Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (6): 1289-1296.doi: 10.12122/j.issn.1673-4254.2025.06.18
Previous Articles Next Articles
Wei SU1( ), Houhua LAI2, Xin TANG1, Qun ZHOU1, Yachun TANG1, Hao FU1, Xuancai CHEN1(
), Houhua LAI2, Xin TANG1, Qun ZHOU1, Yachun TANG1, Hao FU1, Xuancai CHEN1( )
)
Received:2024-09-13
Online:2025-06-20
Published:2025-06-27
Contact:
Xuancai CHEN
E-mail:suwei022069@163.com;Chenxuancai2015@163.com
Wei SU, Houhua LAI, Xin TANG, Qun ZHOU, Yachun TANG, Hao FU, Xuancai CHEN. Apelin promotes proliferation, migration, and angiogenesis in bladder cancer by activating the FGF2/FGFR1 pathway[J]. Journal of Southern Medical University, 2025, 45(6): 1289-1296.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.06.18
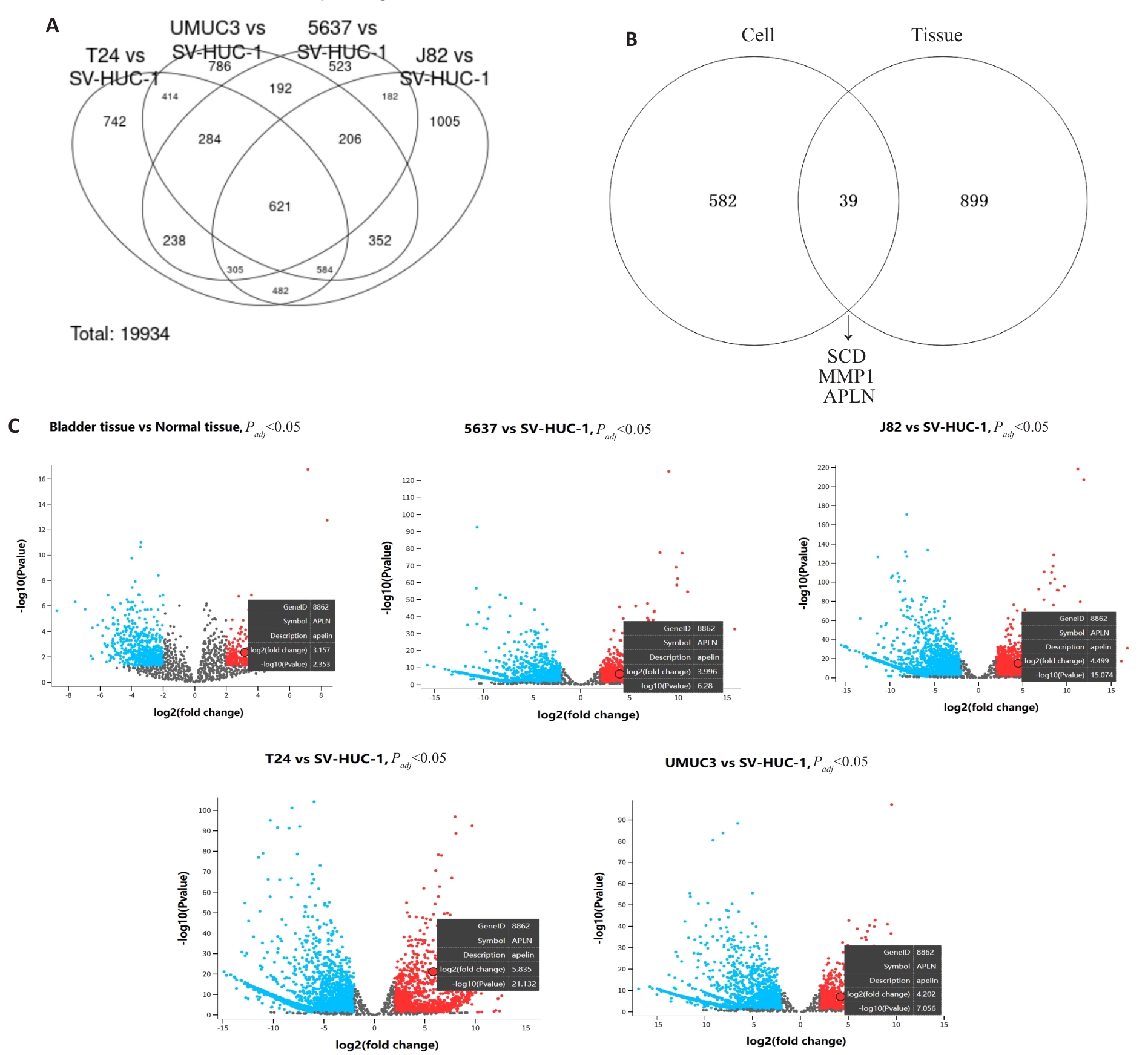
Fig.1 Identification of differentially expressed genes (DEGs) in bladder cancer tissues and cells from GEO datasets. A: Venn diagram showing common DEGs between SV-HUC-1 and 4 bladder cancer cell lines (5637, UMUC3, T24 and J82) in the GSE231383 dataset. B: Venn diagram identifying common DEGs across two GEO datasets. C: Volcano plot of DEGs from two independent GEO datasets, showing upregulated APLN expression in bladder cancer tissues/cells (screening criteria: |log FC|≥2, P<0.05).
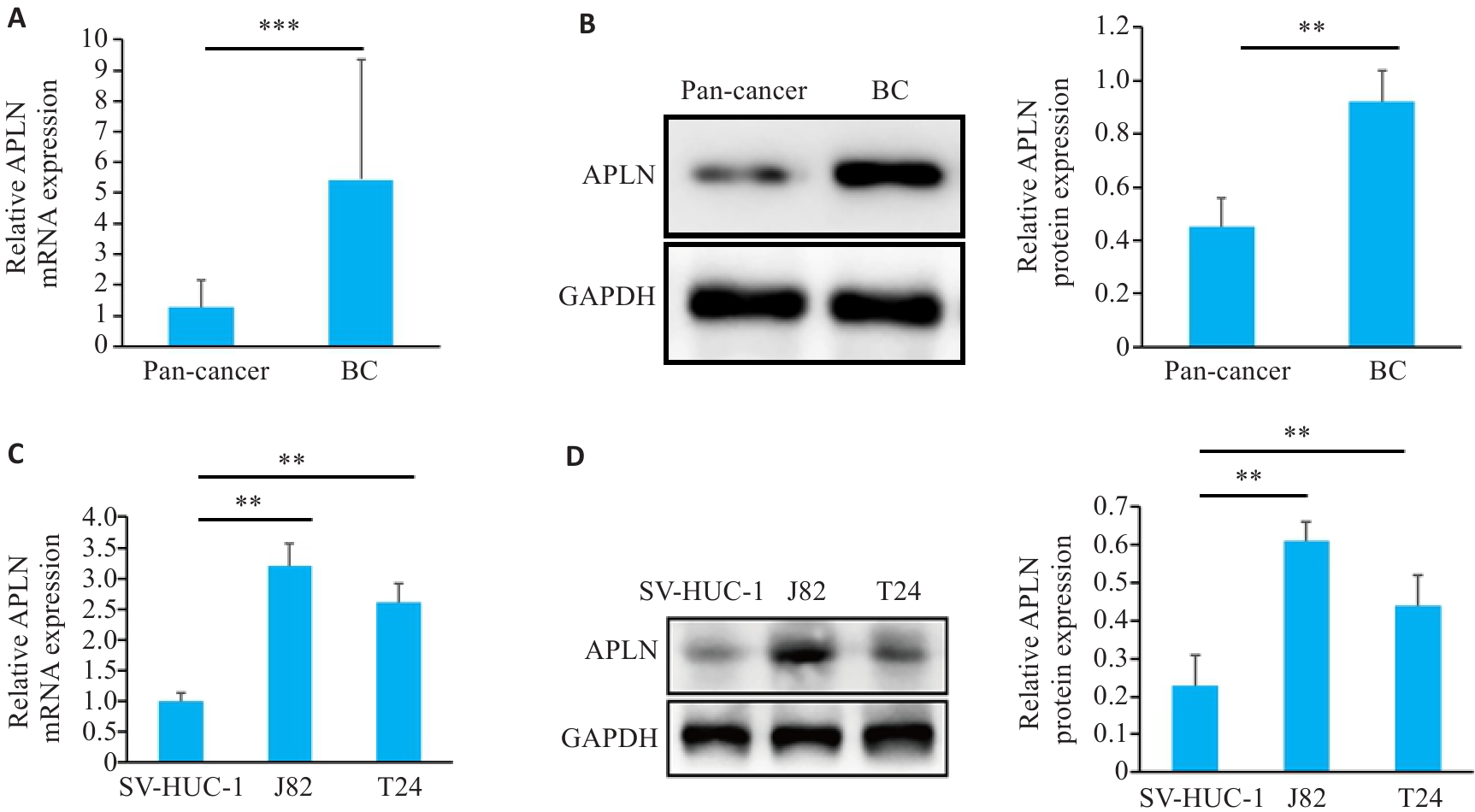
Fig.2 Apelin (APLN) expression in bladder cancer tissues and cells. A: qRT-PCR for detecting APLN mRNA expression in bladder cancer tissues and normal tissues (n=60). B: Western blotting for detecting APLN protein expression in bladder cancer tissues and normal tissues (n=5). C, D: qRT-PCR and Western blotting for detecting APLN expression in bladder cancer cells and SV-HUC-1 cells. Each experiment was repeated 3 times. **P<0.01, ***P<0.001.
| Characteristics | Case | APLN Expression | P | |
|---|---|---|---|---|
| High (n=30) | Low (n=30) | |||
| Age(year) | 0.796 | |||
| ≥60 | 32 | 15 | 13 | |
| <60 | 28 | 15 | 17 | |
| Gender | 0.158 | |||
| Female | 18 | 6 | 12 | |
| Male | 42 | 24 | 18 | |
| Tumor size (cm) | 0.438 | |||
| <3 | 28 | 12 | 16 | |
| ≥3 | 32 | 18 | 14 | |
| Invasion | 0.019 | |||
| T0-T2 | 30 | 10 | 20 | |
| T3-T4 | 30 | 20 | 10 | |
| Distant metastasis | 0.037 | |||
| Yes | 33 | 21 | 22 | |
| No | 27 | 9 | 8 | |
| TNM stage | 0.035 | |||
| 0-II | 35 | 13 | 22 | |
| III-IV | 25 | 17 | 8 | |
| Histological grade | 0.438 | |||
| High/intermediate | 28 | 16 | 12 | |
| Low | 32 | 14 | 18 | |
Tab.1 Correlation of APLN mRNA expression with clinico-pathological features of patients with bladder cancer (n)
| Characteristics | Case | APLN Expression | P | |
|---|---|---|---|---|
| High (n=30) | Low (n=30) | |||
| Age(year) | 0.796 | |||
| ≥60 | 32 | 15 | 13 | |
| <60 | 28 | 15 | 17 | |
| Gender | 0.158 | |||
| Female | 18 | 6 | 12 | |
| Male | 42 | 24 | 18 | |
| Tumor size (cm) | 0.438 | |||
| <3 | 28 | 12 | 16 | |
| ≥3 | 32 | 18 | 14 | |
| Invasion | 0.019 | |||
| T0-T2 | 30 | 10 | 20 | |
| T3-T4 | 30 | 20 | 10 | |
| Distant metastasis | 0.037 | |||
| Yes | 33 | 21 | 22 | |
| No | 27 | 9 | 8 | |
| TNM stage | 0.035 | |||
| 0-II | 35 | 13 | 22 | |
| III-IV | 25 | 17 | 8 | |
| Histological grade | 0.438 | |||
| High/intermediate | 28 | 16 | 12 | |
| Low | 32 | 14 | 18 | |
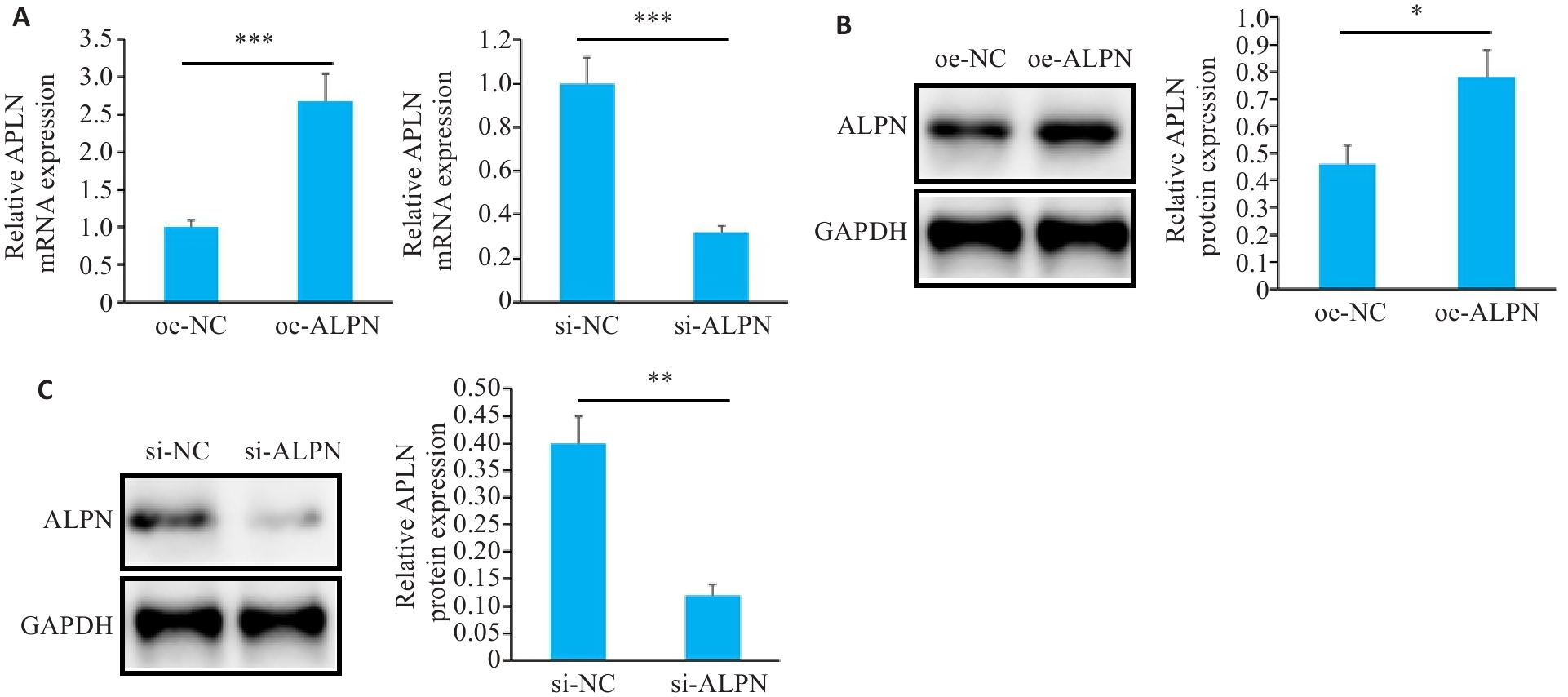
Fig.3 APLN expression in J82 cells after transfection. A: qRT-PCR for detecting APLN mRNA expression in each group of J82 cells. B, C: Western blotting for detecting APLN protein expression in each group of J82 cells. Each experiment was repeated 3 times. *P<0.05, **P<0.01, ***P<0.001.
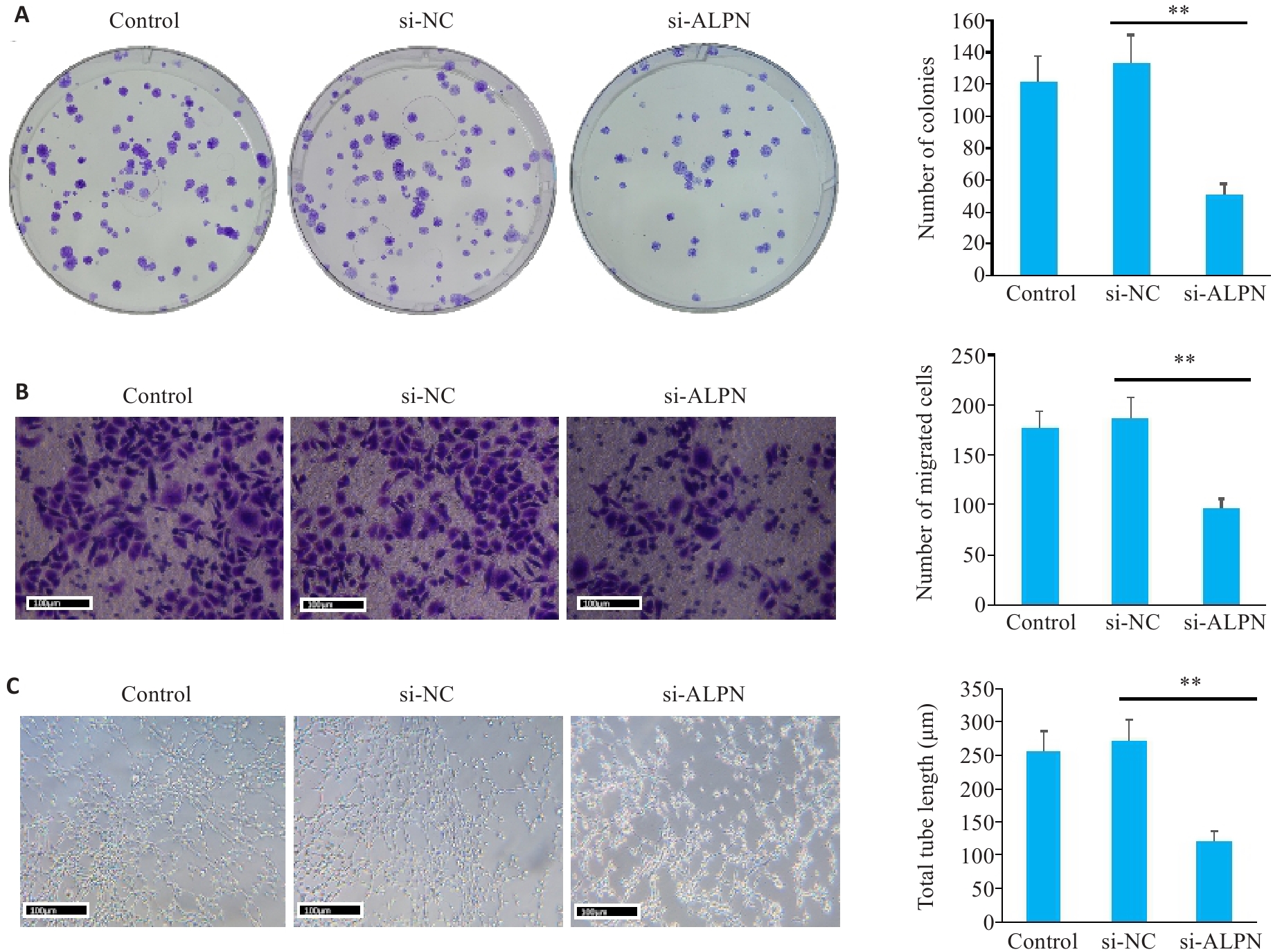
Fig.4 Proliferation, migration and angiogenesis of J82 cells after transfection. A: Plate cloning assayfor assessing J82 cell proliferation in each group. B: Transwell assay for evaluating cell migration in each group. C: Angiogenesis assay for assessing HUVEC tube formation in each group. Each experiment was repeated 3 times. Scale bar=100 μm. **P<0.01.
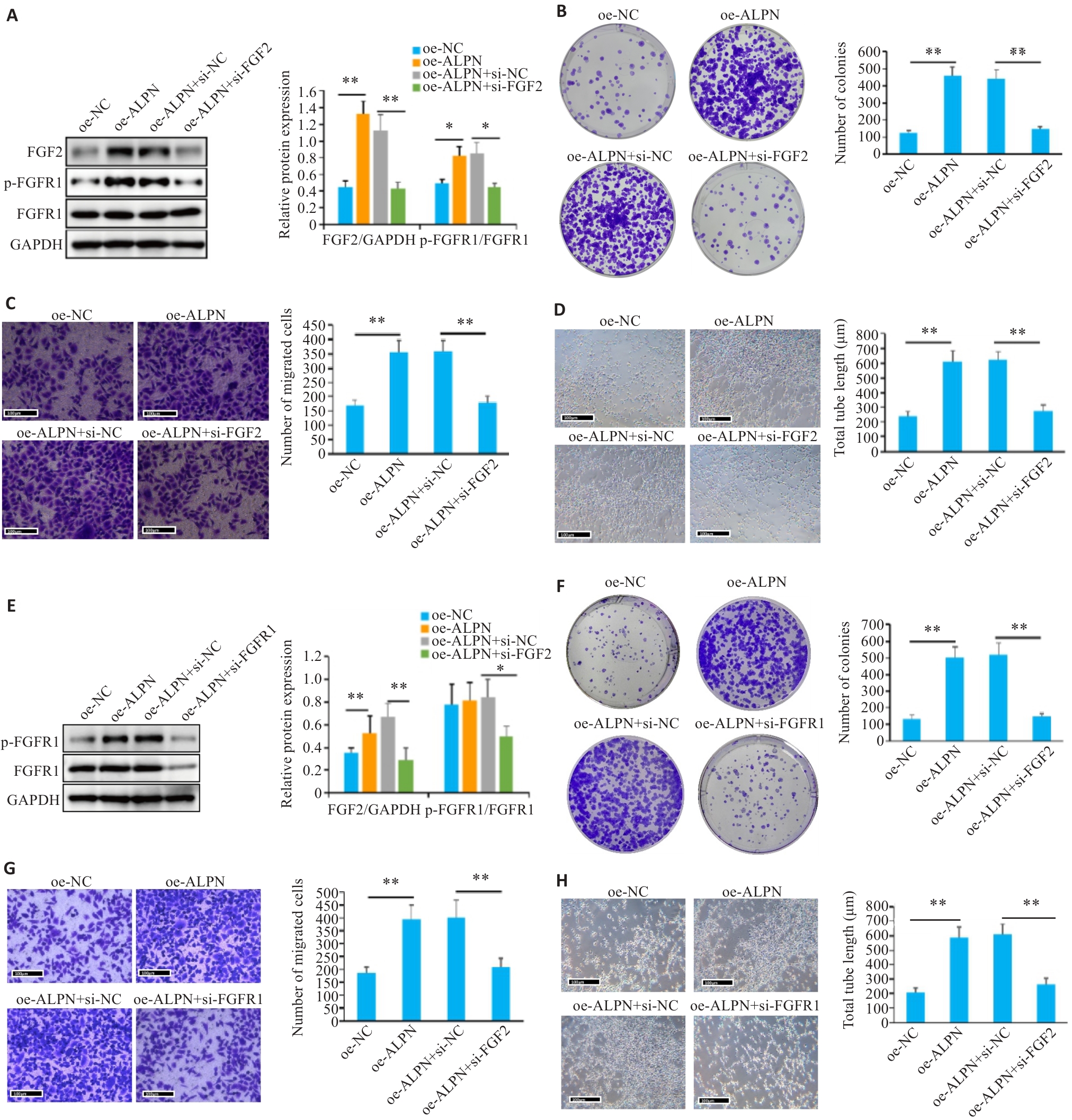
Fig.5 Proliferation, migration, angiogenesis and FGF2/FGFR1 signaling in J82 cells after transfection. A, E: Western blotting for detecting FGF2 expression and FGFR1 phosphorylation in different groups. B, F: Plate cloning assay for assessing J82 cell proliferation. C, G: Transwell assay for evaluating cell migration. D, H: Angiogenesis assay for assessing HUVEC tube formation. Each experiment was repeated 3 times. Scale bar=100 μm. *P<0.05, **P<0.01.
| 1 | Lee YL, Chien TW, Wang JC. Using Sankey diagrams to explore the trend of article citations in the field of bladder cancer: Research achievements in China higher than those in the United States[J]. Medicine: Baltimore, 2022, 101(34): e30217. doi:10.1097/md.0000000000030217 |
| 2 | Witjes JA, Bruins HM, Cathomas R, et al. European association of urology guidelines on muscle-invasive and metastatic bladder cancer: summary of the 2020 guidelines[J]. Eur Urol, 2021, 79(1): 82-104. doi:10.1016/j.eururo.2020.03.055 |
| 3 | Tsai YS, Wu TY, Ou CH, et al. Dynamic changes of quality of life in muscle-invasive bladder cancer survivors[J]. BMC Urol, 2022, 22(1): 126. doi:10.1186/s12894-022-01084-7 |
| 4 | Ciummo SL, Sorrentino C, Fieni C, et al. Interleukin-30 subverts prostate cancer-endothelium crosstalk by fostering angiogenesis and activating immunoregulatory and oncogenic signaling pathways[J]. J Exp Clin Cancer Res, 2023, 42(1): 336. doi:10.1186/s13046-023-02902-y |
| 5 | Xie J, Zhang H, Wang K, et al. M6A-mediated-upregulation of lncRNA BLACAT3 promotes bladder cancer angiogenesis and hematogenous metastasis through YBX3 nuclear shuttling and enhancing NCF2 transcription[J]. Oncogene, 2023, 42(40): 2956-70. doi:10.1038/s41388-023-02814-3 |
| 6 | Ruan R, Li L, Li X, et al. Unleashing the potential of combining FGFR inhibitor and immune checkpoint blockade for FGF/FGFR signaling in tumor microenvironment[J]. Mol Cancer, 2023, 22(1): 60. doi:10.1186/s12943-023-01761-7 |
| 7 | Liu G, Chen T, Ding Z, et al. Inhibition of FGF-FGFR and VEGF-VEGFR signalling in cancer treatment[J]. Cell Prolif, 2021, 54(4): e13009. doi:10.1111/cpr.13009 |
| 8 | Hosni S, Kilian V, Klümper N, et al. Adipocyte precursor-derived NRG1 promotes resistance to FGFR inhibition in urothelial carcinoma[J]. Cancer Res, 2024, 84(5): 725-40. doi:10.1158/0008-5472.can-23-1398 |
| 9 | Chen JC, Shih HC, Lin CY, et al. microRNA-631 resensitizes doxorubicin-resistant chondrosarcoma cells by targeting apelin[J]. Int J Mol Sci, 2023, 24(1): 839. doi:10.3390/ijms24010839 |
| 10 | Frisch A, Kälin S, Monk R, et al. Apelin controls angiogenesis-dependent glioblastoma growth[J]. Int J Mol Sci, 2020, 21(11): E4179. doi:10.3390/ijms21114179 |
| 11 | Lv DG, Luo XL, Chen Z, et al. Apelin/APJ signaling activates autophagy to promote human lung adenocarcinoma cell migration[J]. Life Sci, 2021, 281: 119763. doi:10.1016/j.lfs.2021.119763 |
| 12 | Trang NTN, Lai CY, Tsai HC, et al. Apelin promotes osteosarcoma metastasis by upregulating PLOD2 expression via the Hippo signaling pathway and hsa_circ_0000004/miR-1303 axis[J]. Int J Biol Sci, 2023, 19(2): 412-25. doi:10.7150/ijbs.77688 |
| 13 | Hennigs JK, Cao AQ, Li CG, et al. PPARγ-p53-mediated vasculoregenerative program to reverse pulmonary hypertension[J]. Circ Res, 2021, 128(3): 401-18. doi:10.1161/circresaha.119.316339 |
| 14 | Cardoso Dos Santos LM, Azar P, Brun C, et al. Apelin is expressed in intimal smooth muscle cells and promotes their phenotypic transition[J]. Sci Rep, 2023, 13(1): 18736. doi:10.1038/s41598-023-45470-z |
| 15 | Shen J, Feng J, Wu Z, et al. Apelin prevents and alleviates crystalline silica-induced pulmonary fibrosis via inhibiting transforming growth factor beta 1-triggered fibroblast activation[J]. Int J Biol Sci, 2023, 19(13): 4004-19. doi:10.7150/ijbs.81436 |
| 16 | Jin S, Wang Y, Ma L, et al. Feedback interaction between apelin and endoplasmic reticulum stress in the rat myocardium[J]. J Cardiovasc Pharmacol, 2023, 81(1): 21-34. doi:10.1097/fjc.0000000000001369 |
| 17 | Wang YH, Wang G, Liu XJ, et al. Inhibition of APLN suppresses cell proliferation and migration and promotes cell apoptosis in esophageal cancer cells in vitro, through activating PI3K/mTOR signaling pathway[J]. Eur J Histochem, 2022, 66(3):308-15. doi:10.4081/ejh.2022.3336 |
| 18 | Chen Y, Lin X, Zheng J, et al. APLN: a potential novel biomarker for cervical cancer[J]. Sci Prog, 2021, 104(2): 368504211011341. doi:10.1177/00368504211011341 |
| 19 | Sugimoto K, Yokokawa T, Misaka T, et al. High-fat diet attenuates the improvement of hypoxia-induced pulmonary hypertension in mice during reoxygenation[J]. BMC Cardiovasc Disord, 2021, 21(1): 331. doi:10.21203/rs.3.rs-139169/v1 |
| 20 | Zhou Y, Xu R, Luo J, et al. Dysregulation of miR-204-5p/APLN axis affects malignant progression and cell stemness of esophageal cancer[J]. Mutat Res, 2022, 825: 111791. doi:10.1016/j.mrfmmm.2022.111791 |
| 21 | Wang Q, Wang BY, Zhang WJ, et al. APLN promotes the proliferation, migration, and glycolysis of cervical cancer through the PI3K/AKT/mTOR pathway[J]. Arch Biochem Biophys, 2024, 755: 109983. doi:10.1016/j.abb.2024.109983 |
| 22 | Larionova I, Kazakova E, Gerashchenko T, et al. New angiogenic regulators produced by TAMs: perspective for targeting tumor angiogenesis[J]. Cancers: Basel, 2021, 13(13): 3253. doi:10.3390/cancers13133253 |
| 23 | Anna G, Alessio N, Davide C, et al. Role of TGFβ1 and WNT6 in FGF2 and BMP4-driven endothelial differentiation of murine embryonic stem cells[J]. Angiogenesis, 2021, 25(1): 1-16. doi:10.1007/s10456-021-09815-4 |
| 24 | Huang YC, Chen WC, Yu CL, et al. FGF2 drives osteosarcoma metastasis through activating FGFR1-4 receptor pathway-mediated ICAM-1 expression[J]. Biochem Pharmacol, 2023, 218: 115853. doi:10.1016/j.bcp.2023.115853 |
| 25 | Wang Y, Sun Q, Ye Y, et al. FGF-2 signaling in nasopharyngeal carcinoma modulates pericyte-macrophage crosstalk and metastasis[J]. JCI Insight, 2022, 7(10): e157874. doi:10.1172/jci.insight.157874 |
| 26 | Zheng C, Shi CJ, Du LJ, et al. Expression of fibroblast growth factor receptor like 1 protein in oral squamous cell carcinoma and its influence on tumor cell proliferation and migration[J]. Hua Xi Kou Qiang Yi Xue Za Zhi, 2020, 38(5): 558-65. doi:10.7518/hxkq.2020.05.015 |
| 27 | Cheng C, Wang J, Xu P, et al. Gremlin1 is a therapeutically targetable FGFR1 ligand that regulates lineage plasticity and castration resistance in prostate cancer[J]. Nat Cancer, 2022, 3(5): 565-80. doi:10.1038/s43018-022-00380-3 |
| 28 | Giordano M, Decio A, Battistini C, et al. L1CAM promotes ovarian cancer stemness and tumor initiation via FGFR1/SRC/STAT3 signaling[J]. J Exp Clin Cancer Res, 2021, 40(1): 319. doi:10.1186/s13046-021-02117-z |
| 29 | Biswas PK, Kwak Y, Kim A, et al. TTYH3 modulates bladder cancer proliferation and metastasis via FGFR1/H-ras/A-raf/MEK/ERK pathway[J]. Int J Mol Sci, 2022, 23(18): 10496. doi:10.3390/ijms231810496 |
| 30 | Nian C, Gan X, Liu Q, et al. Synthesis and anti-gastric cancer activity by targeting FGFR1 pathway of novel asymmetric bis-Chalcone compounds[J]. Curr Med Chem, 2024, 31(39): 6521-41. doi:10.2174/0109298673298420240530093525 |
| [1] | Hongbo ZHANG, Mengyu YAN, Jiandong ZHANG, Peiwang SUN, Rui WANG, Yuanyuan GUO. Pirfenidone inhibits bladder cancer xenograft growth in mice by regulating regulatory T cells [J]. Journal of Southern Medical University, 2025, 45(7): 1513-1518. |
| [2] | Yanpeng PU, Zhen WANG, Haoran CHU. Eye acupuncture improves neural function in rats with cerebral ischemia-reperfusion injury by promoting angiogenesis via upregulating METTL3-mediated m6A methylation [J]. Journal of Southern Medical University, 2025, 45(5): 921-928. |
| [3] | Yutong LI, Xingyu SONG, Ruixu SUN, Xuan DONG, Hongwei LIU. A pan-cancer analysis of PYCR1 and its predictive value for chemotherapy and immunotherapy responses in bladder cancer [J]. Journal of Southern Medical University, 2025, 45(4): 880-892. |
| [4] | CHEN Shoufeng, ZHANG Shuchao, FAN Weilin, SUN Wei, LIU Beibei, LIU Jianmin, GUO Yuanyuan. Efficacy of combined treatment with pirfenidone and PD-L1 inhibitor in mice bearing ectopic bladder cancer xenograft [J]. Journal of Southern Medical University, 2024, 44(2): 210-216. |
| [5] | Liqiang LI, Yuanyuan GUO, Chengyong WANG, Rui CHANG, Wei SUN, Wuyue GAO, Chao WANG, Beibei LIU. High expression of miR-204-5p promotes malignant behaviors of bladder cancer cells by negatively regulating RAB22A [J]. Journal of Southern Medical University, 2024, 44(11): 2235-2242. |
| [6] | LUO Rui, TIAN Longhai, YANG Yongyao. Galangin inhibits oxidized low-density lipoprotein-induced angiogenic activity in human aortic endothelial cells by downregulating lncRNA H19 [J]. Journal of Southern Medical University, 2024, 44(1): 52-59. |
| [7] | YAN Qiuxia, ZENG Peng, HUANG Shuqiang, TAN Cuiyu, ZHOU Xiuqin, QIAO Jing, ZHAO Xiaoying, FENG Ling, ZHU Zhenjie, ZHANG Guozhi, HU Hong, CHEN Cairong. RBMX overexpression inhibits proliferation, migration, invasion and glycolysis of human bladder cancer cells by downregulating PKM2 [J]. Journal of Southern Medical University, 2024, 44(1): 9-16. |
| [8] | ZHANG Xiaolin, WU Haosong, WANG Sheng. SLC12A8 promotes proliferation, invasiveness, migration and epithelial-mesenchymal transition of bladder cancer cells by activating JAK/STAT singaling [J]. Journal of Southern Medical University, 2023, 43(9): 1613-1621. |
| [9] | LI Peipei, HU Yinqi, LIU Jia, WANG Lina, WU Yuanjie, HU Jianpeng. Naoluo Xintong Decoction activates caspase-1/Gasdermin D pathway to promote angiogenesis of rat brain microvascular endothelial cells after oxygen glucose deprivation/reperfusion injury [J]. Journal of Southern Medical University, 2023, 43(7): 1093-1101. |
| [10] | CAI Taonong, LU Jiangli, LIN Zhijun, LUP Mingrui, LIANG Haitao, QIN Zike, YE Yunlin. Intravesical instillation of bacillus Calmette-Guerin for non-muscle invasive bladder cancer: outcomes of 421 patients in a single center [J]. Journal of Southern Medical University, 2023, 43(3): 488-494. |
| [11] | WU Xiaofeng, ZHAN Riming, CHENG Dazhao, CHEN Li, WANG Tianyu, TANG Xudong. Exosomal FZD10 derived from non-small cell lung cancer cells promotes angiogenesis of human umbilical venous endothelial cells in vitro [J]. Journal of Southern Medical University, 2022, 42(9): 1351-1358. |
| [12] | ZOU Zhenhai, CHENG Qi, LI Zhong, GAO Wuyue, SUN Wei, LIU Beibei, GUO Yuanyuan, LIU Jianmin. microRNA let-7g-3p regulates proliferation, migration, invasion and apoptosis of bladder cancer cells by targeting HMGB2 [J]. Journal of Southern Medical University, 2022, 42(9): 1335-1343. |
| [13] | LIU Junping, SHI Yutong, WU Minmin, XU Mengqi, ZHANG Fengmei, HE Zhiqiang, TANG Min. JAG1 promotes migration, invasion, and adhesion of triple-negative breast cancer cells by promoting angiogenesis [J]. Journal of Southern Medical University, 2022, 42(7): 1100-1108. |
| [14] | FU Xiaocong, YU Guangchuang, GUO Yanfang. Expression pattern of the histone lysine demethylase family and its potential role in bladder cancer: a multi-omics analysis [J]. Journal of Southern Medical University, 2022, 42(12): 1822-1831. |
| [15] | LIN Yuan, LIU Zhimin, DONG Mengqi, ZHOU Weijie. An update of understanding of the hepatic vascular system and new research strategies [J]. Journal of Southern Medical University, 2022, 42(12): 1907-1910. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||