Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (7): 1519-1526.doi: 10.12122/j.issn.1673-4254.2025.07.19
Previous Articles Next Articles
Xinyue CHANG1,2( ), Ningning YAO3, Yan ZHAO1,2, Yinfeng WANG4, Ancong WANG1,2, Huihui ZHANG1,2, Jing ZHANG1,2,5(
), Ningning YAO3, Yan ZHAO1,2, Yinfeng WANG4, Ancong WANG1,2, Huihui ZHANG1,2, Jing ZHANG1,2,5( )
)
Received:2025-05-31
Online:2025-07-20
Published:2025-07-17
Contact:
Jing ZHANG
E-mail:chang_xy@126.com;2253113841@qq.com
Xinyue CHANG, Ningning YAO, Yan ZHAO, Yinfeng WANG, Ancong WANG, Huihui ZHANG, Jing ZHANG. Exogenous triggering with hCG/GnRHa improves outcomes of natural cycle IVF/ICSI in patients with diminished ovarian reserve: a propensity score matching and logistic regression analysis[J]. Journal of Southern Medical University, 2025, 45(7): 1519-1526.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.07.19
| Variable | Endogenous LH group (n=397) | Exogenous trigger group (n=721) | P |
|---|---|---|---|
| Center | 0.1898 | ||
| Linyi people's hospital | 374 (94.21%) | 664 (92.09%) | |
| Heze TCM hospital | 23 (5.79%) | 57 (7.91%) | |
| Age (year) | 40.0 (35.0-42.0) | 40.0 (35.0-43.0) | 0.4998 |
| Age group (years) | 0.9400 | ||
| <35 | 99 (24.94%) | 173 (23.99%) | |
| 35-39 | 95 (23.93%) | 175 (24.27%) | |
| ≥40 | 203 (51.13%) | 373 (51.73%) | |
| Infertility type: Primary | 89 (22.42%) | 159 (22.05%) | 0.8881 |
| Infertility duration (years) | 0.58 (0.25-3.08) | 0.83 (0.25-5.50) | 0.0129 |
| BMI (kg/m²) | 23.43 (21.09-25.64) | 23.70 (21.50-25.71) | 0.0504 |
| Basal FSH (mIU/mL) | 11.26 (7.70-17.14) | 9.47 (7.17-14.40) | 0.0002 |
| Basal LH (mIU/mL) | 4.57 (3.20-6.45) | 3.90 (2.64-5.70) | <0.0001 |
| Basal E₂ (pg/mL) | 42.11 (25.00-67.25) | 46.07 (28.83-69.32) | 0.0271 |
| Basal P (ng/mL) | 0.40 (0.29-0.65) | 0.38 (0.25-0.60) | 0.0307 |
| AFC (n) | 1.50 (1.00-3.00) | 1.50 (1.00-2.50) | 0.7408 |
| Trigger day follicle diameter (mm) | 16.50 (15.00-18.00) | 16.00 (14.50-17.00) | 0.0013 |
| Trigger day E₂ (pg/mL) | 195.10 (148.15-261.24) | 228.56 (187.40-295.66) | <0.0001 |
| Trigger day LH (mIU/mL) | 34.43 (22.61-48.27) | 8.88 (6.17-12.35) | <0.0001 |
| Trigger day P (ng/mL) | 0.83 (0.54-1.11) | 0.37 (0.23-0.59) | <0.0001 |
| Endometrial thickness (mm) | 9.00 (7.50-10.40) | 8.00 (7.00-10.00) | <0.0001 |
Tab.1 Baseline and ovarian stimulation characteristics of the patients
| Variable | Endogenous LH group (n=397) | Exogenous trigger group (n=721) | P |
|---|---|---|---|
| Center | 0.1898 | ||
| Linyi people's hospital | 374 (94.21%) | 664 (92.09%) | |
| Heze TCM hospital | 23 (5.79%) | 57 (7.91%) | |
| Age (year) | 40.0 (35.0-42.0) | 40.0 (35.0-43.0) | 0.4998 |
| Age group (years) | 0.9400 | ||
| <35 | 99 (24.94%) | 173 (23.99%) | |
| 35-39 | 95 (23.93%) | 175 (24.27%) | |
| ≥40 | 203 (51.13%) | 373 (51.73%) | |
| Infertility type: Primary | 89 (22.42%) | 159 (22.05%) | 0.8881 |
| Infertility duration (years) | 0.58 (0.25-3.08) | 0.83 (0.25-5.50) | 0.0129 |
| BMI (kg/m²) | 23.43 (21.09-25.64) | 23.70 (21.50-25.71) | 0.0504 |
| Basal FSH (mIU/mL) | 11.26 (7.70-17.14) | 9.47 (7.17-14.40) | 0.0002 |
| Basal LH (mIU/mL) | 4.57 (3.20-6.45) | 3.90 (2.64-5.70) | <0.0001 |
| Basal E₂ (pg/mL) | 42.11 (25.00-67.25) | 46.07 (28.83-69.32) | 0.0271 |
| Basal P (ng/mL) | 0.40 (0.29-0.65) | 0.38 (0.25-0.60) | 0.0307 |
| AFC (n) | 1.50 (1.00-3.00) | 1.50 (1.00-2.50) | 0.7408 |
| Trigger day follicle diameter (mm) | 16.50 (15.00-18.00) | 16.00 (14.50-17.00) | 0.0013 |
| Trigger day E₂ (pg/mL) | 195.10 (148.15-261.24) | 228.56 (187.40-295.66) | <0.0001 |
| Trigger day LH (mIU/mL) | 34.43 (22.61-48.27) | 8.88 (6.17-12.35) | <0.0001 |
| Trigger day P (ng/mL) | 0.83 (0.54-1.11) | 0.37 (0.23-0.59) | <0.0001 |
| Endometrial thickness (mm) | 9.00 (7.50-10.40) | 8.00 (7.00-10.00) | <0.0001 |
| Variable | Endogenous LH group (n=397) | Exogenous trigger group (n=397) | P |
|---|---|---|---|
| Center | 1.0000 | ||
| Linyi people's hospital | 374 (94.21%) | 374 (94.21%) | |
| Heze TCM hospital | 23 (5.79%) | 23 (5.79%) | |
| Age (year) | 40.0 (35.0-42.0) | 40.0 (34.0-43.0) | 0.5198 |
| Age group (years) | 0.6941 | ||
| <35 | 99 (24.94%) | 101 (25.44%) | |
| 35-39 | 95 (23.93%) | 85 (21.41%) | |
| ≥40 | 203 (51.13%) | 211 (53.15%) | |
| Infertility type: Primary | 89 (22.42%) | 89 (22.42%) | 1.0000 |
| Infertility duration (years) | 0.58 (0.25-3.08) | 0.50 (0.25-3.08) | 0.3843 |
| BMI (kg/m²) | 23.43 (21.09-25.64) | 23.40 (21.10-25.70) | 0.5879 |
| Basal FSH (mIU/mL) | 11.26 (7.70-17.14) | 9.45 (7.10-14.57) | 0.0018 |
| Basal E₂ (pg/mL) | 42.11 (25.00-67.25) | 49.01 (30.43-71.20) | 0.0172 |
| Basal P (ng/mL) | 0.40 (0.29-0.65) | 0.40 (0.26-0.63) | 0.4502 |
| Basal LH (mIU/mL) | 4.57 (3.20-6.45) | 4.07 (2.87-5.81) | 0.0002 |
| AFC (n) | 1.50 (1.00-3.00) | 1.50 (1.00-2.50) | 0.6952 |
| Trigger day follicle diameter (mm) | 16.50 (15.00-18.00) | 16.00 (14.50-17.00) | 0.0030 |
| Trigger day E₂ (pg/mL) | 195.10 (148.15-261.24) | 228.78 (190.10-293.50) | <0.0001 |
| Trigger day LH (mIU/mL) | 34.43 (22.61-48.27) | 9.04 (6.20-12.47) | <0.0001 |
| Trigger day P (ng/mL) | 0.83 (0.54-1.11) | 0.39 (0.24-0.59) | <0.0001 |
| Endometrial thickness (mm) | 9.00 (7.50-10.40) | 8.00 (7.00-10.00) | 0.0036 |
Tab.2 Baseline and ovarian stimulation characteristics after PSM
| Variable | Endogenous LH group (n=397) | Exogenous trigger group (n=397) | P |
|---|---|---|---|
| Center | 1.0000 | ||
| Linyi people's hospital | 374 (94.21%) | 374 (94.21%) | |
| Heze TCM hospital | 23 (5.79%) | 23 (5.79%) | |
| Age (year) | 40.0 (35.0-42.0) | 40.0 (34.0-43.0) | 0.5198 |
| Age group (years) | 0.6941 | ||
| <35 | 99 (24.94%) | 101 (25.44%) | |
| 35-39 | 95 (23.93%) | 85 (21.41%) | |
| ≥40 | 203 (51.13%) | 211 (53.15%) | |
| Infertility type: Primary | 89 (22.42%) | 89 (22.42%) | 1.0000 |
| Infertility duration (years) | 0.58 (0.25-3.08) | 0.50 (0.25-3.08) | 0.3843 |
| BMI (kg/m²) | 23.43 (21.09-25.64) | 23.40 (21.10-25.70) | 0.5879 |
| Basal FSH (mIU/mL) | 11.26 (7.70-17.14) | 9.45 (7.10-14.57) | 0.0018 |
| Basal E₂ (pg/mL) | 42.11 (25.00-67.25) | 49.01 (30.43-71.20) | 0.0172 |
| Basal P (ng/mL) | 0.40 (0.29-0.65) | 0.40 (0.26-0.63) | 0.4502 |
| Basal LH (mIU/mL) | 4.57 (3.20-6.45) | 4.07 (2.87-5.81) | 0.0002 |
| AFC (n) | 1.50 (1.00-3.00) | 1.50 (1.00-2.50) | 0.6952 |
| Trigger day follicle diameter (mm) | 16.50 (15.00-18.00) | 16.00 (14.50-17.00) | 0.0030 |
| Trigger day E₂ (pg/mL) | 195.10 (148.15-261.24) | 228.78 (190.10-293.50) | <0.0001 |
| Trigger day LH (mIU/mL) | 34.43 (22.61-48.27) | 9.04 (6.20-12.47) | <0.0001 |
| Trigger day P (ng/mL) | 0.83 (0.54-1.11) | 0.39 (0.24-0.59) | <0.0001 |
| Endometrial thickness (mm) | 9.00 (7.50-10.40) | 8.00 (7.00-10.00) | 0.0036 |
| Variable | Endogenous LH group (n=397) | Exogenous trigger group (n=397) | P |
|---|---|---|---|
| Oocytes retrieved | 0.0189 | ||
| 0 | 137 (34.51%) | 106 (26.70%) | |
| 1 | 258 (64.99%) | 291 (73.30%) | |
| 2 | 2 (0.50%) | 0 | |
| Fertilization method | 0.0061 | ||
| IVF | 197 (49.62%) | 223 (56.17%) | |
| ICSI | 31 (7.81%) | 46 (11.59%) | |
| 2PN | 101 (25.44%) | 189 (47.61%) | <0.0001 |
| Available embryos | 93 (23.43%) | 186 (46.85%) | <0.0001 |
| High-quality embryos | 44 (11.08%) | 128 (32.24%) | <0.0001 |
| Cycle outcomes | <0.0001 | ||
| Fresh transfer | 45 (11.34%) | 92 (23.17%) | |
| Embryo cryopreservation | 42 (10.58%) | 88 (22.17%) | |
| No available embryos | 287 (72.29%) | 194 (48.87%) | |
| Clinical pregnancy | 9 (2.27%) | 33 (8.31%) | 0.0001 |
| Live birth | 7 (1.76%) | 23 (5.79%) | 0.0029 |
Tab.3 Clinical outcome measures after propensity score matching [n(%)]
| Variable | Endogenous LH group (n=397) | Exogenous trigger group (n=397) | P |
|---|---|---|---|
| Oocytes retrieved | 0.0189 | ||
| 0 | 137 (34.51%) | 106 (26.70%) | |
| 1 | 258 (64.99%) | 291 (73.30%) | |
| 2 | 2 (0.50%) | 0 | |
| Fertilization method | 0.0061 | ||
| IVF | 197 (49.62%) | 223 (56.17%) | |
| ICSI | 31 (7.81%) | 46 (11.59%) | |
| 2PN | 101 (25.44%) | 189 (47.61%) | <0.0001 |
| Available embryos | 93 (23.43%) | 186 (46.85%) | <0.0001 |
| High-quality embryos | 44 (11.08%) | 128 (32.24%) | <0.0001 |
| Cycle outcomes | <0.0001 | ||
| Fresh transfer | 45 (11.34%) | 92 (23.17%) | |
| Embryo cryopreservation | 42 (10.58%) | 88 (22.17%) | |
| No available embryos | 287 (72.29%) | 194 (48.87%) | |
| Clinical pregnancy | 9 (2.27%) | 33 (8.31%) | 0.0001 |
| Live birth | 7 (1.76%) | 23 (5.79%) | 0.0029 |
| Outcome | Factor | Before PSM | After PSM | ||
|---|---|---|---|---|---|
| OR (95%CI) | P | OR (95%CI) | P | ||
| Retrieved Oocyte number | Exogenous trigger (yes vs no) | 2.04 (1.35-3.08) | 0.0008 | 2.42 (1.53-3.83) | 0.0002 |
| Age (<35 vs 35-39 years) | 1.71 (1.13-2.59) | 0.0117 | - | - | |
| Age (≥40 vs 35-39 years) | 1.28 (0.91-1.79) | 0.1568 | - | - | |
| Infertility duration (years) | - | - | 1.08 (1.02-1.16) | 0.0139 | |
| BMI (kg/m²) | 0.96 (0.92-1.00) | 0.0376 | 0.93 (0.88-0.99) | 0.0176 | |
| Basal FSH (mIU/mL) | 0.97 (0.95-0.98) | <0.0001 | 0.97 (0.95-0.98) | 0.0002 | |
| Decision-day LH (mIU/mL) | 1.01 (1.00-1.02) | 0.0154 | 1.02 (1.01-1.03) | 0.0032 | |
| 2PN | Exogenous trigger (Yes vs No) | 2.32 (1.73-3.11) | <0.0001 | 2.65 (1.91-3.67) | <0.0001 |
| Infertility type (secondary vs primary) | 1.86 (1.33-2.59) | 0.0003 | 2.08 (1.38-3.14) | 0.0004 | |
| BMI (kg/m²) | 0.95 (0.91-0.99) | 0.0240 | - | - | |
| Basal FSH (mIU/mL) | 0.98 (0.96-0.99) | 0.0099 | - | - | |
| Available embryos | Exogenous trigger (Yes vs No) | 2.31 (1.72-3.10) | <0.0001 | 2.72 (1.97-3.78) | <0.0001 |
| Infertility type (secondary vs primary) | 1.56 (1.12-2.16) | 0.0077 | 2.01 (1.34-3.03) | 0.0008 | |
| Basal FSH (mIU/mL) | 0.98 (0.96-1.00) | 0.0118 | - | - | |
| High-quality embryos | Exogenous trigger (Yes vs No) | 3.38 (2.32-4.93) | <0.0001 | 3.78 (2.53-5.67) | <0.0001 |
| Age (<35 vs 35-39 years) | 0.81 (0.52-1.26) | 0.3412 | - | - | |
| Age (≥40 vs 35-39 years) | 0.62 (0.43-0.90) | 0.0108 | - | - | |
| Infertility type (secondary vs primary) | 1.73 (1.14-2.64) | 0.0108 | 2.08 (1.26-3.45) | 0.0044 | |
| Clinical pregnancy | Exogenous trigger (Yes vs No) | 2.95 (1.40-6.24) | 0.0045 | 4.13 (1.86-9.18) | 0.0005 |
| Age (<35 vs 35-39 years) | 0.79 (0.40-1.54) | 0.4882 | 1.14 (0.49-2.62) | 0.7618 | |
| Age (≥40 vs 35-39 years) | 0.25 (0.12-0.50) | 0.0001 | 0.16 (0.07-0.39) | <0.0001 | |
| Infertility type (secondary vs primary) | - | - | 3.97 (1.39-11.31) | 0.0098 | |
| Basal E2 (pg/mL) | 1.00 (1.00-1.01) | 0.0006 | 1.00 (1.00-1.01) | 0.0016 | |
| Live birth | Exogenous trigger (Yes vs No) | 2.94 (1.24-7.00) | 0.0146 | 4.11 (1.64-10.32) | 0.0026 |
| Age (<35 vs 35-39 years) | 1.13 (0.52-2.45) | 0.7535 | 1.31 (0.53-3.22) | 0.5636 | |
| Age (≥40 vs 35-39 years) | 0.13 (0.05-0.34) | <0.0001 | 0.08 (0.02-0.27) | <0.0001 | |
| Infertility type (secondary vs primary) | 3.09 (1.20-7.92) | 0.0191 | 5.90 (1.62-21.53) | 0.0072 | |
| Basal E2 (pg/mL) | 1.00 (1.00-1.01) | 0.0005 | 1.00 (1.00-1.01) | 0.0008 | |
Tab.4 Pre-trigger variables and outcome associations via logistic regression
| Outcome | Factor | Before PSM | After PSM | ||
|---|---|---|---|---|---|
| OR (95%CI) | P | OR (95%CI) | P | ||
| Retrieved Oocyte number | Exogenous trigger (yes vs no) | 2.04 (1.35-3.08) | 0.0008 | 2.42 (1.53-3.83) | 0.0002 |
| Age (<35 vs 35-39 years) | 1.71 (1.13-2.59) | 0.0117 | - | - | |
| Age (≥40 vs 35-39 years) | 1.28 (0.91-1.79) | 0.1568 | - | - | |
| Infertility duration (years) | - | - | 1.08 (1.02-1.16) | 0.0139 | |
| BMI (kg/m²) | 0.96 (0.92-1.00) | 0.0376 | 0.93 (0.88-0.99) | 0.0176 | |
| Basal FSH (mIU/mL) | 0.97 (0.95-0.98) | <0.0001 | 0.97 (0.95-0.98) | 0.0002 | |
| Decision-day LH (mIU/mL) | 1.01 (1.00-1.02) | 0.0154 | 1.02 (1.01-1.03) | 0.0032 | |
| 2PN | Exogenous trigger (Yes vs No) | 2.32 (1.73-3.11) | <0.0001 | 2.65 (1.91-3.67) | <0.0001 |
| Infertility type (secondary vs primary) | 1.86 (1.33-2.59) | 0.0003 | 2.08 (1.38-3.14) | 0.0004 | |
| BMI (kg/m²) | 0.95 (0.91-0.99) | 0.0240 | - | - | |
| Basal FSH (mIU/mL) | 0.98 (0.96-0.99) | 0.0099 | - | - | |
| Available embryos | Exogenous trigger (Yes vs No) | 2.31 (1.72-3.10) | <0.0001 | 2.72 (1.97-3.78) | <0.0001 |
| Infertility type (secondary vs primary) | 1.56 (1.12-2.16) | 0.0077 | 2.01 (1.34-3.03) | 0.0008 | |
| Basal FSH (mIU/mL) | 0.98 (0.96-1.00) | 0.0118 | - | - | |
| High-quality embryos | Exogenous trigger (Yes vs No) | 3.38 (2.32-4.93) | <0.0001 | 3.78 (2.53-5.67) | <0.0001 |
| Age (<35 vs 35-39 years) | 0.81 (0.52-1.26) | 0.3412 | - | - | |
| Age (≥40 vs 35-39 years) | 0.62 (0.43-0.90) | 0.0108 | - | - | |
| Infertility type (secondary vs primary) | 1.73 (1.14-2.64) | 0.0108 | 2.08 (1.26-3.45) | 0.0044 | |
| Clinical pregnancy | Exogenous trigger (Yes vs No) | 2.95 (1.40-6.24) | 0.0045 | 4.13 (1.86-9.18) | 0.0005 |
| Age (<35 vs 35-39 years) | 0.79 (0.40-1.54) | 0.4882 | 1.14 (0.49-2.62) | 0.7618 | |
| Age (≥40 vs 35-39 years) | 0.25 (0.12-0.50) | 0.0001 | 0.16 (0.07-0.39) | <0.0001 | |
| Infertility type (secondary vs primary) | - | - | 3.97 (1.39-11.31) | 0.0098 | |
| Basal E2 (pg/mL) | 1.00 (1.00-1.01) | 0.0006 | 1.00 (1.00-1.01) | 0.0016 | |
| Live birth | Exogenous trigger (Yes vs No) | 2.94 (1.24-7.00) | 0.0146 | 4.11 (1.64-10.32) | 0.0026 |
| Age (<35 vs 35-39 years) | 1.13 (0.52-2.45) | 0.7535 | 1.31 (0.53-3.22) | 0.5636 | |
| Age (≥40 vs 35-39 years) | 0.13 (0.05-0.34) | <0.0001 | 0.08 (0.02-0.27) | <0.0001 | |
| Infertility type (secondary vs primary) | 3.09 (1.20-7.92) | 0.0191 | 5.90 (1.62-21.53) | 0.0072 | |
| Basal E2 (pg/mL) | 1.00 (1.00-1.01) | 0.0005 | 1.00 (1.00-1.01) | 0.0008 | |
| Subgroup | Clinical outcome | P | OR (95% CI) |
|---|---|---|---|
| Logistic regression | |||
| Age<35 years | Available embryos | 0.0264 | 1.95 (1.08-3.53) |
| High-quality embryos | 0.0009 | 3.99 (1.76-9.04) | |
| Age 35-39 years | Available embryos | 0.0014 | 2.70 (1.47-4.98) |
| High-quality embryos | 0.0045 | 2.68 (1.36-5.30) | |
| Age≥40 years | 2PN | <0.0001 | 2.55 (1.70-3.81) |
| Available embryos | <0.0001 | 2.45 (1.63-3.68) | |
| High-quality embryos | <0.0001 | 3.37 (1.96-5.79) | |
| PSM analysis | |||
| Age <35 years | Available embryos | 0.0171 | 2.29 (1.16-4.51) |
| High-quality embryos | 0.0011 | 4.38 (1.81-10.60) | |
| Age 35-39 years | Retrieved oocyte number | 0.0274 | 2.17 (1.09-4.32) |
| Available embryos | 0.0013 | 3.24 (1.58-6.64) | |
| High-quality embryos | 0.0046 | 2.97 (1.40-6.32) | |
| Clinical pregnancy | 0.0151 | 5.01 (1.37-18.37) | |
| Live birth | 0.0199 | 6.25 (1.34-29.23) | |
| Age≥40 years | 2PN | <0.0001 | 3.18 (2.02-5.00) |
| Available embryos | <0.0001 | 2.84 (1.82-4.43) | |
| High-quality embryos | <0.0001 | 4.25 (2.38-7.60) | |
Tab.5 Subgroup analysis: Age-stratified effects of exogenous triggering on clinical outcomes
| Subgroup | Clinical outcome | P | OR (95% CI) |
|---|---|---|---|
| Logistic regression | |||
| Age<35 years | Available embryos | 0.0264 | 1.95 (1.08-3.53) |
| High-quality embryos | 0.0009 | 3.99 (1.76-9.04) | |
| Age 35-39 years | Available embryos | 0.0014 | 2.70 (1.47-4.98) |
| High-quality embryos | 0.0045 | 2.68 (1.36-5.30) | |
| Age≥40 years | 2PN | <0.0001 | 2.55 (1.70-3.81) |
| Available embryos | <0.0001 | 2.45 (1.63-3.68) | |
| High-quality embryos | <0.0001 | 3.37 (1.96-5.79) | |
| PSM analysis | |||
| Age <35 years | Available embryos | 0.0171 | 2.29 (1.16-4.51) |
| High-quality embryos | 0.0011 | 4.38 (1.81-10.60) | |
| Age 35-39 years | Retrieved oocyte number | 0.0274 | 2.17 (1.09-4.32) |
| Available embryos | 0.0013 | 3.24 (1.58-6.64) | |
| High-quality embryos | 0.0046 | 2.97 (1.40-6.32) | |
| Clinical pregnancy | 0.0151 | 5.01 (1.37-18.37) | |
| Live birth | 0.0199 | 6.25 (1.34-29.23) | |
| Age≥40 years | 2PN | <0.0001 | 3.18 (2.02-5.00) |
| Available embryos | <0.0001 | 2.84 (1.82-4.43) | |
| High-quality embryos | <0.0001 | 4.25 (2.38-7.60) | |
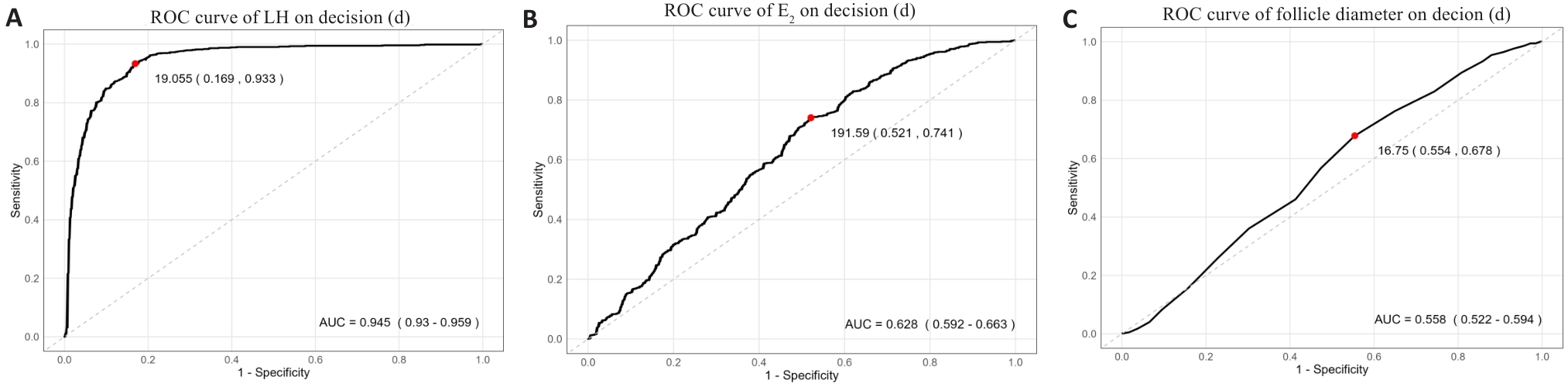
Fig.1 Receiver operating characteristic (ROC) curves of decision-day biomarkers for optimal trigger strategy selection. A: LH levels (AUC=0.945, 95% CI: 0.93-0.959). B: Estradiol (E₂) levels (AUC=0.628, 95% CI: 0.592-0.663). C: Follicle diameter (AUC=0.558, 95% CI: 0.522-0.594). The optimal cutoff values are indicated by red points: 19.055 mIU/mL for LH (sensitivity 93.3%, specificity 93.1%); 191.59 pg/mL for E₂ (sensitivity 74.1%, specificity 47.9%); 16.75 mm for follicle diameter (sensitivity 67.8%, specificity 44.6%). Dashed diagonal lines represent reference (no discrimination; AUC=0.5).
| [1] | Steptoe PC, Edwards RG. Birth after the reimplantation of a human embryo[J]. Lancet, 1978, 312(8085): 366. doi:10.1016/s0140-6736(78)92957-4 |
| [2] | Baker VL, Dyer S, Chambers GM, et al. International committee for monitoring assisted reproductive technologies (ICMART): world report for cycles conducted in 2017-2018[J]. Hum Reprod, 2025, 40(6): 1110-26. doi:10.1093/humrep/deaf049 |
| [3] | Allersma T, Farquhar C, Cantineau AE. Natural cycle in vitro fertilisation (IVF) for subfertile couples[J]. Cochrane Database Syst Rev, 2013(8): CD010550. doi:10.1002/14651858.cd010550.pub2 |
| [4] | von Wolff M. The role of Natural Cycle IVF in assisted reproduction[J]. Best Pract Res Clin Endocrinol Metab, 2019, 33(1): 35-45. doi:10.1016/j.beem.2018.10.005 |
| [5] | Bodri D, Kawachiya S, Kondo M, et al. Oocyte retrieval timing based on spontaneous luteinizing hormone surge during natural cycle in vitro fertilization treatment[J]. Fertil Steril, 2014, 101(4): 1001-7. doi:10.1016/j.fertnstert.2014.01.016 |
| [6] | Tian T, Li Y, Lv J, et al. The potential influence of follicle diameter on natural cycle in vitro fertilization among women with diminished ovarian reserve: a retrospective cohort study[J]. J Ovarian Res, 2023, 16(1): 195. doi:10.1186/s13048-023-01281-4 |
| [7] | Reichman DE, Zakarin L, Chao K, et al. Diminished ovarian reserve is the predominant risk factor for gonadotropin-releasing hormone antagonist failure resulting in breakthrough luteinizing hormone surges in in vitro fertilization cycles[J]. Fertil Steril, 2014, 102(1): 99-102. doi:10.1016/j.fertnstert.2014.04.010 |
| [8] | Lenton EA. Natural cycle IVF with and without terminal HCG: learning from failed cycles[J]. Reprod BioMedicine Online, 2007, 15(2): 149-55. doi:10.1016/S1472-6483(10)60702-X |
| [9] | Gordon JD, DiMattina M, Reh A, et al. Utilization and success rates of unstimulated in vitro fertilization in the United States: an analysis of the Society for Assisted Reproductive Technology database[J]. Fertil Steril, 2013, 100(2): 392-5. doi:10.1016/j.fertnstert.2013.03.037 |
| [10] | Di Guardo F, Blockeel C, De Vos M, et al. Poor ovarian response and the possible role of natural and modified natural cycles[J]. Ther Adv Reprod Health, 2022, 16: 26334941211062026. doi:10.1177/26334941211062026 |
| [11] | Alpha Scientists in Reproductive Medicine and ESHRE Special Interest Group of Embryology. The Istanbul consensus workshop on embryo assessment: proceedings of an expert meeting[J]. Hum Reprod, 2011, 26(6): 1270-83. doi:10.1016/j.rbmo.2011.02.001 |
| [12] | Kochhar PK, Ghosh P. Diminished ovarian reserve predisposes to premature luteinizing hormone surges in gonadotropin-releasing hormone antagonist cycles in In vitro fertilization[J]. J Hum Reprod Sci, 2020, 13(3): 191-5. doi:10.4103/jhrs.jhrs_133_19 |
| [13] | Zhu Q, Li Y, Ma J, et al. Potential factors result in diminished ovarian reserve: a comprehensive review[J]. J Ovarian Res, 2023, 16(1): 208. doi:10.1186/s13048-023-01296-x |
| [14] | Hanson BM, Tao X, Zhan Y, et al. Young women with poor ovarian response exhibit epigenetic age acceleration based on evaluation of white blood cells using a DNA methylation-derived age prediction model[J]. Hum Reprod, 2020, 35(11): 2579-88. doi:10.1093/humrep/deaa206 |
| [15] | Lebovitz O, Haas J, Mor N, et al. Predicting IVF outcome in poor ovarian responders[J]. BMC Womens Health, 2022, 22(1): 395. doi:10.1186/s12905-022-01964-y |
| [16] | Tiwari M, Chaube SK. Human chorionic gonadotropin mediated generation of reactive oxygen species is sufficient to induce meiotic exit but not apoptosis in rat oocytes[J]. Biores Open Access, 2017, 6(1): 110-22. doi:10.1089/biores.2017.0018 |
| [17] | Wang S, He G, Chen M, et al. The role of antioxidant enzymes in the ovaries[J]. Oxid Med Cell Longev, 2017, 2017: 4371714. doi:10.1155/2017/4371714 |
| [18] | Yano S, Ishiuchi T, Abe S, et al. Histone H3K36me2 and H3K36me3 form a chromatin platform essential for DNMT3A-dependent DNA methylation in mouse oocytes[J]. Nat Commun, 2022, 13(1): 4440. doi:10.1038/s41467-022-32141-2 |
| [19] | Uysal F, Sukur G, Bozdemir N, et al. Unveiling the impact of DNA methylation machinery: Dnmt1 and Dnmt3a in orchestrating oocyte development and cellular homeostasis[J]. Genesis, 2024, 62(1): e23579. doi:10.1002/dvg.23579 |
| [20] | Ai J, Jin L, Zheng Y, et al. The morphology of inner cell mass is the strongest predictor of live birth after a frozen-thawed single embryo transfer[J]. Front Endocrinol: Lausanne, 2021, 12: 621221. doi:10.3389/fendo.2021.621221 |
| [21] | von Wolff M, Kollmann Z, Flück CE, et al. Gonadotrophin stimulation for in vitro fertilization significantly alters the hormone milieu in follicular fluid: a comparative study between natural cycle IVF and conventional IVF[J]. Hum Reprod, 2014, 29(5): 1049-57. doi:10.1093/humrep/deu044 |
| [22] | Polyzos NP, Drakopoulos P, Tournaye H. Modified natural cycle IVF for poor ovarian responders: rethink before concluding[J]. Hum Reprod, 2016, 31(1): 221-2. doi:10.1093/humrep/dev272 |
| [23] | Ho JR, Paulson RJ. Modified natural cycle in in vitro fertilization[J]. Fertil Steril, 2017, 108(4): 572-6. doi:10.1016/j.fertnstert.2017.08.021 |
| [24] | Rackow BW, Kliman HJ, Taylor HS. GnRH antagonists may affect endometrial receptivity[J]. Fertil Steril, 2008, 89(5): 1234-9. doi:10.1016/j.fertnstert.2007.04.060 |
| [25] | Orvieto R, Meltzer S, Rabinson J, et al. GnRH agonist versus GnRH antagonist in ovarian stimulation: the role of endometrial receptivity[J]. Fertil Steril, 2008, 90(4): 1294-6. doi:10.1016/j.fertnstert.2007.10.022 |
| [26] | Xu B, Geerts D, Hu S, et al. The depot GnRH agonist protocol improves the live birth rate per fresh embryo transfer cycle, but not the cumulative live birth rate in normal responders: a randomized controlled trial and molecular mechanism study[J]. Hum Reprod, 2020, 35(6): 1306-18. doi:10.1093/humrep/deaa086 |
| [1] | . Association of number and quality of embryos transferred with early pregnancy loss in infertile women at an advanced age undergoing frozen-thawed embryo transfer [J]. Journal of Southern Medical University, 2021, 41(7): 1050-1055. |
| [2] | . Timing of HMG supplementation and clinical outcomes of advanced-age patients with diminished ovarian reserve receiving gonadotropin-releasing hormone antagonist protocol [J]. Journal of Southern Medical University, 2021, 41(3): 412-417. |
| [3] |
.
Effect of spermatozoa from different sources on normal fertilization of oocytes and embryo quality and development in intracytoplasmic sperm injection cycles [J]. Journal of Southern Medical University, 2014, 34(06): 857-. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||