Journal of Southern Medical University ›› 2024, Vol. 44 ›› Issue (9): 1637-1644.doi: 10.12122/j.issn.1673-4254.2024.09.02
Previous Articles Next Articles
Yingbo LI, Han BAO, Sen ZHANG( ), Jingxin MENG(
), Jingxin MENG( )
)
Received:2024-09-06
Online:2024-09-20
Published:2024-09-30
Contact:
Jingxin MENG
E-mail:zhangsen20@mails.ucas.ac.cn;mengjx628@mail.ipc.ac.cn
Yingbo LI, Han BAO, Sen ZHANG, Jingxin MENG. Recent advances in responsive isolation, release and clinical application of circulating tumor cells[J]. Journal of Southern Medical University, 2024, 44(9): 1637-1644.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2024.09.02
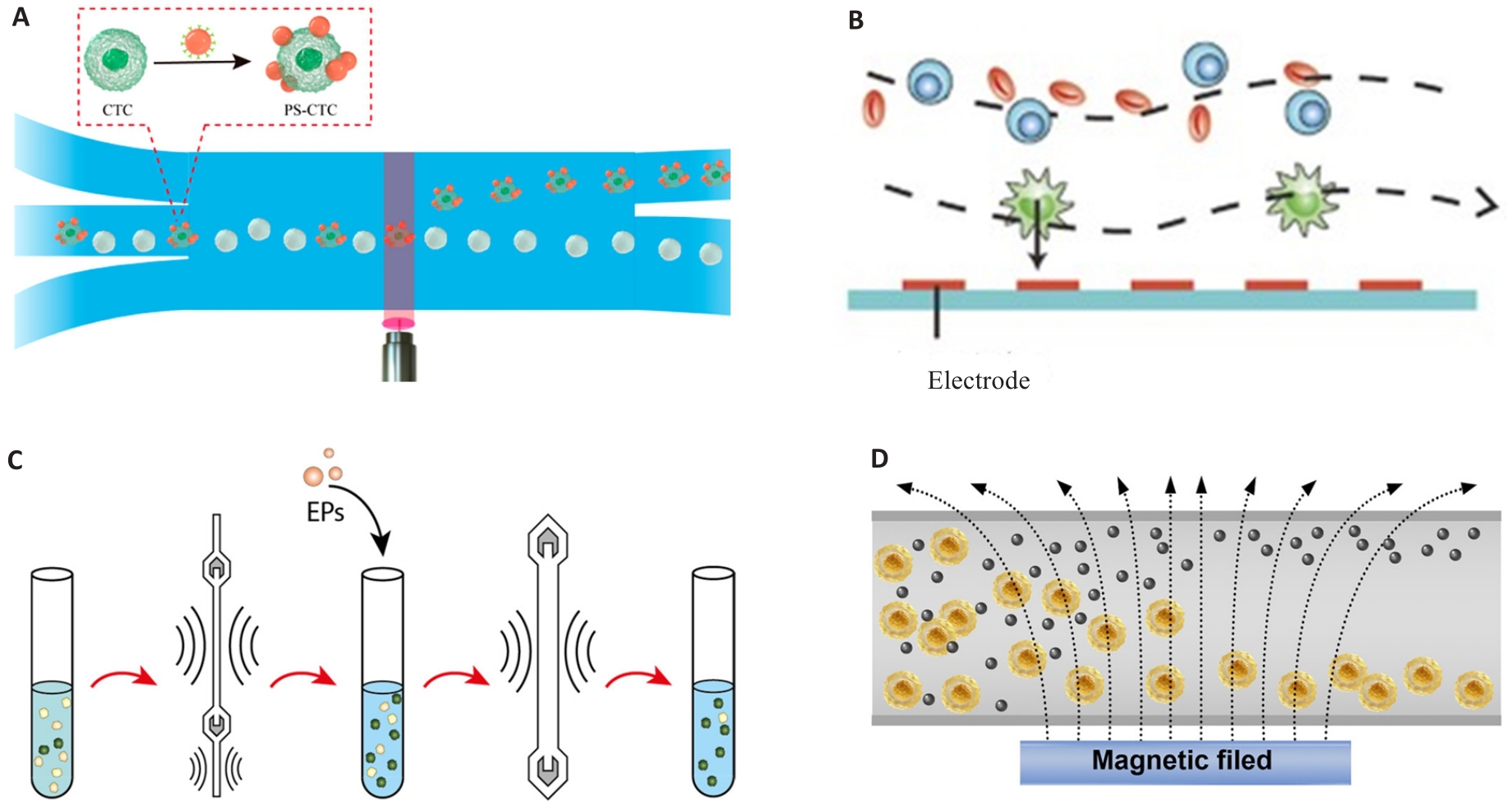
Fig.1 CTC responsive isolation based on physical characteristics. A: Light manipulation. Reproduced with permission[27]. Copyright 2022, American Chemical Society. B: Dielectrophoresis. Reproduced with permission[28]. Copyright 2015, Wiley-VCH. C: Acoustophoresis. Reproduced with permission[31]. Copyright 2021, American Chemical Society. D: Magnetophoresis. Reproduced with permission[35]. Copyright 2023, Wiley-VCH.
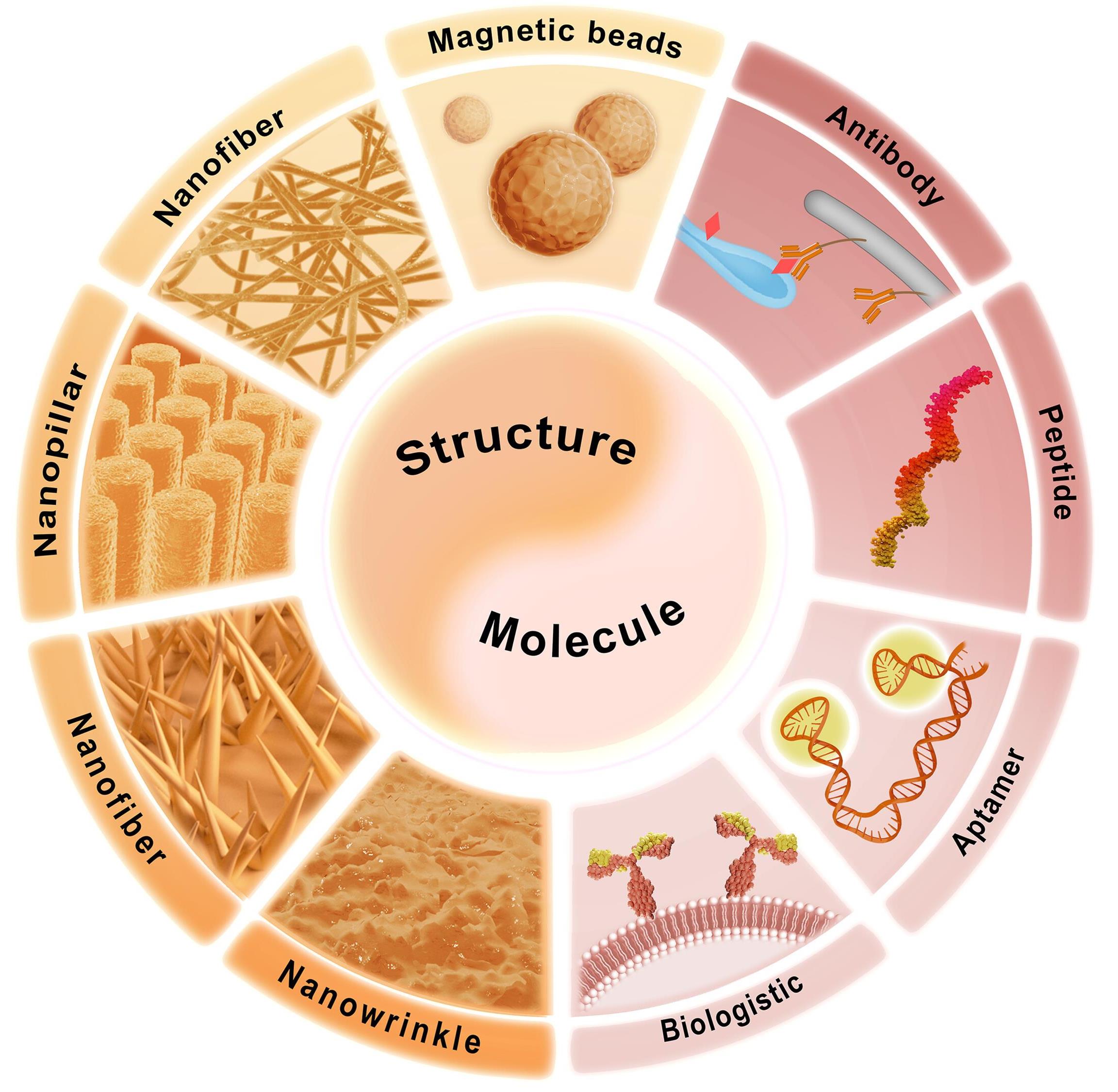
Fig.2 CTC isolation based on chemical features. The combination of specific molecule and topological structure enables the isolation of CTCs. Specific molecules include antibody, peptide, aptamer, and hybrid cell membrane. The topological structure includes magnetic beads, nanofiber, nanopillar, nanowire, and nanowrinkle. Reproduced with permission[35]. Copyright 2023, Wiley-VCH.
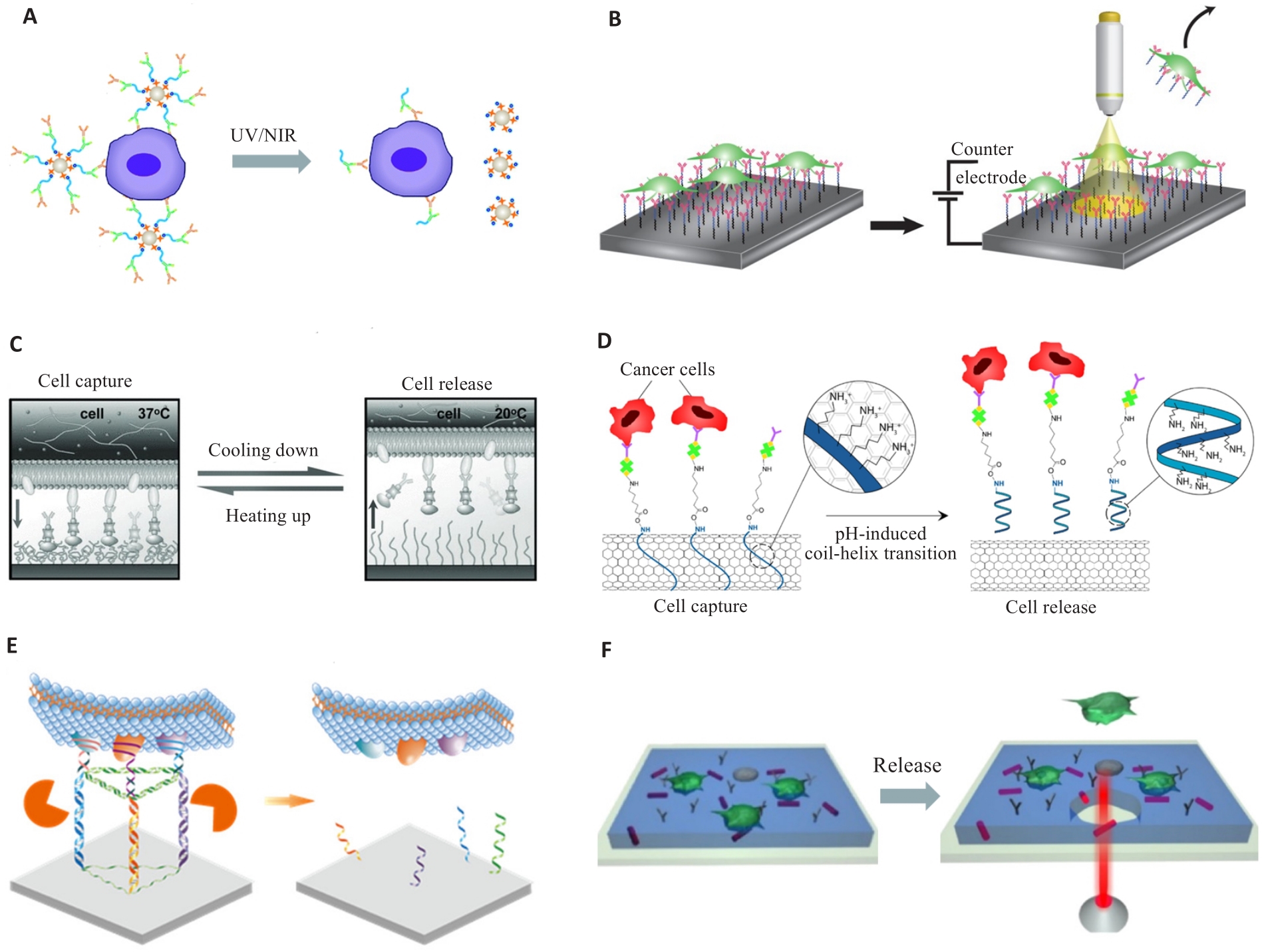
Fig.3 Responsive release of the CTCs. A: Light-response. Reproduced with permission[72]. Copyright 2015, The Royal Society of Chemistry. B: Electro-response. Reproduced with permission[68]. Copyright 2018, Springer Nature. C: Thermo-response. Reproduced with permission[69]. Copyright 2013, WILEY-VCH. D: pH-response. Reproduced with permission[21]. Copyright 2022, American Chemical Society. E: Enzyme-response. Reproduced with permission[73]. Copyright 2022, American Chemical Society. F: Substrate break. Reproduced with permission[71]. Copyright 2016, American Chemical Society.
| 1 | Siravegna G, Marsoni S, Siena S, et al. Integrating liquid biopsies into the management of cancer[J]. Nat Rev Clin Oncol, 2017, 14(9): 531-48. |
| 2 | Nonaka T, Wong DTW. Saliva diagnostics[J]. Annu Rev Anal Chem, 2022, 15(1): 107-21. |
| 3 | Oshi M, Murthy V, Takahashi H, et al. Urine as a source of liquid biopsy for cancer[J]. Cancers, 2021, 13(11): 2652. |
| 4 | Pantel K, Alix-Panabières C. Liquid biopsy and minimal residual disease-latest advances and implications for cure[J]. Nat Rev Clin Oncol, 2019, 16: 409-24. |
| 5 | De Rubis G, Rajeev Krishnan S, Bebawy M. Liquid biopsies in cancer diagnosis, monitoring, and prognosis[J]. Trends Pharmacol Sci, 2019, 40(3): 172-86. |
| 6 | Ahn JC, Teng PC, Chen PJ, et al. Detection of circulating tumor cells and their implications as a biomarker for diagnosis, prognostication, and therapeutic monitoring in hepatocellular carcinoma[J]. Hepatology, 2021, 73(1): 422-36. |
| 7 | Alix-Panabières C, Pantel K. Clinical applications of circulating tumor cells and circulating tumor DNA as liquid biopsy[J]. Cancer Discov, 2016, 6(5): 479-91. |
| 8 | Wang BS, Zhang SD, Meng JX, et al. Evaporation-induced rGO coatings for highly sensitive and non-invasive diagnosis of prostate cancer in the PSA gray zone[J]. Adv Mater, 2021, 33(40): e2103999. |
| 9 | Luo Q, Wang CM, Peng BJ, et al. Circulating tumor-cell-associated white blood cell clusters in peripheral blood indicate poor prognosis in patients with hepatocellular carcinoma[J]. Front Oncol, 2020, 10: 1758. |
| 10 | Zeinali M, Lee M, Nadhan A, et al. High-throughput label-free isolation of heterogeneous circulating tumor cells and CTC clusters from non-small-cell lung cancer patients[J]. Cancers, 2020, 12(1): 127. |
| 11 | Cristofanilli M, Budd GT, Ellis MJ, et al. Circulating tumor cells, disease progression, and survival in metastatic breast cancer[J]. N Engl J Med, 2004, 351(8): 781-91. |
| 12 | Chaffer CL, Weinberg RA. A perspective on cancer cell metastasis[J]. Science, 2011, 331(6024): 1559-64. |
| 13 | Nel I, Morawetz EW, Tschodu D, et al. The mechanical fingerprint of circulating tumor cells (CTCs) in breast cancer patients[J]. Cancers, 2021, 13(5): 1119. |
| 14 | Katz RL, Zaidi TM, Pujara D, et al. Identification of circulating tumor cells using 4-color fluorescence in situ hybridization: validation of a noninvasive aid for ruling out lung cancer in patients with low-dose computed tomography-detected lung nodules[J]. Cancer Cytopathol, 2020, 128(8): 553-62. |
| 15 | Paterlini-Brechot P, Benali NL. Circulating tumor cells (CTC) detection: clinical impact and future directions[J]. Cancer Lett, 2007, 253(2): 180-204. |
| 16 | Zhu S, Jiang FT, Han Y, et al. Microfluidics for label-free sorting of rare circulating tumor cells[J]. Analyst, 2020, 145(22): 7103-24. |
| 17 | Luo LA, He YQ. Magnetically driven microfluidics for isolation of circulating tumor cells[J]. Cancer Med, 2020, 9(12): 4207-31. |
| 18 | Min L, Wang BS, Bao H, et al. Advanced nanotechnologies for extracellular vesicle-based liquid biopsy[J]. Adv Sci, 2021, 8(20): e2102789. |
| 19 | Sun N, Yang YY, Miao H, et al. Discovery and characterization of circulating tumor cell clusters in neuroendocrine tumor patients using nanosubstrate-embedded microchips[J]. Biosens Bioelectron, 2022, 199: 113854. |
| 20 | Huang C, Yang G, Ha Q, et al. Multifunctional “smart” particles engineered from live immunocytes: toward capture and release of cancer cells[J]. Adv Mater, 2015, 27(2): 310-3. |
| 21 | Neoh KH, Cheng SKS, Wu HS, et al. pH-responsive carbon nanotube film-based microfluidic chip for efficient capture and release of cancer cells[J]. ACS Appl Nano Mater, 2022, 5(5): 6911-24. |
| 22 | Luo ZY, He Y, Li M, et al. Tumor microenvironment-inspired glutathione-responsive three-dimensional fibrous network for efficient trapping and gentle release of circulating tumor cells[J]. ACS Appl Mater Interfaces, 2023, 15(20): 24013-22. |
| 23 | Hu XJ, Zhu DM, Chen M, et al. Precise and non-invasive circulating tumor cell isolation based on optical force using homologous erythrocyte binding[J]. Lab Chip, 2019, 19(15): 2549-56. |
| 24 | Moon HS, Kwon K, Kim SI, et al. Continuous separation of breast cancer cells from blood samples using multi-orifice flow fractionation (MOFF) and dielectrophoresis (DEP)[J]. Lab Chip, 2011, 11(6): 1118-25. |
| 25 | Wu ZZ, Jiang HQ, Zhang LL, et al. The acoustofluidic focusing and separation of rare tumor cells using transparent lithium niobate transducers[J]. Lab Chip, 2019, 19(23): 3922-30. |
| 26 | Liu Y, Zhao WJ, Cheng R, et al. Fundamentals of integrated ferrohydrodynamic cell separation in circulating tumor cell isolation[J]. Lab Chip, 2021, 21(9): 1706-23. |
| 27 | Chen B, Zheng JJ, Gao KF, et al. Noninvasive optical isolation and identification of circulating tumor cells engineered by fluorescent microspheres[J]. ACS Appl Bio Mater, 2022, 5(6): 2768-76. |
| 28 | Qian WY, Zhang Y, Chen WQ. Capturing cancer: emerging microfluidic technologies for the capture and characterization of circulating tumor cells[J]. Small, 2015, 11(32): 3850-72. |
| 29 | Kwizera EA, Sun MR, White AM, et al. Methods of generating dielectrophoretic force for microfluidic manipulation of bioparticles[J]. ACS Biomater Sci Eng, 2021, 7(6): 2043-63. |
| 30 | Montoya Mira J, Sapre AA, Walker BS, et al. Label-free enrichment of rare unconventional circulating neoplastic cells using a microfluidic dielectrophoretic sorting device[J]. Commun Biol, 2021, 4(1): 1130. |
| 31 | Undvall Anand E, Magnusson C, Lenshof A, et al. Two-step acoustophoresis separation of live tumor cells from whole blood[J]. Anal Chem, 2021, 93(51): 17076-85. |
| 32 | Jiang YQ, Chen J, Xuan WP, et al. Numerical study of particle separation through integrated multi-stage surface acoustic waves and modulated driving signals[J]. Sensors, 2023, 23(5): 2771. |
| 33 | Cui MY, Kim M, Weisensee PB, et al. Thermal considerations for microswimmer trap-and-release using standing surface acoustic waves[J]. Lab Chip, 2021, 21(13): 2534-43. |
| 34 | Schulze K, Gasch C, Staufer K, et al. Presence of EpCAM-positive circulating tumor cells as biomarker for systemic disease strongly correlates to survival in patients with hepatocellular carcinoma[J]. Int J Cancer, 2013, 133(9): 2165-71. |
| 35 | Bao H, Min L, Bu FQ, et al. Recent advances of liquid biopsy: interdisciplinary strategies toward clinical decision-making[J]. Interdiscip Med, 2023, 1(4): e20230021. |
| 36 | Nagrath S, Sequist LV, Maheswaran S, et al. Isolation of rare circulating tumour cells in cancer patients by microchip technology[J]. Nature, 2007, 450(7173): 1235-9. |
| 37 | Maheswaran S, Sequist LV, Nagrath S, et al. Detection of mutations in EGFR in circulating lung-cancer cells[J]. N Engl J Med, 2008, 359(4): 366-77. |
| 38 | Riethdorf S, Müller V, Zhang LL, et al. Detection and HER2 expression of circulating tumor cells: prospective monitoring in breast cancer patients treated in the neoadjuvant GeparQuattro trial[J]. Clin Cancer Res, 2010, 16(9): 2634-45. |
| 39 | Liu H, Wang ZL, Chen CC, et al. Dual-antibody modified PLGA nanofibers for specific capture of epithelial and mesenchymal CTCs[J]. Colloids Surf B Biointerfaces, 2019, 181: 143-8. |
| 40 | Zhang T, Boominathan R, Foulk B, et al. Development of a novel c-MET-based CTC detection platform[J]. Mol Cancer Res, 2016, 14(6): 539-47. |
| 41 | Jia F, Wang YH, Fang ZG, et al. Novel peptide-based magnetic nanoparticle for mesenchymal circulating tumor cells detection[J]. Anal Chem, 2021, 93(14): 5670-5. |
| 42 | Wu ZE, Pan Y, Wang ZL, et al. A PLGA nanofiber microfluidic device for highly efficient isolation and release of different phenotypic circulating tumor cells based on dual aptamers[J]. J Mater Chem B, 2021, 9(9): 2212-20. |
| 43 | Chang ZM, Zhang R, Yang C, et al. Cancer-leukocyte hybrid membrane-cloaked magnetic beads for the ultrasensitive isolation, purification, and non-destructive release of circulating tumor cells[J]. Nanoscale, 2020, 12(37): 19121-8. |
| 44 | Li YY, Lu QH, Liu HL, et al. Antibody-modified reduced graphene oxide films with extreme sensitivity to circulating tumor cells[J]. Adv Mater, 2015, 27(43): 6848-54. |
| 45 | Wang WS, Yang G, Cui HJ, et al. Bioinspired pollen-like hierarchical surface for efficient recognition of target cancer cells[J]. Adv Healthc Mater, 2017, 6(15): 1700003. |
| 46 | Wang ST, Liu K, Liu J, et al. Highly efficient capture of circulating tumor cells by using nanostructured silicon substrates with integrated chaotic micromixers[J]. Angew Chem Int Ed, 2011, 50(13): 3084-8. |
| 47 | Genna A, Vanwynsberghe AM, Villard AV, et al. EMT-associated heterogeneity in circulating tumor cells: sticky friends on the road to metastasis[J]. Cancers, 2020, 12(6): 1632. |
| 48 | Liang NX, Liu L, Li P, et al. Efficient isolation and quantification of circulating tumor cells in non-small cell lung cancer patients using peptide-functionalized magnetic nanoparticles[J]. J Thorac Dis, 2020, 12(8): 4262-73. |
| 49 | Carmona-Ule N, Gal N, Abuín Redondo C, et al. Peptide-functionalized nanoemulsions as a promising tool for isolation and ex vivo culture of circulating tumor cells[J]. Bioengineering, 2022, 9(8): 380. |
| 50 | Wu LL, Wang YD, Xu X, et al. Aptamer-based detection of circulating targets for precision medicine[J]. Chem Rev, 2021, 121(19): 12035-105. |
| 51 | Ling JJ, Liu D, Zhang JL, et al. Thermodynamic and kinetic modulation of microfluidic interfaces by DNA nanoassembly mediated merit-complementary heteromultivalency[J]. ACS Nano, 2022, 16(12): 20915-21. |
| 52 | Li JX, Yuan YG, Gan HY, et al. Double-tetrahedral DNA probe functionalized Ag nanorod biointerface for effective capture, highly sensitive detection, and nondestructive release of circulating tumor cells[J]. ACS Appl Mater Interfaces, 2022, 14(29): 32869-79. |
| 53 | Rao L, Meng QF, Huang QQ, et al. Platelet-leukocyte hybrid membrane-coated immunomagnetic beads for highly efficient and highly specific isolation of circulating tumor cells[J]. Adv Funct Mater, 2018, 28(34): 1803531. |
| 54 | Ronvaux L, Riva M, Coosemans A, et al. Liquid biopsy in glioblastoma[J]. Cancers, 2022, 14(14): 3394. |
| 55 | Jelski W, Mroczko B. Molecular and circulating biomarkers of gastric cancer[J]. Int J Mol Sci, 2022, 23(14): 7588. |
| 56 | Zigeuner RE, Riesenberg R, Pohla H, et al. Isolation of circulating cancer cells from whole blood by immunomagnetic cell enrichment and unenriched immunocytochemistry in vitro [J]. J Urol, 2003, 169(2): 701-5. |
| 57 | Song YY, Dong XF, Shang DY, et al. Unusual nanofractal microparticles for rapid protein capture and release[J]. Small, 2021, 17(36): e2102802. |
| 58 | Xiao YC, Lin LZ, Shen MW, et al. Design of DNA aptamer-functionalized magnetic short nanofibers for efficient capture and release of circulating tumor cells[J]. Bioconjug Chem, 2020, 31(1): 130-8. |
| 59 | Winograd P, Hou S, Court CM, et al. Hepatocellular carcinoma-circulating tumor cells expressing PD-L1 are prognostic and potentially associated with response to checkpoint inhibitors[J]. Hepatol Commun, 2020, 4(10): 1527-40. |
| 60 | Sun N, Zhang C, Wang J, et al. Hierarchical integration of DNA nanostructures and NanoGold onto a microchip facilitates covalent chemistry-mediated purification of circulating tumor cells in head and neck squamous cell carcinoma[J]. Nano Today, 2023, 49: 101786. |
| 61 | Meng JX, Liu HL, Liu XL, et al. Hierarchical biointerfaces assembled by leukocyte-inspired particles for specifically recognizing cancer cells[J]. Small, 2014, 10(18): 3735-41. |
| 62 | Gu CC, Hou T, Zhang SX, et al. Light-driven ultrasensitive self-powered cytosensing of circulating tumor cells via integration of biofuel cells and a photoelectrochemical strategy[J]. J Mater Chem B, 2019, 7(14): 2277-83. |
| 63 | Huang X, Hu XJ, Song S, et al. Triple-enhanced surface plasmon resonance spectroscopy based on cell membrane and folic acid functionalized gold nanoparticles for dual-selective circulating tumor cell sensing[J]. Sensor Actuat B-Chem, 2020, 305: 127543. |
| 64 | Ho LC, Wu WC, Chang CY, et al. Aptamer-conjugated polymeric nanoparticles for the detection of cancer cells through "turn-on" retro-self-quenched fluorescence[J]. Anal Chem, 2015, 87(9): 4925-32. |
| 65 | Chen B, Wang GG, Huang CY, et al. A light-induced hydrogel responsive platform to capture and selectively isolate single circulating tumor cells[J]. Nanoscale, 2022, 14(9): 3504-12. |
| 66 | Li MR, Liu J, Wang XT, et al. Facile preparation of three-dimensional wafer with interconnected porous structure for high-performance capture and nondestructive release of circulating tumor cells[J]. Anal Chem, 2022, 94(43): 15076-84. |
| 67 | Pahattuge TN, Jackson JM, Digamber R, et al. Visible photorelease of liquid biopsy markers following microfluidic affinity-enrichment[J]. Chem Commun, 2020, 56(29): 4098-101. |
| 68 | Parker SG, Yang Y, Ciampi S, et al. A photoelectrochemical platform for the capture and release of rare single cells[J]. Nat Commun, 2018, 9(1): 2288. |
| 69 | Liu HL, Liu XL, Meng JX, et al. Hydrophobic interaction-mediated capture and release of cancer cells on thermoresponsive nanostructured surfaces[J]. Adv Mater, 2013, 25(6): 922-7. |
| 70 | Meng JX, Zhang PC, Zhang FL, et al. A self-cleaning TiO2 nanosisal-like coating toward disposing nanobiochips of cancer detection[J]. ACS Nano, 2015, 9(9): 9284-91. |
| 71 | Lv SW, Liu Y, Xie M, et al. Near-infrared light-responsive hydrogel for specific recognition and photothermal site-release of circulating tumor cells[J]. ACS Nano, 2016, 10(6): 6201-10. |
| 72 | Lv SW, Wang J, Xie M, et al. Photoresponsive immunomagnetic nanocarrier for capture and release of rare circulating tumor cells[J]. Chem Sci, 2015, 6(11): 6432-8. |
| 73 | Liu Y, Lin Z, Zheng ZW, et al. Accurate isolation of circulating tumor cells via a heterovalent DNA framework recognition element-functionalized microfluidic chip[J]. ACS Sens, 2022, 7(2): 666-73. |
| 74 | Mei ZF, Yan J, Qian L, et al. Enrichment of circulating tumor cells of lung cancer and correlation with serum leukomonocyte and tumor biomarkers: a retrospective study[J]. Technol Cancer Res Treat, 2023, 22: 15330338231167827. |
| 75 | Zhou JM, Zhang ZW, Zhou HH, et al. Preoperative circulating tumor cells to predict microvascular invasion and dynamical detection indicate the prognosis of hepatocellular carcinoma[J]. BMC Cancer, 2020, 20(1): 1047. |
| 76 | Pei XM, Wong HT, Ng SSM, et al. The diagnostic significance of CDH17-positive circulating tumor cells in patients with colorectal cancer[J]. Expert Rev Mol Diagn, 2023, 23(2): 171-9. |
| 77 | Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries[J]. CA Cancer J Clin, 2021, 71(3): 209-49. |
| 78 | Lindsay CR, Blackhall FH, Carmel A, et al. EPAC-lung: pooled analysis of circulating tumour cells in advanced non-small cell lung cancer[J]. Eur J Cancer, 2019, 117: 60-8. |
| 79 | Wang CM, Luo Q, Huang WB, et al. Correlation between circulating tumor cell DNA genomic alterations and mesenchymal CTCs or CTC-associated white blood cell clusters in hepatocellular carcinoma[J]. Front Oncol, 2021, 11: 686365. |
| 80 | Magri V, Marino L, Nicolazzo C, et al. Prognostic role of circulating tumor cell trajectories in metastatic colorectal cancer[J]. Cells, 2023, 12(8): 1172. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||