Qian G, Qin H, Deng D, et al. Prognostic value of angiographic microvascular resistance in patients with ST-segment elevation myocardial infarction[J]. Clinics: Sao Paulo, 2024, 79: 100429. doi:10.1016/j.clinsp.2024.100429 |
| [29] | Luo D, Wu H, Zhou W, et al. Angio-based coronary functional assessment predicts 30-day new-onset heart failure after acute myocardial infarction[J]. ESC Heart Fail, 2023, 10(5): 2914-26. doi:10.1002/ehf2.14452 |
| [30] | Ma J, Xia R, Lan Y, et al. Angiographic microvascular resistance in patients with obstructive hypertrophic cardiomyopathy[J]. Microvasc Res, 2024, 153: 104656. doi:10.1016/j.mvr.2024.104656 |
| [31] | Westra J, Andersen BK, Campo G, et al. Diagnostic performance of in-procedure angiography-derived quantitative flow reserve compared to pressure-derived fractional flow reserve: the FAVOR II Europe-Japan study[J]. J Am Heart Assoc, 2018, 7(14): e009603. doi:10.1161/jaha.118.009603 |
| [32] | Watarai M, Otsuka M, Yazaki K, et al. Applicability of quantitative flow ratio for rapid evaluation of intermediate coronary stenosis: comparison with instantaneous wave-free ratio in clinical practice[J]. Int J Cardiovasc Imag, 2019, 35(11): 1963-9. doi:10.1007/s10554-019-01656-z |
| [1] | 马振岩, 阿鑫, 赵蕾, 张洪博, 刘科, 赵依晴, 钱赓. 急性ST段抬高型心肌梗死经皮冠状动脉介入术后左心室不良重构的新型风险预测模型:基于心脏磁共振的多中心前瞻性研究[J]. 南方医科大学学报, 2025, 45(4): 669-683. |
| [2] | 刘科, 马振岩, 付磊, 张丽萍, 阿鑫, 肖少波, 张震, 张洪博, 赵蕾, 钱赓. 心脏磁共振成像整体纵向应变对急性ST段抬高型心肌梗死后左心室重构的预测价值:403例前瞻性研究[J]. 南方医科大学学报, 2024, 44(6): 1033-1039. |
| [3] | 崔佳宁, 刘文佳, 闫 非, 赵亚男, 陈伟杰, 罗春材, 张兴华, 李 涛. 心脏磁共振成像对急性ST段抬高型心肌梗死后左心室不良重构的预测价值[J]. 南方医科大学学报, 2024, 44(3): 553-562. |
| [4] | 卢丽萍, 钟嘉鑫, 吴锡林, 陈 琴, 林慧中, 陈良龙, 罗育坤. 心肌梗死后室壁瘤患者的静息心率与主要不良心脑血管事件相关:基于227例回顾性队列研究[J]. 南方医科大学学报, 2023, 43(3): 400-404. |
| [5] | 申磊磊,汪成,王嵘,肖苍松,吴扬,王瑶,龚志云,郭鹏飞,赵海智,高长青. 左心室室壁瘤患者行左室成形术与单纯冠脉旁路移植术的中远期疗效对比[J]. 南方医科大学学报, 2016, 36(05): 681-. |
| [6] | 何钕琴,沈淑馨,汪艳,郭胜存,王俊芬,宾建平. 急性ST段抬高型心肌梗死患者血清白介素-37表达的时间变化及与C反应蛋白的关系[J]. 南方医科大学学报, 2015, 35(12): 1751-. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||