Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (4): 819-828.doi: 10.12122/j.issn.1673-4254.2025.04.17
Fei CHU1( ), Xiaohua CHEN2, Bowen SONG2, Jingjing YANG2, Lugen ZUO2,3(
), Xiaohua CHEN2, Bowen SONG2, Jingjing YANG2, Lugen ZUO2,3( )
)
Received:2025-02-07
Online:2025-04-20
Published:2025-04-28
Contact:
Lugen ZUO
E-mail:fiona1215@aliyun.com;zuolugen@126.com
Supported by:Fei CHU, Xiaohua CHEN, Bowen SONG, Jingjing YANG, Lugen ZUO. Moslosooflavone ameliorates dextran sulfate sodium-induced colitis in mice by suppressing intestinal epithelium apoptosis via inhibiting the PI3K/AKT signaling pathway[J]. Journal of Southern Medical University, 2025, 45(4): 819-828.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.04.17
| Gene | Forward (5'-3') | Reverse (5'-3') |
|---|---|---|
| TNF-α | CAGGCGGTGCCTATGTCTC | CGATCACCCCGAAGTTCAGTAG |
| IL-1β | GAAATGCCACCTTTTGACAGTG | TGGATGCTCTCATCAGGACAG |
| IL-6 | TCTATACCACTTCACAAGTCGGA | GAATTGCCATTGCACAACTCTTT |
| IFN-γ | ACAGCAAGGCGAAAAAGGATG | TGGTGGACCACTCGGATGA |
| GAPDH | TGGCCTTCCGTGTTCCTAC | GAGTTGCTGTTGAAGTCGCA |
Tab.1 Primer sequences for the target gene
| Gene | Forward (5'-3') | Reverse (5'-3') |
|---|---|---|
| TNF-α | CAGGCGGTGCCTATGTCTC | CGATCACCCCGAAGTTCAGTAG |
| IL-1β | GAAATGCCACCTTTTGACAGTG | TGGATGCTCTCATCAGGACAG |
| IL-6 | TCTATACCACTTCACAAGTCGGA | GAATTGCCATTGCACAACTCTTT |
| IFN-γ | ACAGCAAGGCGAAAAAGGATG | TGGTGGACCACTCGGATGA |
| GAPDH | TGGCCTTCCGTGTTCCTAC | GAGTTGCTGTTGAAGTCGCA |
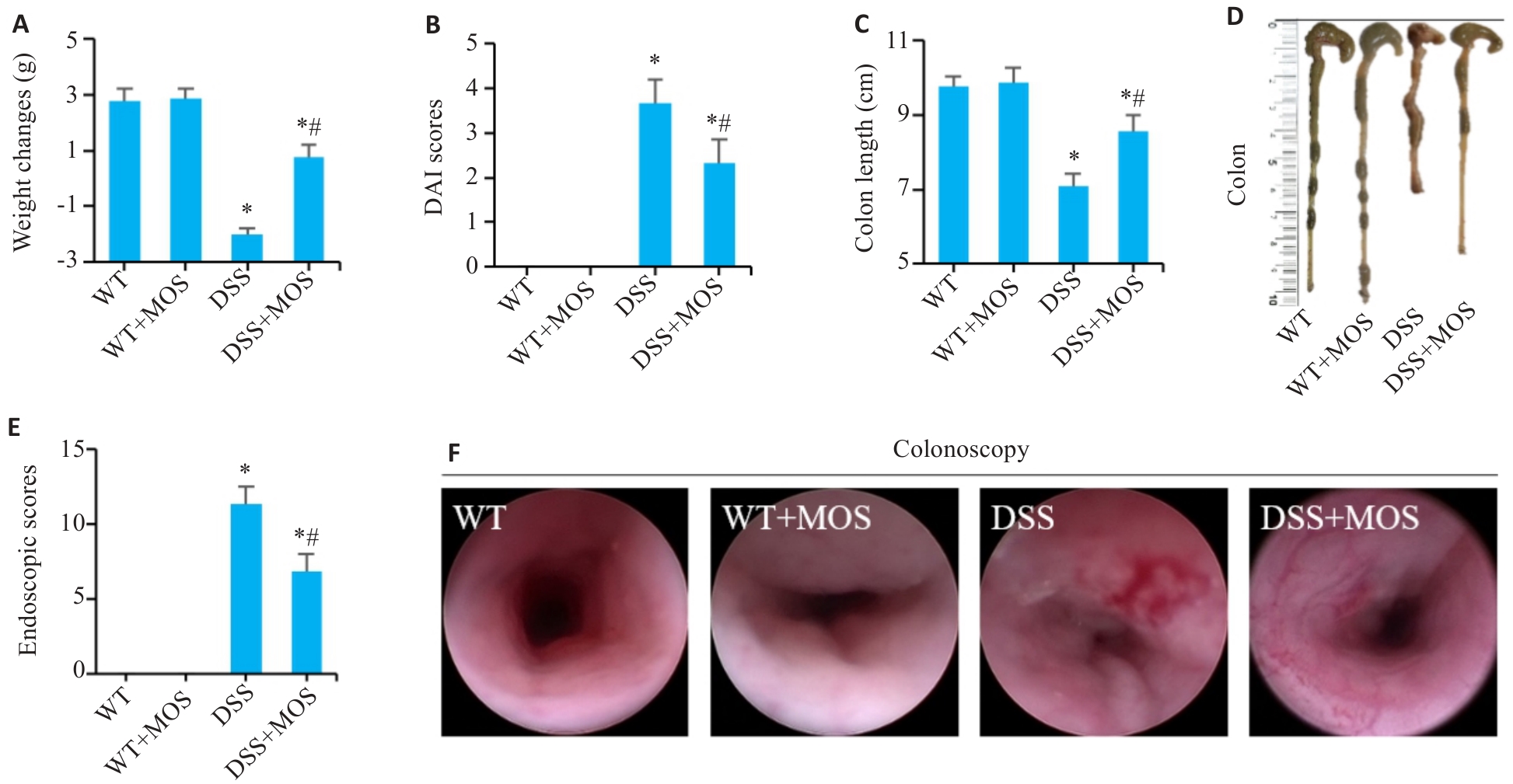
Fig.1 Effect of MOS on symptoms in DSS mice. A: Weight changes. B: DAI scores. C, D: Colon length. E, F: Colonoscopy and endoscopic scores. n=6, *P<0.05 vs WT; #P<0.05 vs DSS.
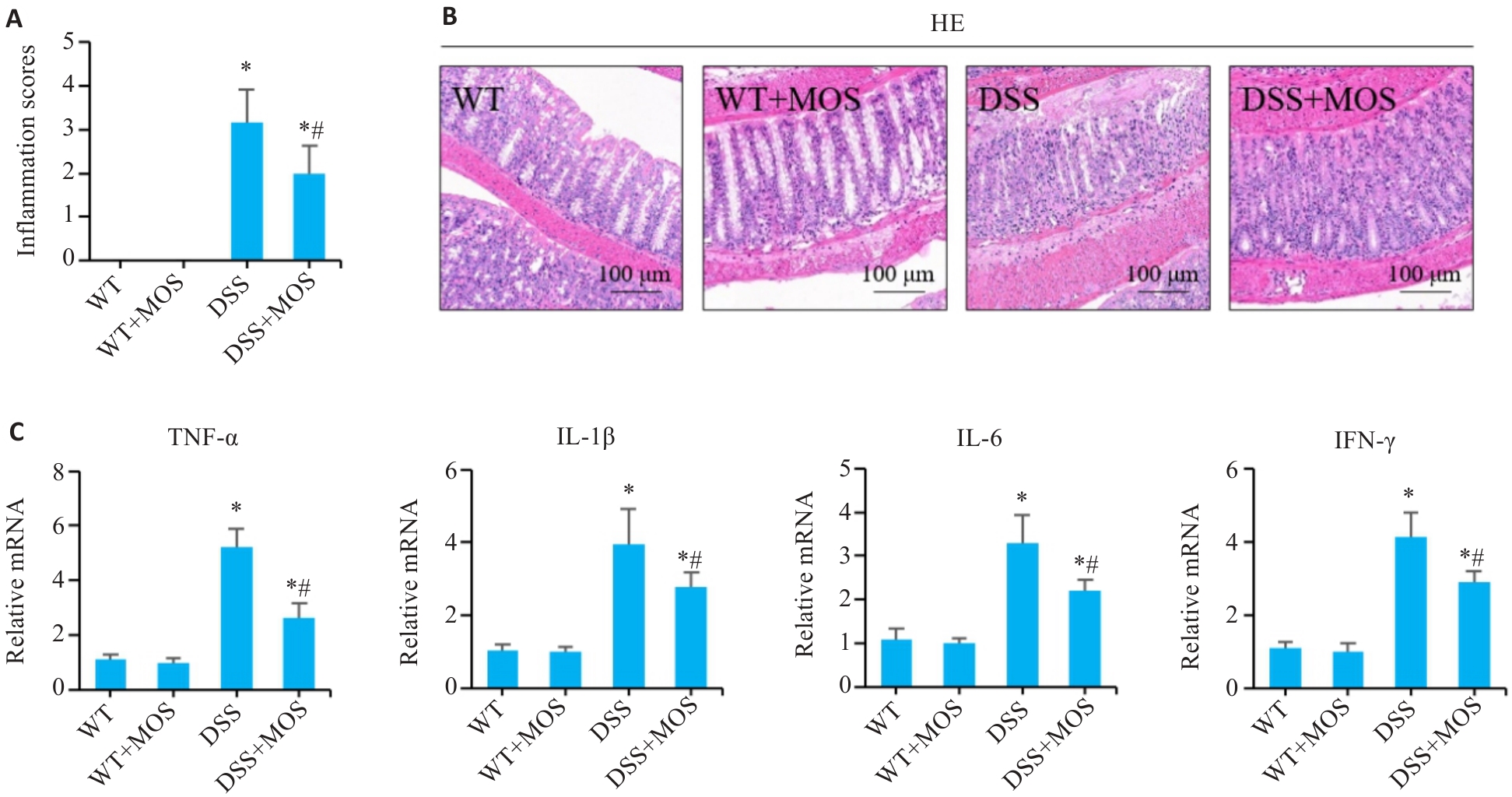
Fig.2 MOS improves intestinal mucosal damage in DSS-treated mice. A, B: HE staining of mouse colon tissues and the inflammation scores. C: Relative mRNA levels of TNF-α, IL-1β, IL-6 and IFN-γ in the colon tissues. n=6, *P<0.05 vs WT; #P<0.05 vs DSS.
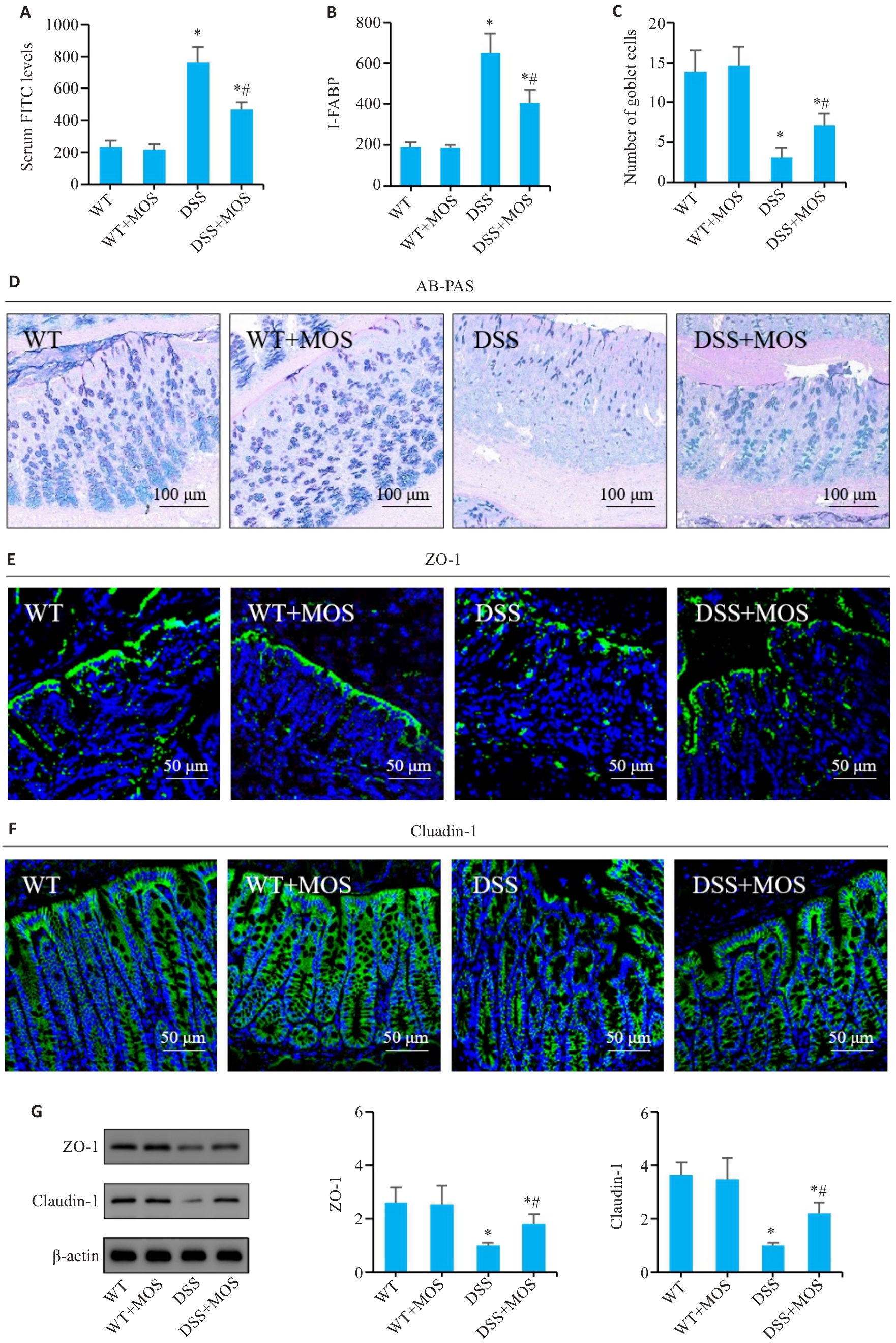
Fig.3 Effect of MOS on intestinal barrier function in DSS-treated mice. A, B: Comparison of serum FITC levels and I-FABP among the groups. C: Number of goblet cells. D: AB-PAS staining. E, F: Immunofluorescence assay of ZO-1 and claudin-1 expression. G: Western blotting for claudin-1 and ZO-1 expressions. n=6, *P<0.05 vs WT; #P<0.05 vs DSS.
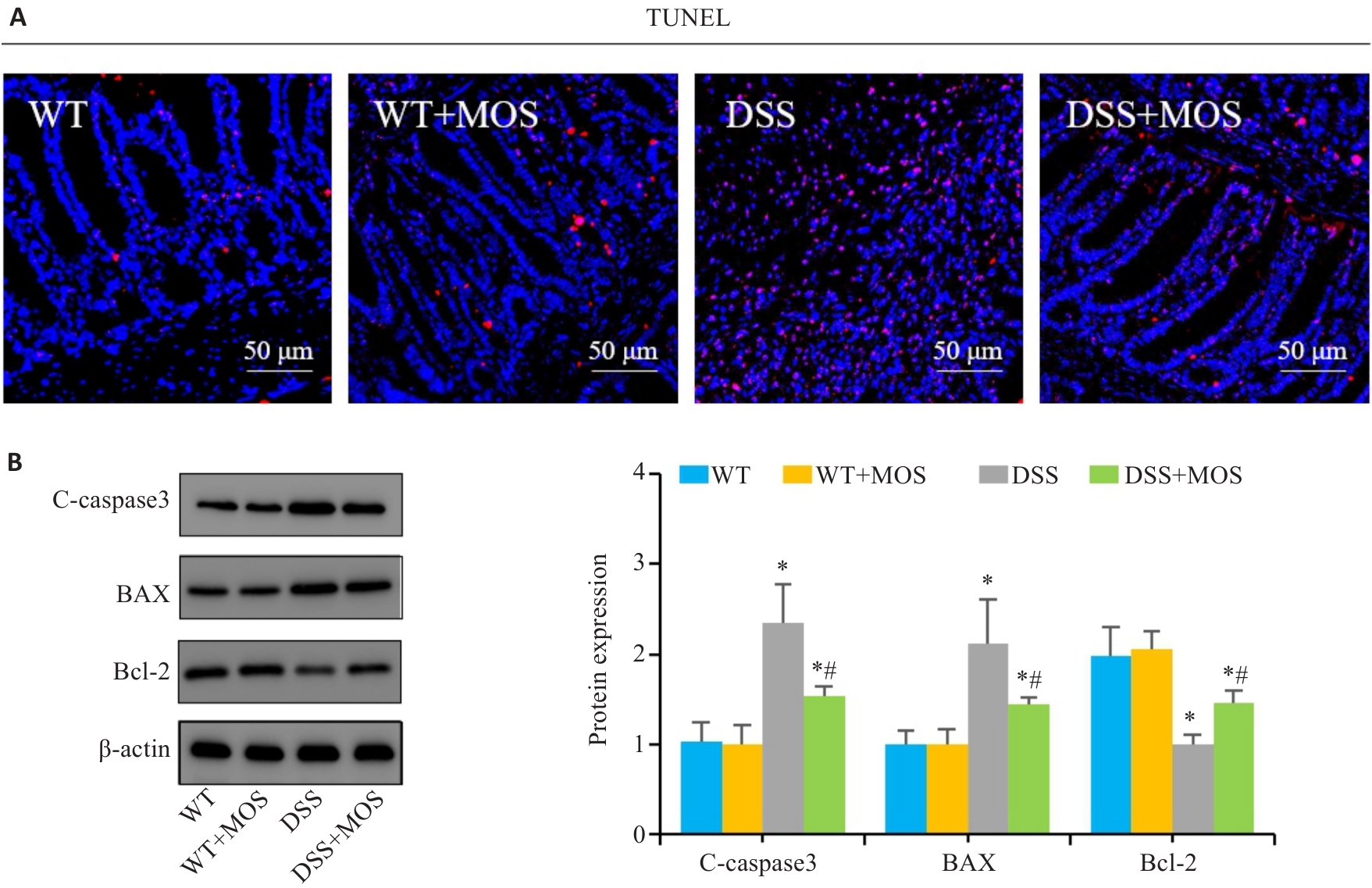
Fig.4 Effect of MOS on intestinal epithelium apoptosis in DSS-treated mice. A: TUNEL staining. B: Western blotting for C-caspase-3, Bax and Bcl-2. n=6,*P<0.05 vs WT; #P<0.05 vs DSS.
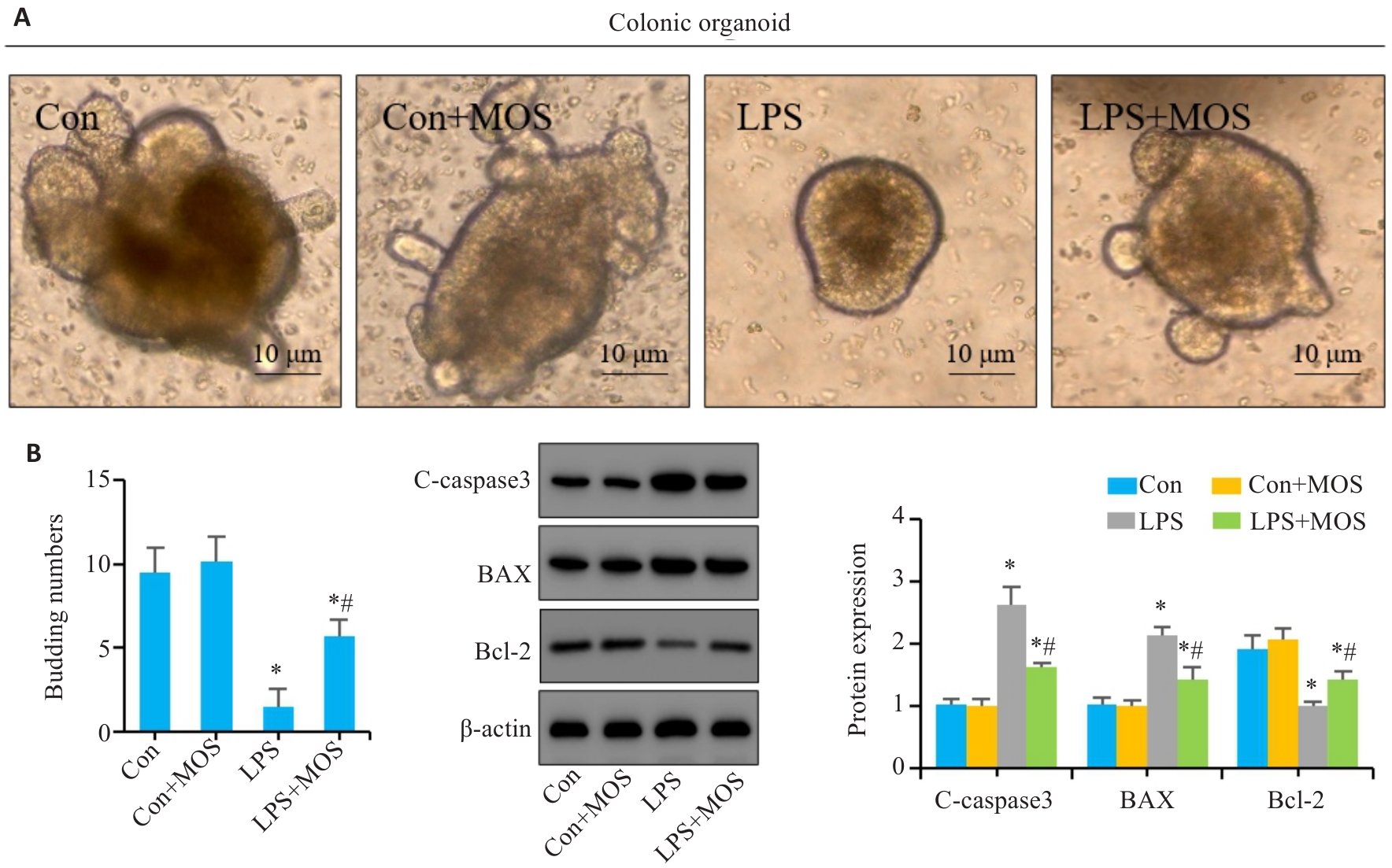
Fig.5 Effect of MOS on LPS-induced intestinal epithelial cell apoptosis in mouse colon organoids. A: Representative images of colon organoids. B: Number of organoids budding. C: Western blotting for C-caspase-3, Bax and Bcl-2. n=6,*P<0.05 vs Con; #P<0.05 vs LPS.
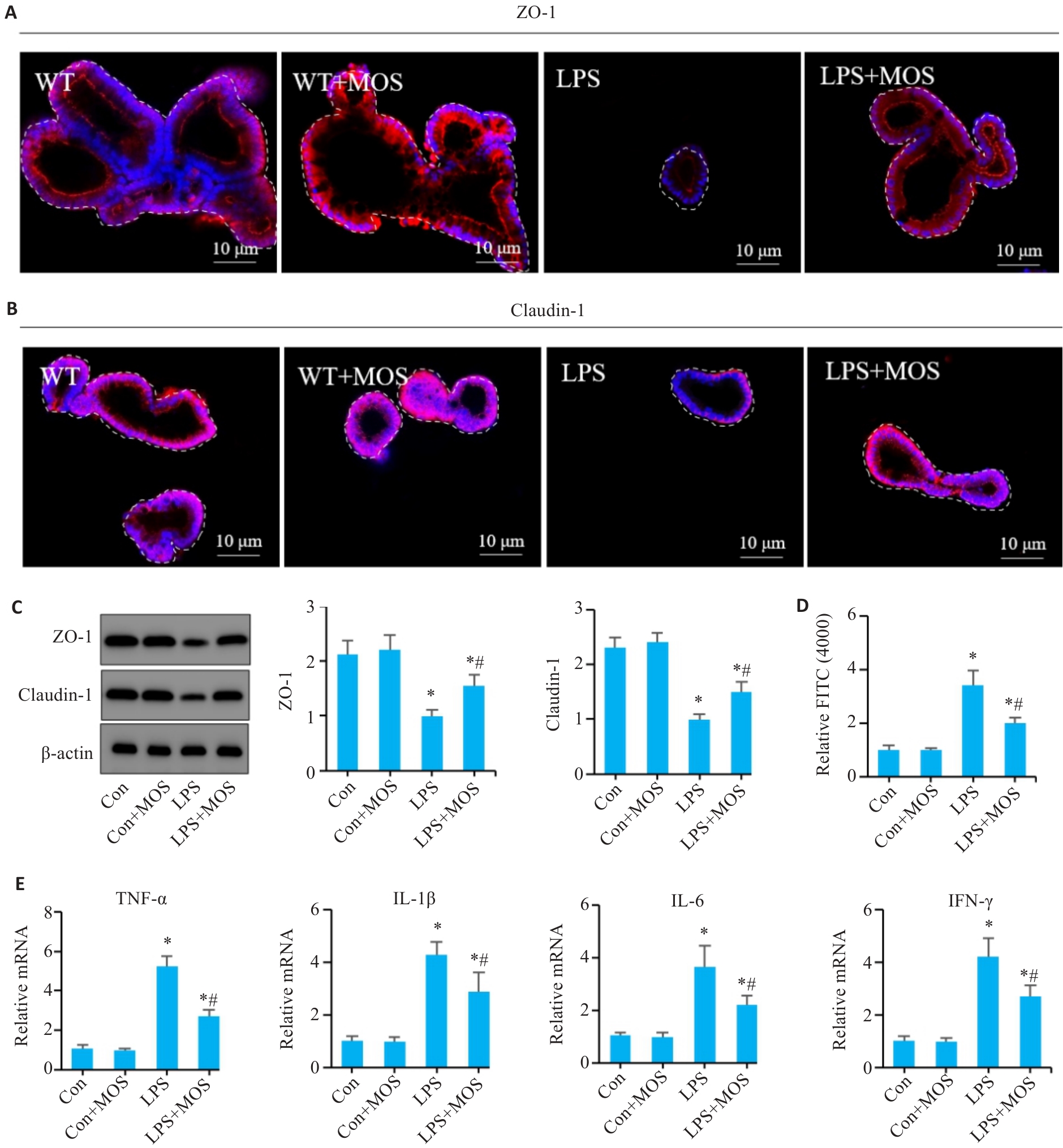
Fig.6 Effects of MOS on barrier function and inflammation in LPS-induced intestinal organoids. A, B: Immunofluorescence assay of ZO-1 and claudin-1. C: Western blotting of ZO-1and claudin-1. D: Permeability assay of the intestinal barrier. E: qRT-PCR for detecting mRNA levels of TNF-α, IL-1β, IL-6, and INF-γ in the colonic organoids. n=6, *P<0.05 vs Con; #P<0.05 vs LPS.
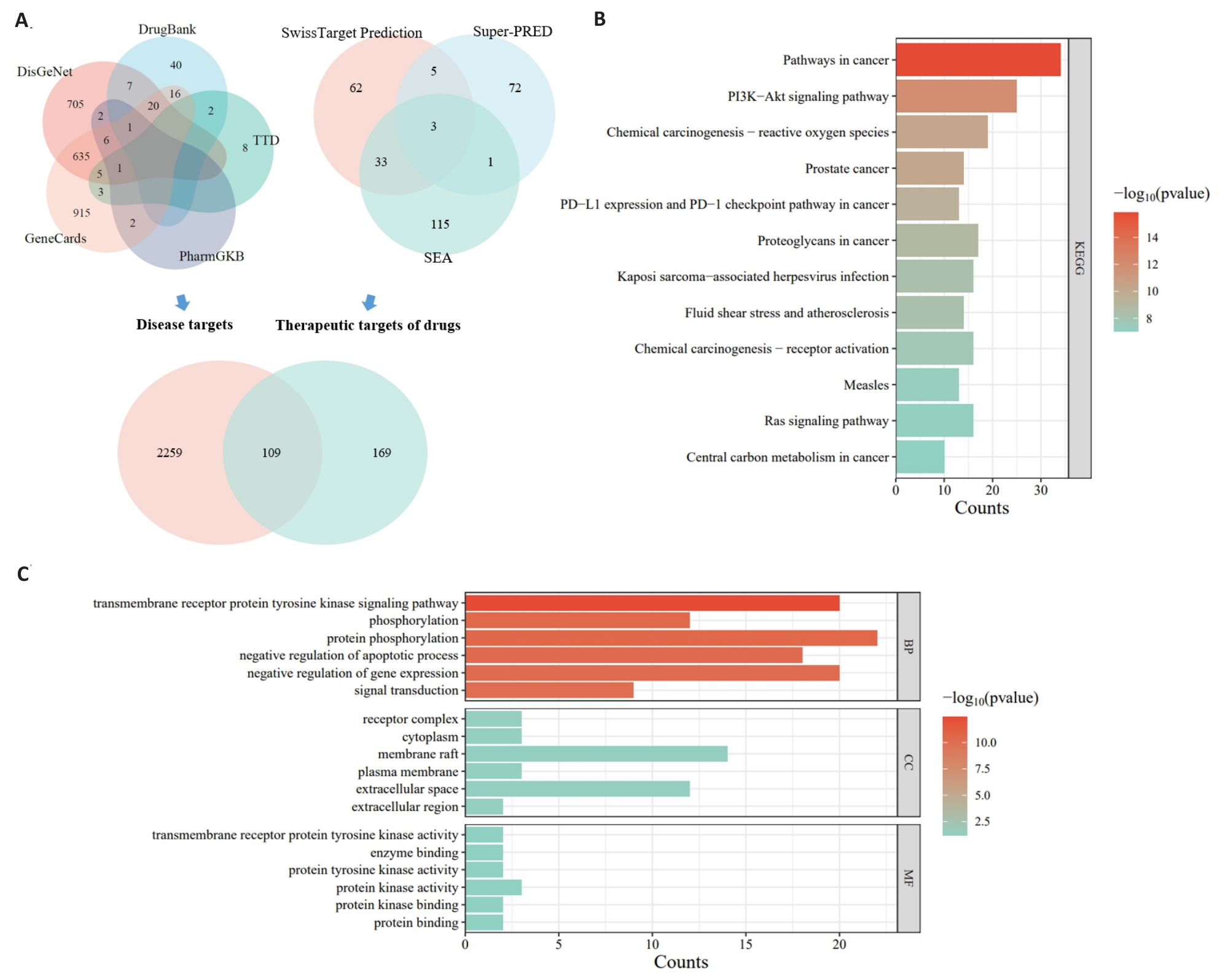
Fig.7 Network pharmacological analysis of the anti-apoptotic effect of MOS involving PI3K/AKT signaling. A: Venn diagram. B: GO enrichment analysis. C: KEGG enrichment analysis.
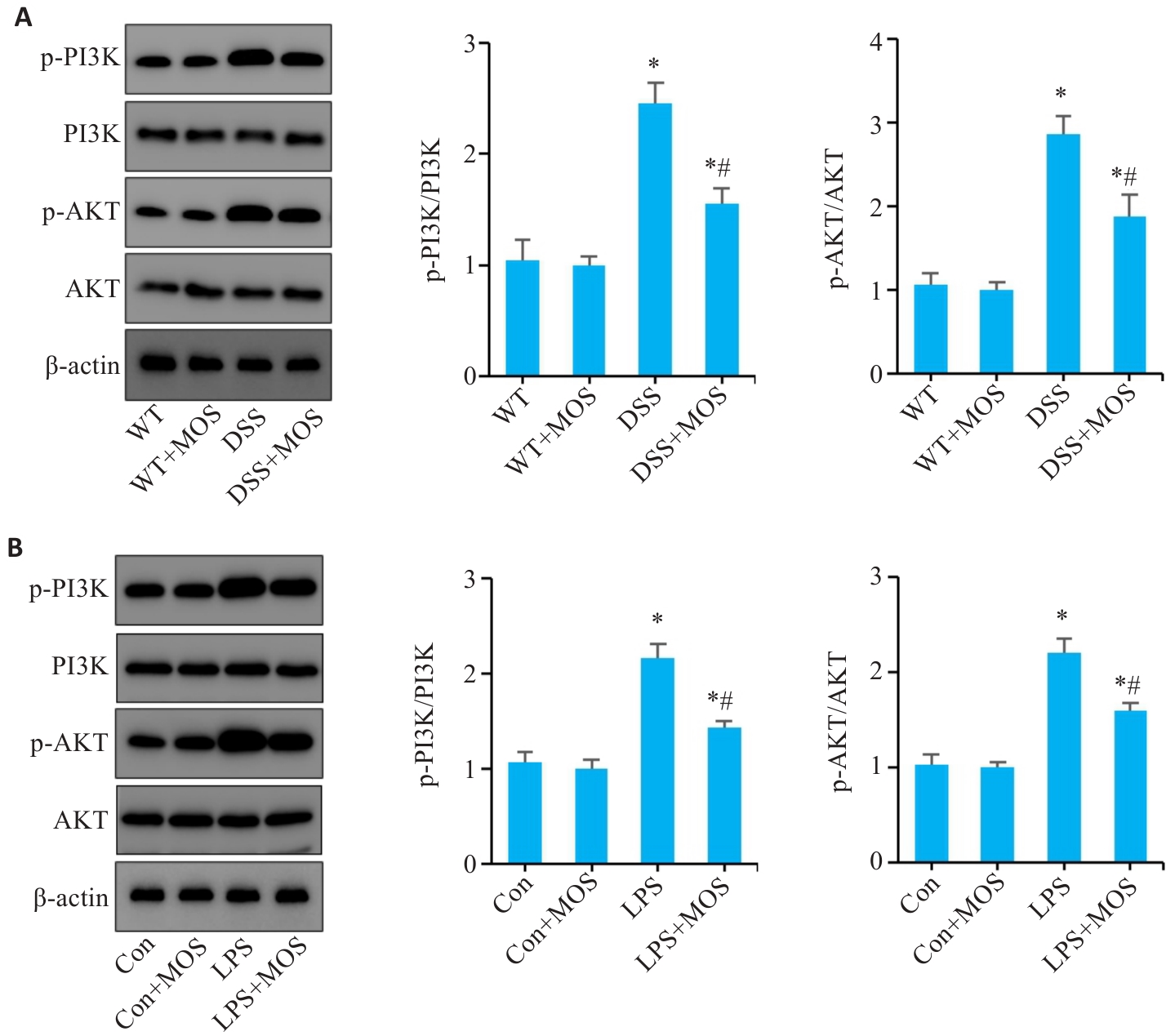
Fig.8 MOS inhibits apoptosis of intestinal epithelial cells possibly through the PI3K/AKT signaling pathway. A: Western blotting of PI3K, p-PI3K, AKT and p-AKT expressions in the colon tissue. B: Western blotting of PI3K, p-PI3K, AKT and p-AKT expressions in the colonic organoids. n=6, *P<0.05 vs WT or Con; #P<0.05 vs DSS or LPS.
| 1 | Geng ZJ, Zuo LG, Li J, et al. Ginkgetin improved experimental colitis by inhibiting intestinal epithelial cell apoptosis through EGFR/PI3K/AKT signaling[J]. FASEB J, 2024, 38(14): e23817. |
| 2 | Torres J, Mehandru S, Colombel JF, et al. Crohn's disease[J]. Lancet, 2017, 389(10080): 1741-55. |
| 3 | Nóbrega VG, Silva INN, Brito BS, et al. The onset of clinical manifestations in inflammatory bowel disease patients[J]. Arq Gastroenterol, 2018, 55(3): 290-5. |
| 4 | Veauthier B, Hornecker JR. Crohn's disease: diagnosis and management[J]. Am Fam Physician, 2018, 98(11): 661-9. |
| 5 | Wu JC, Xu XQ, Duan JQ, et al. EFHD2 suppresses intestinal inflammation by blocking intestinal epithelial cell TNFR1 internalization and cell death[J]. Nat Commun, 2024, 15(1): 1282. |
| 6 | Zhu LG, Xie Z, Yang G, et al. Stanniocalcin-1 promotes PARP1-dependent cell death via JNK activation in colitis[J]. Adv Sci, 2024, 11(5): e2304123. |
| 7 | Zuo LG, Li J, Ge ST, et al. Bryostatin-1 ameliorated experimental colitis in Il-10-/- Mice by protecting the intestinal barrier and limiting immune dysfunction[J]. J Cell Mol Med, 2019, 23(8): 5588-99. |
| 8 | Gupta M, Mishra V, Gulati M, et al. Natural compounds as safe therapeutic options for ulcerative colitis[J]. Inflammopharm-acology, 2022, 30(2): 397-434. |
| 9 | Xie YC, Gong SC, Wang LK, et al. Unraveling the treatment effects of Huanglian Jiedu decoction on drug-induced liver injury based on network pharmacology, molecular docking and experimental validation[J]. BMC Complement Med Ther, 2024, 24(1): 219. |
| 10 | Chao WW, Kuo YH, Lin BF. Anti-inflammatory activity of new compounds from Andrographis paniculata by NF-kappaB transactivation inhibition[J]. J Agric Food Chem, 2010, 58(4): 2505-12. |
| 11 | Zhang J, Zhao T, Zhang PP, et al. Moslosooflavone protects against brain injury induced by hypobaric hypoxic via suppressing oxidative stress, neuroinflammation, energy metabolism disorder, and apoptosis[J]. J Pharm Pharmacol, 2024, 76(1): 44-56. |
| 12 | Li MX, Li MY, Lei JX, et al. Huangqin decoction ameliorates DSS-induced ulcerative colitis: Role of gut microbiota and amino acid metabolism, mTOR pathway and intestinal epithelial barrier[J]. Phytomedicine, 2022, 100: 154052. |
| 13 | Zuo LG, Geng ZJ, Song X, et al. Browning of mesenteric white adipose tissue in Crohn's disease: a new pathological change and therapeutic target[J]. J Crohns Colitis, 2023, 17(8): 1179-92. |
| 14 | Wang L, Song X, Zhou YQ, et al. Sclareol protected against intestinal barrier dysfunction ameliorating Crohn's disease-like colitis via Nrf2/NF-B/MLCK signalling[J]. Int Immunopharmacol, 2024, 133: 112140. |
| 15 | Zuo LG, Li J, Zhang XF, et al. Aberrant mesenteric adipose extracellular matrix remodelling is involved in adipocyte dysfunction in Crohn's disease: the role of TLR-4-mediated macrophages[J]. J Crohns Colitis, 2022, 16(11): 1762-76. |
| 16 | Tsai PJ, Huang WC, Hsieh MC, et al. Flavones isolated from scutellariae Radix suppress Propionibacterium acnes-induced cytokine production in vitro and in vivo [J]. Molecules, 2015, 21(1): E15. |
| 17 | Song Y, Song Q, Tan FY, et al. Seliciclib alleviates ulcerative colitis by inhibiting ferroptosis and improving intestinal inflammation[J]. Life Sci, 2024, 351: 122794. |
| 18 | Marincola Smith P, Choksi YA, Markham NO, et al. Colon epithelial cell TGFβ signaling modulates the expression of tight junction proteins and barrier function in mice[J]. Am J Physiol Gastrointest Liver Physiol, 2021, 320(6): G936-57. |
| 19 | Ma J, Zhang JQ, Wang YF, et al. Modified Gegen Qinlian decoction ameliorates DSS-induced chronic colitis in mice by restoring the intestinal mucus barrier and inhibiting the activation of γδT17 cells[J]. Phytomedicine, 2023, 111: 154660. |
| 20 | Wei YY, Fan YM, Ga Y, et al. Shaoyao decoction attenuates DSS-induced ulcerative colitis, macrophage and NLRP3 inflammasome activation through the MKP1/NF‑κB pathway[J]. Phytomedicine, 2021, 92: 153743. |
| 21 | Yang Y, Zhou XC, Jia GY, et al. Network pharmacology based research into the effect and potential mechanism of Portulaca oleracea L. polysaccharide against ulcerative colitis[J]. Comput Biol Med, 2023, 161: 106999. |
| 22 | Xu Y, Wang XC, Jiang W, et al. Porphyra haitanensis polysaccharide-functionalized selenium nanoparticles for effective alleviation of ulcerative colitis[J]. Int J Biol Macromol, 2023, 253(Pt 8): 127570. |
| 23 | Turpin W, Lee SH, Garay JAR, et al. Increased intestinal permeability is associated with later development of Crohn's disease[J]. Gastroenterology, 2020, 159(6): 2092-100.e5. |
| 24 | Jarret A, Jackson R, Duizer C, et al. Enteric nervous system-derived IL-18 orchestrates mucosal barrier immunity[J]. Cell, 2020, 180(1): 50-63.e12. |
| 25 | Qiu Y, Yang H. Effects of intraepithelial lymphocyte-derived cytokines on intestinal mucosal barrier function[J]. J Interferon Cytokine Res, 2013, 33(10): 551-62. |
| 26 | Magarian Blander J. Death in the intestinal epithelium-basic biology and implications for inflammatory bowel disease[J]. FEBS J, 2016, 283(14): 2720-30. |
| 27 | Subramanian S, Geng H, Tan XD. Cell death of intestinal epithelial cells in intestinal diseases[J]. Sheng Li Xue Bao, 2020, 72(3): 308-24. |
| 28 | Liang BX, Zhong YZ, Huang YJ, et al. Underestimated health risks: polystyrene micro- and nanoplastics jointly induce intestinal barrier dysfunction by ROS-mediated epithelial cell apoptosis[J]. Part Fibre Toxicol, 2021, 18(1): 20. |
| 29 | Zhang Y, Yang X, Ge XH, et al. Puerarin attenuates neurological deficits via Bcl-2/Bax/cleaved caspase-3 and Sirt3/SOD2 apoptotic pathways in subarachnoid hemorrhage mice[J]. Biomed Pharmacother, 2019, 109: 726-33. |
| 30 | Zhang ZQ, Fan K, Meng JJ, et al. Deoxynivalenol hijacks the pathway of Janus kinase 2/signal transducers and activators of transcription 3 (JAK2/STAT-3) to drive caspase-3-mediated apoptosis in intestinal porcine epithelial cells[J]. Sci Total Environ, 2023, 864: 161058. |
| 31 | Eskandari E, Eaves CJ. Paradoxical roles of caspase-3 in regulating cell survival, proliferation, and tumorigenesis[J]. J Cell Biol, 2022, 221(6): e202201159. |
| 32 | Yang JL, Pi CC, Wang GH. Inhibition of PI3K/Akt/mTOR pathway by apigenin induces apoptosis and autophagy in hepatocellular carcinoma cells[J]. Biomed Pharmacother, 2018, 103: 699-707. |
| 33 | Chen SP, Peng JH, Sherchan P, et al. TREM2 activation attenuates neuroinflammation and neuronal apoptosis via PI3K/Akt pathway after intracerebral hemorrhage in mice[J]. J Neuroinflammation, 2020, 17(1): 168. |
| 34 | Yan XD, Tong XY, Jia YR, et al. Baiheqingjin formula reduces inflammation in mice with asthma by inhibiting the PI3K/AKT/NF-κb signaling pathway[J]. J Ethnopharmacol, 2024, 321: 117565. |
| [1] | Haonan¹ XU, Fang³ ZHANG, Yuying² HUANG, Qisheng⁴ YAO, Yueqin⁴ GUAN, Hao CHEN. Thesium chinense Turcz. alleviates antibiotic-associated diarrhea in mice by modulating gut microbiota structure and regulating the EGFR/PI3K/Akt signaling pathway [J]. Journal of Southern Medical University, 2025, 45(2): 285-295. |
| [2] | Yuejiao PEI, Huimin LIU, Yu XIN, Bo LIU. High expression of miR-124 improves cognitive function of sleep-deprived rats by modulating the PI3K/AKT signaling pathway [J]. Journal of Southern Medical University, 2025, 45(2): 340-346. |
| [3] | Yuru ZHANG, Lei WAN, Haoxiang FANG, Fangze LI, Liwen WANG, Kefei LI, Peiwen YAN, Hui JIANG. Inhibiting miR-155-5p promotes proliferation of human submandibular gland epithelial cells in primary Sjogren's syndrome by negatively regulating the PI3K/AKT signaling pathway via PIK3R1 [J]. Journal of Southern Medical University, 2025, 45(1): 65-71. |
| [4] | Xianheng ZHANG, Jian LIU, Qi HAN, Yiming CHEN, Xiang DING, Xiaolu CHEN. Huangqin Qingrechubi Capsule alleviates inflammation and uric acid and lipid metabolism imbalance in rats with gouty arthritis by inhibiting the PTEN/PI3K/AKT signaling pathway [J]. Journal of Southern Medical University, 2024, 44(8): 1450-1458. |
| [5] | Shan XIANG, Zongxing ZHANG, Lu JIANG, Daozhong LIU, Weiyi LI, Zhuoma BAO, Rui TIAN, Dan CHENG, Lin YUAN. Tujia medicine Toddalia asiatica improves synovial pannus in rats with collagen-induced arthritis through the PI3K/Akt signaling pathway [J]. Journal of Southern Medical University, 2024, 44(8): 1582-1588. |
| [6] | Yao CHENG, Yuanying WANG, Feiyang YAO, Pan HU, Mingxian CHEN, Ning WU. Baicalin suppresses type 2 dengue virus-induced autophagy of human umbilical vein endothelial cells by inhibiting the PI3K/AKT pathway [J]. Journal of Southern Medical University, 2024, 44(7): 1272-1283. |
| [7] | Yuanyuan WANG, Teng CHEN, Xiaofan CONG, Yiran LI, Rui CHEN, Pei ZHANG, Xiaojin SUN, Surong ZHAO. Pristimerin enhances cisplatin-induced apoptosis in nasopharyngeal carcinoma cells via ROS-mediated deactivation of the PI3K/AKT signaling pathway [J]. Journal of Southern Medical University, 2024, 44(5): 904-912. |
| [8] | SHAO Rongrong, YANG Zi, ZHANG Wenjing, ZHANG Nuo, ZHAO Yajing, ZHANG Xiaofeng, ZUO Lugen, GE Sitang. Pachymic acid protects against Crohn's disease-like intestinal barrier injury and colitis in mice by suppressing intestinal epithelial cell apoptosisviainhibiting PI3K/AKT signaling [J]. Journal of Southern Medical University, 2023, 43(6): 935-942. |
| [9] | XIAO Shuzhe, CHENG Yanling, ZHU Yun, TANG Rui, GU Jianbiao, LAN Lin, HE Zhihua, LIU Danqiong, GENG Lanlan, CHENG Yang, GONG Sitang. Fibroblasts overpressing WNT2b cause impairment of intestinal mucosal barrier [J]. Journal of Southern Medical University, 2023, 43(2): 206-212. |
| [10] | GAO Xiaoyang, ZHAO Xiaolu, ZHANG Chunyan, YAN Yuxin, JIN Rong, MA Yuehong. Quercetin induces hepatic stellate cell apoptosis by inhibiting the PI3K/Akt signaling pathway via upregulating miR-146 [J]. Journal of Southern Medical University, 2023, 43(10): 1725-1733. |
| [11] | FAN Xiaoli, WANG Juan, WANG Liming. Licochalcone A induces cell cycle arrest in human lung squamous carcinoma cells via the PI3K/Akt signaling pathway [J]. Journal of Southern Medical University, 2023, 43(1): 111-116. |
| [12] | LIU Jianrong, SHEN Weixing, CHENG Haibo, FAN Minmin, XIAO Jun, XU Changliang, TAN Jiani, LAI Yueyang, YU Chengtao, SUN Dongdong, LI Liu. Shenbai Jiedu Fang inhibits AOM/DSS-induced colorectal adenoma formation and carcinogenesis in mice via miRNA-22-mediated regulation of the PTEN/PI3K/AKT signaling pathway [J]. Journal of Southern Medical University, 2022, 42(10): 1452-1461. |
| [13] | LIANG Xiaofang, YANG Yue, XU Shuaishuai, LIU Ying, CHU Hanyu, TANG Yan, YANG Fei. Long-term low-dose microcystin-LR exposure induces renal injury in mice by activating PI3K/AKT signaling pathway [J]. Journal of Southern Medical University, 2022, 42(10): 1486-1494. |
| [14] | . PI3K/Akt signaling pathway mediates the protective effect of endomorphin-1 post-conditioning against myocardial ischemia-reperfusion injury in rats [J]. Journal of Southern Medical University, 2021, 41(6): 870-875. |
| [15] | . Inhibitory effect of apatinib on HCT-116 cells and its mechanism [J]. Journal of Southern Medical University, 2017, 37(03): 367-. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||