Journal of Southern Medical University ›› 2024, Vol. 44 ›› Issue (10): 1955-1964.doi: 10.12122/j.issn.1673-4254.2024.10.14
Lei WANG1,2( ), Fenlan BIAN1,2, Feiyang MA3, Shu FANG3, Zihan LING3, Mengran LIU3, Hongyan SUN1,2, Chengwen FU4, Shiyao NI5, Xiaoyang ZHAO1, Xinru FENG1, Zhengyu SUN1,2, Guoqing LU1,2, Pinfang KANG1,2(
), Fenlan BIAN1,2, Feiyang MA3, Shu FANG3, Zihan LING3, Mengran LIU3, Hongyan SUN1,2, Chengwen FU4, Shiyao NI5, Xiaoyang ZHAO1, Xinru FENG1, Zhengyu SUN1,2, Guoqing LU1,2, Pinfang KANG1,2( ), Shili WU1,2(
), Shili WU1,2( )
)
Received:2024-05-31
Online:2024-10-20
Published:2024-10-31
Contact:
Pinfang KANG, Shili WU
E-mail:568733358@qq.com;kangpinfang.1016@163.com;chinawsl@126.com
Supported by:Lei WANG, Fenlan BIAN, Feiyang MA, Shu FANG, Zihan LING, Mengran LIU, Hongyan SUN, Chengwen FU, Shiyao NI, Xiaoyang ZHAO, Xinru FENG, Zhengyu SUN, Guoqing LU, Pinfang KANG, Shili WU. Activation of ALDH2 alleviates hypoxic pulmonary hypertension in mice by upregulating the SIRT1/PGC-1α signaling pathway[J]. Journal of Southern Medical University, 2024, 44(10): 1955-1964.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2024.10.14
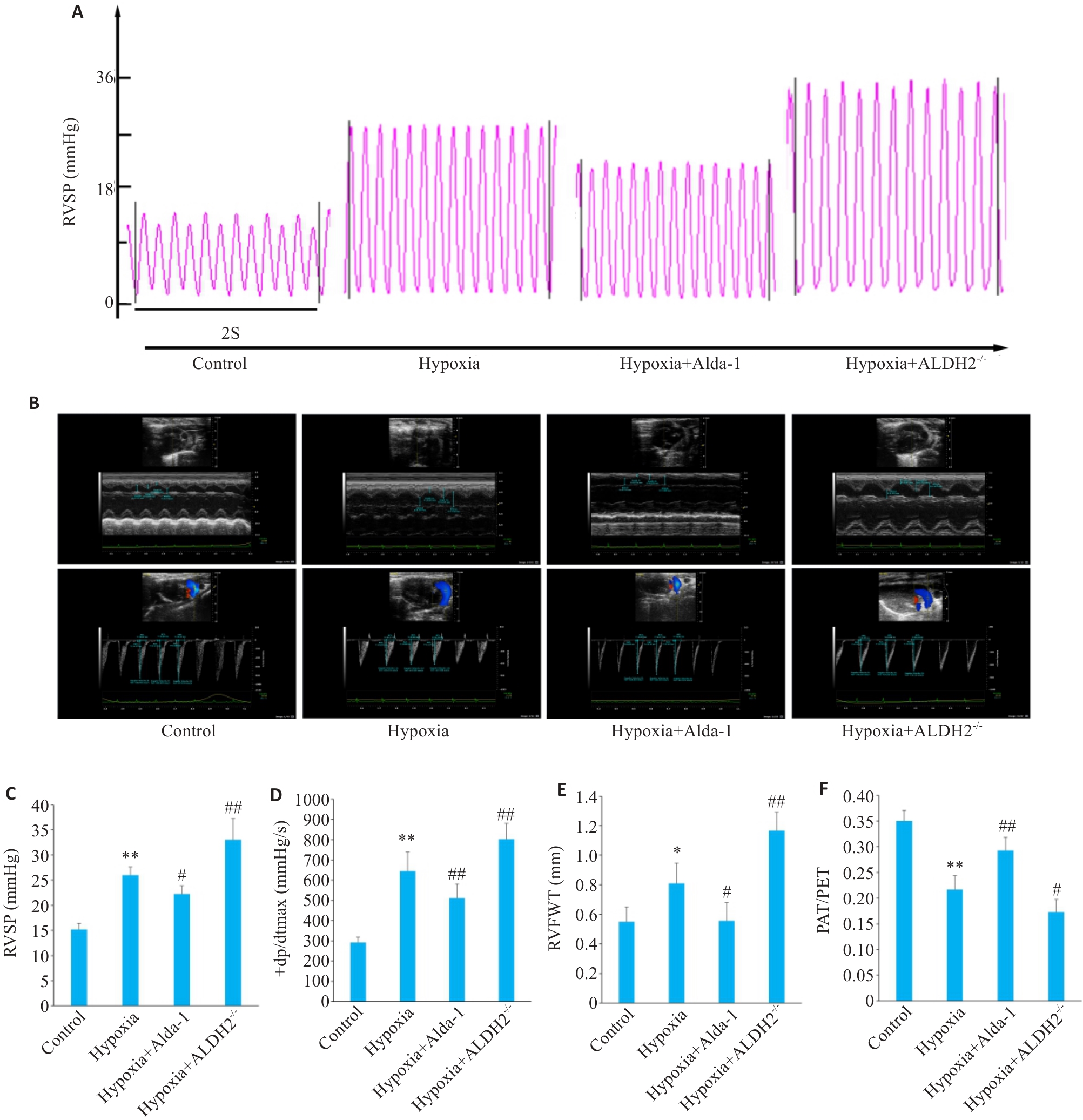
Fig.1 Comparison of right ventricular pressure (RVSP) and cardiac function of the mice among the groups. A: RVSP of the mice in each group. B: Heart color ultrasound in each group. C: Statistical diagram of RVSP in each group. D: Statistical diagram of maximum rise rate of RVSP in each group. E: Statistical map of right ventricular free wall thickness in each group. F: Statistical chart of pulmonary artery acceleration to ejection time ratio in each group. Data are presented as Mean±SD (n=6). *P<0.05, **P<0.01 vs control group; #P<0.05, ##P<0.01 vs hypoxia group.
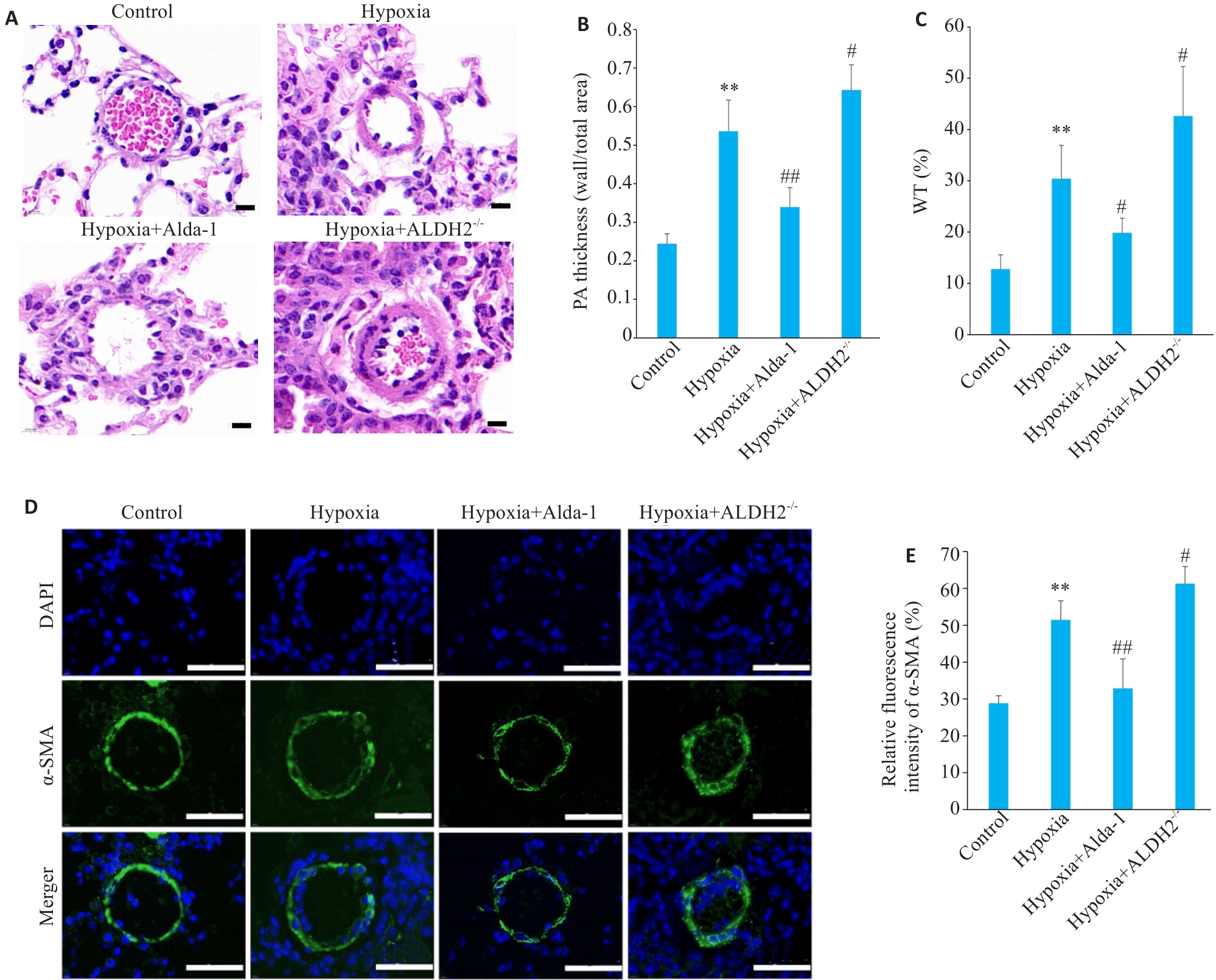
Fig.2 Pulmonary artery remodeling in each group. A: HE staining of pulmonary arteries in each group (scale bar=10 μm). B: Pulmonary artery smooth muscle to total vascular area ratio in each group. C: Percentage of pulmonary artery wall thickness to vessel diameter in each group. D: Immunofluorescence staining of pulmonary artery smooth muscle in each group (scale bar=6 μm). E: Relative fluorescence intensity of α-SMA in each group. Data are presented as Mean±SD (n=6). **P<0.01 vs control group; #P<0.05, ##P<0.01 vs hypoxia group.
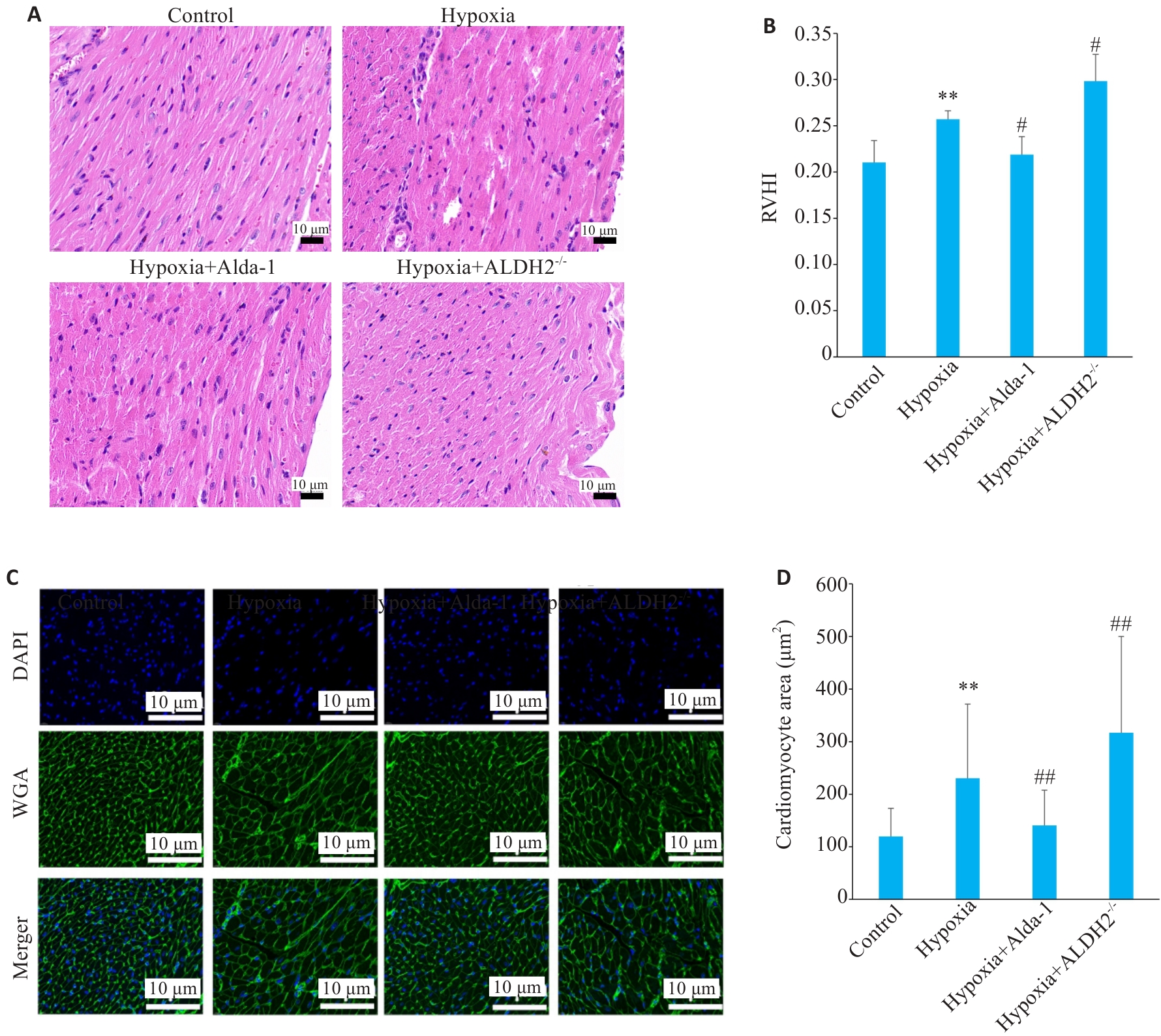
Fig.3 Right ventricular remodeling in each group. A: HE staining of the right ventricle in each group. B: Right ventricular cardiac hypertrophy index of each group. C: WGA staining of the right ventricle in each group. D: Cross-sectional area of mouse cardiomyocytes in each group. Data are presented as Mean±SD (n=6). **P<0.01 vs control group; #P<0.05, ##P<0.01 vs hypoxia group.
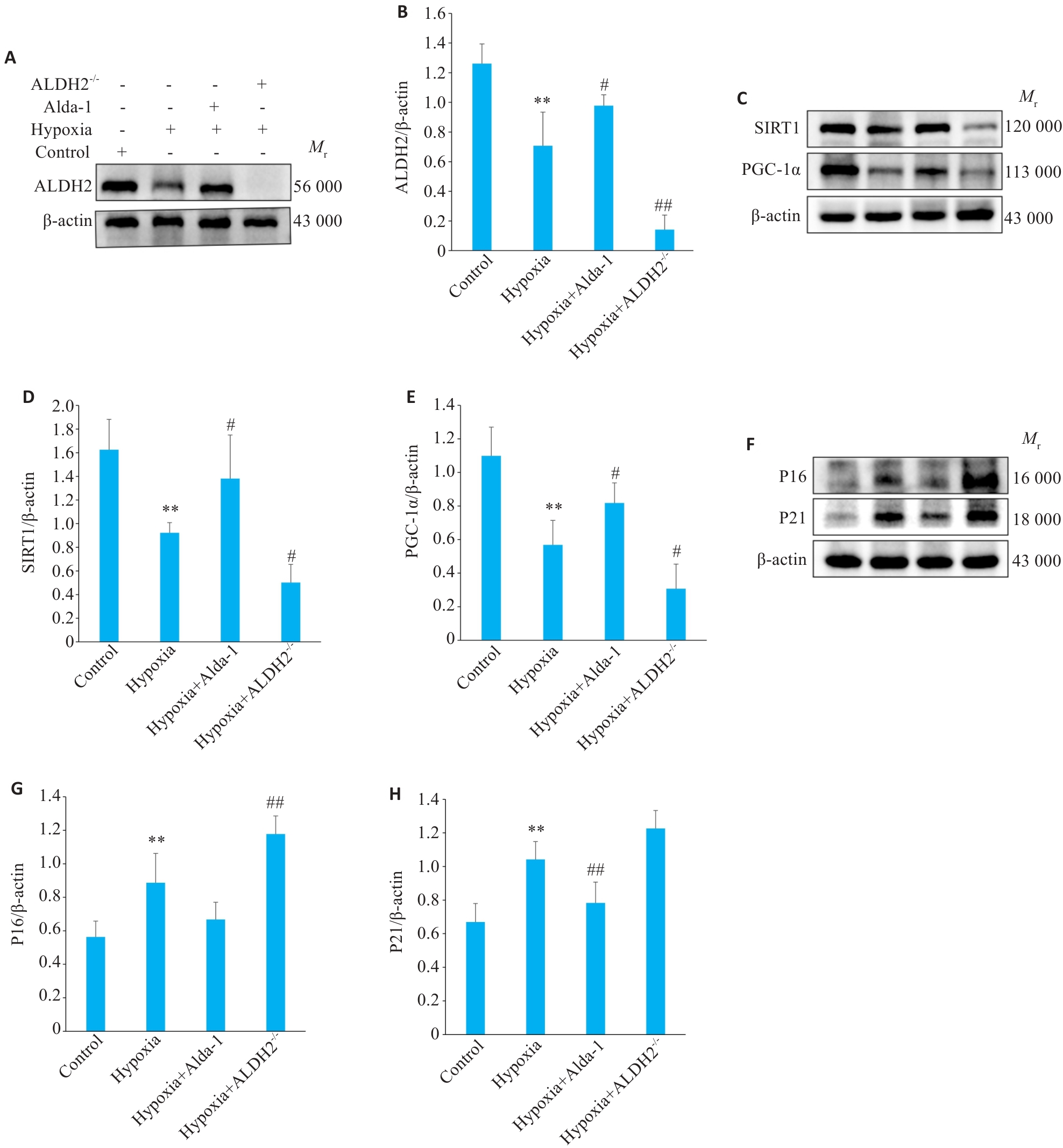
Fig.4 Wetsern blotting for detecting protein expressions of ALDH2, SIRT1, PGC-1α, P16INK4A and P21CIP1 in the lung tissues in each group. A, B: Western blots of ALDH2 protein and its relative expression levels. C-E: Western blots of SIRT1 and PGC-1α proteins and their relative expression levels. F-H: Western blots of P16INK4A and P21CIP1 and their relative protein expression levels. Data are presented as Mean±SD (n=6). **P<0.01 vs control group; #P<0.05, ##P<0.01 vs hypoxia group.
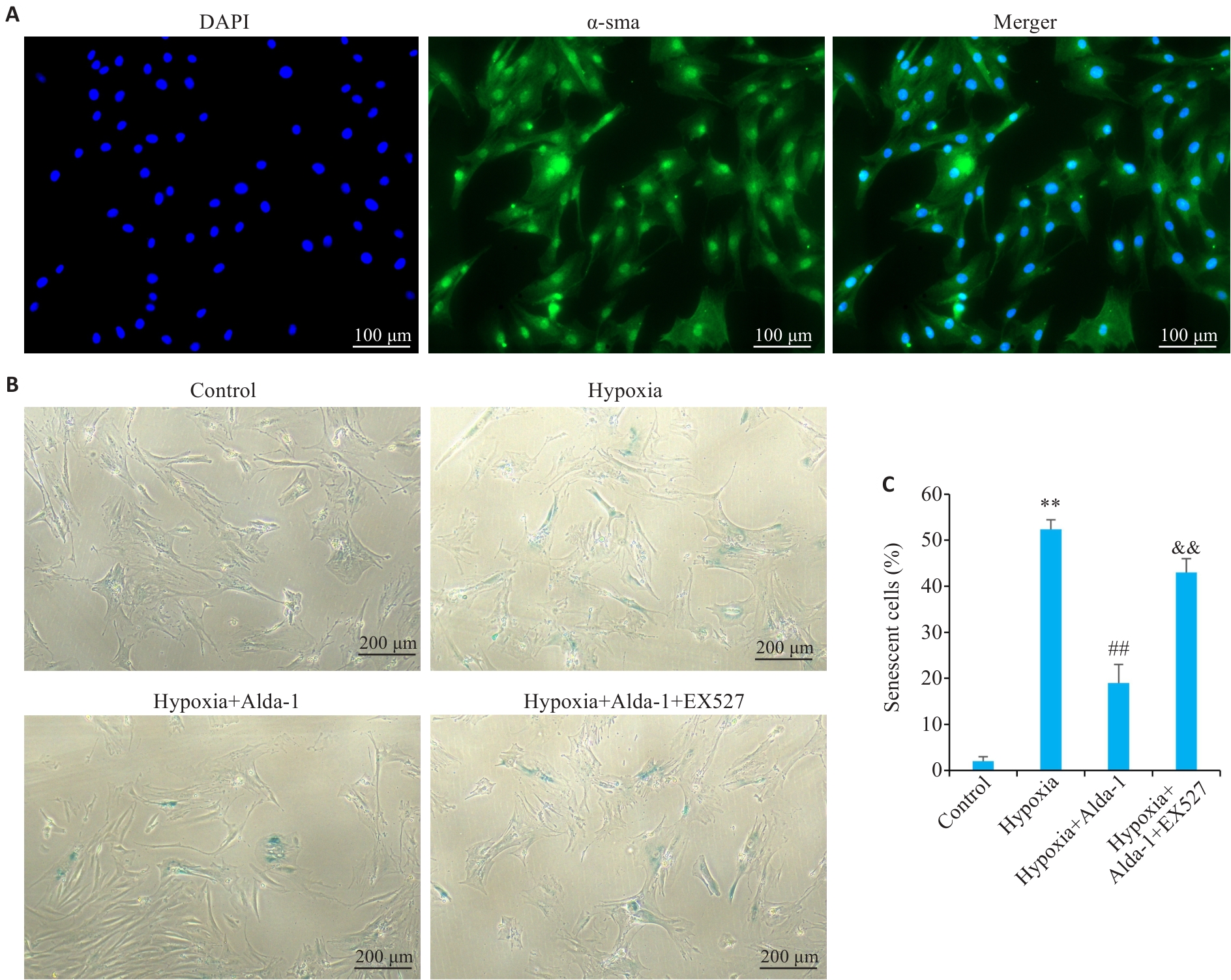
Fig.5 Protective effect of ALDH2 against pulmonary artery smooth muscle cell senescence mediated by the SIRT1 pathway. A: Immunofluorescence staining for α-SMA for identification of mouse pulmonary artery smooth muscle cells. B: β-galactose staining of pulmonary artery smooth muscle cells in each group. C: Percentage of senescent cells in each group. Data are presented as Mean±SD (n=3). **P<0.01 vs control group; ##P<0.01 vs hypoxia group; &&P<0.01 vs Hypoxia+Alda-1 group.
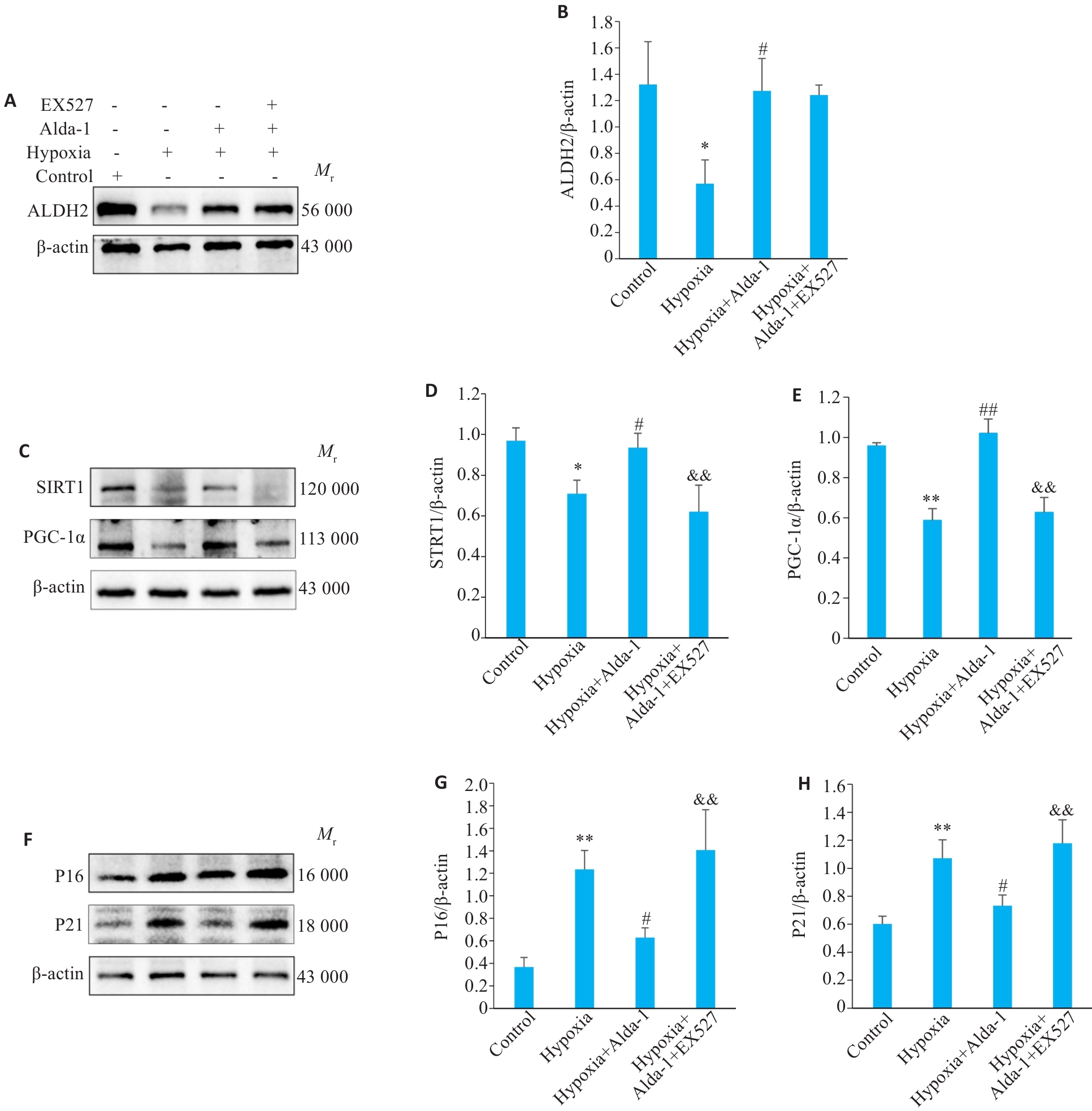
Fig.6 Protein expressions of ALDH2, SIRT1, PGC-1α, P16INK4A and P21CIP1 in mouse pulmonary artery smooth muscle cells in each group. A, B: Western blots of ALDH2 protien and its relative expression levels. C-E: Western blots of SIRT1 and PGC-1α proteins and their relative expression levels. F-H: Western blots of P16INK4A and P21CIP1 proteins and their relative expression levels. Data are presented as Mean±SD (n=3). *P<0.05, **P<0.01 vs control group; #P<0.05, ##P<0.01 vs Hypoxia group; &&P<0.01 vs Hypoxia+Alda-1 group.
| 1 | Rabinovitch M. Molecular pathogenesis of pulmonary arterial hypertension[J]. J Clin Invest, 2012, 122(12): 4306-13. |
| 2 | Simonneau G, Montani D, Celermajer DS, et al. Haemodynamic definitions and updated clinical classification of pulmonary hypertension[J]. Eur Respir J, 2019, 53(1): 1801913. |
| 3 | Sitbon O, Gomberg-Maitland M, Granton J, et al. Clinical trial design and new therapies for pulmonary arterial hypertension[J]. Eur Respir J, 2019, 53(1): 1801908. |
| 4 | Liu LM, Wei YQ, Giunta S, et al. Potential role of cellular senescence in pulmonary arterial hypertension[J]. Clin Exp Pharmacol Physiol, 2022, 49(10): 1042-9. |
| 5 | Semen KO, Bast A. Senescence in pulmonary arterial hypertension: is there a link?[J]. Curr Opin Pulm Med, 2022, 28(4): 303-6. |
| 6 | Noureddine H, Gary-Bobo G, Alifano M, et al. Pulmonary artery smooth muscle cell senescence is a pathogenic mechanism for pulmonary hypertension in chronic lung disease[J]. Circ Res, 2011, 109(5): 543-53. |
| 7 | Wang AP, Yang F, Tian Y, et al. Pulmonary artery smooth muscle cell senescence promotes the proliferation of PASMCs by paracrine IL-6 in hypoxia-induced pulmonary hypertension[J]. Front Physiol, 2021, 12: 656139. |
| 8 | Xia Y, Zhang X, An P, et al. Mitochondrial homeostasis in VSMCs as a central hub in vascular remodeling[J]. Int J Mol Sci, 2023, 24(4): 3483. |
| 9 | Zurlo G, Piquereau J, Moulin M, et al. Sirtuin 1 regulates pulmonary artery smooth muscle cell proliferation: role in pulmonary arterial hypertension[J]. J Hypertens, 2018, 36(5): 1164-77. |
| 10 | Jin JY, Chen JY, Wang YP. Aldehyde dehydrogenase 2 and arrhythmogenesis[J]. Heart Rhythm, 2022, 19(9): 1541-7. |
| 11 | Zhu WZ, Feng DC, Shi X, et al. The potential role of mitochondrial acetaldehyde dehydrogenase 2 in urological cancers from the perspective of ferroptosis and cellular senescence[J]. Front Cell Dev Biol, 2022, 10: 850145. |
| 12 | Zhu H, Wang Z, Dong Z, et al. Aldehyde dehydrogenase 2 deficiency promotes atherosclerotic plaque instability through accelerating mitochondrial ROS-mediated vascular smooth muscle cell senescence[J]. Biochim Biophys Acta Mol Basis Dis, 2019, 1865(7): 1782-92. |
| 13 | Xu T, Liu SY, Ma TT, et al. Aldehyde dehydrogenase 2 protects against oxidative stress associated with pulmonary arterial hypertension[J]. Redox Biol, 2017, 11: 286-96. |
| 14 | Liu HR, Hu Q, Ren K, et al. ALDH2 mitigates LPS-induced cardiac dysfunction, inflammation, and apoptosis through the cGAS/STING pathway[J]. Mol Med, 2023, 29(1): 171. |
| 15 | Li D, Shao NY, Moonen JR, et al. ALDH1A3 coordinates metabolism with gene regulation in pulmonary arterial hypertension[J]. Circulation, 2021, 143(21): 2074-90. |
| 16 | Qin ZR, Fang XW, Sun WH, et al. Deactylation by SIRT1 enables liquid-liquid phase separation of IRF3/IRF7 in innate antiviral immunity[J]. Nat Immunol, 2022, 23(8): 1193-207. |
| 17 | van der Feen DE, Berger RMF, Bartelds B. Converging paths of pulmonary arterial hypertension and cellular senescence[J]. Am J Respir Cell Mol Biol, 2019, 61(1): 11-20. |
| 18 | Stacher E, Graham BB, Hunt JM, et al. Modern age pathology of pulmonary arterial hypertension[J]. Am J Respir Crit Care Med, 2012, 186(3): 261-72. |
| 19 | van der Feen DE, Bossers GPL, Hagdorn QAJ, et al. Cellular senescence impairs the reversibility of pulmonary arterial hypertension[J]. Sci Transl Med, 2020, 12(554): eaaw4974. |
| 20 | Roger L, Tomas F, Gire V. Mechanisms and regulation of cellular senescence[J]. Int J Mol Sci, 2021, 22(23): 13173. |
| 21 | Tan X, Chen YF, Zou SY, et al. ALDH2 attenuates ischemia and reperfusion injury through regulation of mitochondrial fusion and fission by PI3K/AKT/mTOR pathway in diabetic cardiomyopathy[J]. Free Radic Biol Med, 2023, 195: 219-30. |
| 22 | Zhang YM, Zou RJ, Abudureyimu M, et al. Mitochondrial aldehyde dehydrogenase rescues against diabetic cardiomyopathy through GSK3β-mediated preservation of mitochondrial integrity and Parkin-mediated mitophagy[J]. J Mol Cell Biol, 2024, 15(9): mjad056. |
| 23 | 李小荣, 鲜 维, 谭 鑫, 等. 线粒体ALDH2通过调控自噬对缺氧性肺动脉高压的保护机制研究[J]. 蚌埠医学院学报, 2023, 48(1): 66-71. |
| 24 | Masson B, Le Ribeuz H, Sabourin J, et al. Orai1 inhibitors as potential treatments for pulmonary arterial hypertension[J]. Circ Res, 2022, 131(9): e102-19. |
| 25 | Al-Qazazi R, Lima PDA, Prisco SZ, et al. Macrophage-NLRP3 activation promotes right ventricle failure in pulmonary arterial hypertension[J]. Am J Respir Crit Care Med, 2022, 206(5): 608-24. |
| 26 | Veith C, Vartürk-Özcan I, Wujak M, et al. SPARC, a novel regulator of vascular cell function in pulmonary hypertension[J]. Circulation, 2022, 145(12): 916-33. |
| 27 | Neurohr GE, Terry RL, Lengefeld J, et al. Excessive cell growth causes cytoplasm dilution and contributes to senescence[J]. Cell, 2019, 176(5): 1083-97. e18. |
| 28 | Park CS, Kim SH, Yang HY, et al. Sox17 deficiency promotes pulmonary arterial hypertension via HGF/c-met signaling[J]. Circ Res, 2022, 131(10): 792-806. |
| 29 | Zhang J, Guo YY, Zhao XK, et al. The role of aldehyde dehydrogenase 2 in cardiovascular disease[J]. Nat Rev Cardiol, 2023, 20(7): 495-509. |
| 30 | Chang SC, Wu J, Jin JF, et al. Aldehyde dehydrogenase 2 (ALDH2) elicits protection against pulmonary hypertension via inhibition of ERK1/2-mediated autophagy[J]. Oxid Med Cell Longev,2022: 2555476. |
| 31 | Zhao Y, Wang BL, Zhang J, et al. ALDH2 (aldehyde dehydrogenase 2) protects against hypoxia-induced pulmonary hypertension[J]. Arterioscler Thromb Vasc Biol, 2019, 39(11): 2303-19. |
| 32 | Shahgaldi S, Kahmini FR. A comprehensive review of Sirtuins: with a major focus on redox homeostasis and metabolism[J]. Life Sci, 2021, 282: 119803. |
| 33 | Bost F, Kaminski L. The metabolic modulator PGC-1α in cancer[J]. Am J Cancer Res, 2019, 9(2): 198-211. |
| 34 | Kong SF, Cai BL, Nie QH. PGC-1α affects skeletal muscle and adipose tissue development by regulating mitochondrial biogenesis[J]. Mol Genet Genomics, 2022, 297(3): 621-33. |
| 35 | Abu Shelbayeh O, Arroum T, Morris S, et al. PGC-1α is a master regulator of mitochondrial lifecycle and ROS stress response[J]. Antioxidants, 2023, 12(5): 1075. |
| 36 | Singh V, Ubaid S. Role of silent information regulator 1 (SIRT1) in regulating oxidative stress and inflammation[J]. Inflammation, 2020, 43(5): 1589-98. |
| 37 | Teng WL, Huang PH, Wang HC, et al. Pterostilbene attenuates particulate matter-induced oxidative stress, inflammation and aging in keratinocytes[J]. Antioxidants, 2021, 10(10): 1552. |
| [1] | Hongzhe WANG, Haitang XIE, Wulan XU, Ming Li. Urolithin A alleviates respiratory syncytial virus-induced lung infection in neonatal mice by activating miR-136-mediated Sirt1 signaling [J]. Journal of Southern Medical University, 2024, 44(7): 1370-1381. |
| [2] | ZHOU Fengmin, GUO Yanju, CHEN Ning. Exercise promotes irisin expression to ameliorate renal injury in type 2 diabetic rats [J]. Journal of Southern Medical University, 2024, 44(4): 675-681. |
| [3] | YE Hongwei, ZHANG Yuming, YUN Qi, DU Ruoli, LI Lu, LI Yuping, GAO Qin. Resveratrol alleviates hyperglycemia-induced cardiomyocyte hypertrophy by maintaining mitochondrial homeostasis via enhancing SIRT1 expression [J]. Journal of Southern Medical University, 2024, 44(1): 45-51. |
| [4] | XIN Chen, WANG Xiaoying, LI Xiang, CHEN Yu, WANG Xue, NING Jiaxi, YANG Shi, WANG Zhongqiong. LncRNA SOX2OT enhances 5-fluorouracil resistance of cholangiocarcinoma cells by promoting autophagy via up-regulating SIRT1 expression [J]. Journal of Southern Medical University, 2024, 44(1): 187-193. |
| [5] | GUO Jingjing, ZHANG Wenlong, LIANG Piao, ZHANG Longjun, PENG Lingyin, MIN Yuqi, PAN Xiaozhen, YANG Zhiying, DENG Huafei. Puerarin alleviates lipopolysaccharide-induced acute kidney injury in mice by modulating the SIRT1/NF-κB pathway [J]. Journal of Southern Medical University, 2023, 43(7): 1248-1253. |
| [6] | XIN Chen, WANG Xiaoying, LI Xiang, CHEN Yu, WANG Xue, NING Jiaxi, YANG Shi, WANG Zhongqiong. Silencing SIRT1 reduces 5-fluorouracil resistance of cholangiocarcinoma cells by inhibiting the FOXO1/Rab7 autophagy pathway [J]. Journal of Southern Medical University, 2023, 43(3): 454-459. |
| [7] | WAN Lu, QIAN Yuchi, NI Wenjing, LU Yuxin, LI Wei, PAN Yan, CHEN Weidong. Linagliptin improves diabetic kidney disease in rats by promoting mitochondrial biogenesis through the AMPK/PGC-1α/TFAM pathway [J]. Journal of Southern Medical University, 2023, 43(12): 2053-2060. |
| [8] | ZHANG Ximin, LIU Sijia, SUN Yabin, LI Guofeng. Tanshinone IIA alleviates monocrotaline-induced pulmonary hypertension in rats through the PI3K/Akt-eNOS signaling pathway [J]. Journal of Southern Medical University, 2022, 42(5): 718-723. |
| [9] | WANG Shasha, LÜ Heng, WANG Liya, TIAN Meihui, GAO Jie, LIU Zhongyi, WANG Jiahui, YU Ying. ALDH2 attenuates LPS-induced increase of brain microvascular endothelial cell permeability by promoting fusion and inhibiting fission of the mitochondria [J]. Journal of Southern Medical University, 2022, 42(12): 1882-1888. |
| [10] | QIN Na, HUANG Lin, DONG Rui, LI Fen, TANG Xuheng, ZENG Zhenhua, WANG Xingmin, YANG Hong. Polydatin improves intestinal barrier injury after traumatic brain injury in rats by reducing oxidative stress and inflammatory response via activating SIRT1-mediated deacetylation of SOD2 and HMGB1 [J]. Journal of Southern Medical University, 2022, 42(1): 93-100. |
| [11] | . Angiotensin II inhibits AMPK/SIRT1 pathway by inducing oxidative stress in RAW264.7 macrophages [J]. Journal of Southern Medical University, 2021, 41(3): 384-390. |
| [12] | . Chaihu Guizhi decoction produces antidepressant-like effects via sirt1-p53 signaling pathway [J]. Journal of Southern Medical University, 2021, 41(3): 399-405. |
| [13] | . SIRT1 participates in epithelial-mesenchymal transition of EC-9706 and Eca-109 cells in vitro by regulating Snail expression [J]. Journal of Southern Medical University, 2018, 38(11): 1325-. |
| [14] | . Exendin-4 alleviates diabetic cardiomyopathy in mice by regulating Sirt1/PGC1α [J]. Journal of Southern Medical University, 2018, 38(05): 520-. |
| [15] | . Clinical significance of serum carbohydrate antigen 125 in acute exacerbation of chronic obstructive pulmonary disease [J]. Journal of Southern Medical University, 2016, 36(10): 1386-. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||