Journal of Southern Medical University ›› 2024, Vol. 44 ›› Issue (12): 2265-2275.doi: 10.12122/j.issn.1673-4254.2024.12.01
Yuxue ZAHNG1( ), Jieying LAN1, Xinyi MA2, Qiong ZHOU1, Mengchen QIN1, Lei GAO1,3,4(
), Jieying LAN1, Xinyi MA2, Qiong ZHOU1, Mengchen QIN1, Lei GAO1,3,4( )
)
Received:2024-08-21
Online:2024-12-20
Published:2024-12-26
Contact:
Lei GAO
E-mail:1610045163@qq.com;rayg@foxmail.com
Supported by:Yuxue ZAHNG, Jieying LAN, Xinyi MA, Qiong ZHOU, Mengchen QIN, Lei GAO. Exocarpium Citri Grandis formula granules alleviate fatty liver disease in Zebrafish by maintaining iron homeostasis and suppressing lipid peroxidation and ferroptosis[J]. Journal of Southern Medical University, 2024, 44(12): 2265-2275.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2024.12.01
| Primer | Primer sequence (5'-3') | Primer sequence (5'-3') |
|---|---|---|
| β-actin | ATGGATGAGGAAATCGCTGCC | CTCCCTGATGTCTGGGTCGTC |
| FASN | GAGAAAGCTTGCCAAACAGG | GAGGGTCTTGCAGGAGACAG |
| SREBP1 | CATCCACATGGCTCTGAGTG | CTCATCCACAAAGAAGCGGT |
| HMGCRA | CCTGTTAGCCGTCAGTGGA | TCTTTGACCACTCGTGCCG |
| PPARα | TGCTGGACTACCAGAACTGTGACA | TGCTGGCTGAGAACACTTCTGAG |
| Apoa1 | GCACTAAGCTGACCGAGCGT | GGAGGTCCTGGGTGTGTGGA |
| TNF-α | GCTTATGAGCCATGCAGTGA | TGCCCAGTCTGTCTCCTTCT |
| IL6 | CCTCAAACCTTCAGACCGCT | GAACAGGATCGAGTGGACCG |
| Tf | GTTGATGGTGGCCAGGTGTA | AGCGTAGTAACTTGCGGTCC |
| TfR | CCGCTCATACTCGCGGTTTA | TGGTTCAGAACGACCTGTGG |
| FPN | GCCAACGTCACCGTTTTTGA | CGGTCAAGTCGAAGGACCAA |
| GPX4 | GAGGTTTACGCATCCTGGCT | GGCTGATCCTTCAGCCACTT |
| SLC7A11 | TGTGGGAATGTCACTGGTGG | ACGCCTCCAGAATGTACGTG |
Tab.1 Primer sequences for RT-qPCR
| Primer | Primer sequence (5'-3') | Primer sequence (5'-3') |
|---|---|---|
| β-actin | ATGGATGAGGAAATCGCTGCC | CTCCCTGATGTCTGGGTCGTC |
| FASN | GAGAAAGCTTGCCAAACAGG | GAGGGTCTTGCAGGAGACAG |
| SREBP1 | CATCCACATGGCTCTGAGTG | CTCATCCACAAAGAAGCGGT |
| HMGCRA | CCTGTTAGCCGTCAGTGGA | TCTTTGACCACTCGTGCCG |
| PPARα | TGCTGGACTACCAGAACTGTGACA | TGCTGGCTGAGAACACTTCTGAG |
| Apoa1 | GCACTAAGCTGACCGAGCGT | GGAGGTCCTGGGTGTGTGGA |
| TNF-α | GCTTATGAGCCATGCAGTGA | TGCCCAGTCTGTCTCCTTCT |
| IL6 | CCTCAAACCTTCAGACCGCT | GAACAGGATCGAGTGGACCG |
| Tf | GTTGATGGTGGCCAGGTGTA | AGCGTAGTAACTTGCGGTCC |
| TfR | CCGCTCATACTCGCGGTTTA | TGGTTCAGAACGACCTGTGG |
| FPN | GCCAACGTCACCGTTTTTGA | CGGTCAAGTCGAAGGACCAA |
| GPX4 | GAGGTTTACGCATCCTGGCT | GGCTGATCCTTCAGCCACTT |
| SLC7A11 | TGTGGGAATGTCACTGGTGG | ACGCCTCCAGAATGTACGTG |
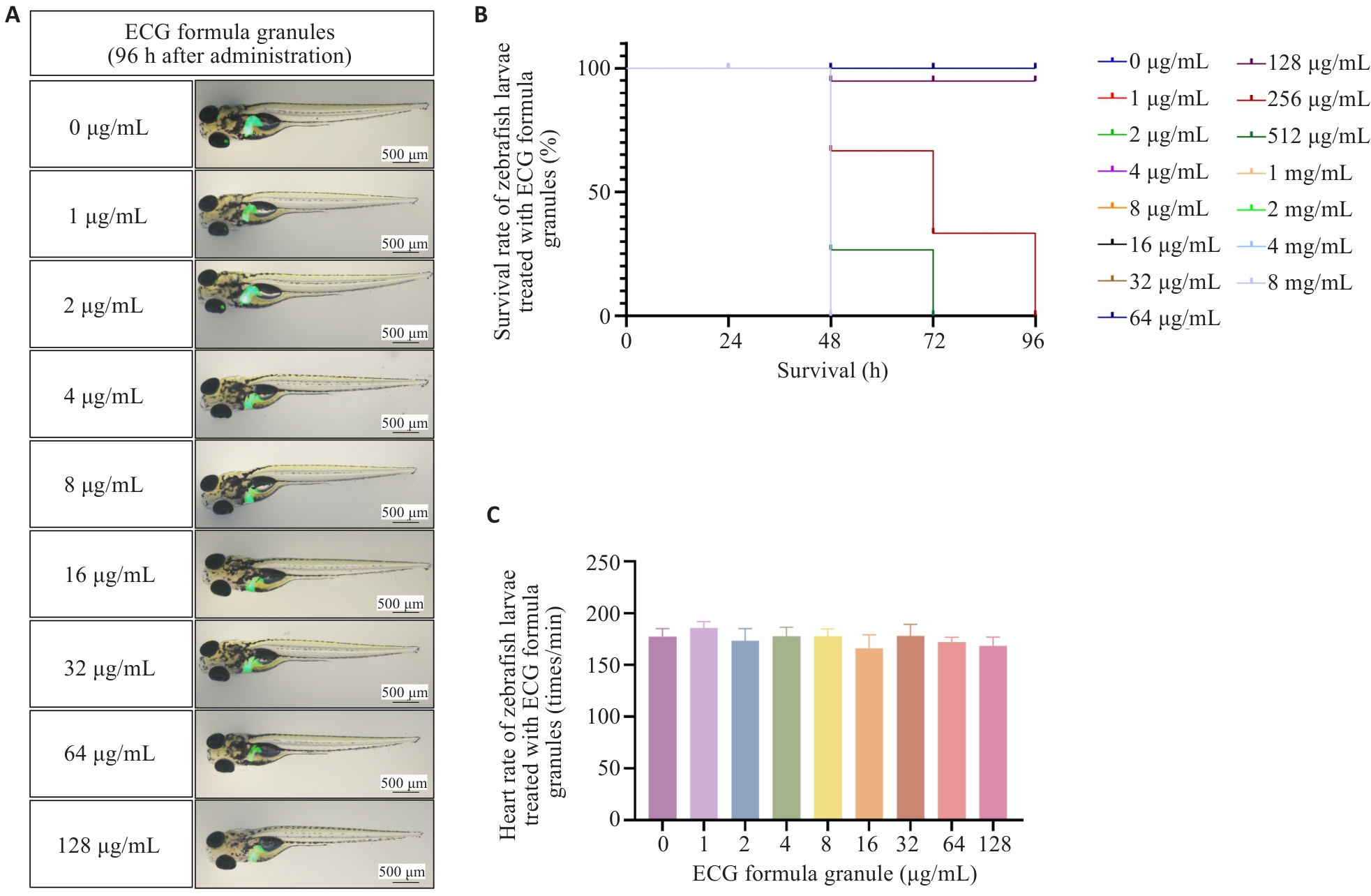
Fig.1 Results of acute toxicity test of Exocarpium Citri Grandis (ECG) in zebrafish larvae. A: Development of zebrafish larvae 96 h after ECG administration. B: Effects of ECG granules on survival of zebrafish. C: Effects of ECG granules on heart rate of zebrafish at 96 h after administration.

Fig.2 Efficacy evaluation of ECG decoction tablets and ECG granules for treatment of NAFLD in zebrafish larvae. A: HE staining of the liver of zebrafish larvae in each group. B: Whole fish oil red O staining in different groups. C: Effects of ECG decoction tablets and ECG granules on lipid metabolism-related genes and inflammatory factors. ECGFG:Exocarpium Citri Grandis formula granules.*P<0.05, **P<0.01, ***P<0.001, ****P<0.0001.
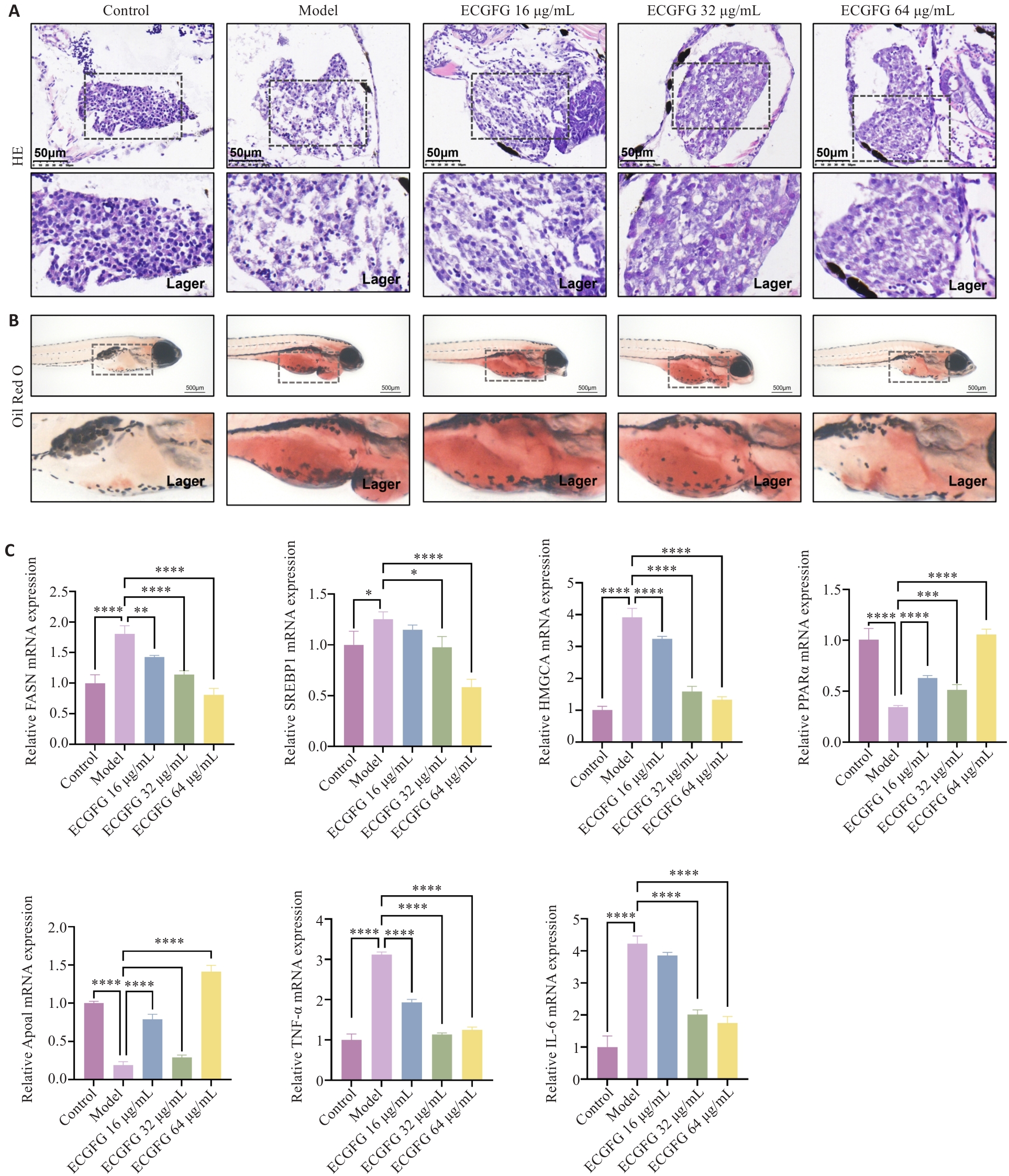
Fig.3 Efficacy evaluation of ECG decoction tablets and ECG granules for treatment of ALD in zebrafish larvae. A: HE staining of the liver of zebrafish larvae in each group. B: Whole fish oil red O staining in different groups. C: Effects of ECG decoction tablets and ECG granules on lipid metabolism-related genes and inflammatory factors. *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001.
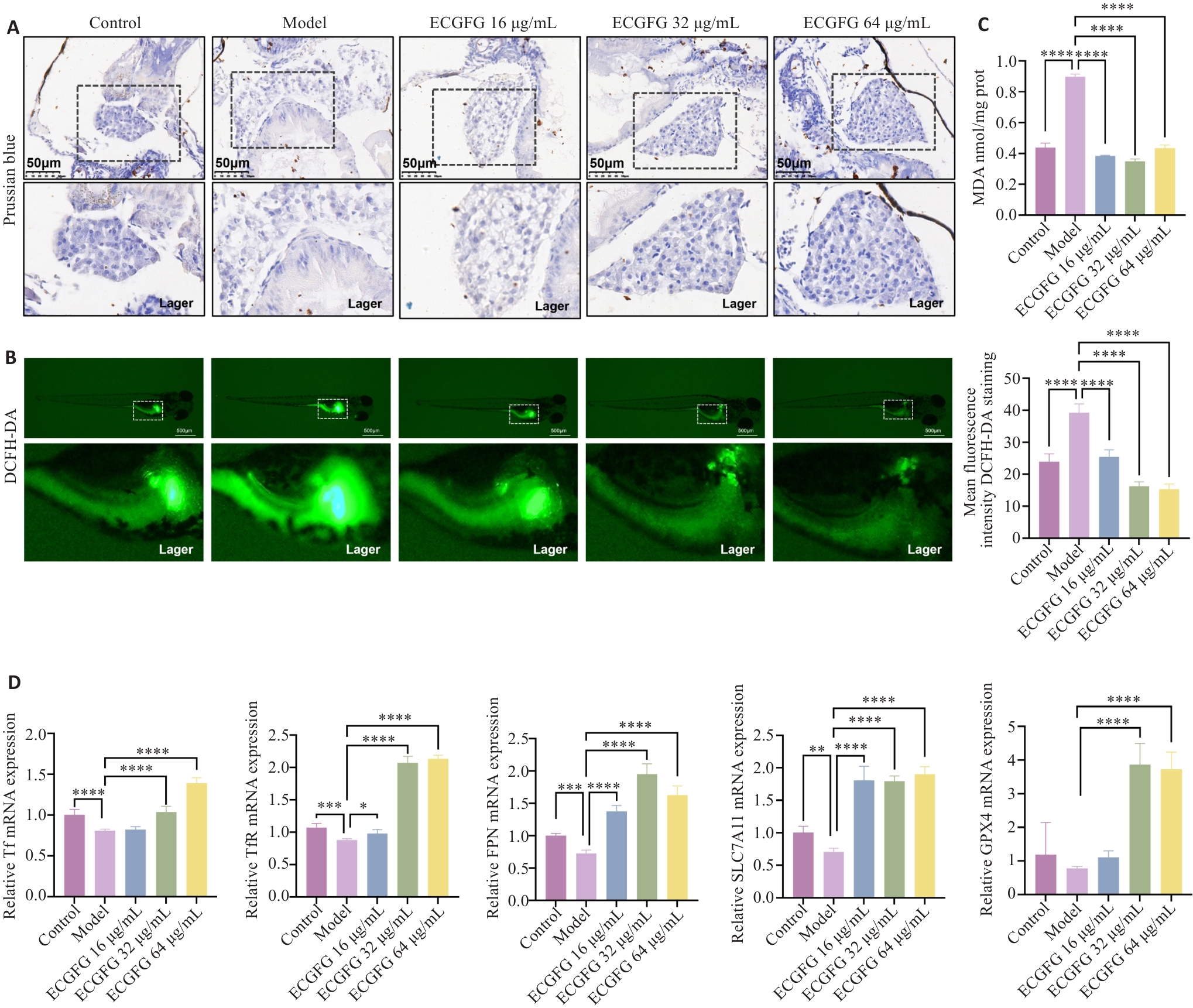
Fig.4 Effect of ECG granules on iron metabolism and ferroptosis in zebrafish larvae models of NAFLD. A: Prussian blue staining of the liver of zebrafish larvae in each group. B: DCFH-DA probe detection of zebrafish larvae in each group. C: Detection of MDA content in zebrafish larvae in each group. D: Effects of ECG granules on iron metabolism- and ferroptosis-related genes. *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001.
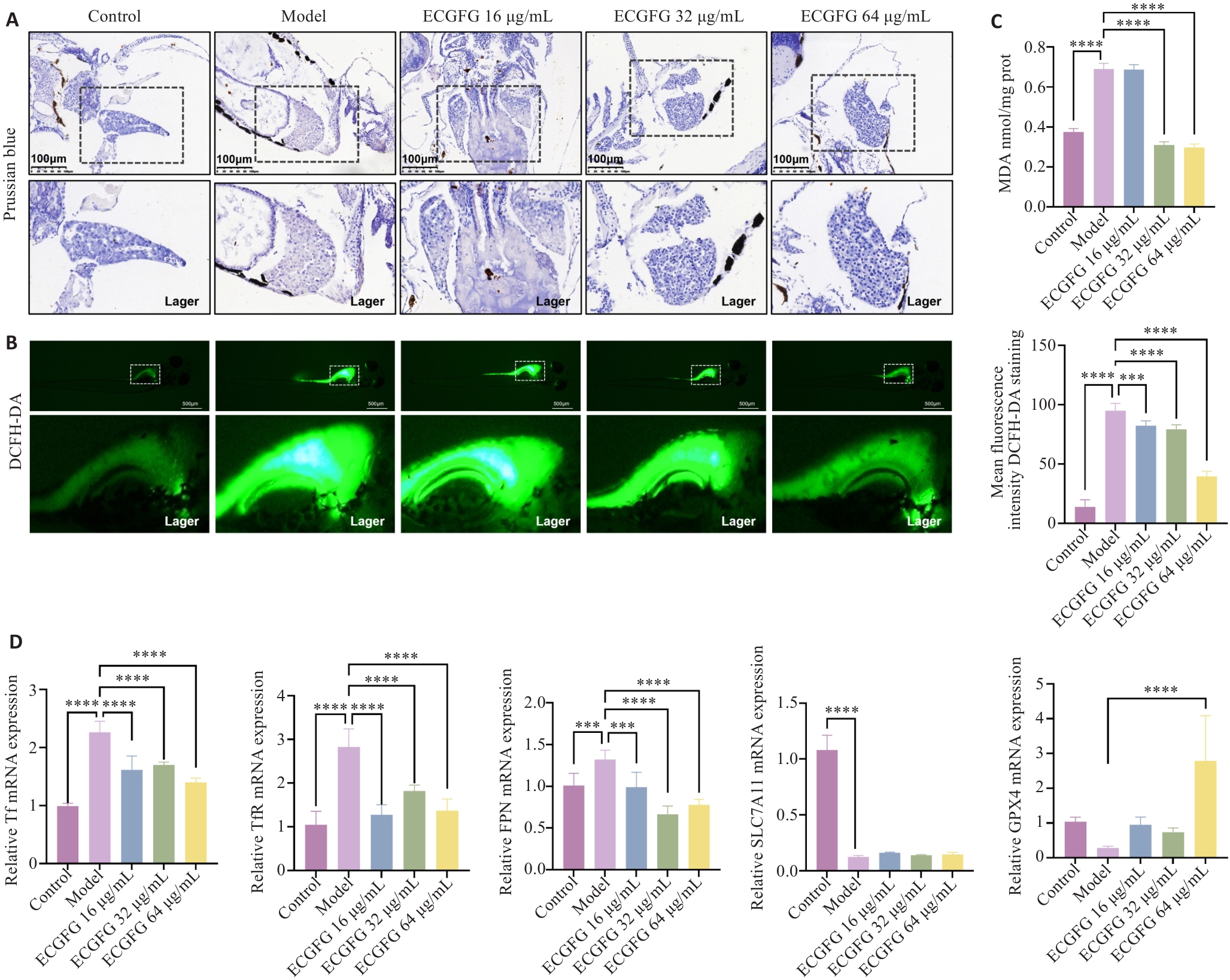
Fig.5 Effect of ECG granules on iron metabolism and ferroptosis in zebrafish larvae models of ALD. A: Prussian blue staining of the liver of zebrafish larvae in each group. B: DCFH-DA probe detection of zebrafish larvae in each group. C: Detection of MDA content in zebrafish larvae in each group. D: Effects of ECG granules on expressions of iron metabolism- and ferroptosis-related genes. ***P<0.001, ****P<0.0001.
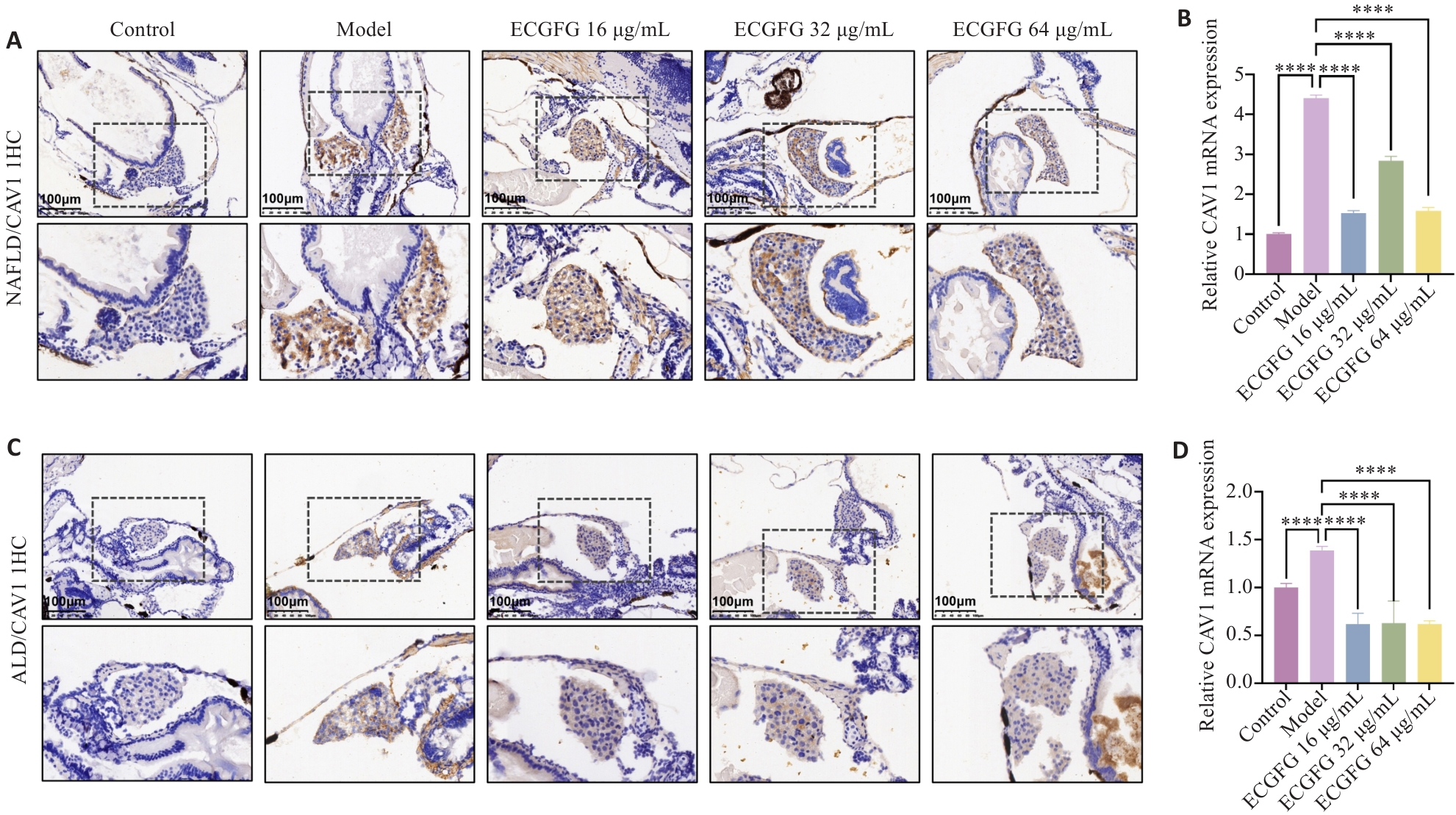
Fig.6 ECG granules regulate hepatic iron metabolism and ferroptosis possibly through CAV1 in zebrafish larvae. A: Liver CAV1 immunohistochemical staining in zebrafish larvae models of NAFLD. B: Effect of ECG granules on CAV1 expression in zebrafish larvae models of NAFLD. C: Liver CAV1 immunohistochemical staining in zebrafish larvae models of ALD. D: Effect of ECG granules on CAV1 expression in zebrafish larvae models of ALD. ****P<0.0001.
| 1 | 国家药典委员会. 中华人民共和国药典-一部: 2020年版[M]. 北京: 中国 医药科技出版社, 2020. |
| 2 | 范会云, 邓乔华, 宋松泉. “一片值千金”: 化橘红[J]. 生命世界, 2020(9): 40-1. |
| 3 | Musso G, Bo S, Cassader M, et al. Impact of sterol regulatory element-binding factor-1c polymorphism on incidence of nonalcoholic fatty liver disease and on the severity of liver disease and of glucose and lipid dysmetabolism[J]. Am J Clin Nutr, 2013, 98(4): 895-906. |
| 4 | 中华中医药学会脾胃病分会, 张 莉, 季 光, 等. 非酒精性脂肪性肝病中医诊疗专家共识(2023)[J]. 中国中西医结合消化杂志, 2024, 10(1): 1-7. |
| 5 | 毕占阳, 杨 柱, 郭 斌, 等. 基于酒伤理论探讨酒精性肝病的中医治疗[J]. 云南中医中药杂志, 2022, 43(5): 16-9. |
| 6 | 李锦坤, 金刚亮, 王艳慧, 等. 化橘红提取物的制备工艺优化及其降脂作用[J/OL]. 现代食品 科技, 2024,06. 10.13982/j.mfst.1673-9078.2024.10.0892 |
| 7 | 吴道顺, 王梦晨, 张雪涟, 等. 化橘红水提物对酒精诱导的急性肝损伤保护作用[J]. 中国实验方剂学杂志, 2022, 28(19): 42-8. |
| 8 | Deng GH, Liu C, Zhao JM, et al. Exocarpium Citri Grandis alleviates the aggravation of NAFLD by mitigating lipid accumulation and iron metabolism disorders[J]. J Ethnopharmacol, 2023, 313: 116559. |
| 9 | 吴雄志, 卞兆祥, 陈新宇, 等. 中药配方颗粒临床应用国际专家共识[J]. TMR经典中医研究, 2021, 7(1): 19-26. |
| 10 | 谭婉清, 王术玲, 刘潇潇, 等. 化橘红配方颗粒与饮片汤剂的化学等量性和药效等效性研究[J]. 中药新药与临床药理, 2023, 34(4): 541-9. |
| 11 | 米永佳, 王茂泓, 李龙华, 等. 全国名中医张小萍教授治疗非酒精性脂肪肝经验[J]. 中国民族民间医药, 2024, 33(12): 80-3. |
| 12 | 方俐晖, 郭志玲, 张轶斐, 等. 田德禄教授三期三脏辨治酒精性肝病经验[J]. 现代中医临床, 2021, 28(5): 38-42. |
| 13 | 王艳慧. 化橘红的研究进展[J]. 世界科学技术-中医药现代化, 2017, 19(6): 1076-82. |
| 14 | 苏志鹏. 化橘红活性成分的综合利用及对降血糖血脂活性的研究[D]. 广州: 广东药科大学, 2019. |
| 15 | 吴 祎. 化橘红解酒功效与保健食品的研究[D]. 广州: 广州中医药大学, 2014. |
| 16 | 黄凯伟, 任应宗, 张 辉, 等. 化橘红(柚)饮片、标准汤剂和配方颗粒相关性研究[J]. 中国药业, 2023, 32(17): 57-62. |
| 17 | Silva B, Faustino P. An overview of molecular basis of iron metabolism regulation and the associated pathologies[J]. Biochim Biophys Acta, 2015, 1852(7): 1347-59. |
| 18 | Vogt AC S, Arsiwala T, Mohsen M, et al. On iron metabolism and its regulation[J]. Int J Mol Sci, 2021, 22(9): 4591. |
| 19 | Graham RM, Chua AC, Herbison CE, et al. Liver iron transport[J]. World J Gastroenterol, 2007, 13(35): 4725-36. |
| 20 | Aigner E, Weiss G, Datz C. Dysregulation of iron and copper homeostasis in nonalcoholic fatty liver[J]. World J Hepatol, 2015, 7(2): 177-88. |
| 21 | Bessone F, Razori MV, Roma MG. Molecular pathways of nonalcoholic fatty liver disease development and progression[J]. Cell Mol Life Sci, 2019, 76(1): 99-128. |
| 22 | Sun KX, Zhao JV, Nelson EAS, et al. Iron status and non-alcoholic fatty liver disease: a Mendelian randomization study[J]. Nutrition, 2024, 118: 112295. |
| 23 | Yu GF, Liu L, Qin T, et al. Associations of serum iron status with MAFLD and liver fibrosis in the USA: a nationwide cross-section study[J]. Biol Trace Elem Res, 2024, 202(1): 87-98. |
| 24 | Deng GH, Liu C, Zhao JM, et al. Exocarpium Citri Grandis alleviates |
| the aggravation of NAFLD by mitigating lipid accumulation and iron | |
| metabolism disorders[J]. J Ethnopharmacol, 2023, 313: 116559. | |
| 25 | Ali N, Ferrao K, Mehta KJ. Liver iron loading in alcohol-associated liver disease[J]. Am J Pathol, 2023, 193(10): 1427-39. |
| 26 | Li LX, Guo FF, Liu H, et al. Iron overload in alcoholic liver disease: |
| mechanismsunderlying, effectsdetrimental, and therapeuticpotential | |
| targets[J]. Cell Mol Life Sci, 2022, 79(4): 201. | |
| 27 | Chen JY, Li XP, Ge CD, et al. The multifaceted role of ferroptosis in liver disease[J]. Cell Death Differ, 2022, 29(3): 467-80. |
| 28 | Chen X, Li J, Kang R, et al. Ferroptosis: machinery and regulation[J]. Autophagy, 2021, 17(9): 2054-81. |
| 29 | Koppula P, Zhuang L, Gan BY. Cystine transporter SLC7A11/xCT in cancer: ferroptosis, nutrient dependency, and cancer therapy[J]. Protein Cell, 2021, 12(8): 599-620. |
| 30 | Xie YC, Kang R, Klionsky DJ, et al. GPX4 in cell death, autophagy, and disease[J]. Autophagy, 2023, 19(10): 2621-38. |
| 31 | Stockwell BR. Ferroptosis turns 10: emerging mechanisms, physiological functions, and therapeutic applications[J]. Cell, 2022, 185(14): 2401-21. |
| 32 | Chen X, Li JB, Kang R, et al. Ferroptosis: machinery and regulation[J]. Autophagy, 2021, 17(9): 2054-81. |
| 33 | Sui YT, Geng X, Wang ZW, et al. Targeting the regulation of iron homeostasis as a potential therapeutic strategy for nonalcoholic fatty liver disease[J]. Metabolism, 2024, 157: 155953. |
| 34 | Luo J, Song G, Chen NN, et al. Ferroptosis contributes to ethanol-induced hepatic cell death via labile iron accumulation and GPx4 inactivation[J]. Cell Death Discov, 2023, 9(1): 311. |
| 35 | Fernández-Rojo MA, Gongora M, Fitzsimmons RL, et al. Caveolin-1 is necessary for hepatic oxidative lipid metabolism: evidence for crosstalk between caveolin-1 and bile acid signaling[J]. Cell Rep, 2013, 4(2): 238-47. |
| 36 | Haddad D, Al Madhoun A, Nizam R, et al. Role of caveolin-1 in diabetes and its complications[J]. Oxid Med Cell Longev, 2020, 2020: 9761539. |
| 37 | Jiang Y, Krantz S, Qin X, et al. Caveolin-1 controls mitochondrial damage and ROS production by regulating fission - fusion dynamics and mitophagy[J]. Redox Biol, 2022, 52: 102304. |
| 38 | Fernández MA, Albor C, Ingelmo-Torres M, et al. Caveolin-1 is essential for liver regeneration[J]. Science, 2006, 313(5793): 1628-32. |
| 39 | Fernandez-Rojo MA, Ramm GA. Caveolin-1 function in liver physiology and disease[J]. Trends Mol Med, 2016, 22(10): 889-904. |
| 40 | Gao L, Zhou YC, Zhong WC, et al. Caveolin-1 is essential for protecting against binge drinking-induced liver damage through inhibiting reactive nitrogen species[J]. Hepatology, 2014, 60(2): 687-99. |
| 41 | Tao L, Wang JP, Wang K, et al. Exerkine FNDC5/irisin-enriched exosomes promote proliferation and inhibit ferroptosis of osteoblasts through interaction with Caveolin-1[J]. Aging Cell, 2024, 23(8): e14181. |
| 42 | Zhang T, Yang F, Dai XY, et al. Role of Caveolin-1 on the molybdenum and cadmium exposure induces pulmonary ferroptosis and fibrosis in the sheep[J]. Environ Pollut, 2023, 334: 122207. |
| 43 | Liu WH, Luo GH. CAV1 inhibits Xc (-) system through IFNGR1 to promote ferroptosis to inhibit stemness and improves anti-PD-1 efficacy in breast cancer[J]. Transl Oncol, 2024, 50: 102149. |
| 44 | Deng GH, Li YJ, Ma SY, et al. Caveolin-1 dictates ferroptosis in the execution of acute immune-mediated hepatic damage by attenuating nitrogen stress[J]. Free Radic Biol Med, 2020, 148: 151-61. |
| 45 | Huang S, Wang YH, Xie SW, et al. Isoliquiritigenin alleviates liver |
| fibrosis through caveolin-1-mediated hepatic stellate cells ferroptosis | |
| in zebrafish and mice[J]. Phytomedicine, 2022, 101: 154117. | |
| 46 | Amali AA, Rekha RD, Lin CJ, et al. Thioacetamide induced liver damage in zebrafish embryo as a disease model for steatohepatitis[J]. J Biomed Sci, 2006, 13(2): 225-32. |
| 47 | Tacke F. Cenicriviroc for the treatment of non-alcoholic steatohepatitis and liver fibrosis[J]. Expert Opin Investig Drugs, 2018, 27(3): 301-11. |
| 48 | Bautista AP. Neutrophilic infiltration in alcoholic hepatitis[J]. Alcohol, 2002, 27(1): 17-21. |
| [1] | Jing XIAO, Ying LI, Min FANG, Hong GONG, Wen LI, Chunyan ZHANG, Fangyao CHEN, Yan ZHANG, Tuo HAN. Triglyceride-glucose index in non-obese individuals: its association with and predictive value for non-alcoholic fatty liver disease [J]. Journal of Southern Medical University, 2024, 44(7): 1266-1271. |
| [2] | Guangya CHEN, Xingliang XIANG, Zhaoxiang ZENG, Rongzeng HUANG, Shuna JIN, Mingzhong XIAO, Chengwu SONG. Regulatory effect of Diwu Yanggan Decoction on lysoglycerophospholipids in circulating exosomes in a mouse model of nonalcoholic fatty liver disease [J]. Journal of Southern Medical University, 2024, 44(7): 1382-1388. |
| [3] | GUO Xindeng, GUO Zhuolin, SUN Dongmei, ZOU Lifang, OU Jinying, YU Linzhong, LU Zibin, CAO Huihui, LIU Junshan. Single extract of Forsythia Suspense versus the prepared drug in pieces: comparison of their anti-inflammatory, antitumor and antibacterial effects in zebrafish [J]. Journal of Southern Medical University, 2024, 44(3): 594-604. |
| [4] | KONG Xiang, ZHANG Teng, ZHANG Yan, GAO Linxi, WANG Wen, WANG Mengyan, WANG Guodong, LÜ Kun. Overexpression of lncRNA HEM2M alleviates liver injury in mice with non-alcoholic fatty liver disease [J]. Journal of Southern Medical University, 2024, 44(1): 1-8. |
| [5] | DENG Guanghui, JIA Hui, LI Yunjia, LI Junjie, WU Chaofeng, SHI Hao, QIN Mengchen, ZHAO Jiamin, LIU Chang, LIAO Yuxin, GAO Lei. Erchen Decoction improves iron homeostasis in mice with non-alcoholic fatty liver disease by regulating iron transport capacity in the spleen [J]. Journal of Southern Medical University, 2023, 43(8): 1287-1296. |
| [6] | XU Longfei, HAN Jing, YANG Zhe, YANG Yanping, CHEN Jinhui, WU Xijun, WANG Qi, HONG Yan. LRG1 inhibits hepatic macrophage activation by enhancing TGF-β1 signaling to alleviate MAFLD in mice [J]. Journal of Southern Medical University, 2023, 43(7): 1164-1171. |
| [7] | GAO Yinan, WANG Peijun, LU Sumei, MA Wanshan. METTL3 inhibitor STM2457 improves metabolic dysfunction-associated fatty liver disease by regulating mitochondrial function in mice [J]. Journal of Southern Medical University, 2023, 43(10): 1689-1696. |
| [8] | GUO Zhihua, WANG Zhipeng, ZENG Linling, JI Xuexia. Effects of propofol on myelin basic protein expression in zebrafish at different developmental stages [J]. Journal of Southern Medical University, 2023, 43(10): 1810-1814. |
| [9] | ZHANG Jia, XUE Wei, ZHANG Shujun, ZHU Yali, YANG Cheng, GAO Yue, SHI Lingfeng, HUANG Wenxiang. TSPAN8 is involved in lipid metabolism in non-alcoholic fatty liver disease in mice [J]. Journal of Southern Medical University, 2022, 42(5): 705-711. |
| [10] | LIAO Xiaoshan, HAO Yuting, WU Mengting, LIU Huiping, JIANG Liang, YE Zichong, LIAO Wenzhen, DENG Hong. Dihydromyricetin reduces lipid accumulation in LO2 cells via AMPK/mTOR-mediated lipophagy pathway and inhibits HepG2 cell proliferation in vitro [J]. Journal of Southern Medical University, 2022, 42(4): 518-527. |
| [11] | . Parathyroid hormone-related protein aggravates nonalcoholic fatty liver disease induced by methionine choline-deficient diet in mice [J]. Journal of Southern Medical University, 2021, 41(7): 1037-1043. |
| [12] | . Exendin-4 promotes autophagy to relieve lipid deposition in a NAFLD cell model by activating AKT/mTOR signaling pathway [J]. Journal of Southern Medical University, 2021, 41(7): 1073-1078. |
| [13] | . Predictive value of body mass index combined with waist circumference for new-onset nonalcoholic fatty liver disease in patients with type 2 diabetes mellitus [J]. Journal of Southern Medical University, 2019, 39(11): 1293-1297. |
| [14] | . Correlation between serum 25(OH) vitamin D and liver fat content in nonalcoholic fatty liver disease [J]. Journal of Southern Medical University, 2019, 39(09): 1118-. |
| [15] | . Bortezomib and obatoclax for dual blockade of protein degradation pathways show synergistic anti-tumor effect in human acute T lymphoblastic leukemia cells [J]. Journal of Southern Medical University, 2019, 39(04): 401-. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||