南方医科大学学报 ›› 2025, Vol. 45 ›› Issue (8): 1581-1588.doi: 10.12122/j.issn.1673-4254.2025.08.02
• • 上一篇
杜志欣1,2( ), 王悦阳1, 杨丽萍1,2(
), 王悦阳1, 杨丽萍1,2( ), 侯俊林1(
), 侯俊林1( ), 孙建华2, 范朋北3, 王耀辉1, 李笑琳1
), 孙建华2, 范朋北3, 王耀辉1, 李笑琳1
收稿日期:2025-02-11
出版日期:2025-08-20
发布日期:2025-09-05
通讯作者:
杨丽萍,侯俊林
E-mail:dzx19961212@163.com;bioylp@126.com;houjunlin2005@163.com
作者简介:杜志欣,在读博士研究生,E-mail: dzx19961212@163.com
基金资助:
Zhixin DU1,2( ), Yueyang WANG1, Liping YANG1,2(
), Yueyang WANG1, Liping YANG1,2( ), Junlin HOU1(
), Junlin HOU1( ), Jianhua SUN2, Pengbei FAN3, Yaohui WANG1, Xiaolin LI1
), Jianhua SUN2, Pengbei FAN3, Yaohui WANG1, Xiaolin LI1
Received:2025-02-11
Online:2025-08-20
Published:2025-09-05
Contact:
Liping YANG, Junlin HOU
E-mail:dzx19961212@163.com;bioylp@126.com;houjunlin2005@163.com
Supported by:摘要:
目的 探讨孕期恐应激对胎盘氨基酸转运及子代情绪和认知的影响。 方法 将30只Wistar孕鼠随机分为正常组和恐应激组,15只/组。恐应激组通过旁观电击法造模。于孕20 d,每组随机选取6只孕鼠采血并收集胎盘样本,剩余孕鼠自然分娩,子鼠延续母鼠分组并喂养至8周龄。通过行为学实验评估孕鼠及子鼠的情绪变化及认知能力;HE染色观察孕鼠胎盘结构变化;生物信息学筛选恐应激胎盘差异表达的转运体基因并进行功能富集分析;Western blotting与qRT-PCR检测胎盘A系氨基酸转运体,L系氨基酸转运体以及具有特殊转运功能的转运体的蛋白及基因表达;高效液相色谱法检测胎鼠血清氨基酸含量;相关性分析探讨胎鼠血清氨基酸含量与成年后子代行为学之间的关系。 结果 在旷场实验中,与正常组相比,恐应激组孕鼠穿格次数、中央区时间均降低(P<0.01);在场景恐惧实验中,恐应激组孕鼠的冻结时间与冻结时间百分比均提高(P<0.01);恐应激组胎盘质量,胎鼠质量及胎儿胎盘比重均降低(P<0.01);恐应激组胎盘中共发现28个差异表达的转运体,且主要富集在氨基酸转运等条目上;恐应激组胎鼠血清中的氨基酸的含量降低(P<0.05);恐应激组孕鼠胎盘中的A系氨基酸转运体Slc38a1的蛋白及基因表达均下降(P<0.05);L系氨基转运体Slc43a1与Slc43a2的基因及蛋白表达均下降(P<0.05),Slc7a8的蛋白表达下降(P<0.05);其他氨基酸转运体slc6a6、slc1a1与slc6a9的mRNA与蛋白表达均下降(P<0.05);Y迷宫实验与新物体识别实验结果显示,恐应激组子鼠新物体偏好指数降低(P<0.01),自发交替率降低(P<0.01);高架十字迷宫实验与悬尾实验结果显示,恐应激组子鼠进入开臂次数百分比、进入开臂时间百分比均降低(P<0.001),悬尾不动时间增加(P<0.01);相关性分析显示,早期血清氨基酸含量的下降与成年后认知能力降低相关。 结论 孕期恐应激可降低胎盘氨基酸转运体(如Slc38a1、Slc43a1、Slc43a2、Slc6a6、Slc1a1、Slc6a9)的基因与蛋白表达,导致胎鼠血清中的氨基酸水平下降,从而可能影响成年后子代的认知能力。
杜志欣, 王悦阳, 杨丽萍, 侯俊林, 孙建华, 范朋北, 王耀辉, 李笑琳. 孕期恐应激通过降低大鼠胎盘氨基酸转运体表达损害子代认知发育[J]. 南方医科大学学报, 2025, 45(8): 1581-1588.
Zhixin DU, Yueyang WANG, Liping YANG, Junlin HOU, Jianhua SUN, Pengbei FAN, Yaohui WANG, Xiaolin LI. Prenatal fear stress impairs cognitive development in offspring rats by disrupting placental amino acid transport[J]. Journal of Southern Medical University, 2025, 45(8): 1581-1588.
| Name of primers | Primer sequence 5'-3' |
|---|---|
| GAPDH-F | CTGGAGAAACCTGCCAAGTATG |
| GAPDH-R | GGTGGAAGAATGGGAGTTGCT |
| Slc38a2-F | CGTTCACCTCCTCCTCAAGACT |
| Slc38a2-R | TTCAGATACCACAGCCCATTCG |
| Slc38a1-F | CGTTCACCTCCTCCTCAAGACT |
| Slc38a1-R | TTCAGATACCACAGCCCATTCG |
| Slc38a4-F | ATGAAGATGCCGAAAGTCAGAAG |
| Slc38a4-R | GGTGAACCGAGTAGAGCGATAGA |
| Slc43a1-F | TTCTATTCCAGTCTATGCCCAGC |
| Slc43a1-R | CAAGGCCATAAGAGTGCAGGAT |
| Slc43a2-F | TGGGCATCATCATGGACAAGTAT |
| Slc43a2-R | AAGGTAACTGCTGAGGAAGCGTAG |
| Slc6a6-F | GAAGGGTTATCGTCGGGAAAT |
| Slc6a6-R | ATACATGCCACCCTCCGTCA |
| Slc1a1-F | ATCGTGGTAGGAGTCTTGGTTCG |
| Slc1a1-R | AGGATTACAGCAATGACGGTGGT |
| Slc6a9-F | ACTACGCAGCCAGCTTCTCCTT |
| Slc6a9-R | TGGTAGTGGTTGTAAGTGATTGGC |
表1 引物序列
Tab.1 Sequences of primers for RT-qPCR
| Name of primers | Primer sequence 5'-3' |
|---|---|
| GAPDH-F | CTGGAGAAACCTGCCAAGTATG |
| GAPDH-R | GGTGGAAGAATGGGAGTTGCT |
| Slc38a2-F | CGTTCACCTCCTCCTCAAGACT |
| Slc38a2-R | TTCAGATACCACAGCCCATTCG |
| Slc38a1-F | CGTTCACCTCCTCCTCAAGACT |
| Slc38a1-R | TTCAGATACCACAGCCCATTCG |
| Slc38a4-F | ATGAAGATGCCGAAAGTCAGAAG |
| Slc38a4-R | GGTGAACCGAGTAGAGCGATAGA |
| Slc43a1-F | TTCTATTCCAGTCTATGCCCAGC |
| Slc43a1-R | CAAGGCCATAAGAGTGCAGGAT |
| Slc43a2-F | TGGGCATCATCATGGACAAGTAT |
| Slc43a2-R | AAGGTAACTGCTGAGGAAGCGTAG |
| Slc6a6-F | GAAGGGTTATCGTCGGGAAAT |
| Slc6a6-R | ATACATGCCACCCTCCGTCA |
| Slc1a1-F | ATCGTGGTAGGAGTCTTGGTTCG |
| Slc1a1-R | AGGATTACAGCAATGACGGTGGT |
| Slc6a9-F | ACTACGCAGCCAGCTTCTCCTT |
| Slc6a9-R | TGGTAGTGGTTGTAAGTGATTGGC |
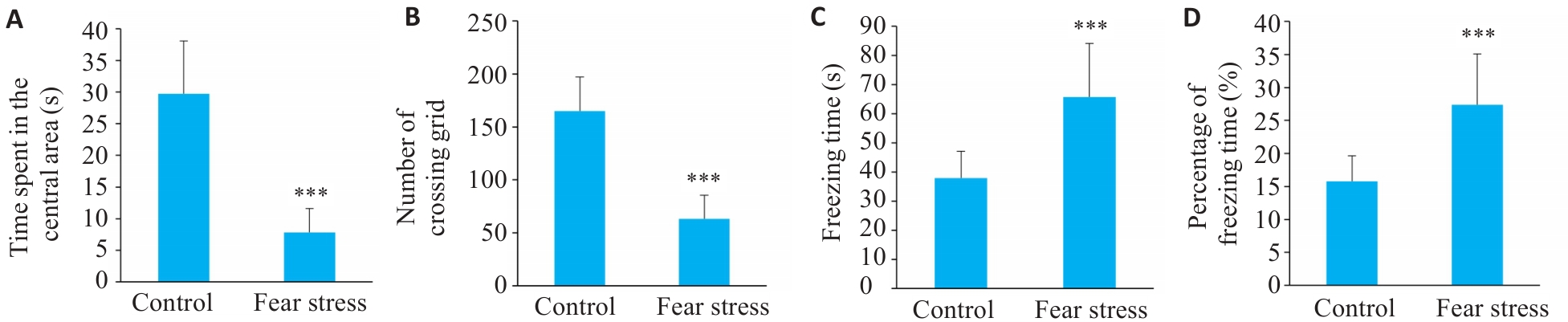
图1 孕期恐应激对孕鼠行为学的影响
Fig.1 Impact of prenatal fear stress on behaviors of pregnant rats. A: Time spent in the central area in open field test; B: Number of grid crossings in open field test; C: Freezing time in contextual Fear Paradigm; D: Percentage of freezing time in contextual Fear Paradigm. ***P<0.001 vs Control group.
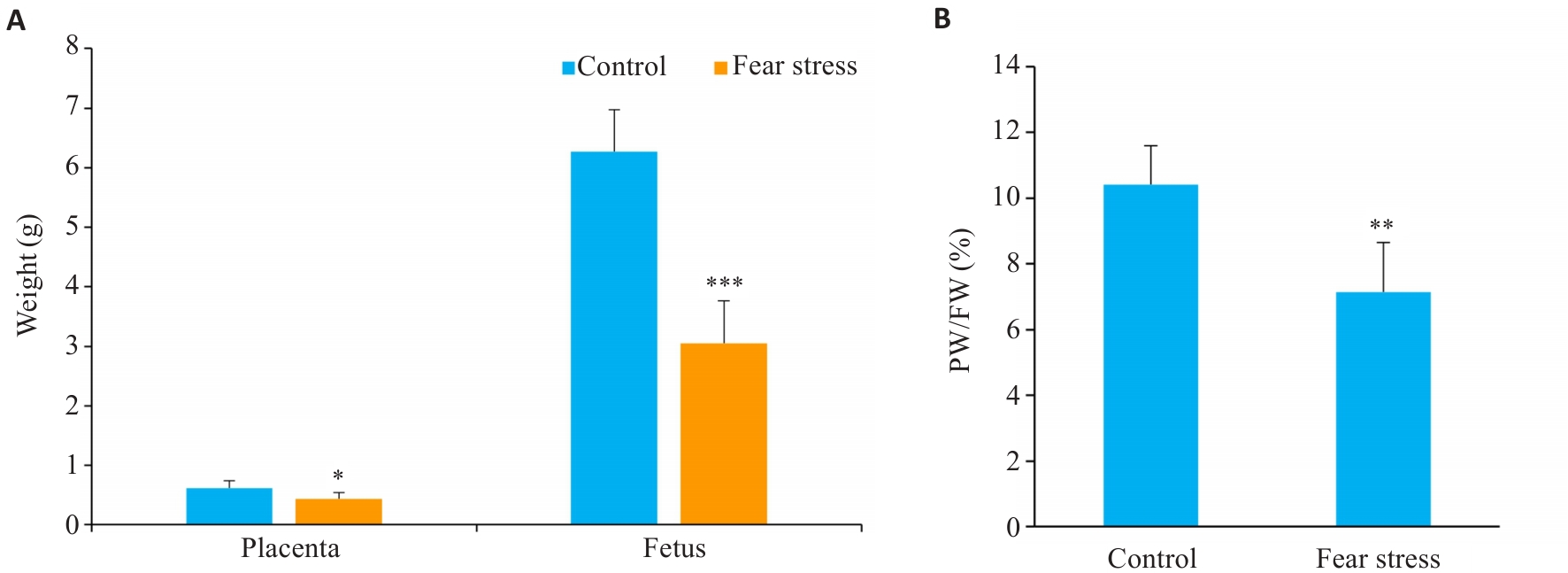
图2 孕期恐应激对胎盘胎鼠重量的影响
Fig.2 Impact of prenatal fear stress on placental weight (PW) and fetal weight (FW). A: Placental and fetal weight; B: Placental-Fetal ratio. *P<0.05,**P<0.01,***P<0.001 vs Control group.
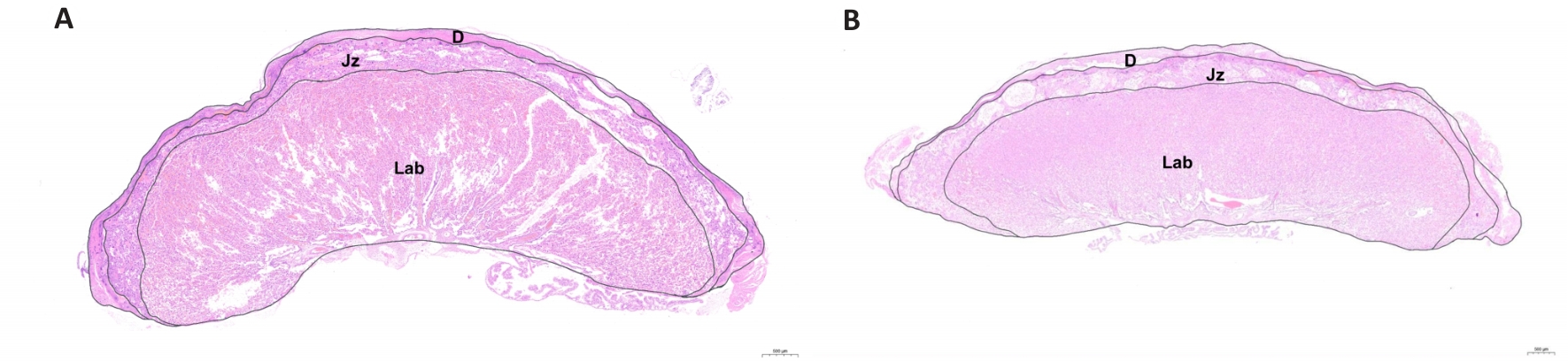
图3 孕期恐应激对胎盘结构的影响
Fig.3 Effect of prenatal fear stress on placental structure (HE staining, Scale bar=500 μm). A: Control group. B: Fear stress group. D: Decidua zone; Jz: Junctional zone; Lab: Labyrinth zone.
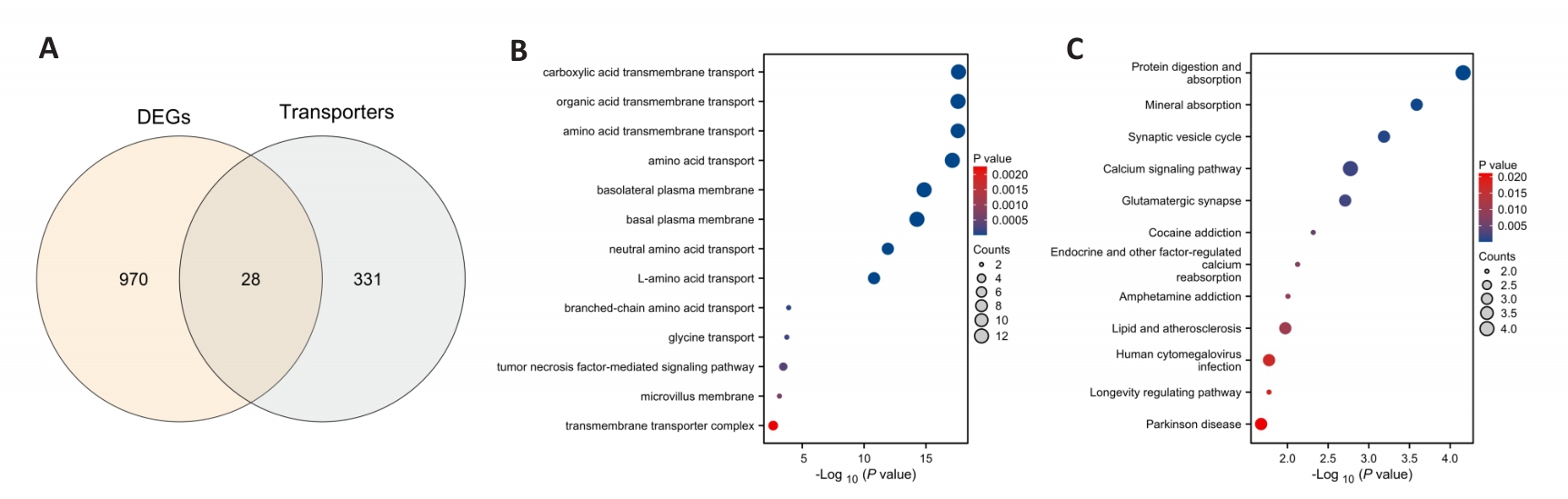
图4 孕期恐应激胎盘的生物信息学分析
Fig.4 Bioinformatics analysis of the placenta under prenatal fear stress. A: Venn diagram. B: Gene ontology analysis. C: Kyoto encyclopedia of genes and genomes pathway analysis. DEGs: Differentially expressed genes.
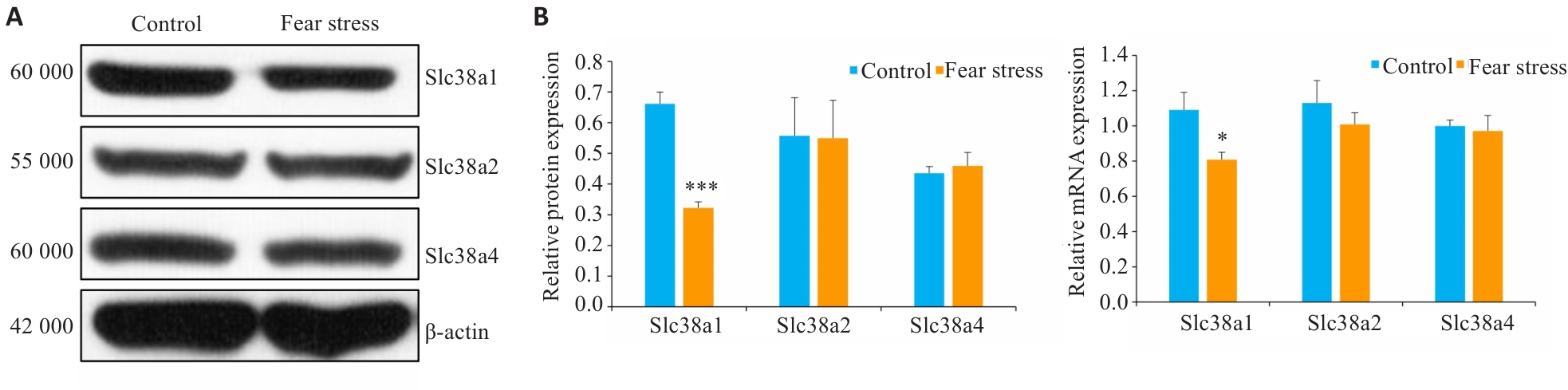
图5 孕期恐应激对胎盘A系氨基酸转运体mRNA与蛋白表达的影响
Fig.5 Effect of prenatal fear stress on protein (A) and mRNA (B) expressions of system A amino acid transporters in the placenta. *P<0.05, ***P<0.001 vs Control group.
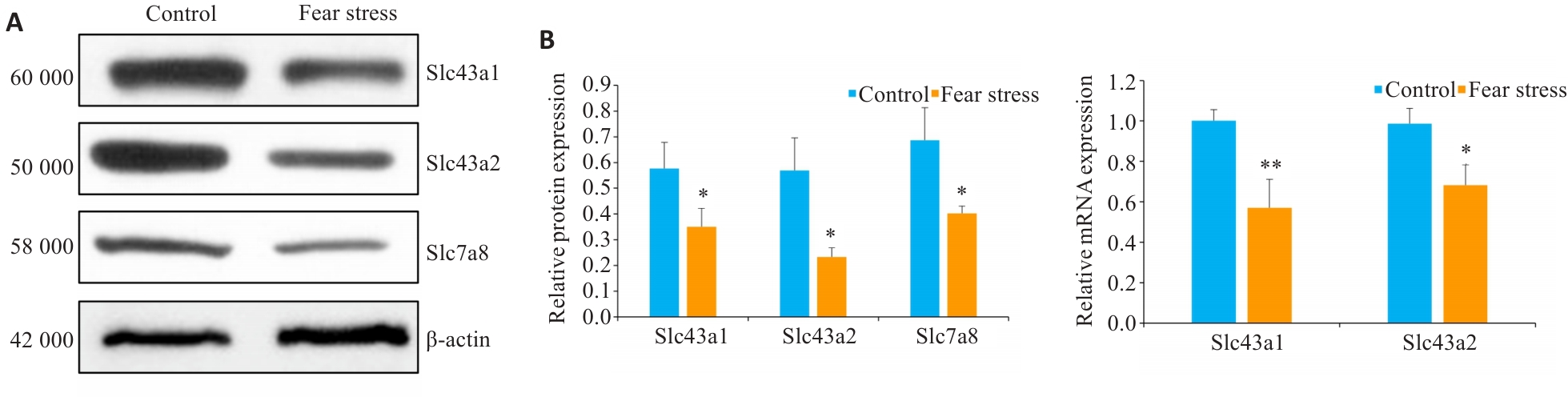
图6 孕期恐应激对胎盘L系氨基酸转运体mRNA与蛋白表达的影响
Fig.6 Effect of prenatal fear stress on protein (A) and mRNA (B) expressions of system L amino acid transporters in the placenta. *P<0.05, **P<0.01 vs Control group.
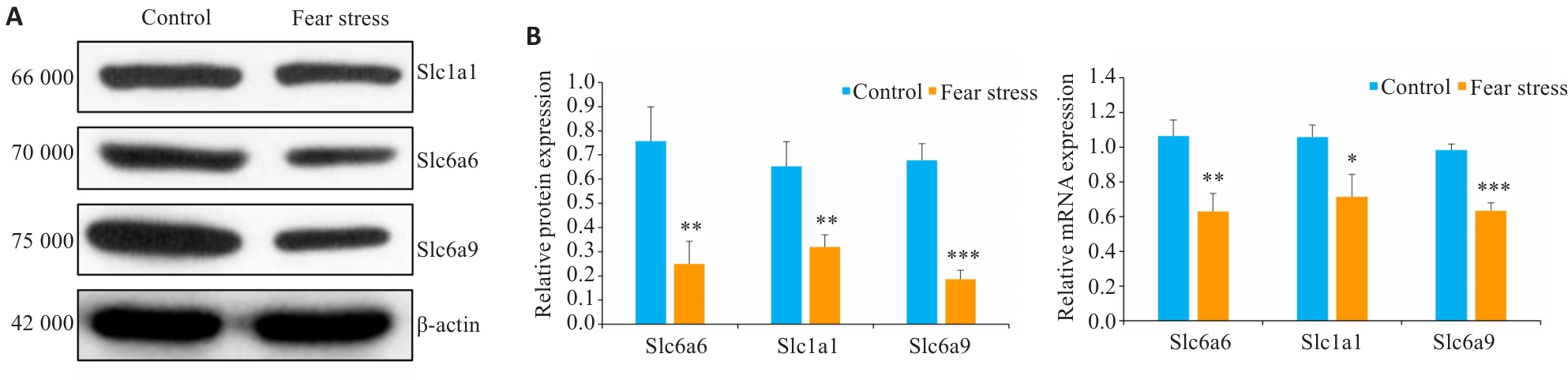
图7 孕期恐应激对Slc6a6、Slc1a1与Slc6a9的mRNA与蛋白表达的影响
Fig.7 Effect of prenatal fear stress on protein (A) and mRNA (B) expressions of Slc6a6, Slc1a1 and Slc6a9. *P<0.05, **P<0.01,***P<0.001 vs Control group.
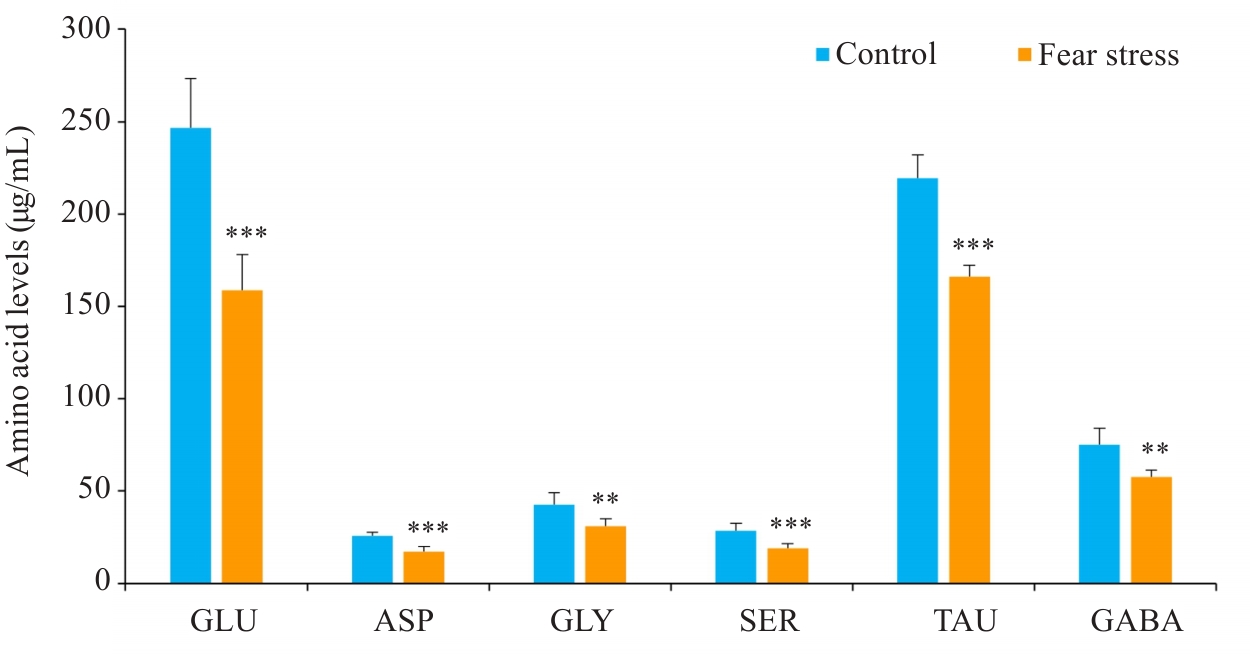
图8 孕期恐应激胎鼠血清氨基酸的影响
Fig.8 Effect of prenatal fear stress on serum amino acid levels in fetal mice.GLU: Glutamate; ASP: Aspartate; GLY: Glycine; SER: Serine; TAU: Taurine; GABA: Gamma-aminobutyric acid. **P<0.01,***P<0.001 vs Control group.
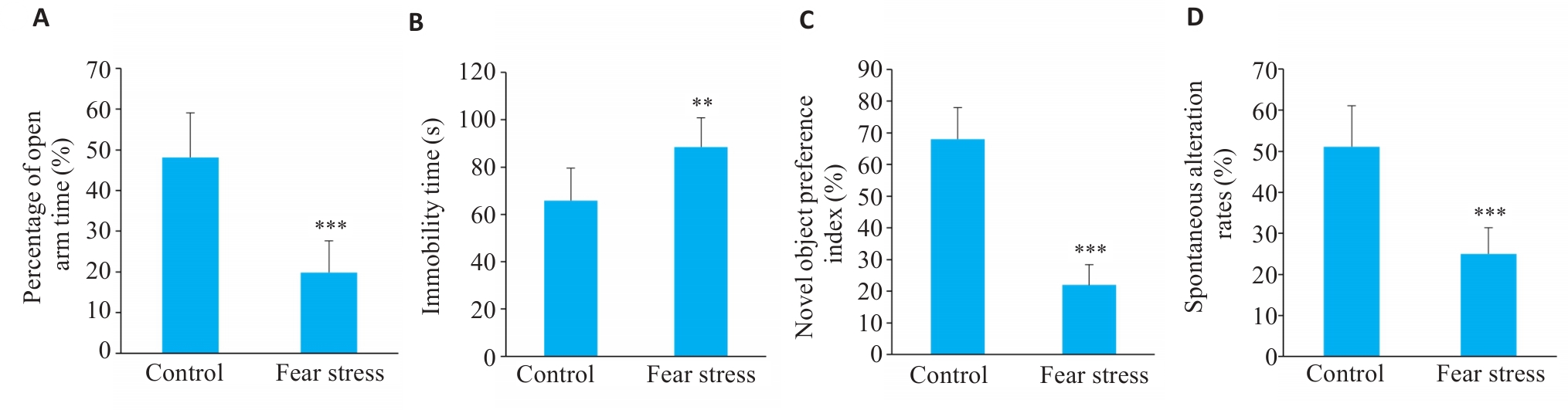
图9 孕期恐应激对子鼠行为学的影响
Fig.9 Effect of prenatal fear stress on behaviors of adult offspring rats. A: Percentage of open arm time in elevated plus maze test. B: Immobility time in tail suspension test. C: Novel object preference index in novel object recognition test. D: Spontaneous alternation rate in Y-maze test (n=10). **P<0.01,***P<0.001 vs Control group.
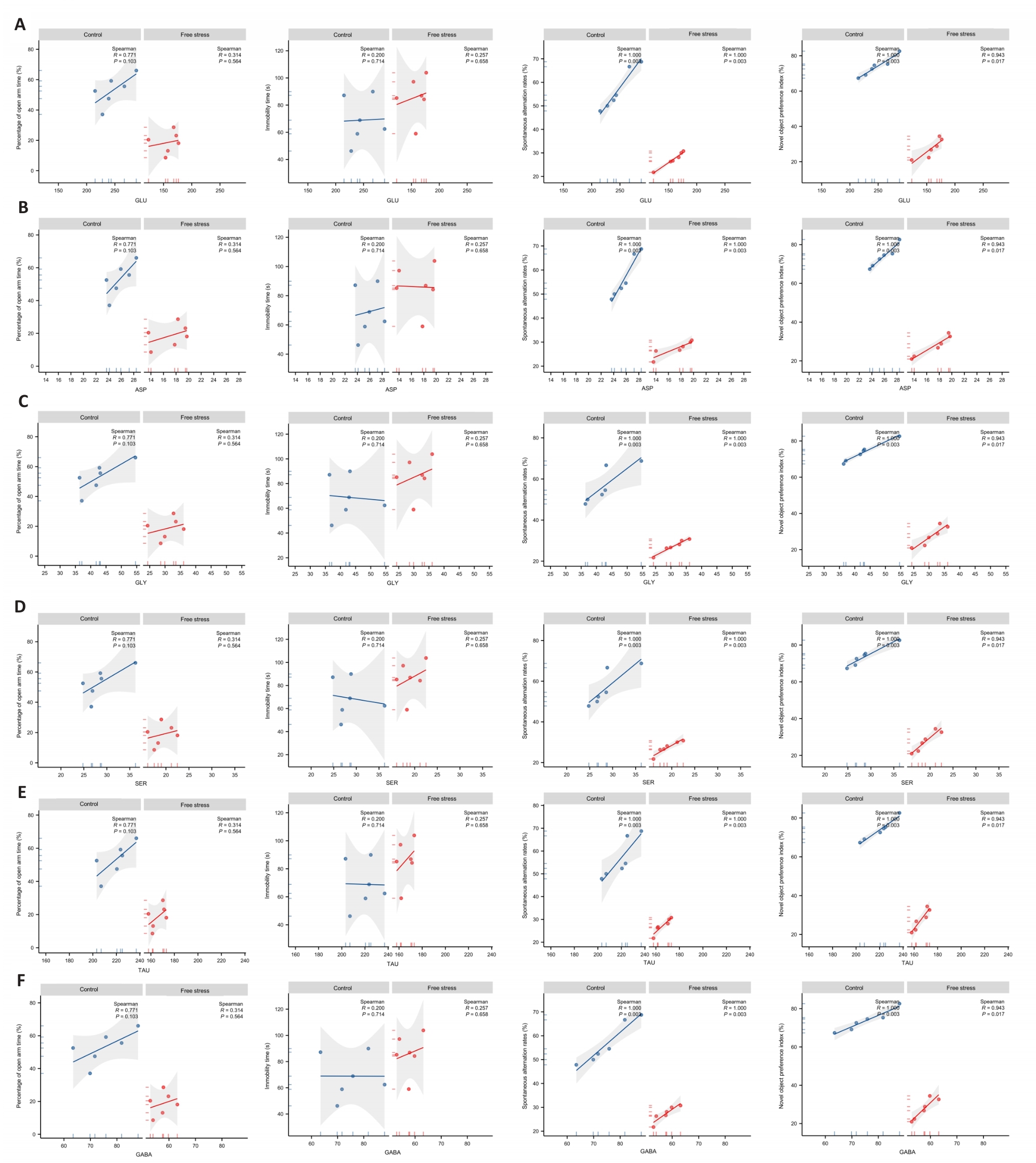
图10 相关性分析
Fig.10 Correlation analysis of serum glutamate (A), aspartate (B), glycine (C), serine (D), taurine (E) and gamma-aminobutyric acid (F) levels with behavioral performance in fetal rats.
| [1] | Li B, Liu T, Ma D, et al. Association of fear of childbirth and postpartum depression with perceived partner response during pregnancy[J]. BMC Pregnancy Childbirth, 2025, 25(1): 211. doi:10.1186/s12884-025-07332-6 |
| [2] | Jing Q, Jie J, Ke X, et al. The relationship between fear of childbirth and prenatal depression in pregnant women during pregnancy: a cross-lagged analysis[J]. BMC Pregnancy Childbirth, 2025, 25(1): 192. doi:10.1186/s12884-025-07321-9 |
| [3] | Levendosky AA, Grimm KJ, Lonstein JS, et al. Pinpointing the timing of prenatal stress associated with infant biobehavioral reactivity[J]. Psychoneuroendocrinology, 2025, 173: 107368. doi:10.1016/j.psyneuen.2025.107368 |
| [4] | Li L, Zhang W, Sun C, et al. Scutellariae Radix ameliorates prenatal stress-induced anxiety-like and depression-like behavior in the offspring via reversing HPA axis hyperfunction and ameliorating neurodevelopmental dysfunction[J]. Dev Neurosci, 2024: 1-19. doi:10.1159/000543152 |
| [5] | Cheng J, Jin H, Zhang Y, et al. Small for gestational age children at risk: Identifying placenta-brain axis genes as biomarkers for early prediction of neurodevelopmental delay[J]. Life Sci, 2025, 365: 123450. doi:10.1016/j.lfs.2025.123450 |
| [6] | Castro-Quintas A, Palma-Gudiel H, Eixarch E, et al. Placental epigenetic signatures of maternal distress in glucocorticoid-related genes and newborn outcomes: a study of Spanish primiparous women[J]. Eur Neuropsychopharmacol, 2025, 90: 36-47. doi:10.1016/j.euroneuro.2024.10.001 |
| [7] | Botía M, Escribano D, Tecles F, et al. Changes in Cortisol, cortisone and 11β-hydroxysteroid dehydrogenase type II activity in saliva during pregnancy and lactation in sows[J]. Domest Anim Endocrinol, 2024, 89: 106875. doi:10.1016/j.domaniend.2024.106875 |
| [8] | Heynen JP, McHugh RR, Boora NS, et al. Urinary 1H NMR metabolomic analysis of prenatal maternal stress due to a natural disaster reveals metabolic risk factors for non-communicable diseases: the QF2011 Queensland flood study[J]. Metabolites, 2023, 13(4): 579. doi:10.3390/metabo13040579 |
| [9] | Cho SKS, Darby JRT, Saini BS, et al. Late-gestation maternal undernutrition induces circulatory redistribution while preserving uteroplacental function independent of fetal glycaemic state[J]. J Physiol, 2024, 602(24): 7065-83. doi:10.1113/jp287171 |
| [10] | Liu S, Hua L, Mo X, et al. Comparative impact of alternate-day fasting and time-restricted feeding on placental function and fetal development in maternal obesity[J]. Nutrients, 2024, 17(1): 25. doi:10.3390/nu17010025 |
| [11] | Oliveira TRDP, Lima-Oliveira DP, de Paula MBM, et al. Consequences of the modulation of gestational resistance training intensity for placental cell composition and nutrient transporter expression[J]. Placenta, 2025, 161: 55-64. doi:10.1016/j.placenta.2025.01.012 |
| [12] | Pereira-Carvalho D, Chagas Valim AC, Borba Vieira Andrade C, et al. Sex-specific effect of antenatal Zika virus infection on murine fetal growth, placental nutrient transporters, and nutrient sensor signaling pathways[J]. FASEB J, 2024, 38(13): e23799. doi:10.1096/fj.202301951rr |
| [13] | Schroeder M, Fuenzalida B, Yi N, et al. LAT1-dependent placental methionine uptake is a key player in fetal programming of metabolic disease[J]. Metabolism, 2024, 153: 155793. doi:10.1016/j.metabol.2024.155793 |
| [14] | Jia Q, Guo X, Cao Q, et al. Assisted reproductive technology causes reduced expression of amino acid transporters in human full-term placentas[J]. Pathol Res Pract, 2022, 239: 154169. doi:10.1016/j.prp.2022.154169 |
| [15] | Duan BB, Ran SJ, Wu L, et al. Maternal supplementation spermidine during gestation improves placental angiogenesis and reproductive performance of high prolific sows[J]. J Nutr Biochem, 2025, 136: 109792. doi:10.1016/j.jnutbio.2024.109792 |
| [16] | 张玉荣, 王瑞忠, 陈 蕊, 等. 产前应激子代大鼠海马Wnt/β-catenin信号通路的改变诱导抑郁和焦虑样行为[J]. 南方医科大学学报, 2019, 39(2): 222-6. doi:10.12122/j.issn.1673-4254.2019.09.15 |
| [17] | Aldinger JK, Abele H, Kranz A. Prenatal maternal psychological stress (PMPS) and its effect on the maternal and neonatal outcome: a retrospective cohort study[J]. Healthcare: Basel, 2024, 12(23): 2431. doi:10.3390/healthcare12232431 |
| [18] | Ren FY, Zhu XW, Liu JN, et al. Associations of multiple risk factors with prenatal depression and anxiety: Evidence from the Tianjin Birth Cohort (TJBC) study[J]. J Affect Disord, 2024, 366: 411-22. doi:10.1016/j.jad.2024.08.122 |
| [19] | Wu Y, De Asis-Cruz J, Limperopoulos C. Brain structural and functional outcomes in the offspring of women experiencing psychological distress during pregnancy[J]. Mol Psychiatry, 2024, 29(7): 2223-40. doi:10.1038/s41380-024-02449-0 |
| [20] | 宋 琦, 杜志欣, 杨丽萍, 等. 恐惧应激对妊娠期大鼠胎盘葡萄糖转运体表达水平的影响[J]. 中国实验动物学报, 2024, 32(7): 828-35. |
| [21] | Jiang Y, Zhang T, Yang LP, et al. Downregulation of FTO in the hippocampus is associated with mental disorders induced by fear stress during pregnancy[J]. Behav Brain Res, 2023, 453: 114598. doi:10.1016/j.bbr.2023.114598 |
| [22] | 吴永叶, 杨丽萍, 张振强, 等. 五行音乐对孕期恐应激子代社交行为的影响及机制研究[J]. 中国比较医学杂志, 2024, 34(4): 28-34. |
| [23] | Li QH, Zhang QZ, Su SL, et al. Maternal fish oil supplementation enhances nutrient transport in the placenta and milk biosynthesis in the mammary gland via the GPR120 signaling pathway[J]. J Adv Res, 2024, 1232(24): 607-16. |
| [24] | Vrooman LA, Rhon-Calderon EA, Suri KV, et al. Placental abnormalities are associated with specific windows of embryo culture in a mouse model[J]. Front Cell Dev Biol, 2022, 10: 884088. doi:10.3389/fcell.2022.884088 |
| [25] | Wang L, Wang H, Luo J, et al. Decorin promotes decidual M1-like macrophage polarization via mitochondrial dysfunction resulting in recurrent pregnancy loss[J]. Theranostics, 2022, 12(17): 7216-36. doi:10.7150/thno.78467 |
| [26] | Kadife E, Harper A, De Alwis N, et al. SLC38A4 amino acid transporter expression is significantly lower in early preterm intrauterine growth restriction complicated placentas[J]. Int J Mol Sci, 2022, 24(1): 403. doi:10.3390/ijms24010403 |
| [27] | Bourdon A, Hannigsberg J, Misbert E, et al. Maternal supplementation with citrulline or arginine during gestation impacts fetal amino acid availability in a model of intrauterine growth restriction (IUGR)[J]. Clin Nutr, 2020, 39(12): 3736-43. doi:10.1016/j.clnu.2020.03.036 |
| [28] | Rosario FJ, Barentsen K, Powell TL, et al. Trophoblast-specific overexpression of the LAT1 increases transplacental transport of essential amino acids and fetal growth in mice[J]. PNAS Nexus, 2024, 3(6): pgae207. doi:10.1093/pnasnexus/pgae207 |
| [29] | Furukawa T, Fukuda A. Maternal taurine as a modulator of Cl- homeostasis as well as of Glycine/GABAA receptors for neocortical development[J]. Front Cell Neurosci, 2023, 17: 1221441. doi:10.3389/fncel.2023.1221441 |
| [30] | Noorlander CW, de Graan PNE, Nikkels PGJ, et al. Distribution of glutamate transporters in the human placenta[J]. Placenta, 2004, 25(6): 489-95. doi:10.1016/j.placenta.2003.10.018 |
| [31] | Crouse MS, McLean KJ, Greseth NP, et al. The effects of maternal nutrient restriction and day of early pregnancy on the location and abundance of neutral amino acid transporters in beef heifer utero-placental tissues[J]. J Anim Sci, 2020, 98(7): skaa197. doi:10.1093/jas/skaa197 |
| [32] | McColl ER, Piquette-Miller M. Poly(I: C) alters placental and fetal brain amino acid transport in a rat model of maternal immune activation[J]. Am J Reprod Immunol, 2019, 81(6): e13115. doi:10.1111/aji.13115 |
| [33] | Feng C, Wu Y, Zhang X, et al. Maternal milk fat globule membrane enriched gut L. murinus and circulating SCFAs to improve placental efficiency and fetal development in intrauterine growth restricted mice model[J]. Gut Microbes, 2025, 17(1): 2449095. doi:10.1080/19490976.2024.2449095 |
| [34] | Ferreira-Rodrigues M, Sousa IS, Baptista FI, et al. Stress in utero: prenatal dexamethasone exposure causes greater structural gliovascular alterations in female offspring than in males[J]. Front Neurosci, 2025, 19: 1539867. doi:10.3389/fnins.2025.1539867 |
| [1] | 谢潇潇, 赵青冬, 胡凌云, 姜淑芳, 王晓萍, 张文玲, 李 珍, 游艳琴, 卢彦平. 非侵入性产前检测对胎儿罕见染色体三体的检测价值[J]. 南方医科大学学报, 2023, 43(12): 2071-2077. |
| [2] | 谢潇潇, 赵青冬, 付玉荣, 张文玲, 孟元光, 卢彦平. 11号染色体三体嵌合体病例的遗传学检测及分析[J]. 南方医科大学学报, 2022, 42(7): 1057-1061. |
| [3] | 何建萍, 唐 健, 苏 虹, 沈翠花, 罗胜军, 王海涛, 钱 源, 吕梦欣. 唐氏综合征胎盘差异miRNA表达谱分析: 基于全转录组测序分析技术[J]. 南方医科大学学报, 2022, 42(3): 418-424. |
| [4] | 高俊杰, 杨丹丹, 曹若雪, 潘雪珊, 夏 俊. 天然虾青素治疗肾透明细胞癌的作用机制:基于网络药理学与生物信息学方法[J]. 南方医科大学学报, 2021, 41(12): 1763-1772. |
| [5] | 吴淑贞,张慧珊,刘雁,王瑞,叶少欣,曾萌,刘正平. 胎盘植入组织lncRNA表达特征与ceRNA调控网络构建[J]. 南方医科大学学报, 2019, 39(10): 1253-. |
| [6] | 周芝熠,李晓娟,蒋国庆,王珏,钱源. 维生素D通过下调miR-21的表达促进人胎盘滋养细胞的迁移和侵袭[J]. 南方医科大学学报, 2019, 39(04): 437-. |
| [7] | 田鎏,廖晖淇,杨慧,马妮,张昌军,刁红录. FABP7 在小鼠胎盘组织及人滋养层细胞HTR-8/Svneo中的表达[J]. 南方医科大学学报, 2017, 37(05): 594-. |
| [8] | 彭永保,黄淑晖,张俊明,罗勇,周群,刘淮. 孕中期热暴露对大鼠子代宫内发育及胎盘HSP70、Bax、Bcl-2表达的影响[J]. 南方医科大学学报, 2017, 37(01): 89-. |
| [9] | 张璐,张腾令,宗滕,陈艺璐,任敏,俞晓春,况海斌. 妊娠期邻苯二甲酸二(2-乙基)己酯暴露对小鼠胎盘生长发育的影响[J]. 南方医科大学学报, 2016, 36(04): 467-. |
| [10] | 林 靓,黄云鹏,余艳红,杨 茵. 重度子痫前期PIBF的表达及其与免疫耐受失衡的关系[J]. 南方医科大学学报, 2015, 35(06): 848-. |
| [11] | 黄赟博,刘倩倩,余艳红. 胎儿生长受限与血管生成因子的关系[J]. 南方医科大学学报, 2014, 34(07): 1068-. |
| [12] | 张园,钟梅,刘凤岩. 低分子肝素抑制子痫前期样大鼠胎盘细胞凋亡[J]. 南方医科大学学报, 2012, 32(06): 862-. |
| [13] | 刘大艳,陈士岭,王晨虹,罗雪梅,黄芳芳. 早发型与晚发型重度子痫前期患者胎盘绒毛组织代谢足迹差异的研究[J]. 南方医科大学学报, 2011, 31(09): 1547-. |
| [14] | 高云飞; 余艳红; 李志琴; . ADM基因在正常孕妇与子痫前期孕妇妊娠晚期胎盘组织表达的研究[J]. 南方医科大学学报, 2006, 26(12): 1828-1830. |
| [15] | 刘春城; 刘青云; 黄莺莺;. 胎盘早剥36例临床分析[J]. 南方医科大学学报, 2006, 26(06): 876-876. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||