Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (3): 595-602.doi: 10.12122/j.issn.1673-4254.2025.03.17
Lixia YIN1,3( ), Minzhu NIU2, Keni ZHANG1,3, Zhijun GENG2, Jianguo HU1,2, Jiangyan LI1,2, Jing LI1,2(
), Minzhu NIU2, Keni ZHANG1,3, Zhijun GENG2, Jianguo HU1,2, Jiangyan LI1,2, Jing LI1,2( )
)
Received:2024-12-03
Online:2025-03-20
Published:2025-03-28
Contact:
Jing LI
E-mail:lixiayin311@163.com;sdlj13409@163.com
Supported by:Lixia YIN, Minzhu NIU, Keni ZHANG, Zhijun GENG, Jianguo HU, Jiangyan LI, Jing LI. Cimifugin ameliorates Crohn's disease-like colitis in mice by modulating Th-cell immune balance via inhibiting the MAPK pathway[J]. Journal of Southern Medical University, 2025, 45(3): 595-602.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.03.17
| Gene | Primer sequences (5'-3') |
|---|---|
| IL-17A | F:GGCCCTCAGACTACCTCAAC |
| R:TCTCGACCCTGAAAGTGAAGG | |
| IL-4 | F:CCCCAGCTAGTTGTCATCCTG |
| R:CAAGTGATTTTTGTCGCATCCG | |
| IL-10 | F:GCTGGACAACATACTGCTAACC |
| R:ATTTCCGATAAGGCTTGGCAA | |
| IFN-γ | F:ACAGCAAGGCGAAAAAGGATG |
| R:TGGTGGACCACTCGGATGA | |
| GAPDH | F:TGACCTCAACTACATGGTCTACA |
| R:CTTCCCATTCTCGGCCTTG |
Tab.1 Primer sequences for RT-qPCR
| Gene | Primer sequences (5'-3') |
|---|---|
| IL-17A | F:GGCCCTCAGACTACCTCAAC |
| R:TCTCGACCCTGAAAGTGAAGG | |
| IL-4 | F:CCCCAGCTAGTTGTCATCCTG |
| R:CAAGTGATTTTTGTCGCATCCG | |
| IL-10 | F:GCTGGACAACATACTGCTAACC |
| R:ATTTCCGATAAGGCTTGGCAA | |
| IFN-γ | F:ACAGCAAGGCGAAAAAGGATG |
| R:TGGTGGACCACTCGGATGA | |
| GAPDH | F:TGACCTCAACTACATGGTCTACA |
| R:CTTCCCATTCTCGGCCTTG |
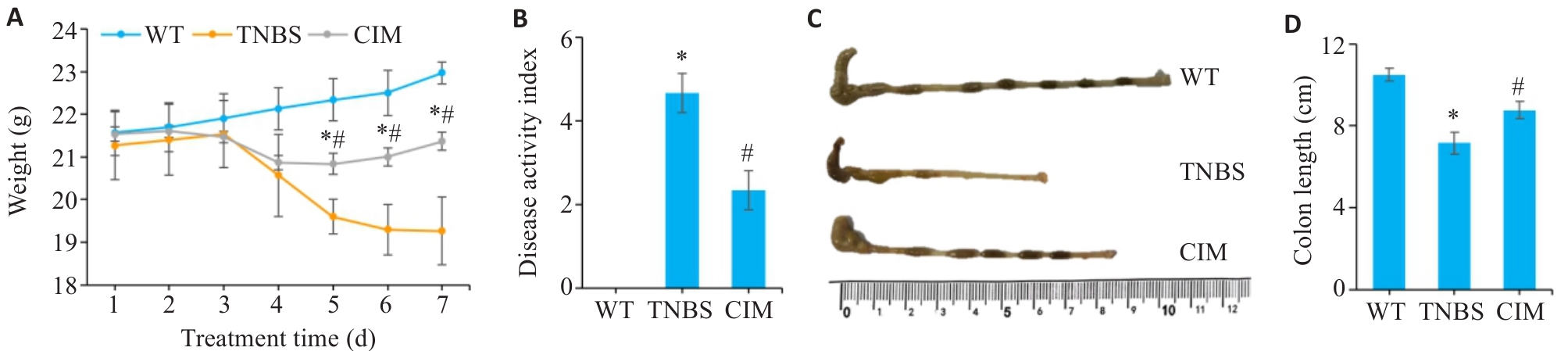
Fig.1 Effect of cimifugin (CIM) on symptoms of TNBS-induced colitis in mice. A: Daily body weight changes of the mice in each group. B: Changes in DAI scores of the mice in each group. C: Gross observation of the mouse colon in each group. D: Comparison of colonic lengths of the mice among the 3 groups. *P<0.05 vs WT; #P<0.05 vs TNBS. WT: Type; TNBS: 2,4,6-trinitrobenzenesulfonic acid.
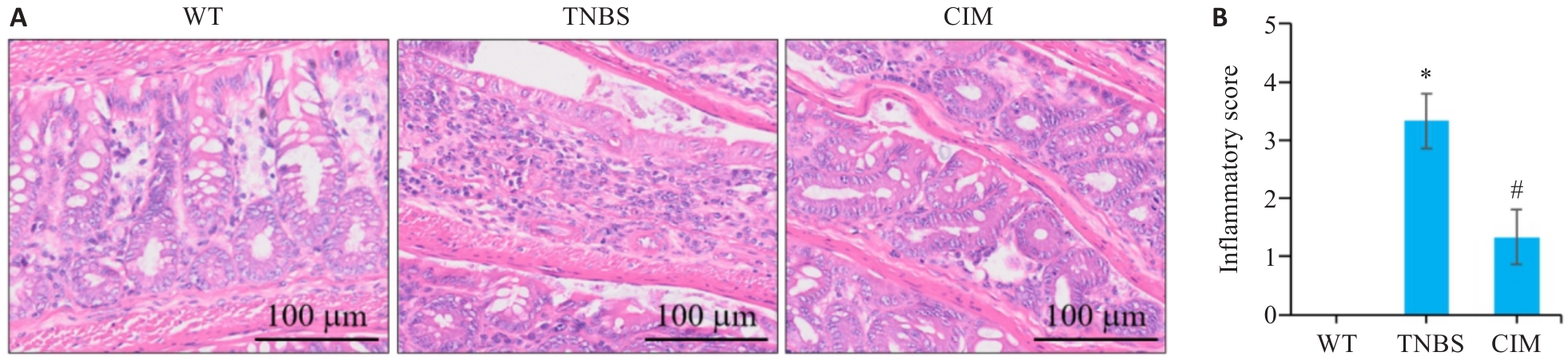
Fig.2 Effect of CIM on intestinal tissue damage in mice with TNBS-induced colitis. A: HE staining of mouse colon tissues. B: Inflammation scores of mouse colon tissue in each group. *P<0.05 vs WT; #P<0.05 vs TNBS.
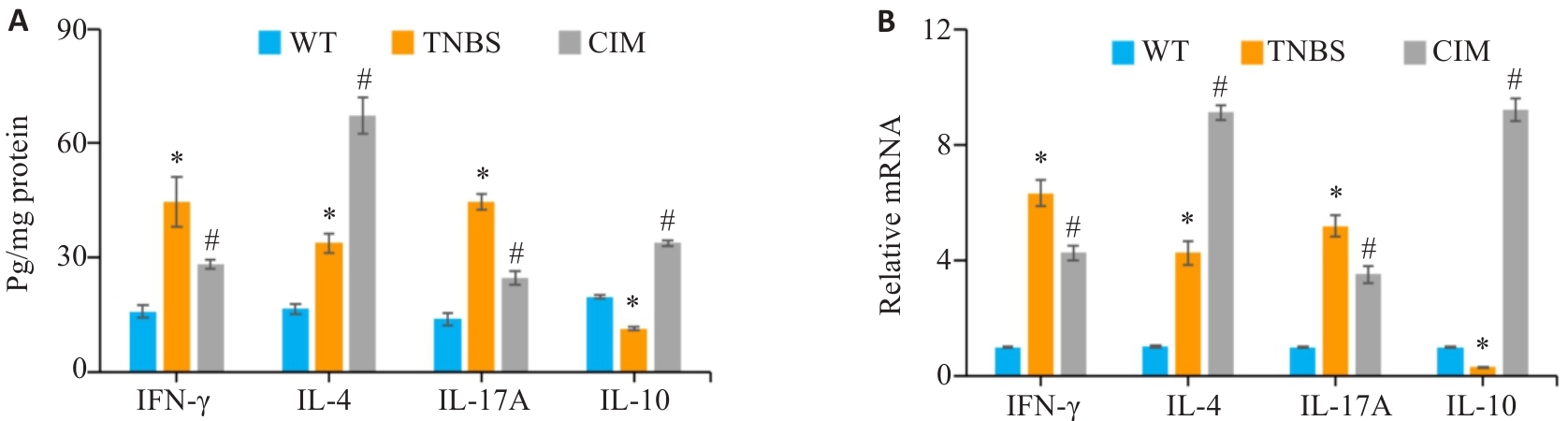
Fig.3 Effect of CIM on intestinal mucosa inflammation of the mice in each group. A: Levels of inflammatory factors in the colonic mucosa detected by ELISA. B: mRNA expressions of inflammatory factors in the colonic mucosa detected by PCR. *P<0.05 vs WT; #P<0.05 vs TNBS.
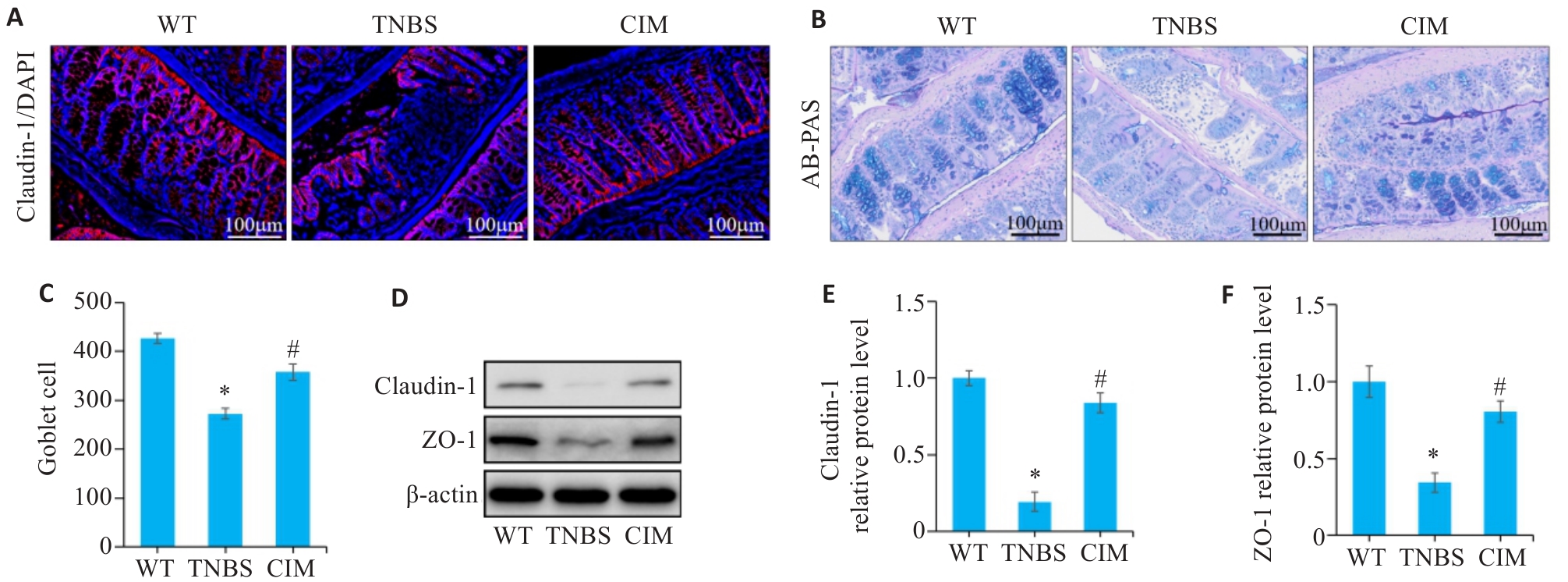
Fig.4 Effect of CIM on intestinal barrier damage in mice with TNBS-induced colitis. A: Immunofluorescence staining of claudin-1 in the colon of the mice in each group. B: AB-PAS staining of mouse colon. C: Numbers of goblet cells based on AB-PAS staining. D-F: Western blotting for detecting expression levels of ZO-1 and claudin-1 in colonic mucosal tissue. *P<0.05 vs WT; #P<0.05 vs TNBS.
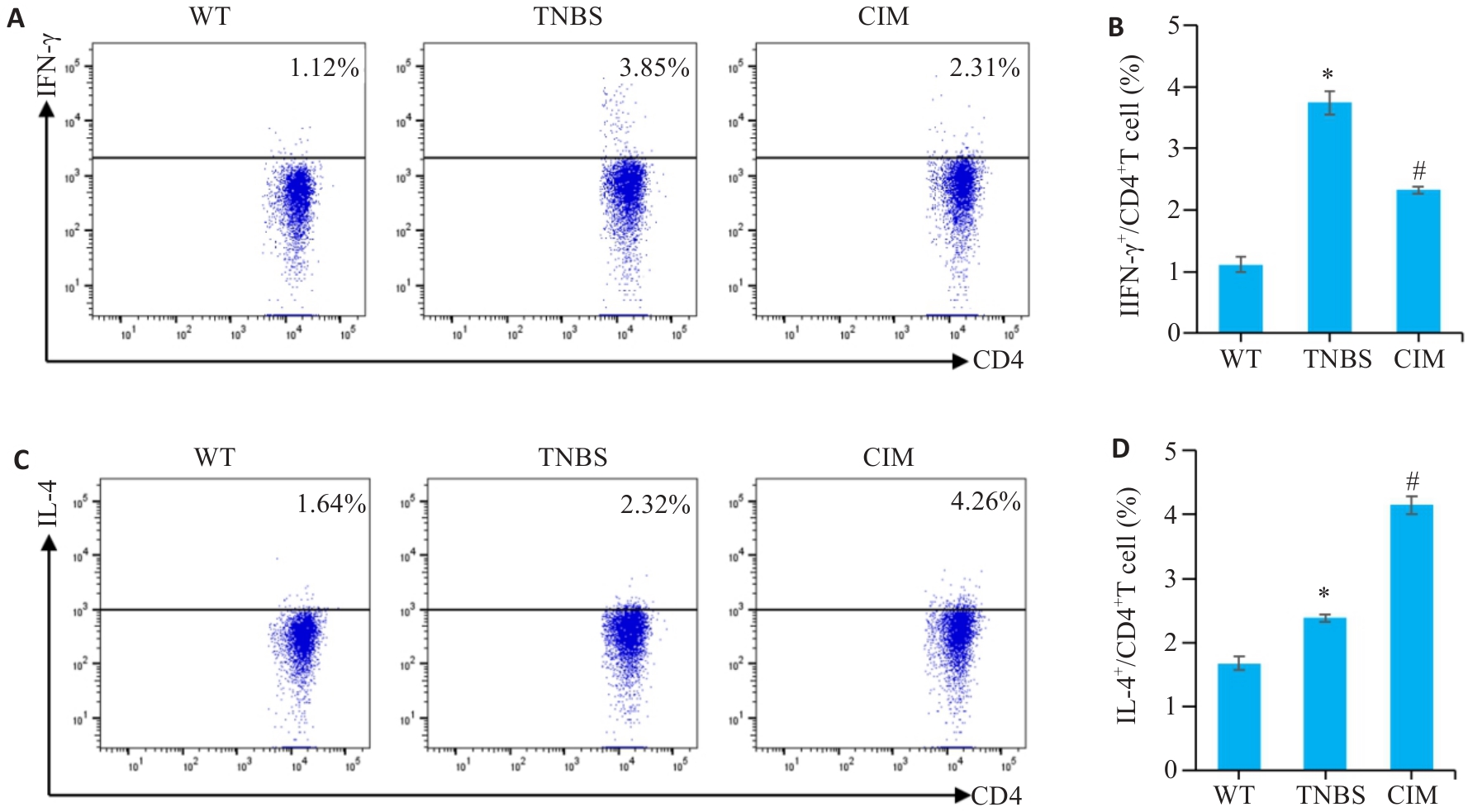
Fig.5 Effect of CIM on balance of Th1/Th2 cell response in mice with TNBS-induced colitis. A, B: Assessment of Th1 cell percentage in mouse mesenteric lymph nodes by flow cytometry. C, D: Assessment of Th2 cell percentage in mouse mesenteric lymph nodes by flow cytometry. *P<0.05 vs WT; #P<0.05 vs TNBS.
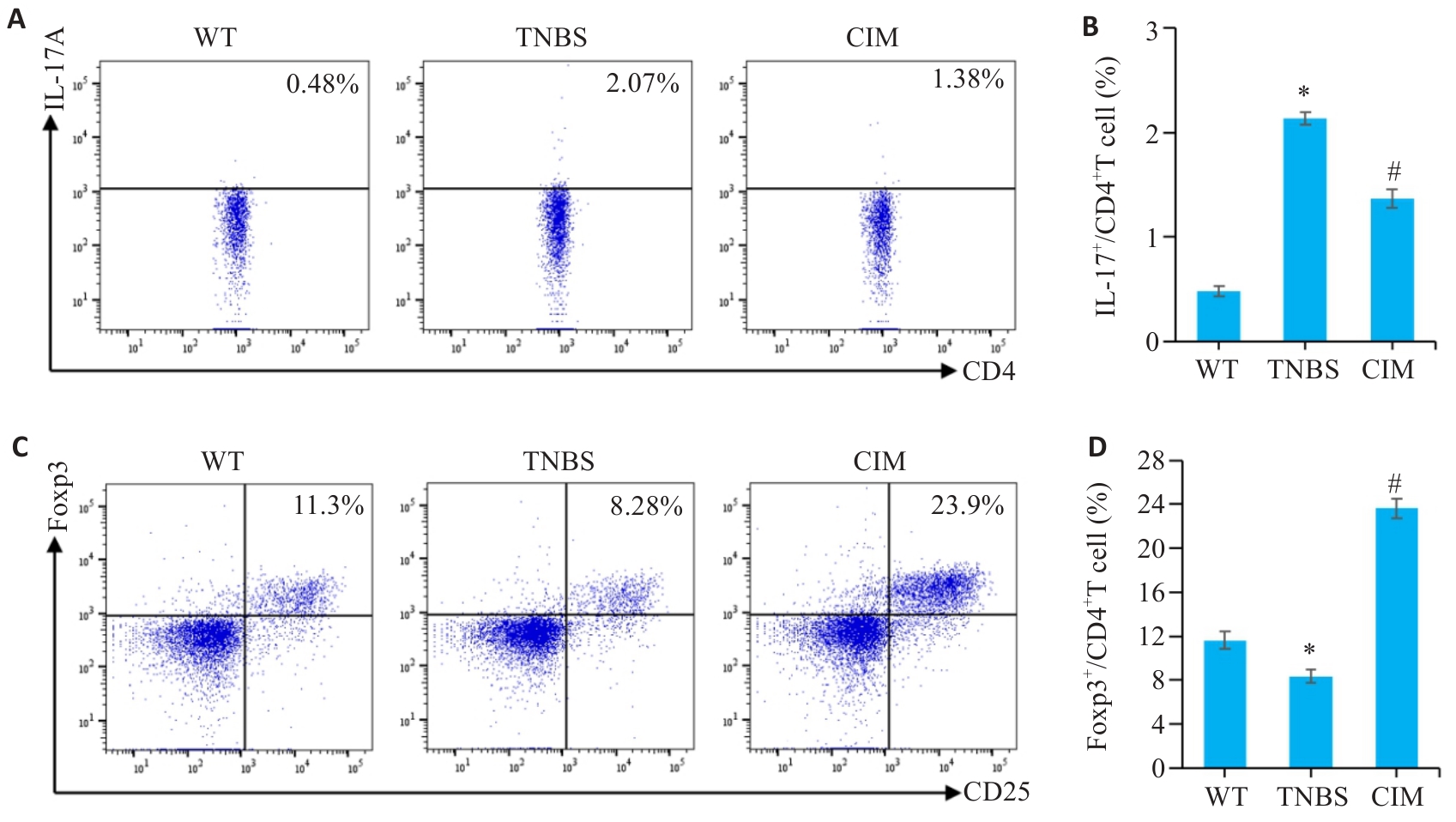
Fig.6 Effect of CIM on balance of Th17/Treg cell response in mice with TNBS-induced colitis. A, B: Assessment of Th17 cell percentage in mouse mesenteric lymph nodes by flow cytometry. C, D: Assessment of Treg cell percentage in mouse mesenteric lymph nodes by flow cytometry. *P<0.05 vs WT; #P<0.05 vs TNBS.
| Compound | Target | PDB | Energy (kcal/mol) |
|---|---|---|---|
| CIM | MAP3K14 | 8YHW | -8.4 |
| CIM | MAP2K1 | 3EQI | -8.3 |
| CIM | MAPK14 | 6SFO | -8.2 |
| CIM | MAPK1 | 6SLG | -7.6 |
| CIM | IKBKB | 4KIK | -7.5 |
| CIM | BRAF | 5VYK | -6.7 |
| CIM | CASP3 | 1RE1 | -6.5 |
| CIM | JUN | 6Y3V | -5.7 |
Tab.2 Molecular docking results
| Compound | Target | PDB | Energy (kcal/mol) |
|---|---|---|---|
| CIM | MAP3K14 | 8YHW | -8.4 |
| CIM | MAP2K1 | 3EQI | -8.3 |
| CIM | MAPK14 | 6SFO | -8.2 |
| CIM | MAPK1 | 6SLG | -7.6 |
| CIM | IKBKB | 4KIK | -7.5 |
| CIM | BRAF | 5VYK | -6.7 |
| CIM | CASP3 | 1RE1 | -6.5 |
| CIM | JUN | 6Y3V | -5.7 |
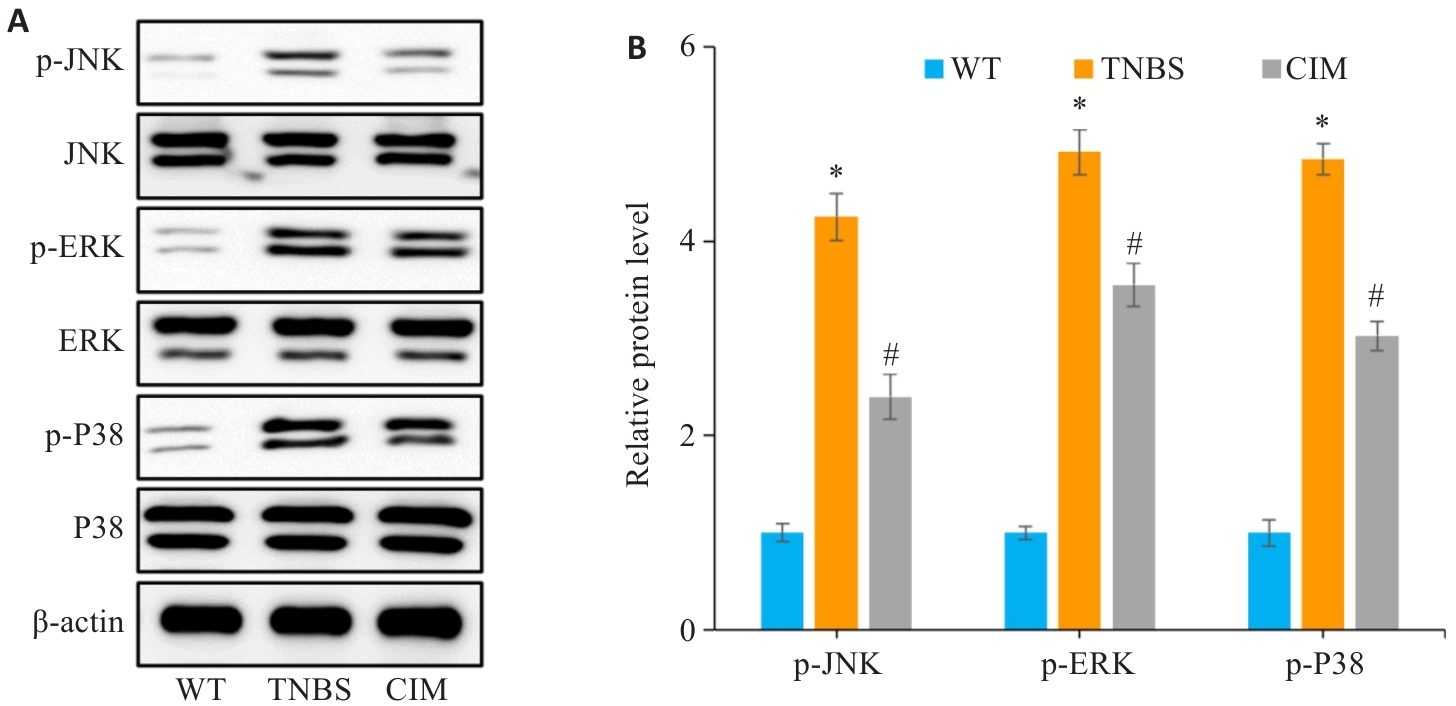
Fig.8 Verification of the role of the MAPK signaling pathway in mediating the therapeutic effect of CIM on TNBS-induced colitis in mice. A, B: Expressions of key proteins of the MAPK pathway (p-p38, p-ERK and p-JNK) detected in the intestinal mucosal tissues of the mice by Western blotting. *P<0.05 vs WT; #P<0.05 vs TNBS.
| 1 | Liang WJ, Zhang W, Tian JY, et al. Advances in carbohydrate-based nanoparticles for targeted therapy of inflammatory bowel diseases: a review[J]. Int J Biol Macromol, 2024, 281: 136392. |
| 2 | Peyrin-Biroulet L, Ghosh S, Lee SD, et al. Effect of risankizumab on health-related quality of life in patients with Crohn's disease: results from phase 3 MOTIVATE, ADVANCE and FORTIFY clinical trials[J]. Aliment Pharmacol Ther, 2023, 57(5): 496-508. |
| 3 | Chen RR, Li C, Zheng JQ, et al. Lymphocyte subsets for predicting inflammatory bowel disease progression and treatment response: a systematic review[J]. Front Immunol, 2024, 15: 1403420. |
| 4 | Leibovitzh H, Lee SH, Garay JAR, et al. Immune response and barrier dysfunction-related proteomic signatures in preclinical phase of Crohn's disease highlight earliest events of pathogenesis[J]. Gut, 2023, 72(8): 1462-71. |
| 5 | Chang JT. Pathophysiology of inflammatory bowel diseases[J]. N Engl J Med, 2020, 383(27): 2652-64. |
| 6 | Duan SH, Cao YB, Chen PR, et al. Circulating and intestinal regulatory T cells in inflammatory bowel disease: a systemic review and meta-analysis[J]. Int Rev Immunol, 2024, 43(2): 83-94. |
| 7 | Rivera Rodríguez R, Johnson JJ. Terpenes: Modulating anti-inflammatory signaling in inflammatory bowel disease[J]. Pharmacol Ther, 2023, 248: 108456. |
| 8 | Wei XN, Leng XH, Liang JW, et al. Pharmacological potential of natural medicine Astragali Radix in treating intestinal diseases[J]. Biomed Pharmacother, 2024, 180: 117580. |
| 9 | Zhu N, Zhu LY, Zhang XL, et al. Triptolide attenuates irritable bowel syndrome via inhibiting ODC1[J]. BMC Gastroenterol, 2023, 23(1): 202. |
| 10 | 李晴晴, 黄 菊, 孙 洋, 等. 乙酰紫堇灵通过抑制肠上皮细胞凋亡改善三硝基苯磺酸诱导的小鼠克罗恩病样结肠炎[J]. 南方医科大学学报, 2023, 43(8): 1306-14. |
| 11 | 杨 子, 赵天豪, 程 阳, 等. 香叶木素通过调节小鼠的肠道免疫平衡减轻克罗恩病样结肠炎: 基于抑制PI3K/AKT通路[J]. 南方医科大学学报, 2023, 43(3): 474-82. |
| 12 | Duan J, Hu XT, Li T, et al. Cimifugin suppresses NF-κB signaling to prevent osteoclastogenesis and periprosthetic osteolysis[J]. Front Pharmacol, 2021, 12: 724256. |
| 13 | Zhang H, Xiong ZK, He YS, et al. Cimifugin improves intestinal barrier dysfunction by upregulating SIRT1 to regulate the NRF2/HO-1 signaling pathway[J]. Naunyn Schmiedebergs Arch Pharmacol, 2024. |
| 14 | Huang CY, Tan HS, Song MY, et al. Maternal Western diet mediates susceptibility of offspring to Crohn's-like colitis by deoxycholate generation[J]. Microbiome, 2023, 11(1): 96. |
| 15 | Li CL, Liu MG, Deng L, et al. Oxyberberine ameliorates TNBS-induced colitis in rats through suppressing inflammation and oxidative stress via Keap1/Nrf2/NF‑κB signaling pathways[J]. Phytomedicine, 2023, 116: 154899. |
| 16 | Gu XQ, Chen YY, Qian PY, et al. Cimifugin suppresses type 2 airway inflammation by binding to SPR and regulating its protein expression in a non-enzymatic manner[J]. Phytomedicine, 2023, 111: 154657. |
| 17 | Huang LY, Qian WW, Xu YH, et al. Mesenteric adipose tissue contributes to intestinal fibrosis in Crohn's disease through the ATX-LPA axis[J]. J Crohns Colitis, 2022, 16(7): 1124-39. |
| 18 | 韩康宁, 胡俊杰, 李 娟, 等. 二妙四土汤调控JAK/STAT通路治疗湿热型湿疹大鼠的药效与作用机制探讨[J]. 中国实验方剂学杂志, 2024,[Epub ahead of print]. |
| 19 | Li XW, Di QQ, Li XL, et al. Kumujan B suppresses TNF-α-induced inflammatory response and alleviates experimental colitis in mice[J]. Front Pharmacol, 2024, 15: 1427340. |
| 20 | Liu AM, Zhao W, Zhang BX, et al. Cimifugin ameliorates imiquimod-induced psoriasis by inhibiting oxidative stress and inflammation via NF-κB/MAPK pathway[J]. Biosci Rep, 2020, 40(6): BSR20200471. |
| 21 | Han B, Dai Y, Wu HY, et al. Cimifugin inhibits inflammatory responses of RAW264.7 cells induced by lipopolysaccharide[J]. Med Sci Monit, 2019, 25: 409-17. |
| 22 | Xiang ZJ, Zhang BB, Cao SY, et al. SPH7854, a gut-limited RORγt antagonist, ameliorates TNBS-induced experimental colitis in rat[J]. Int Immunopharmacol, 2024, 140: 112884. |
| 23 | Chen GX, Ran X, Li B, et al. Sodium butyrate inhibits inflammation and maintains epithelium barrier integrity in a TNBS-induced inflammatory bowel disease mice model[J]. EBioMedicine, 2018, 30: 317-25. |
| 24 | 李前昆, 宾东华, 尹园缘, 等. 参苓白术散对克罗恩病大鼠炎症因子IL-1β、IL-1、IL-17C、IL-10及IL-4的影响[J]. 湖南中医药大学学报, 2023, 43(8): 1361-7. |
| 25 | Zhou Y, Xiong XY, Cheng Z, et al. Ginsenoside Rb1 alleviates DSS-induced ulcerative colitis by protecting the intestinal barrier through the signal network of VDR, PPARγ and NF-κB[J]. Drug Des Devel Ther, 2024, 18: 4825-38. |
| 26 | Zhou LY, Zhu LG, Wu XM, et al. Decreased TMIGD1 aggravates colitis and intestinal barrier dysfunction via the BANF1-NF‑κB pathway in Crohn’s disease[J]. BMC Med, 2023, 21(1): 287. |
| 27 | Hou QH, Huang JX, Ayansola H, et al. Intestinal stem cells and immune cell relationships: potential therapeutic targets for inflammatory bowel diseases[J]. Front Immunol, 2021, 11: 623691. |
| 28 | Naama M, Telpaz S, Awad A, et al. Autophagy controls mucus secretion from intestinal goblet cells by alleviating ER stress[J]. Cell Host Microbe, 2023, 31(3): 433-46. e4. |
| 29 | Gustafsson JK, Johansson MEV. The role of goblet cells and mucus in intestinal homeostasis[J]. Nat Rev Gastroenterol Hepatol, 2022, 19(12): 785-803. |
| 30 | Clough JN, Omer OS, Tasker S, et al. Regulatory T-cell therapy in Crohn's disease: challenges and advances[J]. Gut, 2020, 69(5): 942-52. |
| 31 | Zeng F, Shi YH, Wu CN, et al. A drug-free nanozyme for mitigating oxidative stress and inflammatory bowel disease[J]. J Nanobio-technology, 2022, 20(1): 107. |
| 32 | Kosinsky RL, Gonzalez MM, Saul D, et al. The FOXP3+ pro-inflammatory T cell: a potential therapeutic target in Crohn's disease[J]. Gastroenterology, 2024, 166(4): 631-44. e17. |
| 33 | Feng YJ, Li YY. The role of p38 mitogen-activated protein kinase in the pathogenesis of inflammatory bowel disease[J]. J Dig Dis, 2011, 12(5): 327-32. |
| 34 | Li JH, Jia JH, Teng Y, et al. Gastrodin alleviates DSS-induced colitis in mice through strengthening intestinal barrier and modulating gut microbiota[J]. Foods, 2024, 13(15): 2460. |
| 35 | Broom OJ, Widjaya B, Troelsen J, et al. Mitogen activated protein kinases: a role in inflammatory bowel disease[J]? Clin Exp Immunol, 2009, 158(3): 272-80. |
| 36 | Liu ML, Ding JH, Zhang HM, et al. Lactobacillus casei LH23 modulates the immune response and ameliorates DSS-induced colitis via suppressing JNK/p-38 signal pathways and enhancing histone H3K9 acetylation[J]. Food Funct, 2020, 11(6): 5473-85. |
| [1] | Xiupeng LONG, Shun TAO, Shen YANG, Suyun LI, Libing RAO, Li LI, Zhe ZHANG. Quercetin improves heart failure by inhibiting cardiomyocyte apoptosis via suppressing the MAPK signaling pathway [J]. Journal of Southern Medical University, 2025, 45(1): 187-196. |
| [2] | Shuo LIU, Jing LI, Xingwang WU. Swertiamarin ameliorates 2,4,6-trinitrobenzenesulfonic acid-induced colitis in mice by inhibiting intestinal epithelial cell apoptosis [J]. Journal of Southern Medical University, 2024, 44(8): 1545-1552. |
| [3] | Nan WANG, Bin SHI, Xiaolan MAN, Weichao WU, Jia CAO. High expression of fragile X mental retardation protein inhibits ferroptosis of colorectal tumor cells by activating the RAS/MAPK signaling pathway [J]. Journal of Southern Medical University, 2024, 44(5): 885-893. |
| [4] | RONG Shengwei, LI Hongfang, WEI Yiran, FENG Zihang, GAN Lu, DENG Zhonghao, ZHAO Liang. Zinc finger protein-36 deficiency inhibits osteogenic differentiation of mouse bone marrow-derived mesenchymal stem cells and preosteoblasts by activating the ERK/MAPK pathway [J]. Journal of Southern Medical University, 2024, 44(4): 697-705. |
| [5] | Minzhu NIU, Lixia YIN, Ting DUAN, Ju HUANG, Jing LI, Zhijun GENG, Jianguo HU, Chuanwang SONG. Asperosaponin VI alleviates TNBS-induced Crohn's disease-like colitis in mice by reducing intestinal epithelial cell apoptosis via inhibiting the PI3K/AKT/NF-κB signaling pathway [J]. Journal of Southern Medical University, 2024, 44(12): 2335-2346. |
| [6] | LIU Tongjia, WANG Wanlun, ZHANG Ting, LIU Shuang, BIAN Yanchao, ZHANG Chuanling, XIAO Rui. Expression of TUBB4B in mouse primary spermatocyte GC-2 cells and its regulatory effect on NF-κB and MAPK signaling pathway [J]. Journal of Southern Medical University, 2023, 43(6): 1002-1009. |
| [7] | SHAO Rongrong, YANG Zi, ZHANG Wenjing, ZHANG Nuo, ZHAO Yajing, ZHANG Xiaofeng, ZUO Lugen, GE Sitang. Pachymic acid protects against Crohn's disease-like intestinal barrier injury and colitis in mice by suppressing intestinal epithelial cell apoptosisviainhibiting PI3K/AKT signaling [J]. Journal of Southern Medical University, 2023, 43(6): 935-942. |
| [8] | ZHOU Hui, ZHANG Yuqing, GAN Chao, FAN Xirui, QI Zhilin, QI Shimei. Eriocitrin suppresses proliferation and migration of hepatocellular carcinoma SMMC-7721 cells by promoting ROS production and activating the MAPK pathway [J]. Journal of Southern Medical University, 2023, 43(3): 412-419. |
| [9] | ZENG Xindian, CHEN Li, ZHOU Peng, TANG Ting, CHEN Xi, HU Dan, WANG Chuan, CHEN Lili. Type III secretory protein SINC of Chlamydia psittaci promotes host cell autophagy by activating the MAPK/ERK signaling pathway [J]. Journal of Southern Medical University, 2023, 43(2): 294-299. |
| [10] | LIU Zhenglu, XUAN Chengrui, HAN Xiran, ZHENG Zeze, XIAO Ru, BAO Luri, XU Xiaoyan. LASS2/TMSG1 overexpression inhibits proliferation and promotes apoptosis of human lung cancer A549 cells possibly by upregulating ceramide and p38 MAPK to activate a signaling cascade [J]. Journal of Southern Medical University, 2023, 43(2): 166-174. |
| [11] | ZHANG Jiafa, YANG Canhong, ZHANG Shufen, CAO Tingting, PENG Rui, GUO Weihong, YAN Yuping, XIE Shuting, PENG Xiaojia, LÜ Tianming, HUANG Tianrong. Sulforaphane reverses Aβ fiber-mediated M1 type microglia polarization and neuroinflammation-mediated necroptosis of neural stem cells by downregulating the MAPK/NF-κB signaling pathways [J]. Journal of Southern Medical University, 2023, 43(12): 2132-2138. |
| [12] | CAO Jing, LIU Haibo, AN Qi, HAN Feng. Metformin alleviates pathologic pain in mice with radiation dermatitis by inhibiting p38MAPK/NF-κB signaling pathway [J]. Journal of Southern Medical University, 2023, 43(10): 1815-1820. |
| [13] | KANG Huiwen, JIANG Shoufang, SONG Qian, ZHANG Yili. Activation of cannabinoid receptor 2 alleviates acute lung injury in rats with lipopolysaccharide-induced sepsis [J]. Journal of Southern Medical University, 2022, 42(9): 1374-1380. |
| [14] | FANG Shangping, YUAN Ran, SUN Renke, MA Tongjun. Knockout of S1PR3 attenuates acute lung injury in mice by inhibiting the MAPK pathway [J]. Journal of Southern Medical University, 2022, 42(12): 1815-1821. |
| [15] | . Changes of guanylate cyclase C in colon tissues of rats with intestinal injury associated with severe acute pancreatitis [J]. Journal of Southern Medical University, 2021, 41(3): 376-383. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||