Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (10): 2171-2181.doi: 10.12122/j.issn.1673-4254.2025.10.13
Ying DENG( ), Minyi ZHANG, Shiao WANG, Shunchang FAN, Jiaqi CHEN, Juxian XIAN, Qing CHEN(
), Minyi ZHANG, Shiao WANG, Shunchang FAN, Jiaqi CHEN, Juxian XIAN, Qing CHEN( )
)
Received:2025-07-04
Online:2025-10-20
Published:2025-10-24
Contact:
Qing CHEN
E-mail:rebeccatung@163.com;qch2009@163.com
Supported by:Ying DENG, Minyi ZHANG, Shiao WANG, Shunchang FAN, Jiaqi CHEN, Juxian XIAN, Qing CHEN. Global burden and predicted trends of diarrheal disease in children under five from 1990 to 2021[J]. Journal of Southern Medical University, 2025, 45(10): 2171-2181.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.10.13
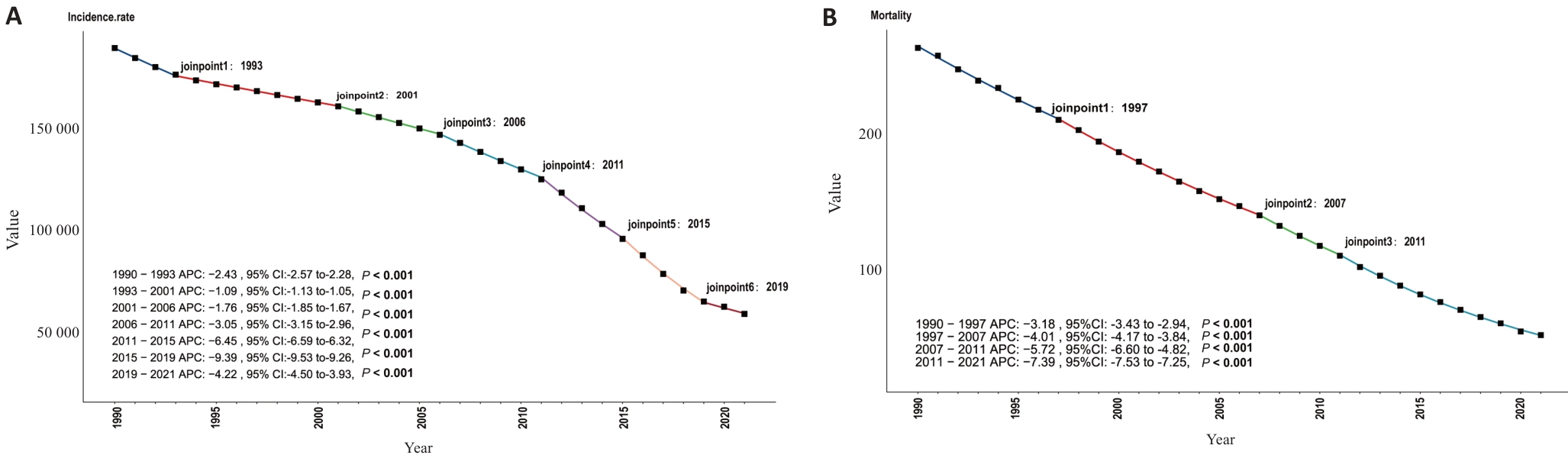
Fig.1 Joinpoint regression analysis of the incidence (A) and mortality (B) rates of diarrheal diseases in Children under 5 globally from 1990 to 2021. AAPC: Average annual percentage change. The joinpoints are labeled, and the corresponding annual percent change (APC) and P values (P<0.001 indicates a statistically significant difference) are shown in the legend. Different colors represent different segments.
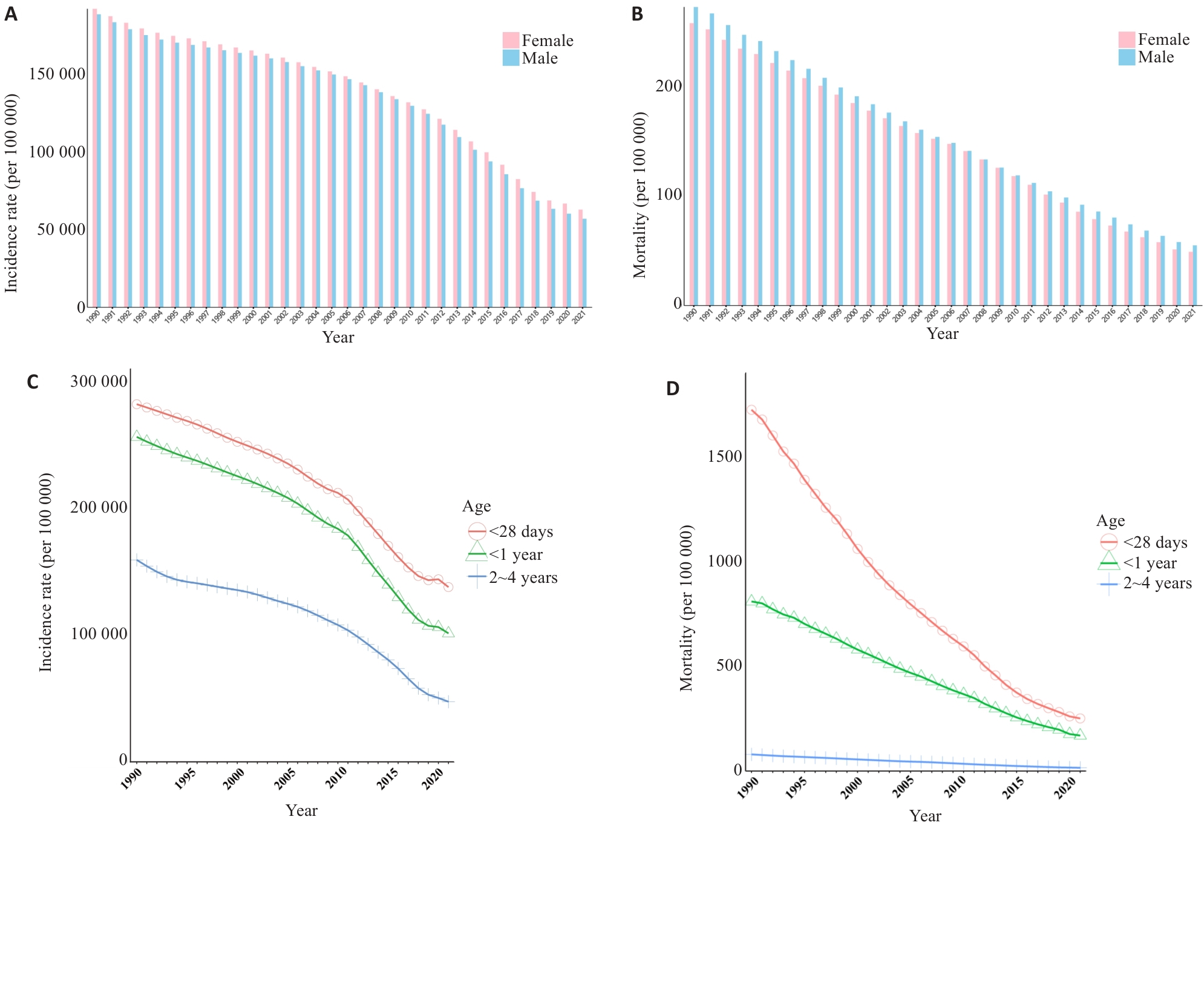
Fig.2 Gender and age-specific burden of diarrheal diseases among children under 5 years globally in 1990-2021 (per 100 000). A, B: Bar charts showing the incidence rate and mortality rate of diarrheal diseases among children under 5 years stratified by sex from 1990 to 2021. C, D: Line charts showing the incidence rate and mortality rate of diarrheal diseases among children under 5 years stratified by age, from 1990 to 2021.
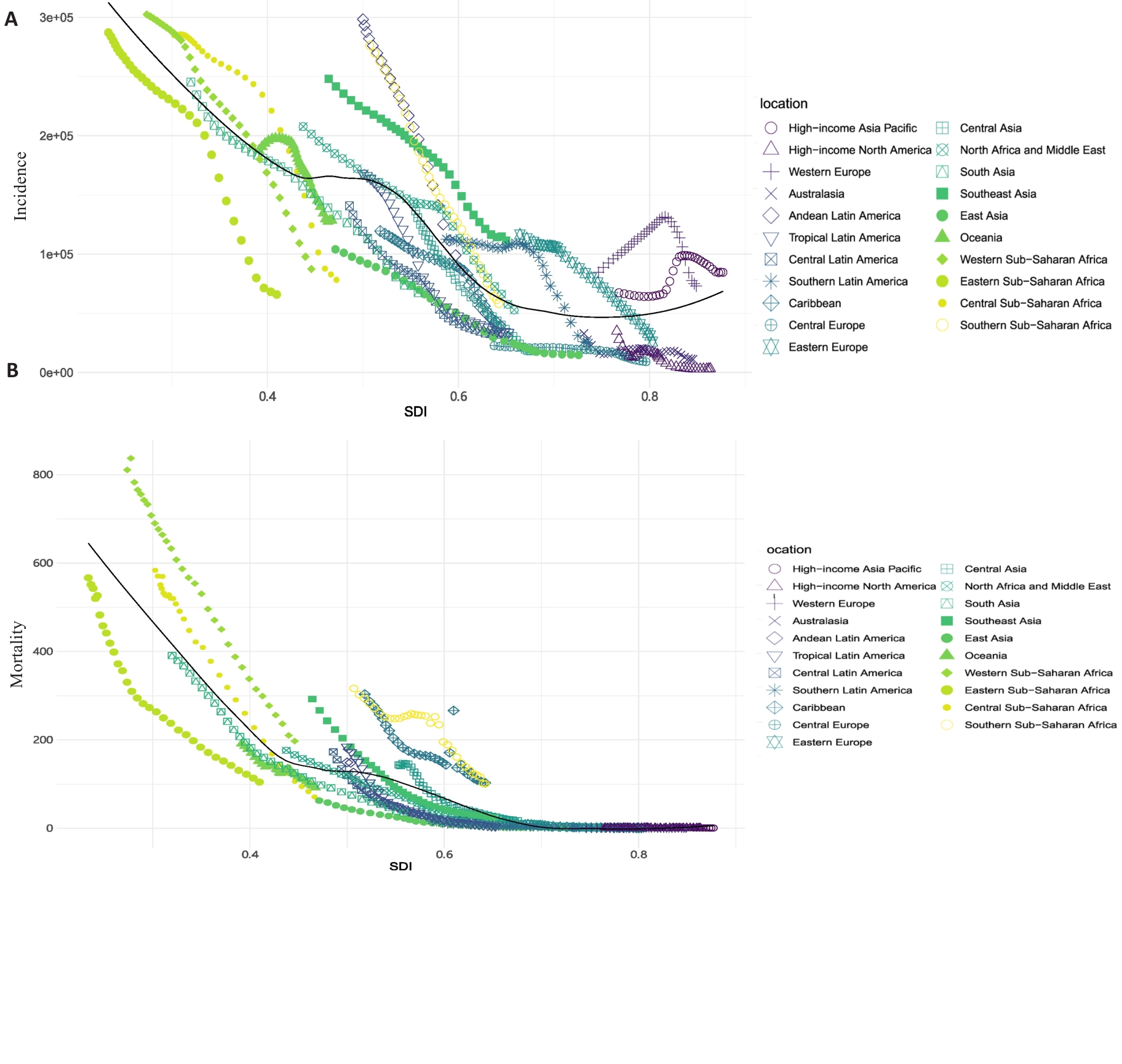
Fig.3 Incidence and mortality rates (per 100 000) of diarrheal diseases among children under 5 in 21 GBD regions in 2021 and the trends and their correlation with the socio-demographic index (SDI) across GBD regions worldwide from 1990 to 2021. A: Trends of the incidence rates and SDI. B: Trends of the mortality rates and SDI by GBD regions. The black line represents the expected rate based solely on SDI.
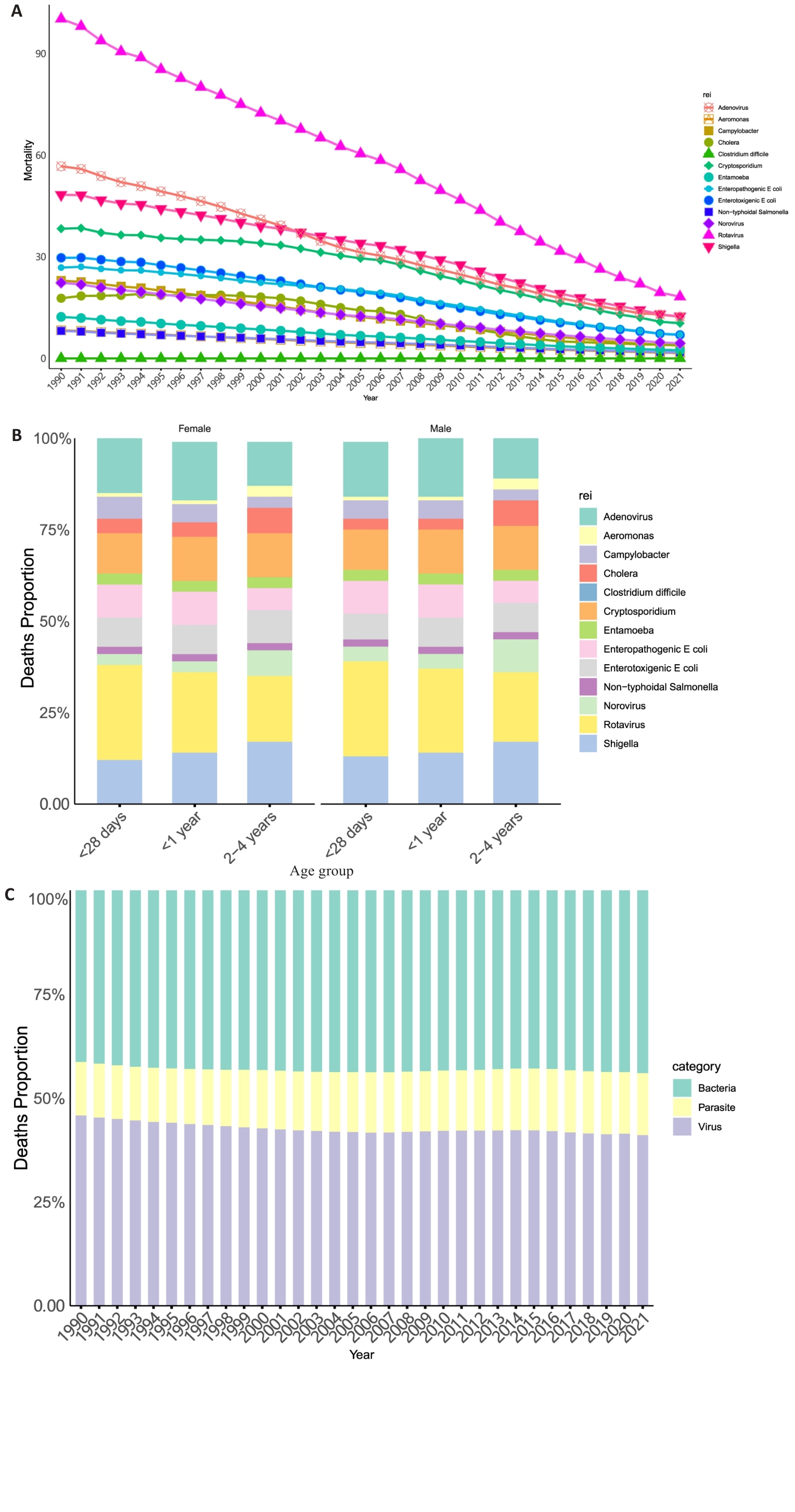
Fig.4 Mortality rates of diarrheal diseases caused by different pathogens among children under 5 years globally in 1990-2021 (per 100 000). A: Trends in diarrhoeal mortality rate by pathogen in children under 5 regionally in 1990-2021. B: Pathogen attributed death proportion of diarrhea in children of different age groups in 1990 to 2021. C: Distribution of diarrhoeal mortality by pathogen in children under 5 globally from 1990 to 2021.
| Global | Mortality rate, 1990 (per 100 000) | Mortality rate, 2021 (per 100 000) | AAPC, 1990-2021 (95% CI) |
|---|---|---|---|
| Adenovirus | 56.78 (32.70 to 90.28) | 12.32 (6.82 to 20.21) | -4.82 (-4.99 to -4.65) |
| Aeromonas | 8.31 (3.62 to 15.15) | 1.63 (0.73 to 3.07) | -5.17 (-5.27 to -5.07) |
| Campylobacter | 22.98 (10.17 to 42.40) | 3.84 (1.56 to 7.41) | -5.63 (-5.77 to -5.49) |
| Cholera | 17.76 (14.75 to 21.43) | 3.92 (2.81 to 5.31) | -4.83 (-5.12 to -4.53) |
| Clostridium difficile | 0.02 (0.01 to 0.03) | 0.02 (0.01 to 0.03) | -0.01 (-0.22 to 0.19) |
| Cryptosporidium | 38.32 (23.65 to 59.95) | 10.4 (5.91 to 16.65) | -4.2 (-4.34 to -4.07) |
| Enterotoxigenic E coli | 29.72 (17.32 to 47.09) | 6.96 (3.83 to 11.72) | -4.62 (-4.73 to -4.52) |
| Enteropathogenic E coli | 26.83 (15.46 to 42.14) | 7.04 (3.95 to 11.59) | -4.31 (-4.39 to -4.23) |
| Entamoeba | 12.28 (5.88 to 23.03) | 2.44 (1.07 to 4.91) | -5.11 (-5.28 to -4.95) |
| Non-typhoidal salmonella | 8.16 (1.20 to 17.77) | 1.8 (0.24 to 4.17) | -4.8 (-5.12 to -4.48) |
| Norovirus | 22.35 (7.64 to 40.06) | 4.49 (1.47 to 8.36) | -5.09 (-5.24 to -4.94) |
| Rotavirus | 100.31 (74.21 to 127.24) | 18.21 (12.63 to 25.74) | -5.41 (-5.51 to -5.31) |
| Shigella | 48.35 (29.24 to 78.08) | 12.42 (7.28 to 20.96) | -4.34 (-4.51 to -4.18) |
Tab.2 Mortality rate and average annual percentage changes (AAPC) of diarrheal disease in children under 5 years stratified by different pathogens worldwide
| Global | Mortality rate, 1990 (per 100 000) | Mortality rate, 2021 (per 100 000) | AAPC, 1990-2021 (95% CI) |
|---|---|---|---|
| Adenovirus | 56.78 (32.70 to 90.28) | 12.32 (6.82 to 20.21) | -4.82 (-4.99 to -4.65) |
| Aeromonas | 8.31 (3.62 to 15.15) | 1.63 (0.73 to 3.07) | -5.17 (-5.27 to -5.07) |
| Campylobacter | 22.98 (10.17 to 42.40) | 3.84 (1.56 to 7.41) | -5.63 (-5.77 to -5.49) |
| Cholera | 17.76 (14.75 to 21.43) | 3.92 (2.81 to 5.31) | -4.83 (-5.12 to -4.53) |
| Clostridium difficile | 0.02 (0.01 to 0.03) | 0.02 (0.01 to 0.03) | -0.01 (-0.22 to 0.19) |
| Cryptosporidium | 38.32 (23.65 to 59.95) | 10.4 (5.91 to 16.65) | -4.2 (-4.34 to -4.07) |
| Enterotoxigenic E coli | 29.72 (17.32 to 47.09) | 6.96 (3.83 to 11.72) | -4.62 (-4.73 to -4.52) |
| Enteropathogenic E coli | 26.83 (15.46 to 42.14) | 7.04 (3.95 to 11.59) | -4.31 (-4.39 to -4.23) |
| Entamoeba | 12.28 (5.88 to 23.03) | 2.44 (1.07 to 4.91) | -5.11 (-5.28 to -4.95) |
| Non-typhoidal salmonella | 8.16 (1.20 to 17.77) | 1.8 (0.24 to 4.17) | -4.8 (-5.12 to -4.48) |
| Norovirus | 22.35 (7.64 to 40.06) | 4.49 (1.47 to 8.36) | -5.09 (-5.24 to -4.94) |
| Rotavirus | 100.31 (74.21 to 127.24) | 18.21 (12.63 to 25.74) | -5.41 (-5.51 to -5.31) |
| Shigella | 48.35 (29.24 to 78.08) | 12.42 (7.28 to 20.96) | -4.34 (-4.51 to -4.18) |
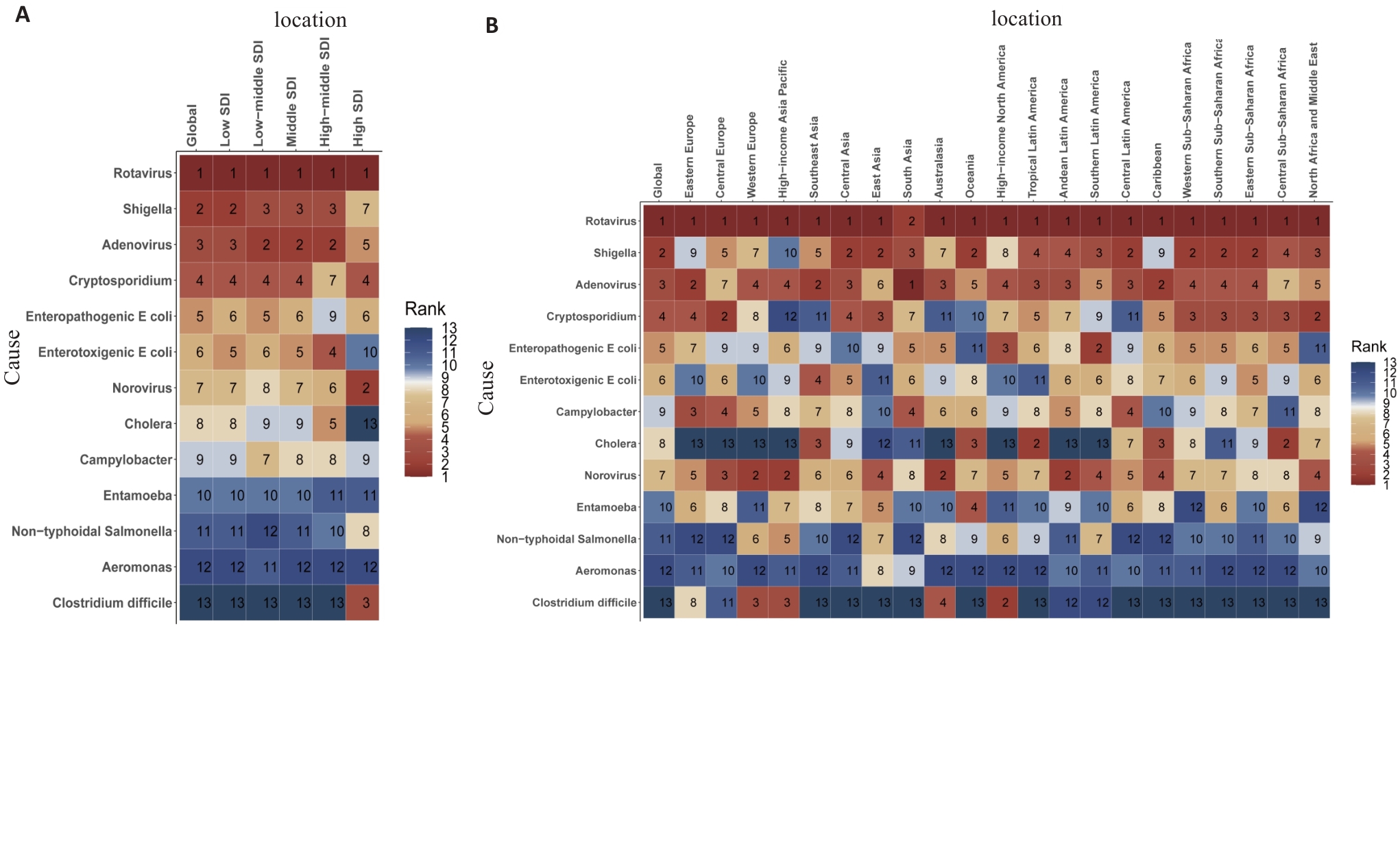
Fig.5 Causes of diarrheal deaths in children under 5 across GBD regions in 2021. A: Etiology of diarrheal deaths ranked by mortality rate globally (by SDI in 2021). B: Etiology of diarrheal deaths ranked by mortality rate globally (by GBD regions in 2021). The numbers represent the rank of diarrheal mortality rates among children under 5 for the corresponding GBD regions and pathogen. A smaller number indicates a higher mortality rate.
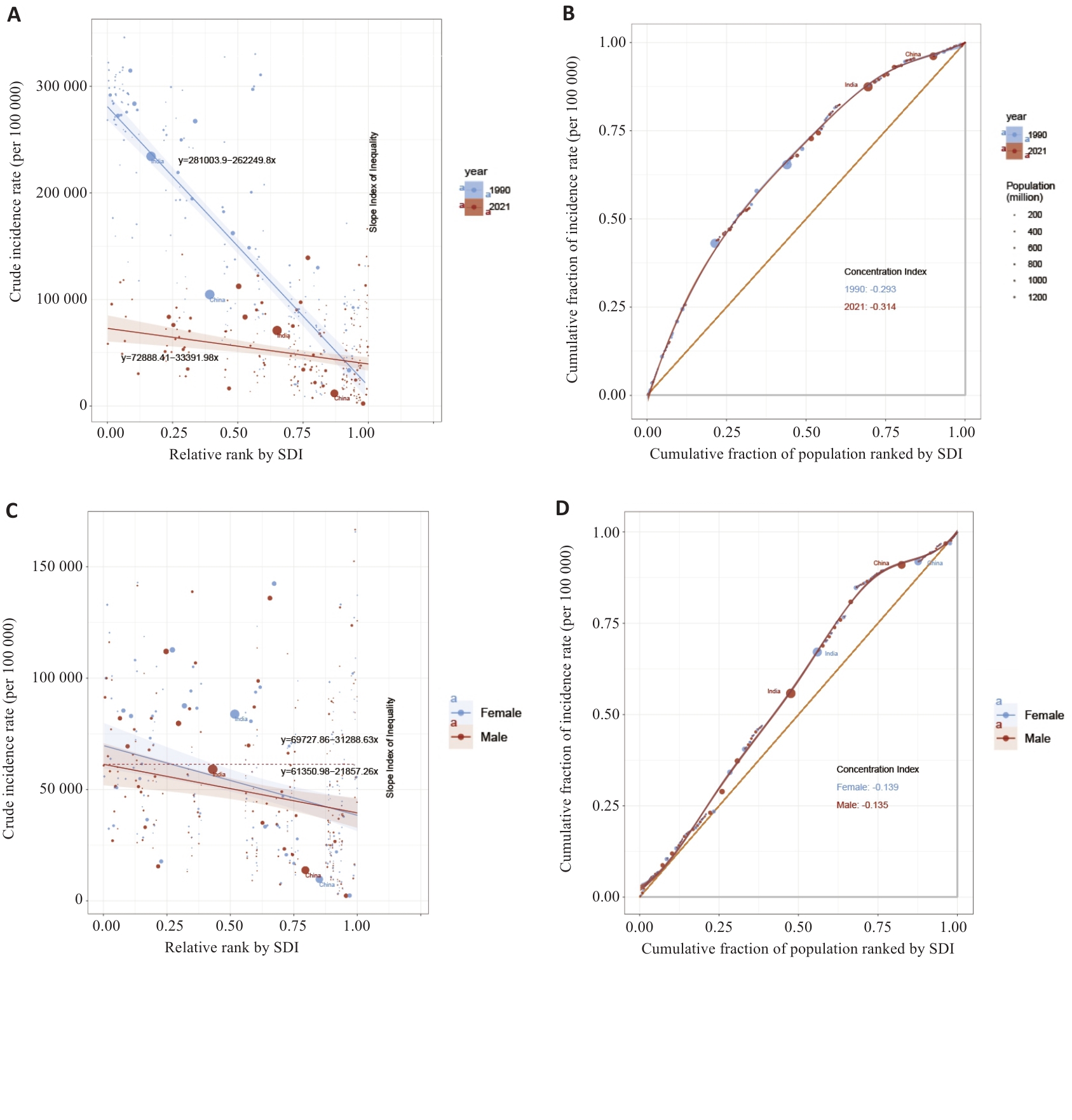
Fig.6 Global inequality analysis for diarrheal diseases in children under 5 years. A: Inequality regression curve between 1999 and 2021. B: Concentration curve between 1999 and 2021. C: Inequality regression curve between male and female. D: Concentration curve between male and female.
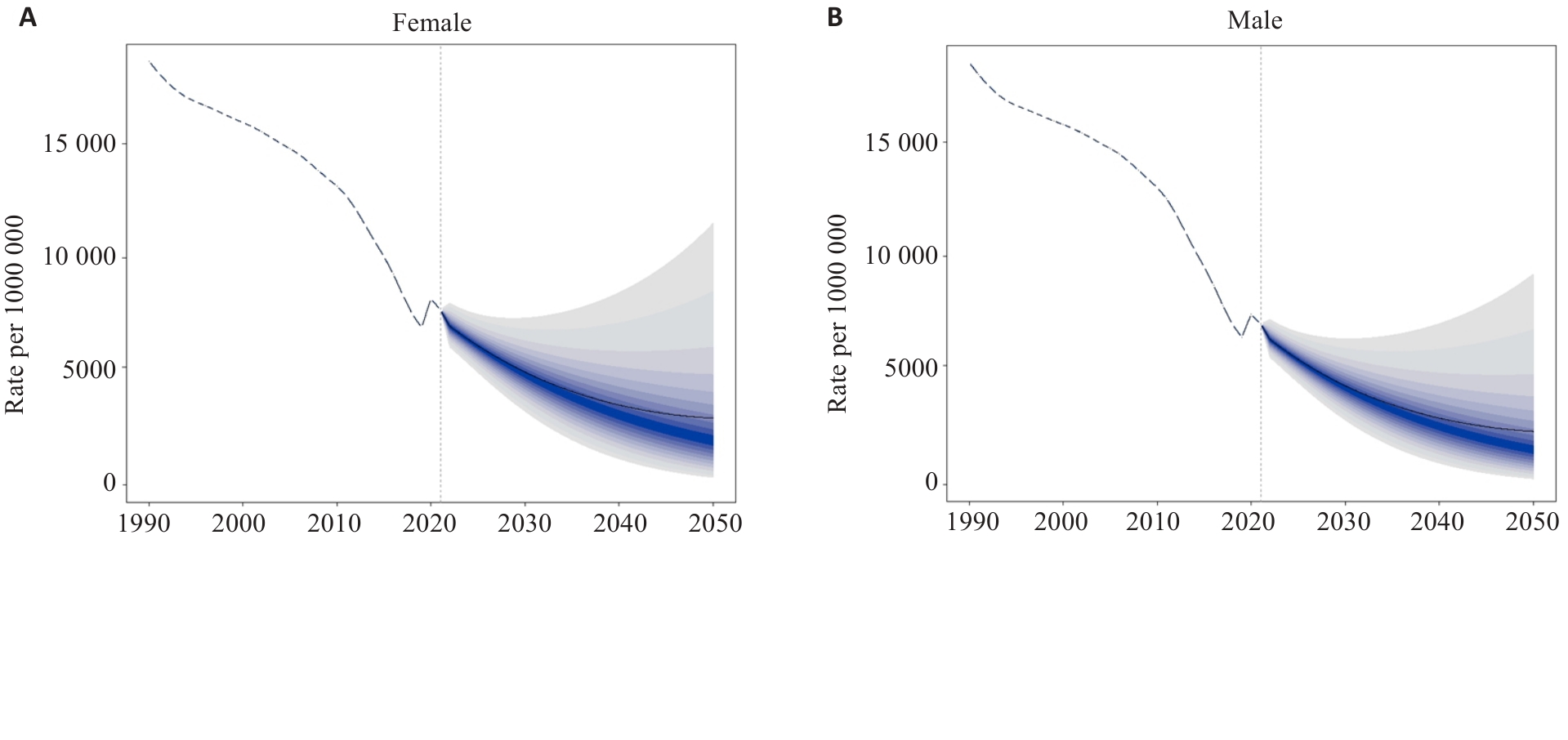
Fig.7 Predicted global incidence rate of diarrheal diseases among female (A) and male (B) children under 5 years from 2022 to 2050 based on the BAPC model (per 100 000). The black line represents the predicted mean incidence rate, and the gradient area is its 95% confidence interval.
| [1] | GBD 2016 Diarrhoeal Disease Collaborators. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of diarrhoea in 195 countries: a systematic analysis for the Global Burden of Disease Study 2016[J]. Lancet Infect Dis, 2018, 18(11): 1211-28. |
| [2] | Behera DK, Mishra S. The burden of diarrhea, etiologies, and risk factors in India from 1990 to 2019: evidence from the global burden of disease study[J]. BMC Public Health, 2022, 22(1): 92. doi:10.1186/s12889-022-12515-3 |
| [3] | Chowdhury F, Ross AG, Islam MT, et al. Diagnosis, management, and future control of cholera[J]. Clin Microbiol Rev, 2022, 35(3): e0021121. doi:10.1128/cmr.00211-21 |
| [4] | Khalil I, Colombara DV, Forouzanfar MH, et al. Burden of diarrhea in the eastern Mediterranean Region, 1990-2013: findings from the global burden of disease study 2013[J]. Am J Trop Med Hyg, 2016, 95(6): 1319-29. |
| [5] | Atherly DE, Lewis KDC, Tate J, et al. Projected health and economic impact of rotavirus vaccination in GAVI-eligible countries: 2011-2030[J]. Vaccine, 2012, 30(): A7-14. doi:10.1016/j.vaccine.2011.12.096 |
| [6] | Black RE. Progress in the use of ORS and zinc for the treatment of childhood diarrhea[J]. J Glob Health, 2019, 9(1): 010101. doi:10.7189/jogh.09.010101 |
| [7] | Munos MK, Walker CL, Black RE. The effect of oral rehydration solution and recommended home fluids on diarrhoea mortality[J]. Int J Epidemiol, 2010, 39(): i75-87. doi:10.1093/ije/dyq025 |
| [8] | Nonvignon J, Atherly D, Pecenka C, et al. Cost-effectiveness of rotavirus vaccination in Ghana: examining impacts from 2012 to 2031[J]. Vaccine, 2018, 36(47): 7215-21. doi:10.1016/j.vaccine.2017.11.080 |
| [9] | Kotloff KL, Nataro JP, Blackwelder WC, et al. Burden and aetiology of diarrhoeal disease in infants and young children in developing countries (the Global Enteric Multicenter Study, GEMS): a prospective, case-control study[J]. Lancet, 2013, 382(9888): 209-22. |
| [10] | Lawn JE, Wilczynska-Ketende K, Cousens SN. Estimating the causes of 4 million neonatal deaths in the year 2000[J]. Int J Epidemiol, 2006, 35(3): 706-18. doi:10.1093/ije/dyl043 |
| [11] | Black RE, Perin J, Yeung D, et al. Estimated global and regional causes of deaths from diarrhoea in children younger than 5 years during 2000-21: a systematic review and Bayesian multinomial analysis[J]. Lancet Glob Health, 2024, 12(6): e919-28. doi:10.1016/s2214-109x(24)00078-0 |
| [12] | Heine L, Alfinete NW, Potgieter N, et al. Multi- and extensively drug resistant Escherichia coli isolated from South African children under 5 years old with diarrhoea[J]. Diagn Microbiol Infect Dis, 2024, 109(2): 116279. doi:10.1016/j.diagmicrobio.2024.116279 |
| [13] | Shumetie G, Gedefaw M, Kebede A, et al. Exclusive breastfeeding and rotavirus vaccination are associated with decreased diarrheal morbidity among under-five children in Bahir Dar, northwest Ethiopia[J]. Public Health Rev, 2018, 39: 28. doi:10.1186/s40985-018-0107-6 |
| [14] | Collinson S, Deans A, Padua-Zamora A, et al. Probiotics for treating acute infectious diarrhoea[J]. Cochrane Database Syst Rev, 2020, 12(12): CD003048. doi:10.1002/14651858.cd003048.pub4 |
| [15] | Feleke Y, Legesse A, Abebe M. Prevalence of diarrhea, feeding practice, and associated factors among children under five years in bereh district, Oromia, ethiopia [J]. Infect Dis Obstet Gynecol, 2022, 2022: 4139648. doi:10.1155/2022/4139648 |
| [16] | Girma M, Gobena T, Medhin G, et al. Determinants of childhood diarrhea in west gojjam, northwest Ethiopia: a case control study[J]. Pan Afr Med J, 2018, 30: 234. |
| [17] | Hailu B, Wu JG, Hailu T. Water, sanitation, and hygiene risk factors on the prevalence of diarrhea among under-five children in the rural community of dangila district, northwest Ethiopia[J]. J Trop Med, 2021, 2021: 2688500. doi:10.1155/2021/2688500 |
| [18] | Natnael T, Lingerew M, Adane M. Prevalence of acute diarrhea and associated factors among children under five in semi-urban areas of northeastern Ethiopia[J]. BMC Pediatr, 2021, 21(1): 290. doi:10.1186/s12887-021-02762-5 |
| [19] | GBD Diarrhoeal Diseases Collaborators. Estimates of global, regional, and national morbidity, mortality, and aetiologies of diarrhoeal diseases: a systematic analysis for the Global Burden of Disease Study 2015[J]. Lancet Infect Dis, 2017, 17(9): 909-48. |
| [20] | Ugboko HU, Nwinyi OC, Oranusi SU, et al. Childhood diarrhoeal diseases in developing countries[J]. Heliyon, 2020, 6(4): e03690. doi:10.1016/j.heliyon.2020.e03690 |
| [21] | Simen-Kapeu A, Bogler L, Weber AC, et al. Prevalence of diarrhoea, acute respiratory infections, and malaria over time (1995-2017): a regional analysis of 23 countries in West and Central Africa[J]. J Glob Health, 2021, 11: 13008. doi:10.7189/jogh.11.13008 |
| [22] | Florez ID, Niño-Serna LF, Beltrán-Arroyave CP. Acute infectious diarrhea and gastroenteritis in children[J]. Curr Infect Dis Rep, 2020, 22(2): 4. doi:10.1007/s11908-020-0713-6 |
| [23] | Poly F, Noll AJ, Riddle MS, et al. Update on Campylobacter vaccine development[J]. Hum Vaccin Immunother, 2019, 15(6): 1389-400. doi:10.1080/21645515.2018.1528410 |
| [24] | Hartman RM, Cohen AL, Antoni S, et al. Risk factors for mortality among children younger than age 5 years with severe diarrhea in low- and middle-income countries: findings from the World Health Organization-coordinated global rotavirus and pediatric diarrhea surveillance networks[J]. Clin Infect Dis, 2023, 76(3): e1047-53. doi:10.1093/cid/ciac865 |
| [25] | Atchison CJ, Tam CC, Hajat S, et al. Temperature-dependent transmission of rotavirus in Great Britain and the Netherlands[J]. Proc Biol Sci, 2010, 277(1683): 933-42. doi:10.1098/rspb.2009.1755 |
| [26] | Lopez AL, Dutta S, Qadri F, et al. Cholera in selected countries in Asia[J]. Vaccine, 2020, 38(): A18-24. doi:10.1016/j.vaccine.2019.07.035 |
| [27] | Smits SL, Schapendonk CME, van Beek J, et al. New viruses in idiopathic human diarrhea cases, the Netherlands[J]. Emerg Infect Dis, 2014, 20(7): 1218-22. doi:10.3201/eid2007.140190 |
| [28] | Alkaissy Y, Serre-Delcor N, Vicente MA, et al. Trends in imported infections among migrants and travellers to Spain: a decade of analysis through the +Redivi network (2012-2022)[J]. J Travel Med, 2024, 31(6): taae067. doi:10.1093/jtm/taae067 |
| [29] | van Dongen JAP, Rouers EDM, Schuurman R, et al. Acute gastroenteritis disease burden in infants with medical risk conditions in the Netherlands[J]. Pediatr Infect Dis J, 2021, 40(4): 300-5. doi:10.1097/inf.0000000000003002 |
| [30] | Antoni S, Nakamura T, Cohen AL, et al. Rotavirus genotypes in children under five years hospitalized with diarrhea in low and middle-income countries: Results from the WHO-coordinated Global Rotavirus Surveillance Network[J]. PLoS Glob Public Health, 2023, 3(11): e0001358. doi:10.1371/journal.pgph.0001358 |
| [31] | Ardura-Garcia C, Kreis C, Rakic M, et al. Rotavirus disease and health care utilisation among children under 5 years of age in highly developed countries: a systematic review and meta-analysis[J]. Vaccine, 2021, 39(22): 2917-28. doi:10.1016/j.vaccine.2021.04.039 |
| [32] | Hallowell BD, Tate J, Parashar U. An overview of rotavirus vaccination programs in developing countries[J]. Expert Rev Vaccines, 2020, 19(6): 529-37. doi:10.1080/14760584.2020.1775079 |
| [33] | Lee B, Damon CF, Platts-Mills JA. Pediatric acute gastroenteritis associated with adenovirus 40/41 in low-income and middle-income countries[J]. Curr Opin Infect Dis, 2020, 33(5): 398-403. doi:10.1097/qco.0000000000000663 |
| [34] | Ahmed AK, Sijercic VC, Akhtar MS, et al. Cholera Rages in Africa and the middle east: a narrative review on challenges and solutions[J]. Health Sci Rep, 2024, 7(5): e2013. doi:10.1002/hsr2.2013 |
| [35] | Chavda VP, Vuppu S, Mishra T, et al. Combatting infectious diarrhea: innovations in treatment and vaccination strategies[J]. Expert Rev Vaccines, 2024, 23(1): 246-65. doi:10.1080/14760584.2023.2295015 |
| [1] | Yitong LIU, Ke ZHAO, Xiaodong WANG. Lip and oral cancers in East Asia from 1990 to 2035: trends of disease burden and future projections [J]. Journal of Southern Medical University, 2025, 45(7): 1554-1562. |
| [2] | WU Ke-rong Foreign Language Center,Medical School, Sun Yat-sen University, Guangzhou 510089, China. Thoughts on modern aphasic discourse studies [J]. Journal of Southern Medical University, 2006, 26(04): 497-499. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||