Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (2): 296-303.doi: 10.12122/j.issn.1673-4254.2025.02.10
Mengyao XIE( ), Min YANG, Xin LI, Yonghong DU(
), Min YANG, Xin LI, Yonghong DU( )
)
Received:2024-07-17
Online:2025-02-20
Published:2025-03-03
Contact:
Yonghong DU
E-mail:1049424697@qq.com;duyonghong@cqmu.edu.cn
Mengyao XIE, Min YANG, Xin LI, Yonghong DU. Low-intensity pulsed ultrasound combined with nystatin treatment synergistically inhibits vaginal Candida albicans biofilm infection in rabbits[J]. Journal of Southern Medical University, 2025, 45(2): 296-303.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.02.10
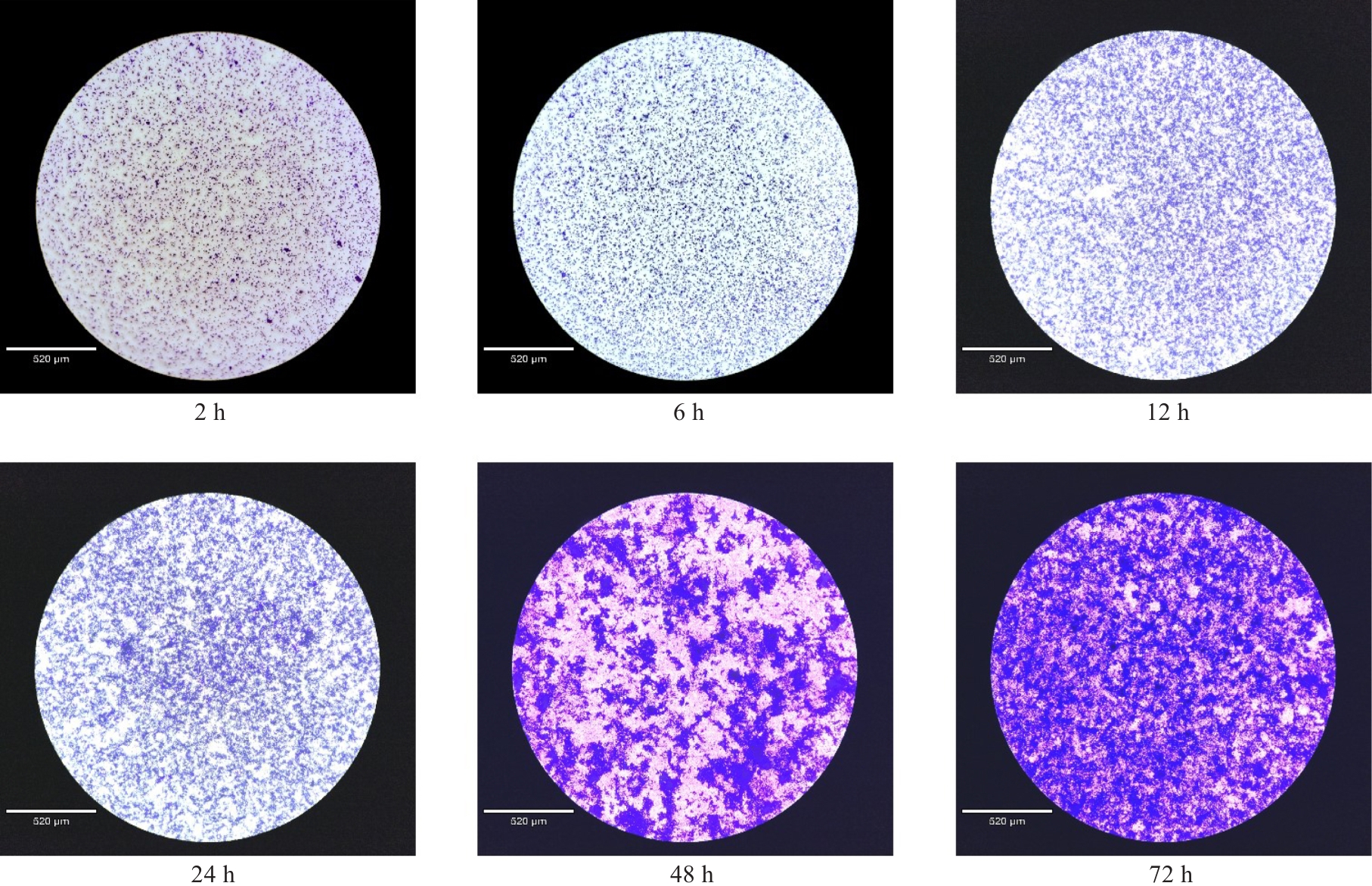
Fig.1 Crystalline violet staining and microscopic observation of changes in the structure of Candida albicans biofilm from 2 h to 72 h in culture (scale bar=520 μm).
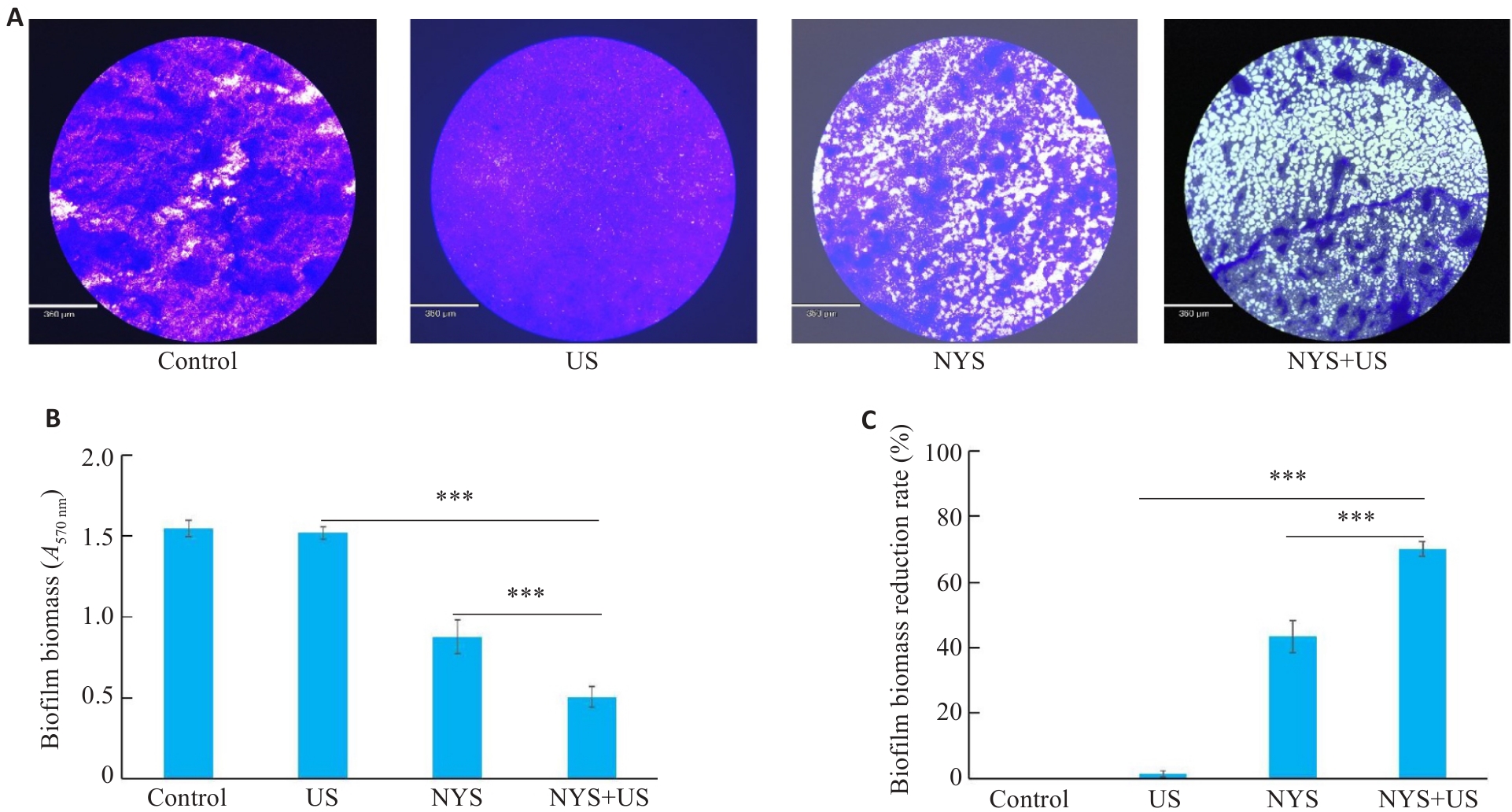
Fig.2 Quantification of Candida albicans biofilm by crystalline violet staining. A: Crystalline violet staining to observe the changes in the structural characteristics of biofilm after different treatments (Scale bar=360 μm). B: Detection of A570 nm of crystal violet stained biofilm by enzyme marker. C: Biofilm reduction rate after different treatments. ***P<0.001.
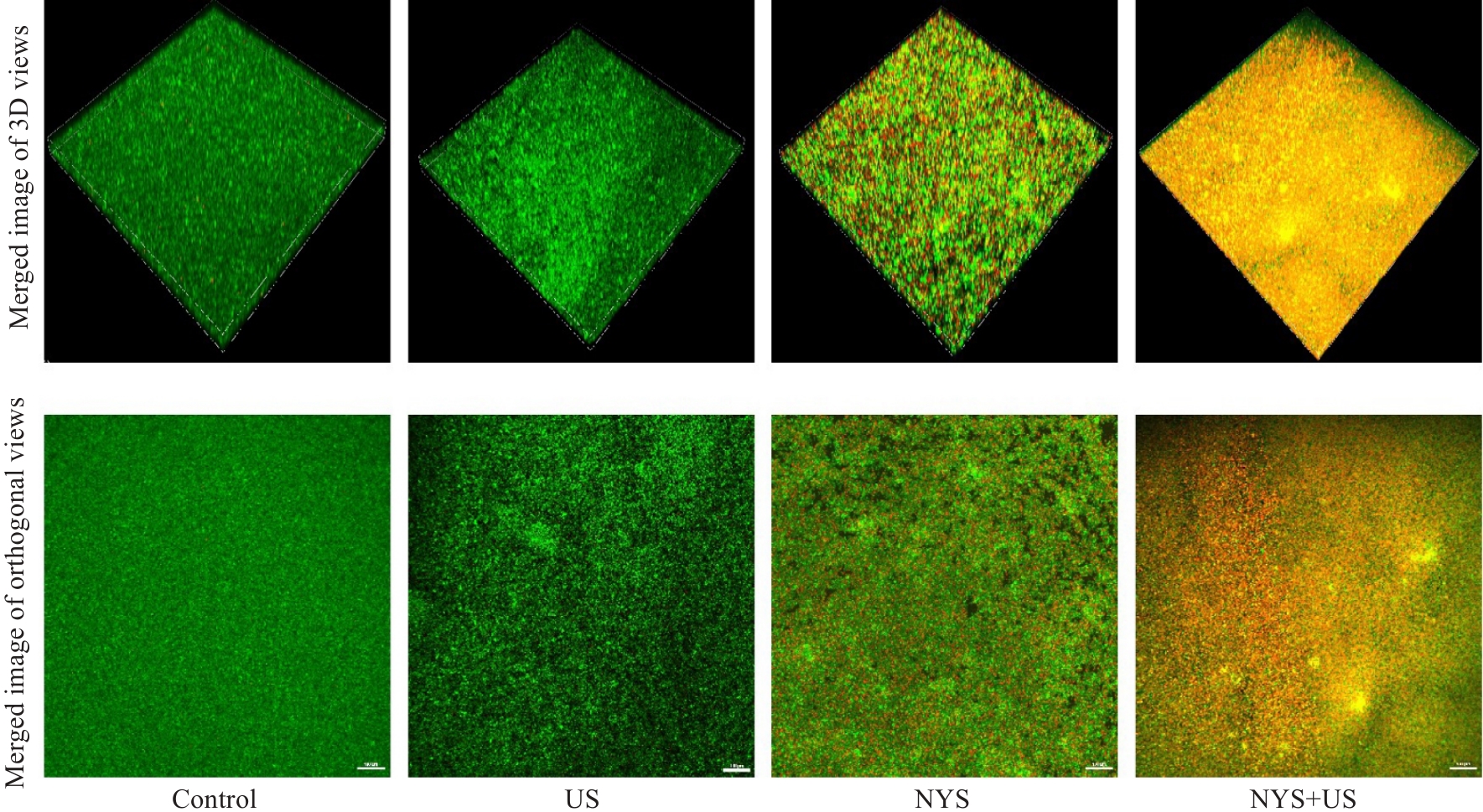
Fig.3 Confocal laser scanning microscopy for observing 3D and orthogonal views of Candida albicans biofilm activity after different treatments (scale bar=100 μm). Green and red fluorescence signals represent live and dead fungi, respectively.
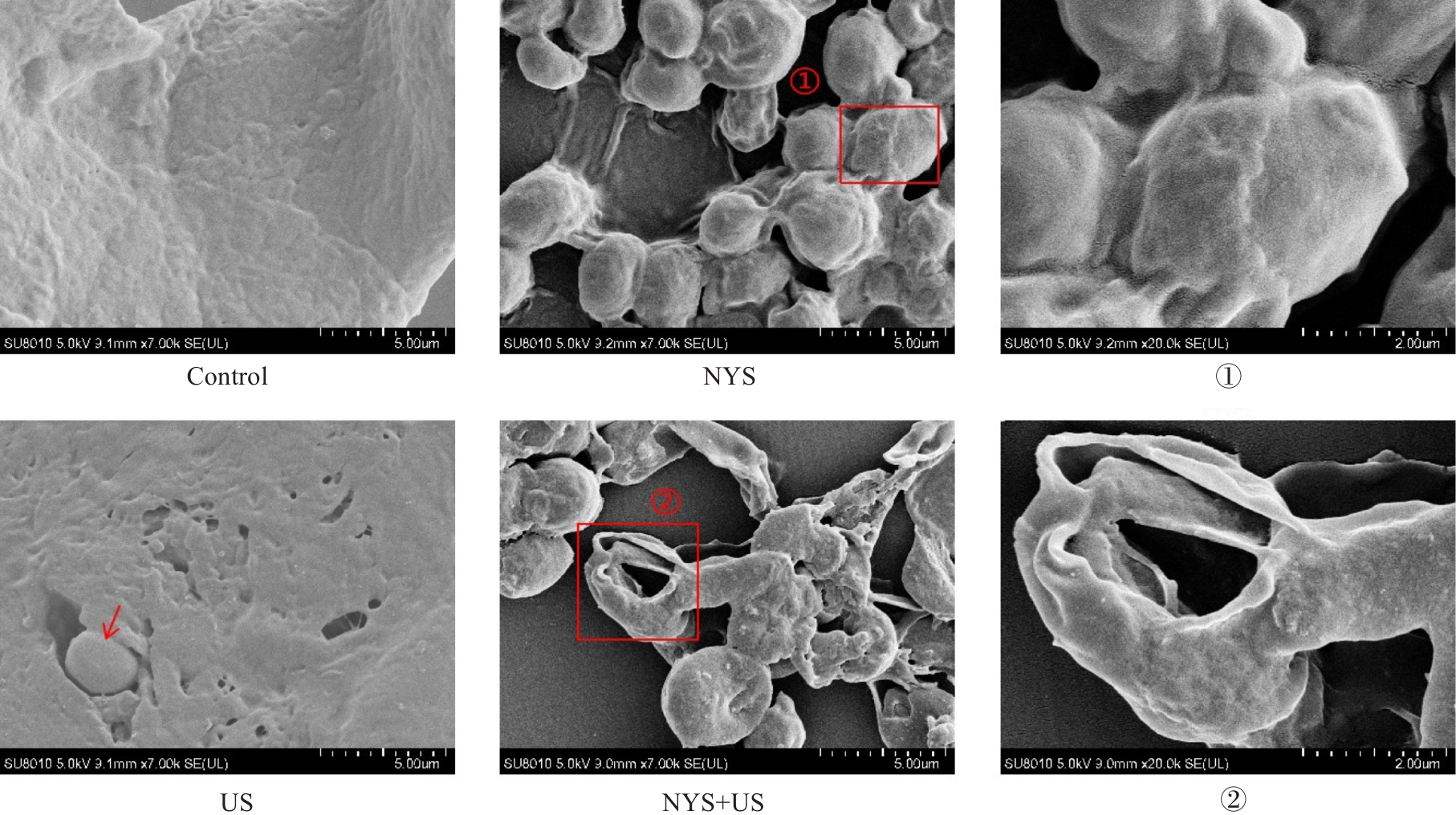
Fig.4 Scanning electron microscopy for observing Candida albicans biofilm ultrastructure. ①Partial magnification of the dense biofilm structure destroyed and Candida albicans exposed inside the membrane after nystatin (NYS) treatment; ② Partial magnification of severely destroyed structure of Candida albicans inside the biofilm after NYS combined with ultrasound treatment. Red arrows represent exposed Candida albicans. Scale bar: 5 μm; ①, ② Scale bar=2 μm.
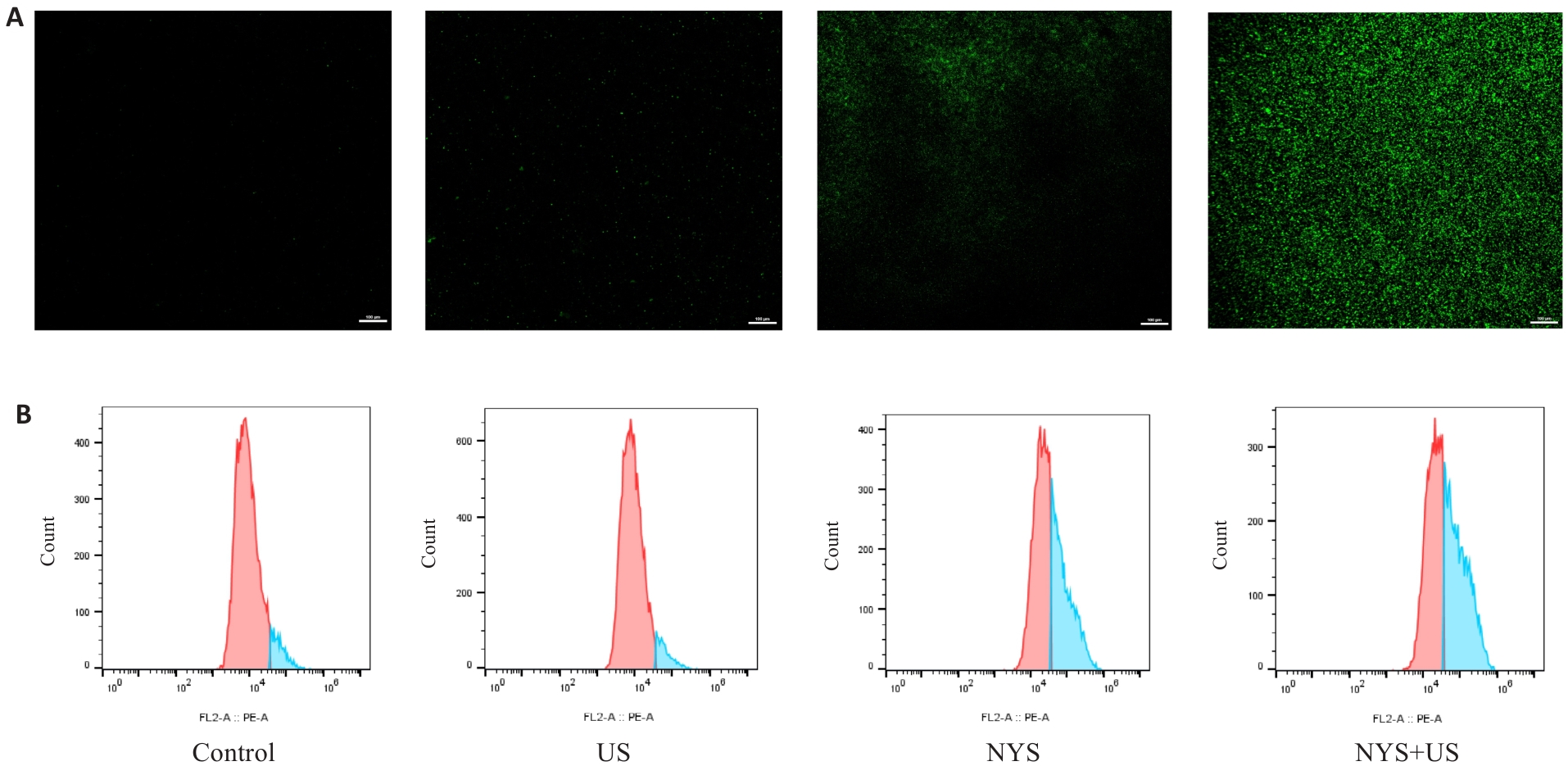
Fig.5 Production of ROS by Candida albicans biofilm in each group. A: Confocal laser scanning microscopy for observing ROS fluorescence (green) intensity produced by the biofilm after different treatment (scale bar=100 μm). B: Flow cytometry detection of ROS fluorescence intensity produced by the biofilms in each group (the horizontal coordinate represents the fluorescence intensity and the vertical coordinate represents the number of cells).
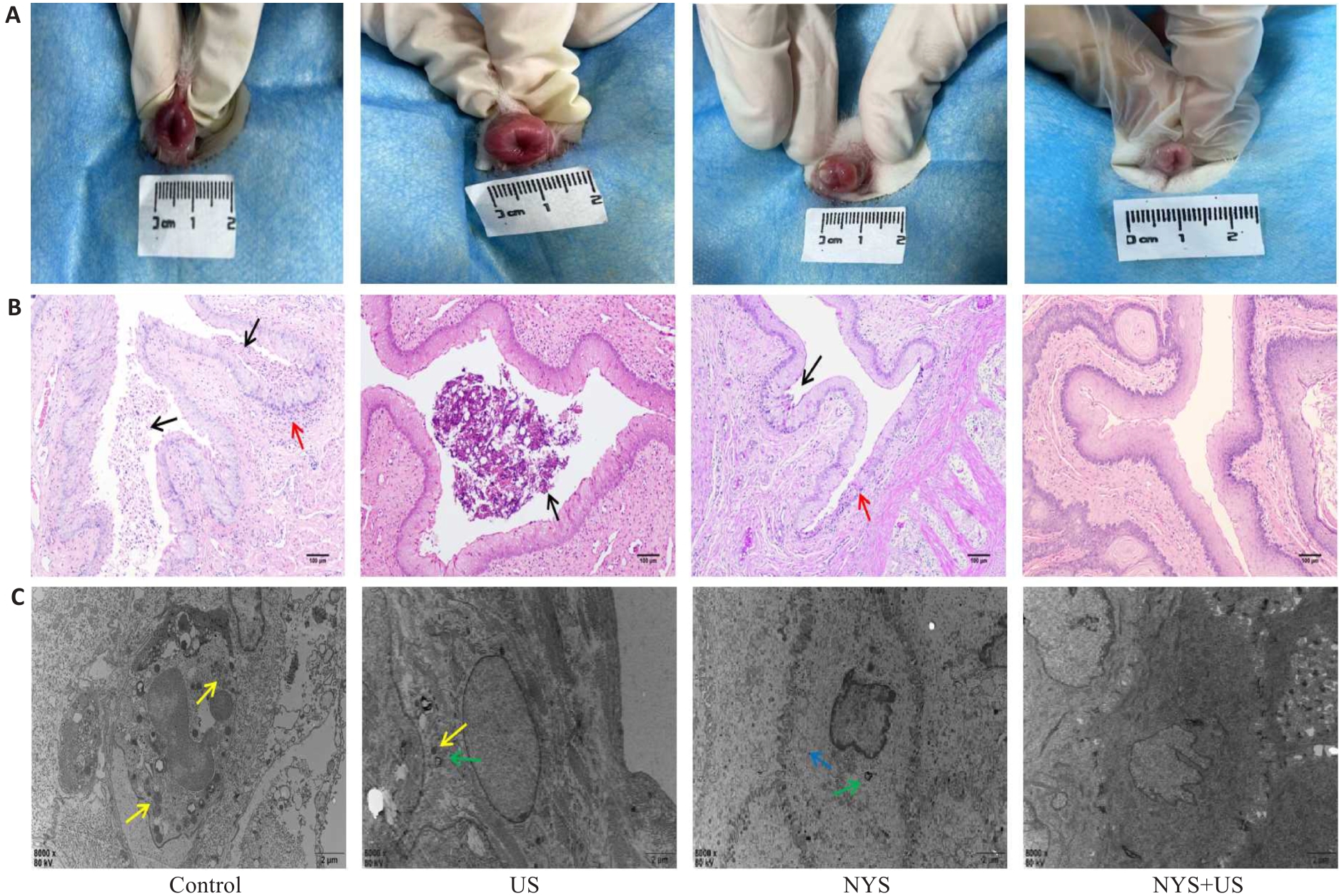
Fig.6 Assessment of treatment efficacy against Candida albicans vaginal biofilm infections in the rabbits. A: Vulvar symptoms of the rabbits after 7 days of continuous treatment. B: HE staining of the vaginal tissues after 7 days of treatment (black arrows indicate Candida albicans aggregation and red arrows indicate submucosal inflammatory infiltration. scale bar=100 μm). C: Transmission electron microscopy of observing vaginal epithelial ultrastructure (scale bar=2 μm). Yellow arrows indicate Candida albicans infection, green arrows indicate infiltrated neutrophils, and blue arrows indicate swollen mitochondria.
| 1 | Macias-Paz IU, Pérez-Hernández S, Tavera-Tapia A, et al. Candida albicans the main opportunistic pathogenic fungus in humans[J]. Rev Argent Microbiol, 2023, 55(2): 189-98. |
| 2 | 瞿 嵘, 蔡绍曦, 佟万成, 等. 呼吸机相关性肺部念珠菌感染危险因素及耐药分析[J]. 南方医科大学学报, 2009, 29(1): 57-9. |
| 3 | de Oliveira DC, Silva LB, da Silva BV, et al. A new acridone with antifungal properties against Candida spp. and dermatophytes, and antibiofilm activity against C. albicans[J]. J Appl Microbiol, 2019, 127(5): 1362-72. |
| 4 | Pierce CG, Vila T, Romo JA, et al. The Candida albicans biofilm matrix: composition, structure and function[J]. J Fungi, 2017, 3(1): 14. |
| 5 | Chandra J, Kuhn DM, Mukherjee PK, et al. Biofilm formation by the fungal pathogen Candida albicans: development, architecture, and drug resistance[J]. J Bacteriol, 2001, 183(18): 5385-94. |
| 6 | Muzny CA, Schwebke JR. Biofilms: an underappreciated mechanism of treatment failure and recurrence in vaginal infections[J]. Clin Infect Dis, 2015, 61(4): 601-6. |
| 7 | Achkar JM, Fries BC. Candida infections of the genitourinary tract[J]. Clin Microbiol Rev, 2010, 23(2): 253-73. |
| 8 | Chew SY, Than LTL. Vulvovaginal candidosis: contemporary challenges and the future of prophylactic and therapeutic approaches[J]. Mycoses, 2016, 59(5): 262-73. |
| 9 | Harriott MM, Lilly EA, Rodriguez TE, et al. Candida albicans forms biofilms on the vaginal mucosa[J]. Microbiology, 2010, 156(Pt 12): 3635-44. |
| 10 | Lacroix G, Gouyer V, Gottrand F, et al. The cervicovaginal mucus barrier[J]. Int J Mol Sci, 2020, 21(21): 8266. |
| 11 | 郭 霜, 满江位, 姜春倩, 等. 低强度脉冲超声的生物物理学效应及相关机制的研究进展[J]. 中国医学物理学杂志, 2019, 36(5): 605-9. |
| 12 | Greish K. Enhanced permeability and retention of macromolecular drugs in solid tumors: a royal gate for targeted anticancer nanomedicines[J]. J Drug Target, 2007, 15(7/8): 457-64. |
| 13 | Roy J, Pandey V, Gupta I, et al. Antibacterial sonodynamic therapy: current status and future perspectives[J]. ACS Biomater Sci Eng, 2021, 7(12): 5326-38. |
| 14 | Mendling W, Brasch J, Cornely OA, et al. Guideline: vulvovaginal candidosis (AWMF 015/072), S2k (excluding chronic mucocutaneous candidosis)[J]. Mycoses, 2015, 58(): 1-15. |
| 15 | Coutinho A, Prieto M. Cooperative partition model of nystatin interaction with phospholipid vesicles[J]. Biophys J, 2003, 84(5): 3061-78. |
| 16 | Yang M, Cao YC, Zhang ZF, et al. Low intensity ultrasound-mediated drug-loaded nanoparticles intravaginal drug delivery: an effective synergistic therapy scheme for treatment of vulvovaginal candidiasis[J]. J Nanobiotechnology, 2023, 21(1): 53. |
| 17 | Song RT, Yan F, Cheng M, et al. Ultrasound-assisted preparation of exopolysaccharide/nystatin nanoemulsion for treatment of vulvovaginal candidiasis[J]. Int J Nanomedicine, 2020, 15: 2027-44. |
| 18 | Donders G, Sziller IO, Paavonen J, et al. Management of recurrent vulvovaginal candidosis: narrative review of the literature and European expert panel opinion[J]. Front Cell Infect Microbiol, 2022, 12: 934353. |
| 19 | Sobel JD. Vulvovaginal candidosis[J]. Lancet, 2007, 369(9577): 1961-71. |
| 20 | Yu H, Chen SP, Cao P. Synergistic bactericidal effects and mechanisms of low intensity ultrasound and antibiotics against bacteria: a review[J]. Ultrason Sonochem, 2012, 19(3): 377-82. |
| 21 | Powell LC, Adams JYM, Quoraishi S, et al. Alginate oligosaccharides enhance the antifungal activity of nystatin against candidal biofilms[J]. Front Cell Infect Microbiol, 2023, 13: 1122340. |
| 22 | Janeth Rimachi Hidalgo K, Carmello JC, Carolina Jordão C, et al. Antimicrobial photodynamic therapy in combination with nystatin in the treatment of experimental oral candidiasis induced by Candida albicans resistant to fluconazole[J]. Pharmaceuticals, 2019, 12(3): 140. |
| 23 | Wang T, Ma W, Jiang ZN, et al. The penetration effect of HMME-mediated low-frequency and low-intensity ultrasound against the Staphylococcus aureus bacterial biofilm[J]. Eur J Med Res, 2020, 25(1): 51. |
| 24 | Xu PY, Kumar Kankala R, Wang SB, et al. Sonodynamic therapy-based nanoplatforms for combating bacterial infections[J]. Ultrason Sonochem, 2023, 100: 106617. |
| 25 | Pericolini E, Gabrielli E, Ballet N, et al. Therapeutic activity of a Saccharomyces cerevisiae-based probiotic and inactivated whole yeast on vaginal candidiasis[J]. Virulence, 2017, 8(1): 74-90. |
| 26 | Sun CQ, Peng J, Yang LB, et al. A cecropin-4 derived peptide C18 inhibits Candida albicans by disturbing mitochondrial function[J]. Front Microbiol, 2022, 13: 872322. |
| 27 | Bujdáková H. Management of Candida biofilms: state of knowledge and new options for prevention and eradication[J]. Future Microbiol, 2016, 11(2): 235-51. |
| 28 | Sui X, Yan L, Jiang YY. The vaccines and antibodies associated with Als3p for treatment of Candida albicans infections[J]. Vaccine, 2017, 35(43): 5786-93. |
| 29 | Ouyang J, Tang ZM, Farokhzad N, et al. Ultrasound mediated therapy: Recent progress and challenges in nanoscience[J]. Nano Today, 2020, 35: 100949. |
| 30 | Greifová G, Májeková H, Greif G, et al. Analysis of antimicrobial and immunomodulatory substances produced by heterofermentative Lactobacillus reuteri [J]. Folia Microbiol, 2017, 62(6): 515-24. |
| [1] | ZHANG Zhifei, LIAO Hongjian, YANG Min, HU Can, DU Yonghong. Levofloxacin combined with cellulase can eradicate bacille Calmette-Guerin biofilm infection [J]. Journal of Southern Medical University, 2023, 43(2): 257-264. |
| [2] | TANG Wentao, DENG Juan, HE Sicheng, LI Junfen, ZHOU Yiqing, WANG Yan. Inhibitory effect of low-intensity pulsed ultrasound on apoptosis of splenic lymphocytes in septic rats [J]. Journal of Southern Medical University, 2023, 43(10): 1789-1795. |
| [3] | . Design, screening and antibacterial activity evaluation of the novel antibacterial peptide KR-1 [J]. Journal of Southern Medical University, 2021, 41(6): 923-930. |
| [4] | . Effects of low-intensity pulsed ultrasound on hematopoietic function in rats after combined chemotherapy with doxorubicin and cyclophosphamide [J]. Journal of Southern Medical University, 2019, 39(07): 836-. |
| [5] | . Effect of Klebsiella pneumoniae KbvR regulator on bacterial biofilm formation and capsular synthesis [J]. Journal of Southern Medical University, 2016, 36(10): 1435-. |
| [6] | . Effect of DNase I on biofilm formation of Staphylococcus aureus [J]. Journal of Southern Medical University, 2015, 35(09): 1356-. |
| [7] |
.
Construction and functional analysis of mscL knockout mutant of Staphylococcus epidermidis [J]. Journal of Southern Medical University, 2014, 34(10): 1426-. |
| [8] | . Effect of antibacterial peptide LL-37 on the integrity of Acinetobacter baumannii biofilm [J]. Journal of Southern Medical University, 2014, 34(03): 426-. |
| [9] | WANG Ying-bin1,3, WANG Hong2, GUO Hui-yu3, ZHAO Yong-zhong2, LUO Shen-qiu2. Analysis of ERG11 gene mutation in Candida albicans [J]. Journal of Southern Medical University, 2005, 25(11): 1390-1393. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||