In the 1960s, a special lymphadenopathy characterized by fever, polyclonal gammopathy, and neutrophilia was first described. Occurring mostly in childhood and early adulthood, this disease was defined by Rosai and Dorfman in 1969 under the name of sinus histiocytosis with massive lymphadenopathy (SHML) [1]. In the following years, scattered cases were reported to describe extranodal involvement by SHML, including the respiratory tract, visceral organs, skin, bone, central nervous system and the genitourinary system, and these entities were later collectively called Rosai-Dorfman disease (RDD) [2]. RDD has a predilection for lymph nodes and is usually present as nonpainful lymphadenopathy [3]. In 1988, Suster described an unusual RDD that involved only the soft tissue without any lymphadenopathy[4], and later a few cases of RDD were reported presenting with isolated extranodal involvement[5], which is now estimated to occur in more than half of cases[6].
According to the scope of involvement, RDD can be classified into 3 types: the lymph node type with only lymph node involvement (often the cervical lymph nodes, with possible involvement of lymph nodes in other regions); the extranodal type involving multiple extranodal organs (often the head and neck and possible involvement of the limbs and other parts of the trunk); and the mixed type with involvement of both the lymph nodes and extranodal organs [3]. Although massive cervical lymphadenopathy is the hallmark of RDD, the upper respiratory tract is the common site for the extranodal form of this disease.
RDD presenting as isolated extranodal involvement of the larynx is very rare. Of the total of 12 cases retrieved from published literature, only one Chinese case was reported (Tab. 1)[7-18]. Most of these patients were middle-aged without the characteristic features of RDD such as painless cervical lymphadenopathy, fever, or an elevated white cell count, while the presence of laryngeal neoplasms and such symptoms as hoarseness, dyspnea and dysphagia were very common. The clinical diagnosis of RDD is difficult and a definite diagnosis has to rely on histopathological and immunohistochemical evidences. Currently no welldefined treatment guidelines have been available for RDD [3]. Herein we report a rare case of RDD with isolated laryngeal involvement, which needed to be differentiated from a malignant laryngeal tumor. We also reviewed similar cases documented in literature and summarized our experience with the diagnosis and treatment of this disease.
| Table 1 General clinical data, therapy and outcomes of 12 reported cases |
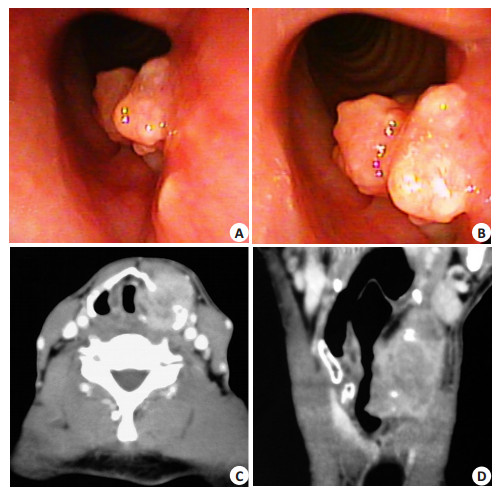
A 51-year-old man was presented to our hospital with the chief complaints of progressive hoarseness for 2 months, and mild dyspnea after activities and anterior neck mass for 1 month. Physical examination revealed a hard, nontender mass measuring 3 cm×4 cm in the neck on the left of the thyroid cartilage. The mass was fixed to the thyroid cartilage without adhesion to the skin. Under laryngoscope, a cauliflower-like neoplasm was observed on the left side of the glottis area, subglottic area and the piriform fossa, and the motion of the left vocal fold was limited (Fig. 1A, B). Computed tomography (CT) scan of the neck showed a 3 cm × 4 cm × 5 cm mass on the left false vocal fold extending to subglottis, causing narrowing of the glottis, subglottic and the left piriform fossa regions. The mass broke through the thyroid cartilage and extended to the cervical collar banding muscles (Fig. 1C, D). Diagnostic hypotheses of laryngeal tuberculosis or squamous cell carcinoma of the left larynx were made based on these findings. Subsequent excisional biopsies under laryngoscopy were performed twice, which showed inflammatory granulation and exudative necrosis without detection of cancer cells.
|
Figure 1 Laryngoscopy showing a cauliflower-like neoplasm located on the left side of the glottis and the subglottic area (A and B). Axial (C) and sagittal (D) enhanced CT showed a mass from the left false vocal fold to the subglottis, breaking through the thyroid cartilage to the anterior cervical muscles. |
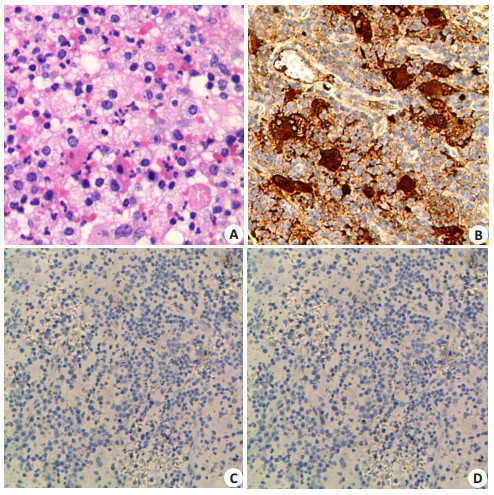
After multidisciplinary case discussion, excision of laryngeal tumor was performed under suspension laryngoscope after tracheotomy. Intraoperative pathological examination reported an inflammatory polyp, for which additional external biopsy of the neck mass was performed. Pathological and immunohistochemical examinations of the surgical specimens showed a fibroadipose tissue mass with extensive infiltration by numerous histiocytes, phagocytosed lymphocytes, plasma cells and occasional neutrophils to support the diagnose of laryngeal RDD. In some areas, lymphophagocytosis by histiocytes (emperipolesis) was found (Fig. 2A). Immunohistochemistry confirmed positivity for S-100 protein and CD68 and negativity for CD1a in RDD cells (Fig. 2).
|
Figure 2 Postoperative pathological examination. Hematoxylin-eosin staining showed histiocytes with foamy cytoplasm and emperipolesis (A), and immunohistochemistry showed that these histiocytes were positive for S-100 protein (B) and CD68 (C) and negative for CD1a (D). |
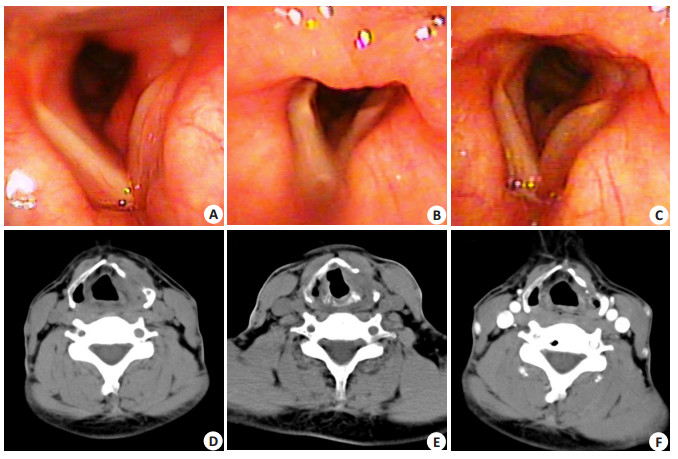
After operation the patient was given steroid therapy with prednilysone at 50 mg/day for two weeks, and the dose was then reduced to 20 mg/day for 2 months. Three months later, the patient reported obvious relief of dyspnea and hoarseness but the neck mass remained unchanged, and he agreed to receive another surgery for resection of the neck mass along with the necrotic thyoid cartilage without opening the laryngeal cavity. The result of pathological examination also confirmed the diagnosis of laryngeal RDD. After the second operation the patient was given prednisone at 10 mg/day for 2 months, and the dose was gradually reduced until discontinuation over a period of 3 weeks. After the treatment, the patient showed satisfactory recovery of the functions of respiration, swallowing and phonation, and laryngoscopic and CT examinations showed that the vocal cords were smooth and mobile. The patient was closely followed up for 2 years, during which no recurrence was found (Fig. 3).
|
Figure 3 Results of follow-up examinations of the patient at 1 month, 3 months, and 24 months after the treatment. Laryngoscope showed that the vocal cords were smooth and mobile (A, B and C). Axial CT showed that the neoplasm had disappeared (D, E and F). A, D: 1 month after treatment; B, E: 3 months after treatment. C, F: 24 months after treatment. |
A differential diagnosis between laryngeal RDD and malignant tumor is difficult by symptoms and imaging findings only, and a definite diagnosis has to be made based on pathological evidence. Laryngoscopic biopsy often fails to obtain a definite diagnosis due to the insufficient amount of tissue specimen collected. In our case, the diagnosis was made only after excision of the mass, and laryngoscopic biopsy for 3 times and an intraoperative frozen section all failed to establish the diagnosis. The histopathological features of extranodal RDD are roughly consistent with those of lymphadenopathy RDD, with heavy infiltration by histiocytes, lymphocytes and plasma cells, and endocytosis of lymphocytes and erythrocytes by histiocytes. But extranodal RDD has more obvious fibrosis with fewer histiocytes and less distinct emperipolesis. The histiocytes of extranodal RDD are immunohistochemically positive for S-100 protein and CD68 and negative for CD1a, which helps in the differential diagnosis from other diseases [3].
According to statistics, RDD are self-limited in more than 20% of the cases and show spontaneous regression without intervention, while 70% of the patients have noticeable symptoms and vital organ involvement to require treatments [19]. The most common treatments include surgery, steroids, radiation and chemotherapy, and surgical excision remains the most effective option for a solitary lesion or lesions of a limited number. In cases of laryngeal RDD with obstructive or compressive symptoms, surgery should be the primary choice of treatment. Glucocorticoid is the first-line therapeutic option for systemic treatment. Most of the patients with RDD, either classical or extranodal, have a favorable response to oral or intravenous glucocorticoid. Radiotherapy and chemotherapy are only considered in cases without surgical indications or with failed glucocorticoid treatment [11, 14]. In the 12 cases reported in literature, 6 received laryngomicrosurgery under suspension laryngoscope, 3 had laryngofissure, and the remaining 3 cases received monotherapy with chemotherapy, radiotherapy, or follow-up observation; steroid therapy as a common treatment for RDD was given in 5 cases. After the treatments, the condition was controlled in all the 12 cases (Tab. 1). Therefore we recommend that microinvasive operation or steroid therapy followed by surgery be the primary choice of treatment once the diagnosis of RDD is established. Microinvasive surgery can quickly relieve such symptoms as hoarseness and dyspnea, and steroid therapy can control the progression and prevent recurrence of the condition. In our case, we performed two microinvasive surgeries inside and outside the larynx with postoperative steroid therapy, and the structure and mucous membrane of the larynx were well preserved. The patient was satisfied with pronunciation during the follow-up period.
ConclusionRDD with isolated laryngeal involvement is a rare benign and self-limited histiocytic disorder mimicking laryngeal malignancy. Biopsy under laryngoscopy often fails to obtain an accurate diagnosis. In such cases, microinvasive surgery with steroid therapy may produce a good long-term outcome. Clinicians should be aware of RDD with isolated laryngeal involvement when performing surgeries for functional damage of the larynx.
Acknowledgement: The authors would like to thank Dr. ZHANG Wei, a pathologist assistant at Guangzhou General Hospital, for reviewing and photographing the biopsy sections.| [1] | Rosai J, Dorfman RF. Sinus histiocytosis with massive lymphadenopathy. A newly recognized benign clinicopathological entity[J]. Arch Pathol, 1969, 87(1): 63-70. |
| [2] | Foucar E, Rosai J, Dorfman R. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease): review of the entity[J]. Semin Diagn Pathol, 1990, 7(1): 19-73. |
| [3] | Dalia S, Sagatys E, Sokol L, et al. Rosai-Dorfman disease: tumor biology, clinical features, pathology, and treatment[J]. Cancer Control, 2014, 21(4): 322-7. DOI: 10.1177/107327481402100408. |
| [4] | Suster S, Cartagena N, Cabello-Inchausti B, et al. Histiocytic lymphophagocytic panniculitis. An unusual extranodal presentation of sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease)[J]. Arch Dermatol, 1988, 124(8): 1246-9. DOI: 10.1001/archderm.1988.01670080058019. |
| [5] | Goodnight JW, Wang MB, Sercarz J A, et al. Extranodal RosaiDorfman disease of the head and neck[J]. Laryngoscope, 1996, 106(1): 253-6. |
| [6] | Mar WA, Yu JH, Knuttinen MG, et al. Rosai-Dorfman disease: manifestations outside of the head and neck[J]. AJR Am J Roentgenol, 2017, 208(4): 721. DOI: 10.2214/AJR.15.15504. |
| [7] | Leighton SE, Gallimore AP. Extranodal sinus histiocytosis with massive lymphadenopathy affecting the subglottis and trachea[J]. Histopathology, 1994, 24(4): 393-4. DOI: 10.1111/his.1994.24.issue-4. |
| [8] | Asrar L, Facharzt EH, Haque I. Rosai-Dorfman disease: presenting as isolated extranodal involvement of larynx[J]. Otolaryngol, 1998, 27(2): 85-6. |
| [9] | Hazarika P, Nayak DR, Balakrishnan R, et al. Rosai-Dorfman disease of the subglottis[J]. Laryngol Otol, 2000, 114(12): 970-3. |
| [10] | Talebi T, Johns MM 3rd, Sequeira J, et al. Rosai-Dorfman disease of the epiglottis[J]. Clin Oncol, 2007, 25(16): 2324-6. DOI: 10.1200/JCO.2006.10.4919. |
| [11] | Tseng YL, Lin YC, Lo CY, et al. Rosai-Dorfman disease of the subglottis diagnosed by ultrasound-guided fine-needle aspiration biopsy: a case report[J]. Clin Ultrasound, 2010, 38(2): 103-6. |
| [12] | Barbalho CE, Vasconcelos DN, Ximenes Filho JA, et al. RosaiDorfman disease as a differential diagnosis in vocal cord ulceration[J]. Braz J Otorhinolaryngol, 2010, 76(6): 795. DOI: 10.1590/S1808-86942010000600021. |
| [13] | Toguri D, Louie AV, Rizkalla K, et al. Radiotherapy for steroidresistant laryngeal Rosai-Dorfman disease[J]. Curr Oncol, 2011, 18(3): 158-62. |
| [14] | Illing EA, Halum SL. Rosai-Dorfman disease with isolated laryngeal involvement[J]. Ear Nose Throat J, 2012, 91(10): 439-40. |
| [15] | Fusconi M, Benincasa AT, Grasso M, et al. Rosai-Dorfman disease in the larynx[J]. Ear Nose Throat J, 2013, 92(6): E66. |
| [16] | Gadde J, Anzilotti K, Liu X, et al. Sinus histiocytosis with massive lymphadenopathy (Rosai-Dorfman disease) of the true vocal cord[J]. Del Med J, 2014, 86(5): 149-52. |
| [17] | Swain SK, Das A, Sahoo S, et al. An unusual presentation of extranodal Rosai-Dorfman disease threatening the airway[J]. Auris Nasus Larynx, 2016, 43(2): 197-9. DOI: 10.1016/j.anl.2015.06.007. |
| [18] | Ma YL, Liang ZP, Xu SE, et al. Rosai-Dorfman disease (RDD) in the paraglottic space: report of a case and review of literature[J]. Int J Clin Exp Pathol, 2015, 8(10): 13532-8. |
| [19] | Lima FB, Barcelos PS, Constâncio AP, et al. Rosai-Dorfman disease with spontaneous resolution: case report of a child[J]. Rev Bras Hematol Hemoter, 2011, 33: 312-4. DOI: 10.5581/1516-8484.20110083. |
 2018, Vol. 38
2018, Vol. 38
