Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (4): 718-724.doi: 10.12122/j.issn.1673-4254.2025.04.06
Zhengwang ZHU1,2( ), Linlin WANG1,2, Jinghan ZHAO1,2, Ruixue MA1, Yuchun YU1, Qingchun CAI3, Bing WANG4, Pingsheng ZHU1,2(
), Linlin WANG1,2, Jinghan ZHAO1,2, Ruixue MA1, Yuchun YU1, Qingchun CAI3, Bing WANG4, Pingsheng ZHU1,2( ), Mingsan MIAO1,2
), Mingsan MIAO1,2
Received:2024-12-25
Online:2025-04-20
Published:2025-04-28
Contact:
Pingsheng ZHU
E-mail:2235848407@qq.com;zhupingsheng@126.com
Supported by:Zhengwang ZHU, Linlin WANG, Jinghan ZHAO, Ruixue MA, Yuchun YU, Qingchun CAI, Bing WANG, Pingsheng ZHU, Mingsan MIAO. Tuihuang Mixture improves α‑naphthylisothiocyanate-induced cholestasis in rats by inhibiting NLRP3 inflammasomes via regulating farnesoid X receptor[J]. Journal of Southern Medical University, 2025, 45(4): 718-724.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.04.06
| Gene | Primer sequence (5'-3') | Length (bp) |
|---|---|---|
| FXR | Forward: CACTGACACGCCCTTTTTGC | 86 |
| Reverse: TGGAGGATAAAACGAGGCGG | ||
| NLRP3 | Forward: CTCACCTCACACTCCTGCTG | 122 |
| Reverse: AGAACCTCACAGAGCGTCAC | ||
| ASC | Forward: CTGCAGATGGACCCCATAGAC | 74 |
| Reverse: GTGAGCTCCAAGCCATACCC | ||
| Caspase-1 | Forward: GACCGAGTGGTTCCCTCAAG | 108 |
| Reverse: GACGTGTACGAGTGGGTGTT | ||
| GSDMD | Forward: CAGAACCAGTGTCTGGCAGT | 86 |
| Reverse: ACGTTGCATGATCTCCCAGG | ||
| IL-1β | Forward: AGGCTGACAGACCCCAAAAG | 178 |
| Reverse: CTCCACGGGCAAGACATAGG | ||
| IL-18 | Forward: ACCACTTTGGCAGACTTCACT | 126 |
| Reverse: CGTTGGCTGTTCGGTCGATA | ||
| β-actin | Forward: ATGGATGACGATATCGCTGC | 150 |
| Reverse: CTTCTGACCCATACCCACCA |
Tab.1 Primer sequences
| Gene | Primer sequence (5'-3') | Length (bp) |
|---|---|---|
| FXR | Forward: CACTGACACGCCCTTTTTGC | 86 |
| Reverse: TGGAGGATAAAACGAGGCGG | ||
| NLRP3 | Forward: CTCACCTCACACTCCTGCTG | 122 |
| Reverse: AGAACCTCACAGAGCGTCAC | ||
| ASC | Forward: CTGCAGATGGACCCCATAGAC | 74 |
| Reverse: GTGAGCTCCAAGCCATACCC | ||
| Caspase-1 | Forward: GACCGAGTGGTTCCCTCAAG | 108 |
| Reverse: GACGTGTACGAGTGGGTGTT | ||
| GSDMD | Forward: CAGAACCAGTGTCTGGCAGT | 86 |
| Reverse: ACGTTGCATGATCTCCCAGG | ||
| IL-1β | Forward: AGGCTGACAGACCCCAAAAG | 178 |
| Reverse: CTCCACGGGCAAGACATAGG | ||
| IL-18 | Forward: ACCACTTTGGCAGACTTCACT | 126 |
| Reverse: CGTTGGCTGTTCGGTCGATA | ||
| β-actin | Forward: ATGGATGACGATATCGCTGC | 150 |
| Reverse: CTTCTGACCCATACCCACCA |
| Group | Dose (g/kg) | ALT (U/L) | AST (U/L) | ALP (U/L) | γ-GT (U/L) |
|---|---|---|---|---|---|
| Blank | - | 17.11±3.72 | 51.53±7.37 | 136.92±23.27 | 0.79±0.19 |
| Model | - | 309.03±61.60** | 340.19±56.20** | 428.38±80.54** | 9.52±2.19** |
| UDCA | 0.1 | 263.38±42.35# | 305.22±51.98 | 385.27±64.91 | 4.74±1.09## |
| THM | 17.25 | 177.98±31.14## | 219.90±45.40## | 359.38±53.84# | 3.93±1.08## |
| *P<0.05, **P<0.01 vs Blank group; #P<0.05, ##P<0.01 vs Model group. | |||||
Tab.2 Effects of Tuihuang Mixture on serum levels of ALT, AST, ALP and γ-GT in rats with cholestasis (Mean±SD, n=12)
| Group | Dose (g/kg) | ALT (U/L) | AST (U/L) | ALP (U/L) | γ-GT (U/L) |
|---|---|---|---|---|---|
| Blank | - | 17.11±3.72 | 51.53±7.37 | 136.92±23.27 | 0.79±0.19 |
| Model | - | 309.03±61.60** | 340.19±56.20** | 428.38±80.54** | 9.52±2.19** |
| UDCA | 0.1 | 263.38±42.35# | 305.22±51.98 | 385.27±64.91 | 4.74±1.09## |
| THM | 17.25 | 177.98±31.14## | 219.90±45.40## | 359.38±53.84# | 3.93±1.08## |
| *P<0.05, **P<0.01 vs Blank group; #P<0.05, ##P<0.01 vs Model group. | |||||
| Group | Dose (g/kg) | TBA (μmol/L) | TBIL (μmol/L) |
|---|---|---|---|
| Blank | - | 8.50±3.29 | 0.89±0.19 |
| Model | - | 106.28±29.19** | 34.95±9.18** |
| UDCA | 0.1 | 84.60±19.95# | 21.51±5.19## |
| THM | 17.25 | 57.62±14.74## | 17.79±4.39## |
| *P<0.05, **P<0.01 vs Blank group; #P<0.05, ##P<0.01 vs Model group. | |||
Tab.3 Effects of Tuihuang Mixture on serum levels of TBA and TBIL in rats with cholestasis (Mean±SD, n=12)
| Group | Dose (g/kg) | TBA (μmol/L) | TBIL (μmol/L) |
|---|---|---|---|
| Blank | - | 8.50±3.29 | 0.89±0.19 |
| Model | - | 106.28±29.19** | 34.95±9.18** |
| UDCA | 0.1 | 84.60±19.95# | 21.51±5.19## |
| THM | 17.25 | 57.62±14.74## | 17.79±4.39## |
| *P<0.05, **P<0.01 vs Blank group; #P<0.05, ##P<0.01 vs Model group. | |||
| Group | Dose (g/kg) | IL-1β (pg/mL) | IL-18 (pg/mL) |
|---|---|---|---|
| Blank | - | 412.74±81.93 | 36.11±8.50 |
| Model | - | 511.75±53.5** | 57.06±5.53** |
| UDCA | 0.1 | 426.78±73.08## | 40.57±8.98## |
| THM | 17.25 | 387.85±68.84## | 30.17±6.18## |
| *P<0.05, **P<0.01 vs Blank group; #P<0.05, ##P<0.01 vs Model group. | |||
Tab.4 Effects of Tuihuang Mixture on hepatic expressions of IL-1β and IL-18 in rats with cholestasis (Mean±SD, n=12)
| Group | Dose (g/kg) | IL-1β (pg/mL) | IL-18 (pg/mL) |
|---|---|---|---|
| Blank | - | 412.74±81.93 | 36.11±8.50 |
| Model | - | 511.75±53.5** | 57.06±5.53** |
| UDCA | 0.1 | 426.78±73.08## | 40.57±8.98## |
| THM | 17.25 | 387.85±68.84## | 30.17±6.18## |
| *P<0.05, **P<0.01 vs Blank group; #P<0.05, ##P<0.01 vs Model group. | |||
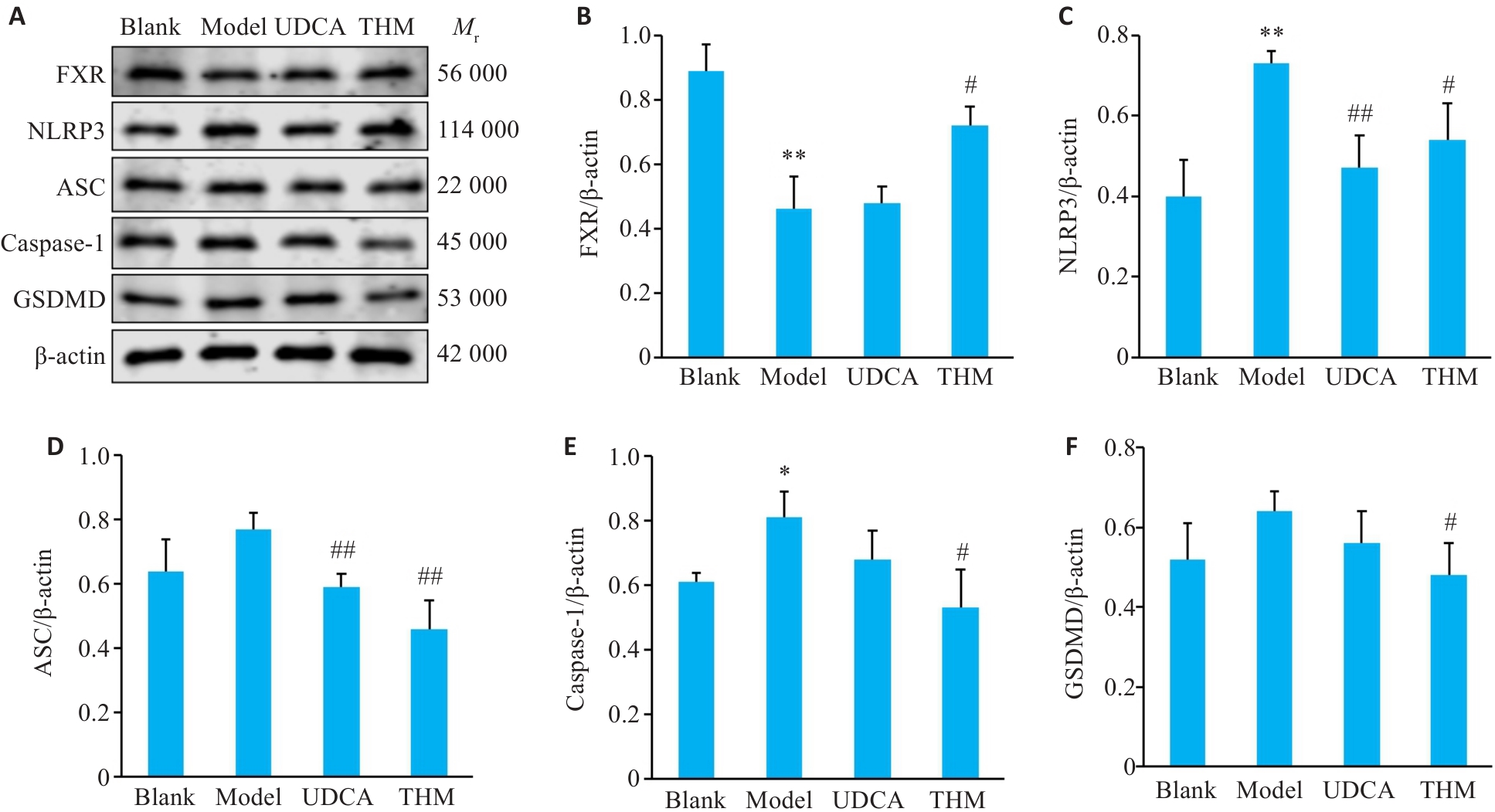
Fig.2 Effect of Tuihuang Mixture on expressions of FXR, NLRP3, ASC, caspase-1 and GSDMD proteins in the liver tissue of rats with cholestasis. A: Western blotting for FXR, NLRP3, ASC, Caspase-1 and GSDMD proteins. B-F: Quantitative analysis of FXR, NLRP3, ASC, Caspase-1 and GSDMD protein expression levels. *P<0.05, **P<0.01 vs Blank group; #P<0.05, ##P<0.01 vs Model group (Mean±SD, n=3).
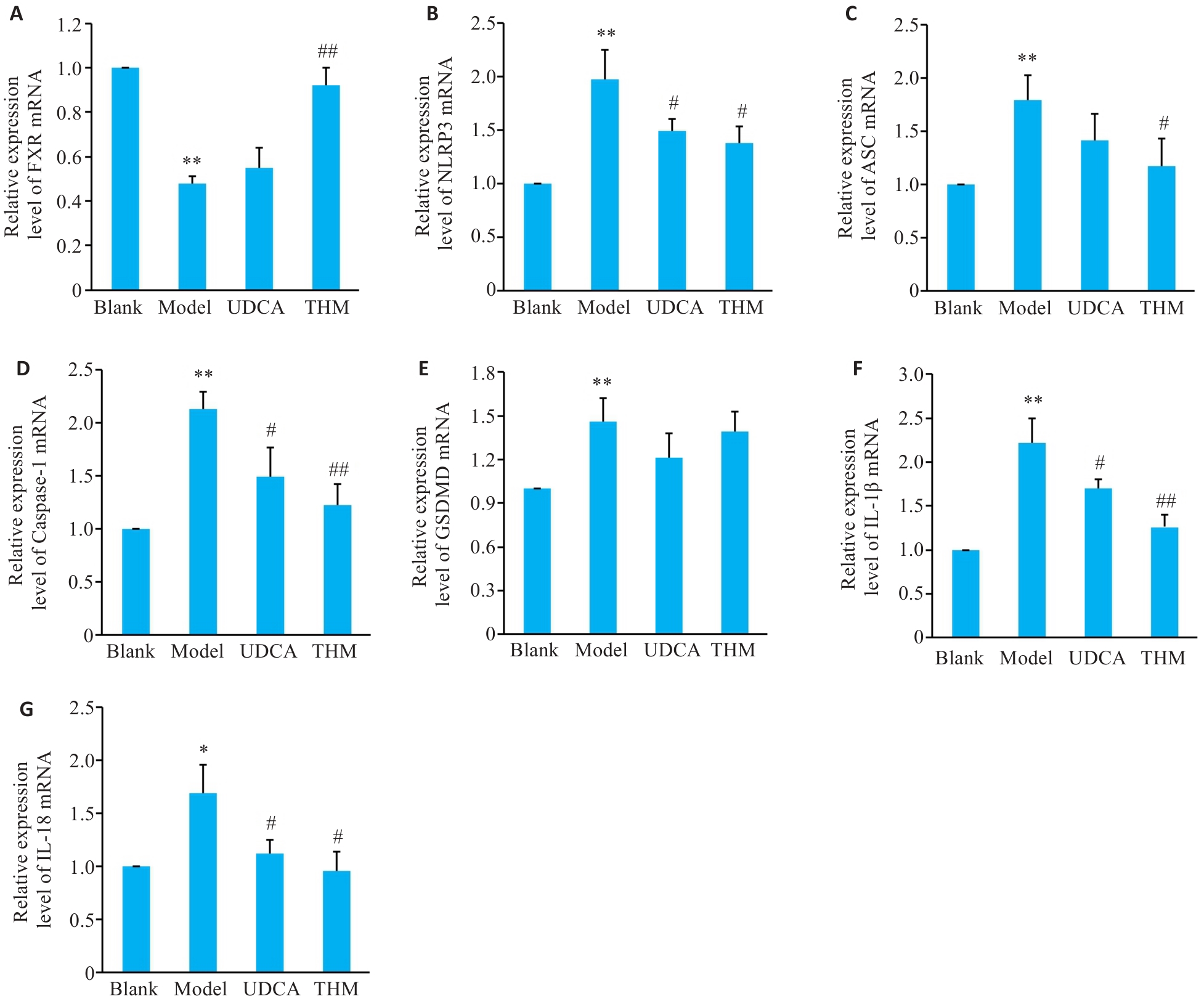
Fig.3 Effect of Tuihuang Mixture on expressions of FXR, NLRP3, ASC, Caspase-1, GSDMD, IL-1β and IL-18 mRNA in the liver tissue of rats with cholestasis. A-G: Relative expression levels of FXR, NLRP3, ASC, Caspase-1, GSDMD, IL-1β and IL-18 mRNA. *P<0.05, **P<0.01 vs Blank group. #P<0.05, ##P<0.01 vs Model group (Mean±SD, n=3).
| 1 | 李国栋, 杨金玉, 马小华, 等. 清热卡森颗粒对肝内胆汁淤积大鼠模型的治疗作用及机制研究[J]. 世界科学技术-中医药现代化, 2022, 24(10): 4038-46. DOI: 10.11842/wst.20220103002 |
| 2 | 中华医学会肝病学分会. 胆汁淤积性肝病管理指南(2021)[J]. 临床肝胆病杂志, 2022, 38(1): 62-9. DOI: 10.3760/cma.j.cn112138-20211112-00795 |
| 3 | Zhang L, Pan Q, Zhang L, et al. Runt-related transcription factor-1 ameliorates bile acid-induced hepatic inflammation in cholestasis through JAK/STAT3 signaling[J]. Hepatology, 2023, 77(6): 1866-81. |
| 4 | Wu H, Chen C, Ziani S, et al. Fibrotic events in the progression of cholestatic liver disease[J]. Cells, 2021, 10(5): 1107. |
| 5 | Fu K, Li Y, Dai S, et al. Exploration of the molecular basis of Forsythia fruit in the prevention and treatment of cholestatic liver injury through network pharmacology and molecular docking[J]. Nutrients, 2023, 15(9): 2065. |
| 6 | Xie W, Cao Y, Xu M, et al. Prognostic significance of elevated cholestatic enzymes for fibrosis and hepatocellular carcinoma in hospital discharged chronic viral hepatitis patients[J]. Sci Rep, 2017, 7(1): 10289. |
| 7 | 陈欣菊, 韩 捷. 退黄合剂联合脐火疗法治疗阴黄型慢性乙型重型肝炎15例[J]. 中国中医药现代远程教育, 2015, 13(10): 45-6. DOI: 10.3969/j.issn.1672-2779.2015.10.024 |
| 8 | 刘光伟, 费景兰, 王春芳, 等. 退黄合剂保留灌肠联合逐水方敷脐治疗肝硬化顽固性腹水临床疗效观察[J]. 时珍国医国药, 2015, 26(3): 662-3. |
| 9 | 江志华. 退黄合剂联合人工肝血浆置换治疗重型肝炎20例[J]. 河南中医, 2011, 31(1): 37-8. |
| 10 | 李 玥, 宋国超, 徐晓青, 等. 栀子柏皮汤对胆酸饲料诱导胆汁淤积症小鼠肝保护机制研究[J]. 上海中医药大学学报, 2022, 36(S1): 154-60. |
| 11 | 姜 宁, 蒲兰香, 黄 峰, 等. 香兰素下调cGAS/STING信号通路改善肝内胆汁淤积大鼠肝组织损伤[J]. 中国药理学通报, 2024, 40(9): 1695-700. |
| 12 | 张奕奕, 王慧凯, 姜学连. 中医药治疗淤胆型肝炎研究进展[J]. 实用中医内科杂志, 2022, 36(8): 55-7. DOI: 10.13729/j.issn.1671-7813.Z20221583 |
| 13 | 赵 阳, 刘凡琪, 田 爽, 等. 中药治疗胆汁淤积性肝病作用机制的研究进展[J]. 药物评价研究, 2022, 45(2): 375-81. |
| 14 | 苏瑞钟. 清热化瘀中药治疗肝胆湿热型急性肝内胆汁淤积症临床研究[J]. 湖北中医杂志, 2021, 43(12): 27-30. |
| 15 | 杨 雯, 王 敏, 唐金模. 胆汁淤积性肝病的中医诊治概况[J]. 中西医结合肝病杂志, 2023, 33(5): 452-5. DOI: 10.3969/j.issn.1005-0264.2023.005.019 |
| 16 | 杨家越, 杨 恒, 代 耀, 等. 基于“湿、热、瘀” 论治胆汁淤积性肝病的研究[J]. 中国中医基础医学杂志, 2022, 28(6): 1009-13, 1018. |
| 17 | 刘江凯, 赵文霞, 许顺畅. 退黄合剂对急性肝衰竭大鼠内毒素及TNF-α、IL-1β、IL-6水平的影响[J]. 时珍国医国药, 2015, 26(3): 587-8. |
| 18 | Zhang WW, Wu HF, Luo SM, et al. Molecular insights into experimental models and therapeutics for cholestasis[J]. Biomed Pharmacother, 2024, 174: 116594. |
| 19 | Qin SS, Tian JZ, Zhao Y, et al. Gardenia extract protects against intrahepatic cholestasis by regulating bile acid enterohepatic circulation[J]. J Ethnopharmacol, 2024, 319: 117083. |
| 20 | 曹家樊, 孙 跃, 丁 鑫, 等. 熊果苷通过抑制巨噬细胞募集并调控Akt/NF-κB和Smad信号通路改善小鼠肝纤维化[J]. 南方医科大学学报, 2024, 44(4): 652-9. DOI: 10.12122/j.issn.1673-4254.2024.04.05 |
| 21 | Iluz-Freundlich D, Zhang M, Uhanova J, et al. The relative expression of hepatocellular and cholestatic liver enzymes in adult patients with liver disease[J]. Ann Hepatol, 2020, 19(2): 204-8. |
| 22 | 高硕玉, 张 秦, 张 帅, 等. 药物性胆汁淤积型肝损伤患者的临床表现、影像学特征以及转归[J]. 肝脏, 2024, 29(8): 971-4, 979. |
| 23 | 张 娜, 晏 旎, 周蒙恩, 等. NLRP3炎症小体在急慢性肝脏疾病发生和治疗中的研究进展[J]. 辽宁中医杂志, 2020, 47(5): 217-20. |
| 24 | Sharma BR, Kanneganti TD. NLRP3 inflammasome in cancer and metabolic diseases[J]. Nat Immunol, 2021, 22(5): 550-9. |
| 25 | 章林聪, 吴家胜, 田 甜, 等.基于网络药理学的茵陈术附汤抗石胆酸诱导的胆汁淤积性肝损伤作用机制研究[J]. 药学学报, 2023, 58(11): 3366-78. |
| 26 | 栾少华, 王 洋, 张长柱, 等. NLRP3炎症小体在肝星状细胞激活引起的肝纤维化中作用的研究进展[J].医学研究与战创伤救治, 2024,37(10): 1114-20. |
| 27 | 孟宪萌, 许 斌, 陈 维. 经方“大柴胡汤” 对梗阻性胆汁淤积性肝损伤细胞焦亡调节作用的研究进展[J]. 中华中医药学刊, 2022, 40(7): 220-4. |
| 28 | Swanson KV, Deng M, Ting JP. The NLRP3 inflammasome: molecular activation and regulation to therapeutics[J]. Nat Rev Immunol, 2019, 19(8): 477-89. |
| 29 | 郭紫云, 杜丽娜, 张艳菊, 等. 基于调控法尼醇X受体的中药及其活性成分抗胆汁淤积的研究进展[J]. 世界科学技术-中医药现代化, 2022, 24(11): 4199-206. DOI: 10.11842/wst.20211109003 |
| 30 | 胡 莉, 杨伟峰, 刘 婷, 等. 法尼醇X受体在治疗胆汁淤积性肝病中的作用机制和药物研究进展[J]. 中国药物警戒, 2024, 21(10): 1184-91, 1199. |
| 31 | 钟艳花, 李颖仪, 林 重, 等. 白花蛇舌草对ANIT诱导的胆汁淤积大鼠保肝作用研究[J]. 中药新药与临床药理, 2021, 32(7): 952-8. |
| 32 | 贾锶琦, 窦晓光. 法尼醇X受体及其激动剂与肝脏疾病[J]. 肝脏, 2021, 26(11): 1293-7. |
| 33 | Hao HP, Cao LJ, Jiang CT, et al. Farnesoid X receptor regulation of the NLRP3 inflammasome underlies cholestasis-associated sepsis[J]. Cell Metab, 2017, 25(4): 856-67.e5. |
| 34 | 吴晓明, 何 强, 侯林毅, 等. 淤胆通方对α-萘异硫氰酸酯诱导的胆汁淤积小鼠肠道菌群和肠道屏障功能的影响[J]. 临床肝胆病杂志, 2023, 39(4): 864-75. DOI: 10.3969/j.issn.1001-5256.2023.04.018 |
| [1] | Mingyuan LI, Wei ZHANG, Mengqing HUA. Bardoxolone methyl alleviates acute liver injury in mice by inhibiting NLRP3 inflammasome activation [J]. Journal of Southern Medical University, 2024, 44(9): 1662-1669. |
| [2] | LING Xuguang, XU Wenwen, PANG Guanlai, HONG Xuxing, LIU Fengqin, LI Yang. Tea polyphenols ameliorates acute lung injury in septic mice by inhibiting NLRP3 inflammasomes [J]. Journal of Southern Medical University, 2024, 44(2): 381-386. |
| [3] | FANG Shangping, SUN Renke, SU Hui, ZHAI Kecheng, XIANG Yu, GAO Yangmengna, GUO Wenjun. Chlorogenic acid alleviates acute kidney injury in septic mice by inhibiting NLRP3 inflammasomes and the caspase-1 canonical pyroptosis pathway [J]. Journal of Southern Medical University, 2024, 44(2): 317-323. |
| [4] | LU Li, LIU Didi, YANG Yanqing, WANG Fengchao. WP1130 relieves septic shock in mice by inhibiting NLRP3 inflammasome activation [J]. Journal of Southern Medical University, 2022, 42(12): 1747-1754. |
| [5] | FANG Shangping, YUAN Ran, SUN Renke, MA Tongjun. Knockout of S1PR3 attenuates acute lung injury in mice by inhibiting the MAPK pathway [J]. Journal of Southern Medical University, 2022, 42(12): 1815-1821. |
| [6] | . Effects of cholestasis and hypoxic hepatitis on prognosis of ICU patients: a retrospective study based on MIMIC III database [J]. Journal of Southern Medical University, 2020, 40(06): 771-777. |
| [7] | . Role of endoplasmic reticulum stress- induced apoptosis of trophoblasts in intrahepatic cholestasis during pregnancy [J]. Journal of Southern Medical University, 2018, 38(05): 572-. |
| [8] |
.
Effect of probucol in improving hepatic steatosis in rats with non-alcoholic steatohepatitis and the mechanism [J]. Journal of Southern Medical University, 2014, 34(05): 731-. |
| [9] | . Effects of farnesoid X receptor agonist on adiponectin and its receptors [J]. Journal of Southern Medical University, 2014, 34(01): 109-. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||