Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (4): 744-750.doi: 10.12122/j.issn.1673-4254.2025.04.09
Previous Articles Next Articles
Xinshun WU1,2( ), Jingcao LI3, Ying LIU3, Renhong QIU3, Henglin WANG2, Rui XYE3, Yang ZHANG3, Shuo LI3, Qiongyin FAN3, Huajin DONG3, Youzhi ZHANG3, Jiangbei CAO4(
), Jingcao LI3, Ying LIU3, Renhong QIU3, Henglin WANG2, Rui XYE3, Yang ZHANG3, Shuo LI3, Qiongyin FAN3, Huajin DONG3, Youzhi ZHANG3, Jiangbei CAO4( )
)
Received:2024-12-30
Online:2025-04-20
Published:2025-04-28
Contact:
Jiangbei CAO
E-mail:185501229@qq.com;caojiangbei@301hospital.com.cn
Supported by:Xinshun WU, Jingcao LI, Ying LIU, Renhong QIU, Henglin WANG, Rui XYE, Yang ZHANG, Shuo LI, Qiongyin FAN, Huajin DONG, Youzhi ZHANG, Jiangbei CAO. Cannabidiol regulates circadian rhythm to improve sleep disorders following general anesthesia in rats[J]. Journal of Southern Medical University, 2025, 45(4): 744-750.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.04.09
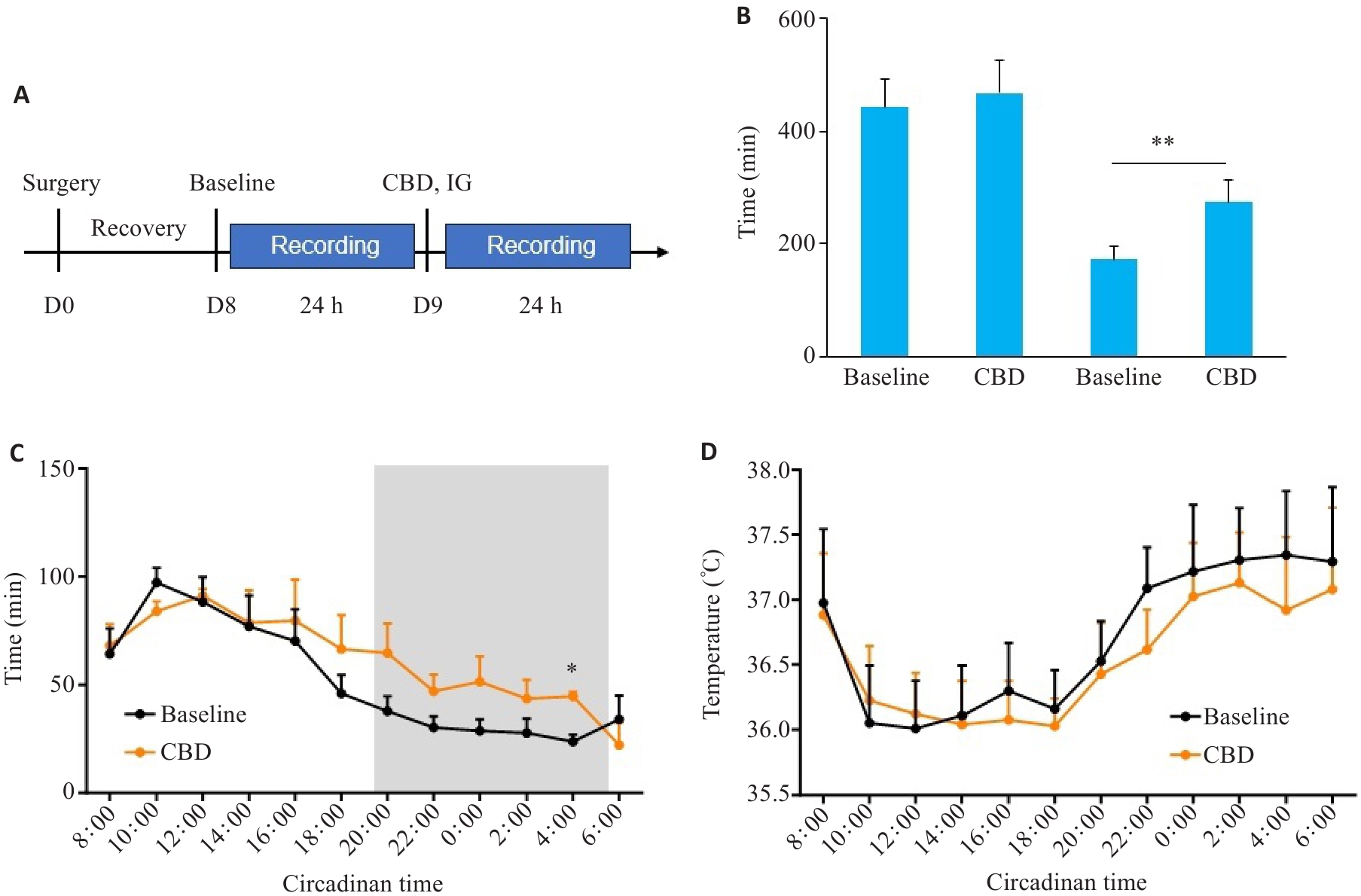
Fig.1 Regulatory effects of CBD on sleep in normal rats. A: Timeline of experiments. B: Sleep duration of the rats in the day time (8:00-18:00) and the night time (20:00-6:00). C: Sleep duration at different time points. D: Average body temperature per hour. CBD: Cannabidiol; IG: Intragastric administration. *P<0.05, **P<0.01 vs baseline.
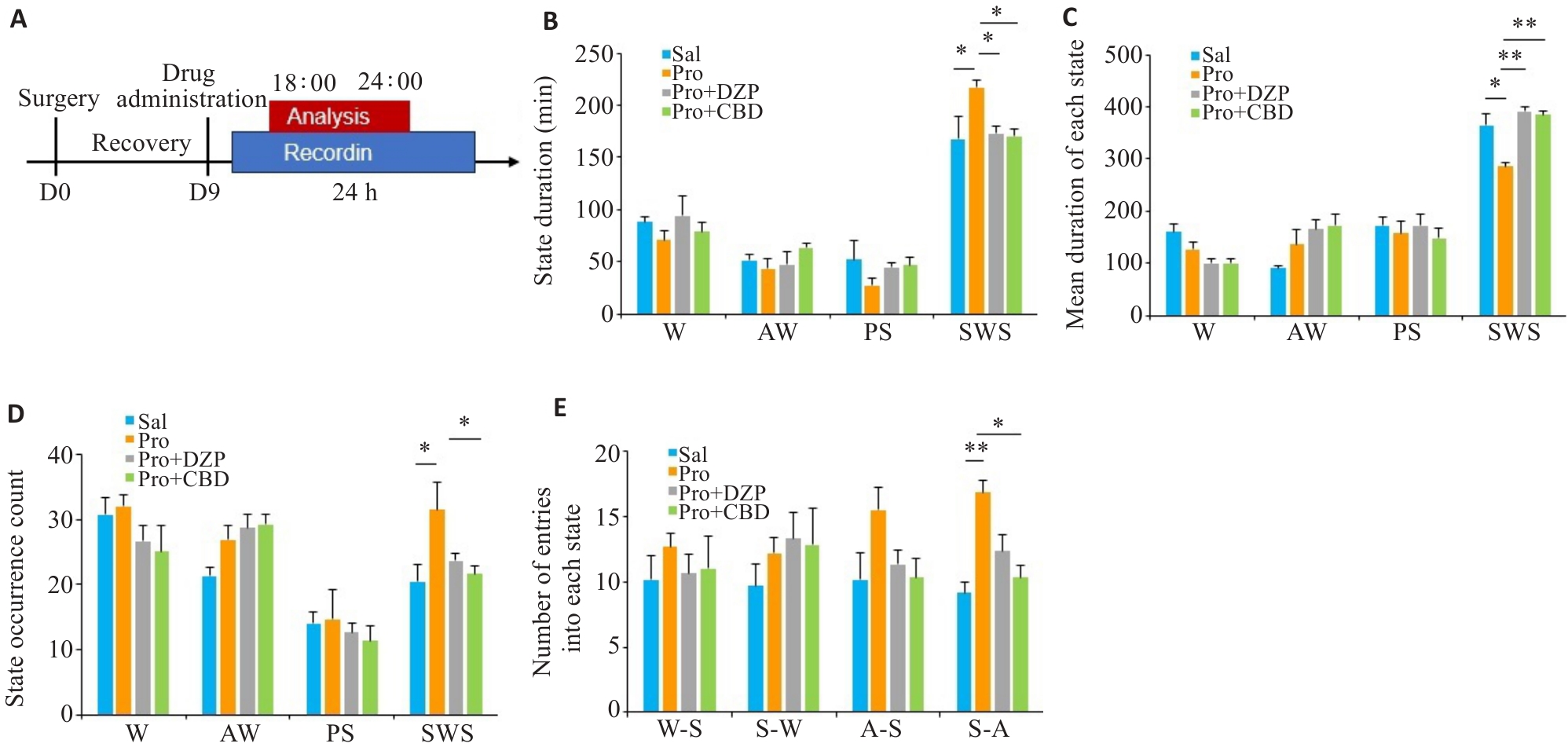
Fig.2 Regulatory effects of CBD on sleep architecture from 18:00 to 24:00 in rats following propofol anesthesia. A: Experimental flowchart. B: Duration of states in different pre-treatment groups. C: Mean duration of each state. D: State occurrence count. E: Number of entries into each state. Pro: Propofol; DZP: Diazepam; CBD: Cannabidiol; W: Wake; AW: Active wake; PS: Paradoxical sleep; SWS: Slow wave sleep. *P<0.05, **P<0.01.
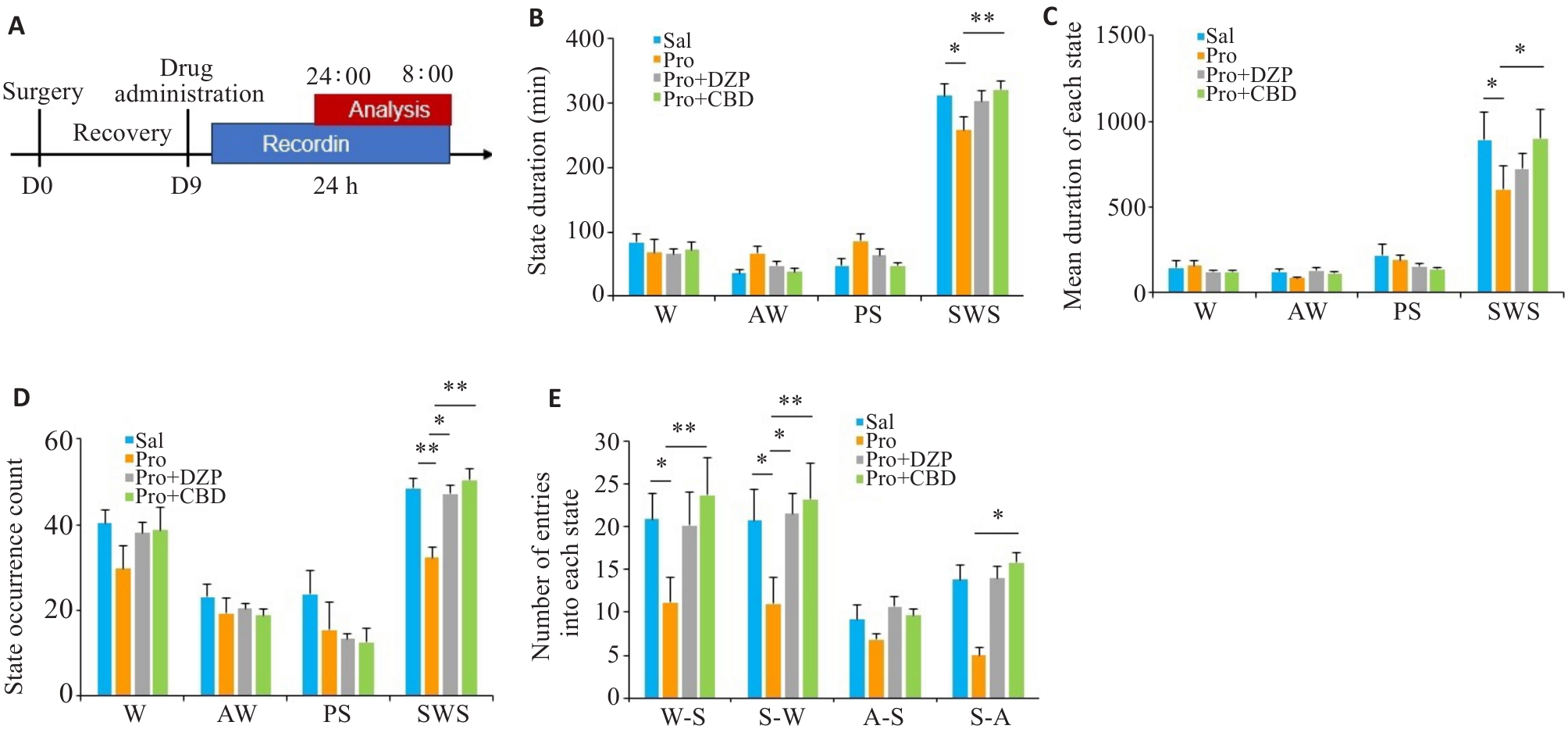
Fig.3 Regulatory effects of CBD on sleep architecture from 24:00 to 08:00 in rats following propofol anesthesia. A: Experimental flowchart. B: Duration of states in different pre-treatment groups. C: Mean duration of each state. D: State occurrence count. E: Number of entries into each state. *P<0.05, **P<0.01.
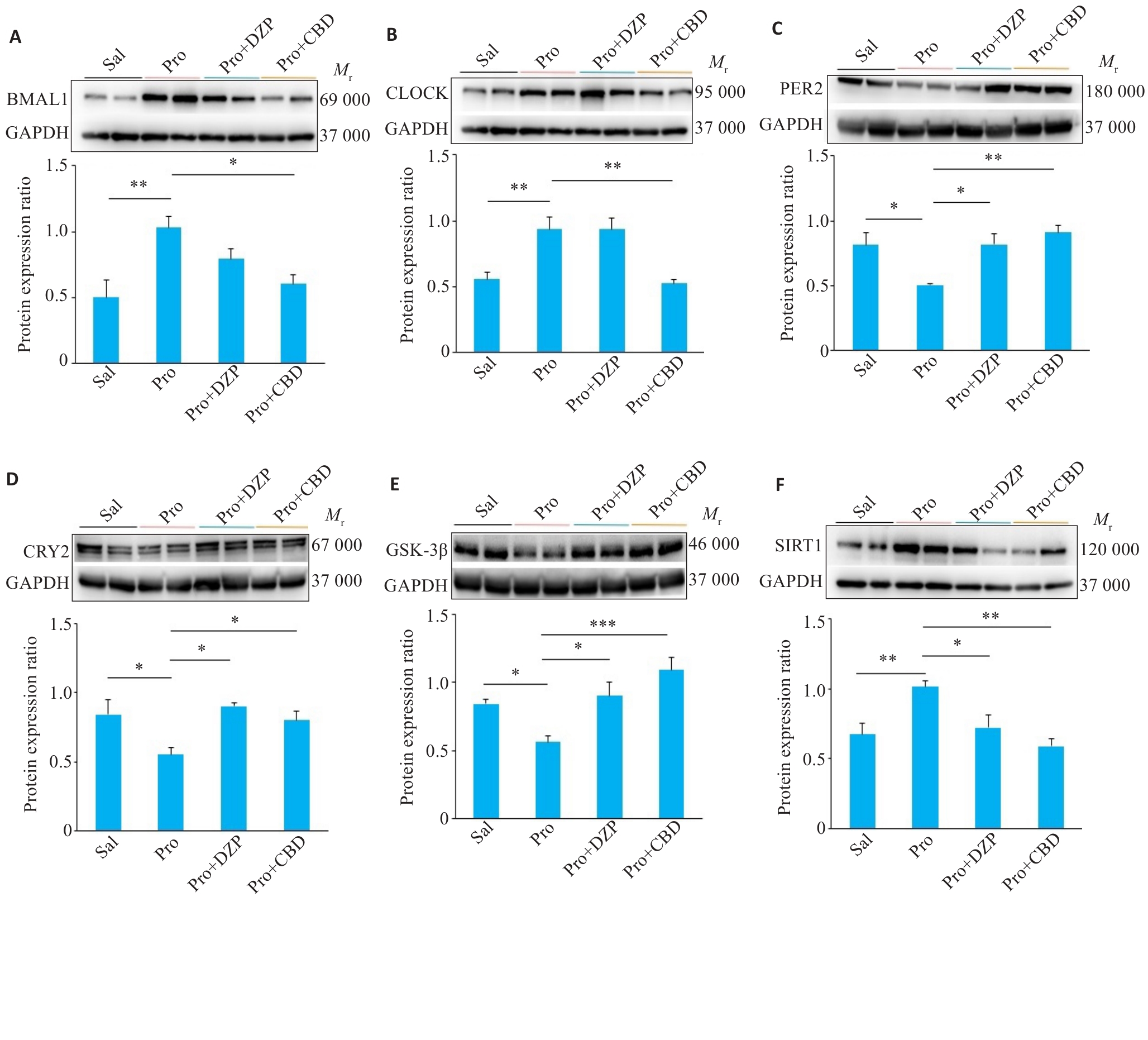
Fig.4 Effects of CBD on expression levels of circadian clock proteins in rats following propofol anesthesia. A-F: Protein expressions of BMAL1, CLOCK, PER2, CRY2, GSK3β and SIRT1 in rat hypothalamus. The expression level of protein was quantified and presented as a ratio relative to GAPDH. *P<0.05, **P<0.01, ***P<0.001.
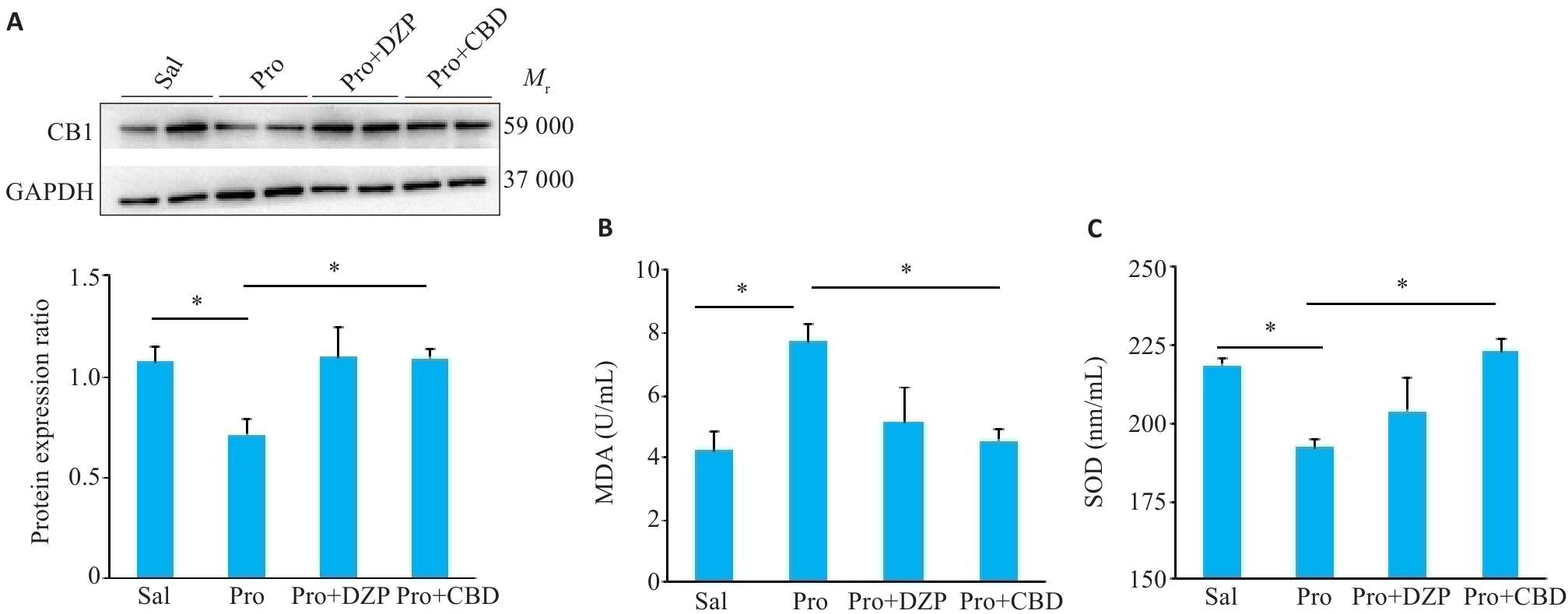
Fig.5 Regulatory effects of CBD on protein expression of CB1 (A) and serum levels of MDA (B) and SOD (C) of the rats. The expression level of protein was quantified and presented as a ratio relative to GAPDH. *P<0.05.
| 1 | Butris N, Tang E, Pivetta B, et al. The prevalence and risk factors of sleep disturbances in surgical patients: a systematic review and meta-analysis[J]. Sleep Med Rev, 2023, 69: 101786. |
| 2 | Öner Ö, Ecevit MC, Gökmen AN. A bibliometric analysis of obstructive sleep apnea and anesthesia[J]. Medicine, 2023, 102(17): e32993. |
| 3 | Lu HF, He F, Huang Y, et al. Different doses of dexmedetomidine reduce postoperative sleep disturbance incidence in patients under general anesthesia by elevating serum neurotransmitter levels[J]. Crit Rev Immunol, 2024, 44(6): 63-73. |
| 4 | van Zuylen ML, Meewisse AG, Ten Hoope W, et al. Effects of surgery and general anaesthesia on sleep-wake timing: CLOCKS observational study[J]. Anaesthesia, 2022, 77(1): 73-81. |
| 5 | Lei M, Zhang P, Liu YF, et al. Propofol and sufentanil may affect the patients' sleep quality independently of the surgical stress response: a prospective nonrandomized controlled trial in 1033 patients' undergone diagnostic upper gastrointestinal endoscopy[J]. BMC Anesthesiol, 2017, 17(1): 53. |
| 6 | Ayuse T, Kurata S, Mishima G, et al. Influence of general anesthesia on the postoperative sleep cycle in patients undergoing surgery and dental treatment: a scoping review on the incidence of postoperative sleep disturbance[J]. J Dent Anesth Pain Med, 2023, 23(2): 59-67. |
| 7 | 刘 影, 李劲草, 薛 瑞, 等. 大麻二酚配伍褪黑素改善大、小鼠失眠和昼夜节律紊乱作用及机制[J]. 中国药理学与毒理学杂志, 2023, 37(2): 81-90. DOI: 10.3867/j.issn.1000-3002.2023.02.001 |
| 8 | Smith MT, Haythornthwaite JA. How do sleep disturbance and chronic pain inter-relate? Insights from the longitudinal and cognitive-behavioral clinical trials literature[J]. Sleep Med Rev, 2004, 8(2): 119-32. |
| 9 | Smegal LF, Vedmurthy P, Ryan M, et al. Cannabidiol treatment for neurological, cognitive, and psychiatric symptoms in sturge-weber syndrome[J]. Pediatr Neurol, 2023, 139: 24-34. |
| 10 | Patke A, Young MW, Axelrod S. Molecular mechanisms and physiological importance of circadian rhythms[J]. Nat Rev Mol Cell Biol, 2020, 21(2): 67-84. |
| 11 | Clarkson SJ, Yayac MF, Rondon AJ, et al. Melatonin does not improve sleep quality in a randomized placebo-controlled trial after primary total joint arthroplasty[J]. J Am Acad Orthop Surg, 2022, 30(2): e287-94. |
| 12 | Anderson LL, Hawkins NA, Yip KL, et al. Preclinical evidence for a drug-drug interaction between cannabinol and melatonin[J]. Basic Clin Pharmacol Toxicol, 2025, 136(1): e14120. |
| 13 | Kirkland AE, Fadus MC, Gruber SA, et al. A scoping review of the use of cannabidiol in psychiatric disorders[J]. Psychiatry Res, 2022, 308: 114347. |
| 14 | Koch M, Dehghani F, Habazettl I, et al. Cannabinoids attenuate norepinephrine-induced melatonin biosynthesis in the rat pineal gland by reducing arylalkylamine N-acetyltransferase activity without involvement of cannabinoid receptors[J]. J Neurochem, 2006, 98(1): 267-78. |
| 15 | Korf HW. Photoneuroendocrine, circadian and seasonal systems: from photoneuroendocrinology to circadian biology and medicine[J]. Cell Tissue Res, 2024, Online ahead of print. |
| 16 | Dispersyn G, Pain L, Touitou Y. Propofol anesthesia significantly alters plasma blood levels of melatonin in rats[J]. Anesthesiology, 2010, 112(2): 333-7. |
| 17 | Rosenblum Y, Bogdány T, Nádasy LB, et al. Aperiodic neural activity distinguishes between phasic and tonic REM sleep[J]. J Sleep Res, 2024: e14439. |
| 18 | Kharas N, Chelaru MI, Eagleman S, et al. NREM sleep improves behavioral performance by desynchronizing cortical circuits[J]. Science, 2024, 386(6724): 892-7. |
| 19 | Challet E, Gourmelen S, Pevet P, et al. Reciprocal relationships between general (Propofol) anesthesia and circadian time in rats[J]. Neuropsychopharmacology, 2007, 32(3): 728-35. |
| 20 | Lee RD, Larson O, Dhaliwal S, et al. Comparative analysis of sleep physiology using qualitative and quantitative criteria for insomnia symptoms[J]. Sleep, 2024: zsae301. |
| 21 | Cankar N, Beschorner N, Tsopanidou A, et al. Sleep deprivation leads to non-adaptive alterations in sleep microarchitecture and amyloid-β accumulation in a murine Alzheimer model[J]. Cell Rep, 2024, 43(11): 114977. |
| 22 | Scott AJ, Webb TL, Martyn-St James M, et al. Improving sleep quality leads to better mental health: a meta-analysis of randomised controlled trials[J]. Sleep Med Rev, 2021, 60: 101556. |
| 23 | McCarter SJ, Hagen PT, St Louis EK, et al. Physiological markers of sleep quality: a scoping review[J]. Sleep Med Rev, 2022, 64: 101657. |
| 24 | Pavlova MK, Latreille V. Sleep disorders[J]. Am J Med, 2019, 132(3): 292-9. |
| 25 | Lafaye G, Desterke C, Marulaz L, et al. Cannabidiol affects circadian clock core complex and its regulation in microglia cells[J]. Addict Biol, 2019, 24(5): 921-34. |
| 26 | Uzbay T, Shahzadi A. A comprehensive analysis of propofol abuse and addiction and neuropharmacological aspects: an updated review[J]. Korean J Anesthesiol, 2025, 78(2): 91-104. |
| 27 | Britch SC, Babalonis S, Walsh SL. Cannabidiol: pharmacology and therapeutic targets[J]. Psychopharmacology, 2021, 238(1): 9-28. |
| 28 | San-juan D, Chiappa KH, Cole AJ. Propofol and the electro-encephalogram[J]. Clin Neurophysiol, 2010, 121(7): 998-1006. |
| 29 | Shilovsky GA, Putyatina TS, Morgunova GV, et al. A crosstalk between the biorhythms and gatekeepers of longevity: dual role of glycogen synthase kinase-3[J]. Biochemistry, 2021, 86(4): 433-48. |
| 30 | Li HX, Meng H, Xu M, et al. BMAL1 regulates osteoblast differentiation through mTOR/GSK3β/β-catenin pathway[J]. J Mol Endocrinol, 2023, 70(4): e220181. |
| 31 | Sagredo O, Ruth Pazos M, Satta V, et al. Neuroprotective effects of phytocannabinoid-based medicines in experimental models of Huntington’s disease[J]. J Neurosci Res, 2011, 89(9): 1509-18. |
| 32 | Blando S, Raffaele I, Chiricosta L, et al. Cannabidiol promotes neuronal differentiation using Akt and erk pathways triggered by Cb1 signaling[J]. Molecules, 2022, 27(17): 5644. |
| 33 | Hamelink C, Hampson A, Wink DA, et al. Comparison of cannabidiol, antioxidants, and diuretics in reversing binge ethanol-induced neurotoxicity[J]. J Pharmacol Exp Ther, 2005, 314(2): 780-8. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||