南方医科大学学报 ›› 2025, Vol. 45 ›› Issue (12): 2718-2725.doi: 10.12122/j.issn.1673-4254.2025.12.19
• • 上一篇
郭旋1,2( ), 刘洋1, 熊燕1, 刘镖水1, 宋婷2, 李云飞1(
), 刘洋1, 熊燕1, 刘镖水1, 宋婷2, 李云飞1( )
)
收稿日期:2025-05-13
出版日期:2025-12-20
发布日期:2025-12-22
通讯作者:
李云飞
E-mail:guoxuan@sysucc.org.cn;liyf1@syusucc.org.cn
作者简介:郭 旋,硕士,技师,E-mail: guoxuan@sysucc.org.cn
基金资助:
Xuan GUO1,2( ), Yang LIU1, Yan XIONG1, Biaoshui LIU1, Ting SONG2, Yunfei LI1(
), Yang LIU1, Yan XIONG1, Biaoshui LIU1, Ting SONG2, Yunfei LI1( )
)
Received:2025-05-13
Online:2025-12-20
Published:2025-12-22
Contact:
Yunfei LI
E-mail:guoxuan@sysucc.org.cn;liyf1@syusucc.org.cn
Supported by:摘要:
目的 通过量化分析4种固定装置在前列腺癌放疗中的摆位误差,评估其精度差异并探讨影响因素,为临床选择最优固定方案提供依据。 方法 回顾性分析中山大学肿瘤防治中心2016年5月~2024年5月240例进行图像引导放疗的前列腺癌患者,按固定装置分为4组:1.2 m真空袋组、1.8 m真空袋组、Orfit架组和个体化俯卧板组,60例/组。所有患者每次治疗前行锥形束CT(CBCT)扫描,采用X射线容积成像仪(XVI)系统灰度配准获取RL、SI、AP三维方向的摆位误差。对所有患者进一步按有无淋巴结照射(各120例)、年龄(<65岁,n=80;≥65,n=160)以及BMI分层(BMI<24 kg/m²,n=120;BMI≥24 kg/m²,n=120)进行亚组分析。 结果 4组在三维方向的摆位误差差异有统计学意义(P<0.05)。个体化俯卧板组RL(0.02±0.25)cm、SI(0.01±0.32)cm方向误差最小,但AP方向误差最大(-0.28±0.36)cm。淋巴结照射组在AP方向的误差(-0.22±0.36cm)高于无淋巴结组(-0.01±0.43 cm)(P<0.001)。BMI与SI方向误差呈负相关(R=-0.45,P<0.001),与年龄相关性无统计学意义(P>0.05)。 结论 个体化俯卧板在RL/SI方向的精度优势具有显著临床意义,但AP方向的系统误差问题亟待解决。对于接受淋巴结照射或BMI较低的患者群体,应当特别关注SI方向的摆位精度控制。本研究为前列腺癌精准放疗的固定装置选择和个体化治疗方案优化提供了更高级别的循证依据。
郭旋, 刘洋, 熊燕, 刘镖水, 宋婷, 李云飞. 图像引导下前列腺癌放疗固定装置的摆位误差与临床因素相关性分析[J]. 南方医科大学学报, 2025, 45(12): 2718-2725.
Xuan GUO, Yang LIU, Yan XIONG, Biaoshui LIU, Ting SONG, Yunfei LI. Analysis of setup errors and their correlation with clinical factors in image-guided radiotherapy for prostate cancer using different immobilization devices[J]. Journal of Southern Medical University, 2025, 45(12): 2718-2725.
| Metric | 1.2 m vacuum bag | 1.8 m vacuum bag | Orfit board | Individualized prone | χ²/F | P |
|---|---|---|---|---|---|---|
| Age (year, Mean±SD) | 64.2±7.8 | 65.1±8.2 | 63.8±6.9 | 65.5±7.5 | 0.78 | 0.505 |
| BMI (kg/m², Mean±SD) | 24.1±2.8 | 23.8±3.1 | 24.3±2.9 | 23.9±3.0 | 0.38 | 0.769 |
| Clinical stage [n (%)] | 2.15 | 0.542 | ||||
| T3 | 36 (60.0) | 33 (55.0) | 35 (58.3) | 35 (58.3) | ||
| T4 | 24 (40.0) | 27 (45.0) | 25 (41.7) | 25 (41.7) | ||
| Risk stratification [n (%)] | 1.08 | 0.782 | ||||
| Intermediate risk | 22 (36.7) | 20 (33.3) | 19 (31.7) | 23 (38.3) | ||
| High risk | 38 (63.3) | 40 (66.7) | 41 (68.3) | 37 (61.7) | ||
| Lymph node irradiation [n (%)] | 32 (53.3) | 30 (50.0) | 28 (46.7) | 30 (50.0) | 0.74 | 0.864 |
表1 4组患者基线资料比较
Tab.1 Comparison of baseline characteristics of the patients in the 4 groups (n=60)
| Metric | 1.2 m vacuum bag | 1.8 m vacuum bag | Orfit board | Individualized prone | χ²/F | P |
|---|---|---|---|---|---|---|
| Age (year, Mean±SD) | 64.2±7.8 | 65.1±8.2 | 63.8±6.9 | 65.5±7.5 | 0.78 | 0.505 |
| BMI (kg/m², Mean±SD) | 24.1±2.8 | 23.8±3.1 | 24.3±2.9 | 23.9±3.0 | 0.38 | 0.769 |
| Clinical stage [n (%)] | 2.15 | 0.542 | ||||
| T3 | 36 (60.0) | 33 (55.0) | 35 (58.3) | 35 (58.3) | ||
| T4 | 24 (40.0) | 27 (45.0) | 25 (41.7) | 25 (41.7) | ||
| Risk stratification [n (%)] | 1.08 | 0.782 | ||||
| Intermediate risk | 22 (36.7) | 20 (33.3) | 19 (31.7) | 23 (38.3) | ||
| High risk | 38 (63.3) | 40 (66.7) | 41 (68.3) | 37 (61.7) | ||
| Lymph node irradiation [n (%)] | 32 (53.3) | 30 (50.0) | 28 (46.7) | 30 (50.0) | 0.74 | 0.864 |
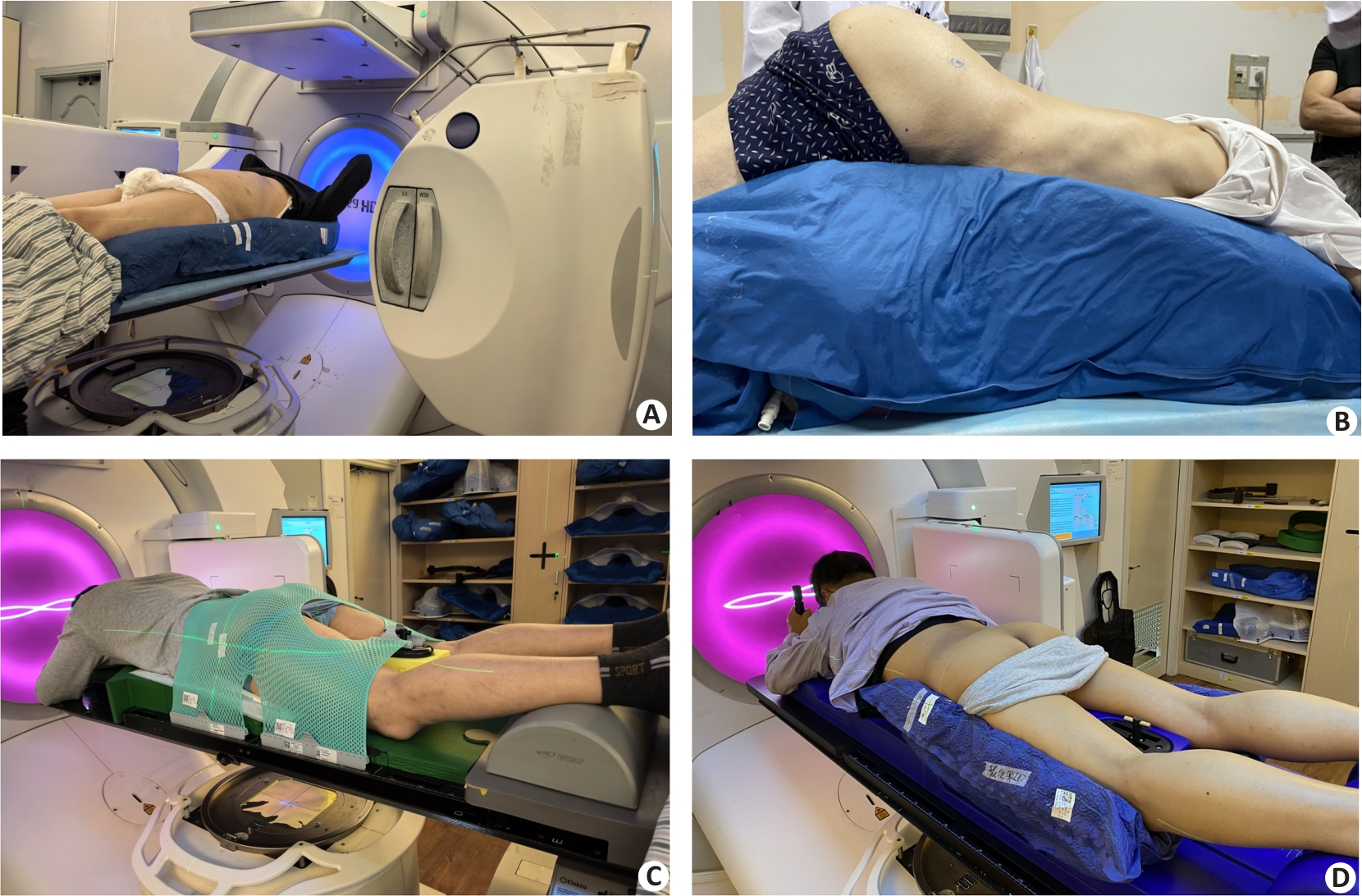
图1 4种固定装置示意图
Fig.1 Schematic illustration of the 4 types of fixation device. A: 1.2 m vacuum bag immobilization. B: 1.8 m vacuum bag immobilization. C: Orfit board immobilization. D: Individualized prone panel immobilization.
| Direction/devices | 1.2 m vacuum bag | 1.8 m vacuum bag | Orfit board | Individualized prone panel | P |
|---|---|---|---|---|---|
| R-Ldirection | 0.05±0.28 | 0.05±0.23 | -0.05±0.28*ΔΟ | 0.02±0.25 | <0.001 |
| S-Idirection | -0.06±0.36*▲ | 0.03±0.30 | -0.13±0.45*▲ | 0.01±0.32 | <0.001 |
| A-Pdirection | 0.03±0.24∆* | -0.10±0.42▲ | -0.02±0.21*▲ | -0.28±0.36Ο | <0.001 |
| ≥0.5 cm (%) | 15.0% | 11.67% | 13.33% | 18.33% | - |
表2 4种固定装置在三维方向上的摆位误差及两两比较
Tab.2 Positioning errors of the 4 fixing devices in 3-dimensional directions and pairwise comparisons (cm, Mean±SD)
| Direction/devices | 1.2 m vacuum bag | 1.8 m vacuum bag | Orfit board | Individualized prone panel | P |
|---|---|---|---|---|---|
| R-Ldirection | 0.05±0.28 | 0.05±0.23 | -0.05±0.28*ΔΟ | 0.02±0.25 | <0.001 |
| S-Idirection | -0.06±0.36*▲ | 0.03±0.30 | -0.13±0.45*▲ | 0.01±0.32 | <0.001 |
| A-Pdirection | 0.03±0.24∆* | -0.10±0.42▲ | -0.02±0.21*▲ | -0.28±0.36Ο | <0.001 |
| ≥0.5 cm (%) | 15.0% | 11.67% | 13.33% | 18.33% | - |
| Direction | R-L | S-I | A-P |
|---|---|---|---|
| Have lymph nodes | -0.04±0.30 | 0.003±0.35 | -0.22±0.36 |
| No lymph nodes | 0.002±0.29 | -0.075±0.47 | -0.01±0.43 |
| t | 2.14 | 3.46 | 4.27 |
| P | 0.033 | 0.001 | <0.001 |
表3 有无淋巴结(配准框大/小)在三维方向的摆位误差
Tab.3 Positioning errors in 3 directions in patients with or without lymph node irradiations (cm, Mean±SD)
| Direction | R-L | S-I | A-P |
|---|---|---|---|
| Have lymph nodes | -0.04±0.30 | 0.003±0.35 | -0.22±0.36 |
| No lymph nodes | 0.002±0.29 | -0.075±0.47 | -0.01±0.43 |
| t | 2.14 | 3.46 | 4.27 |
| P | 0.033 | 0.001 | <0.001 |
| Direction/devices | R-L | S-I | A-P | |
|---|---|---|---|---|
| 1.2 m vacuum bag | ∑ | 0.20 | 0.29 | 0.18 |
| σ | 0.21 | 0.25 | 0.17 | |
| MPTV | 0.64 | 0.9 | 0.57 | |
| 1.8 mvacuum bag | ∑ | 0.13 | 0.19 | 0.35 |
| σ | 0.08 | 0.91 | 0.14 | |
| MPTV | 0.81 | 1.11 | 0.97 | |
| Orfit board | ∑ | 0.23 | 0.35 | 0.19 |
| σ | 0.20 | 0.28 | 0.27 | |
| MPTV | 0.71 | 1.07 | 0.66 | |
| Individualized prone panel | ∑ | 0.15 | 0.20 | 0.26 |
| σ | 0.06 | 0.12 | 0.05 | |
| MPTV | 0.41 | 0.58 | 0.69 | |
| Individualized prone panel | ||||
| With lymph nodes | ∑ | 0.22 | 0.20 | 0.28 |
| σ | 0.07 | 0.07 | 0.09 | |
| MPTV | 0.59 | 0.55 | 0.77 | |
| Withoutlymph nodes | ∑ | 0.18 | 0.37 | 0.32 |
| σ | 0.07 | 0.07 | 0.13 | |
| MPTV | 0.51 | 0.97 | 0.88 | |
表4 4种固定装置之间PTV靶区外放比较 (cm)
Tab.4 Comparison of MPTV among the 4 fixation methods
| Direction/devices | R-L | S-I | A-P | |
|---|---|---|---|---|
| 1.2 m vacuum bag | ∑ | 0.20 | 0.29 | 0.18 |
| σ | 0.21 | 0.25 | 0.17 | |
| MPTV | 0.64 | 0.9 | 0.57 | |
| 1.8 mvacuum bag | ∑ | 0.13 | 0.19 | 0.35 |
| σ | 0.08 | 0.91 | 0.14 | |
| MPTV | 0.81 | 1.11 | 0.97 | |
| Orfit board | ∑ | 0.23 | 0.35 | 0.19 |
| σ | 0.20 | 0.28 | 0.27 | |
| MPTV | 0.71 | 1.07 | 0.66 | |
| Individualized prone panel | ∑ | 0.15 | 0.20 | 0.26 |
| σ | 0.06 | 0.12 | 0.05 | |
| MPTV | 0.41 | 0.58 | 0.69 | |
| Individualized prone panel | ||||
| With lymph nodes | ∑ | 0.22 | 0.20 | 0.28 |
| σ | 0.07 | 0.07 | 0.09 | |
| MPTV | 0.59 | 0.55 | 0.77 | |
| Withoutlymph nodes | ∑ | 0.18 | 0.37 | 0.32 |
| σ | 0.07 | 0.07 | 0.13 | |
| MPTV | 0.51 | 0.97 | 0.88 | |
| Variable | Group | n | RLError | SIError | APError | Statistical method | Statistic | P |
|---|---|---|---|---|---|---|---|---|
| Age (year) | <65 | 80 | 0.02±0.23 | -0.01±0.30 | -0.14±0.32 | Independent t-test | t=1.02 | 0.310 |
| ≥65 | 160 | 0.01±0.25 | 0.03±0.33 | -0.17±0.35 | ||||
| BMI (kg/m2) | <24 | 120 | -0.01±0.21 | -0.13±0.31 | -0.09±0.32 | Independent t-test | t=4.18 | <0.001* |
| ≥24 | 120 | -0.03±0.22 | 0.02±0.27 | -0.20±0.29 | ||||
| Correlation analysis | Age | r=0.03 | r=0.02 | r=-0.04 | Pearson correlation | >0.05 | ||
| BMI | R=-0.12 | r=-0.45 | r=-0.10 | Pearson correlation | <0.001* |
表5 年龄、BMI与摆位误差的相关性分析
Tab.5 Correlation analysis of age, BMI with setup errors (cm, Mean±SD)
| Variable | Group | n | RLError | SIError | APError | Statistical method | Statistic | P |
|---|---|---|---|---|---|---|---|---|
| Age (year) | <65 | 80 | 0.02±0.23 | -0.01±0.30 | -0.14±0.32 | Independent t-test | t=1.02 | 0.310 |
| ≥65 | 160 | 0.01±0.25 | 0.03±0.33 | -0.17±0.35 | ||||
| BMI (kg/m2) | <24 | 120 | -0.01±0.21 | -0.13±0.31 | -0.09±0.32 | Independent t-test | t=4.18 | <0.001* |
| ≥24 | 120 | -0.03±0.22 | 0.02±0.27 | -0.20±0.29 | ||||
| Correlation analysis | Age | r=0.03 | r=0.02 | r=-0.04 | Pearson correlation | >0.05 | ||
| BMI | R=-0.12 | r=-0.45 | r=-0.10 | Pearson correlation | <0.001* |
| [1] | Raychaudhuri R, Lin DW, Montgomery RB. Prostate cancer: areview[J]. JAMA, 2025, 333(16): 1433-46. doi:10.1001/jama.2025.0228 |
| [2] | 李 星, 曾晓勇. 中国前列腺癌流行病学研究进展[J]. 肿瘤防治研究, 2021, 48(1): 98-102. |
| [3] | Zhai Z, Zheng Y, Li N, et al. Incidence and disease burden of prostate cancer from 1990 to 2017: Results from the Global Burden of Disease Study 2017[J]. Cancer, 2020, 126(9): 1969-78. doi:10.1002/cncr.32733 |
| [4] | Tan EH, Burn E, Barclay NL, et al. Incidence, prevalence, and survival of prostate cancer in the UK[J]. JAMA Netw Open, 2024, 7(9): e2434622. doi:10.1001/jamanetworkopen.2024.34622 |
| [5] | Moll M, Nechvile E, Kirisits C, et al. Radiotherapy in localized prostate cancer: a multicenter analysis evaluating tumor control and late toxicity after brachytherapy and external beam radiotherapy in 1293 patients[J]. Strahlenther Onkol, 2024, 200(8): 698-705. doi:10.1007/s00066-024-02222-w |
| [6] | Inui S, Ueda Y, Ohira S, et al. Comparison of interfractional setup reproducibility between two types of patient immobilization devices in image-guided radiation therapy for prostate cancer[J]. J Med Phys, 2018, 43(4): 230-5. doi:10.4103/jmp.jmp_20_18 |
| [7] | 曹 飞, 赵永亮, 李 明, 等. 宫颈癌放疗仰、俯卧位固定下的摆位误差及剂量学差异探讨[J]. 现代肿瘤医学, 2019, 27(21): 3862-5. |
| [8] | 赵丰雨, 杜德成. 锥形束CT用于盆腔肿瘤放射治疗摆位中的效果分析[J]. 影像研究与医学应用, 2021, 5(4): 225-6. |
| [9] | Chen H, Liu YD, Qin SB, et al. Optical surface management system and BladderScan for patient setup during radiotherapy of postoperative prostate cancer[J]. Biomed Res Int, 2024, 2024: 3573796. doi:10.1155/2024/3573796 |
| [10] | 丘敏敏, 钟嘉健, 李 敏, 等. 鼻咽癌调强放疗摆位不同配准方式对实际剂量学的影响[J]. 中国医疗设备, 2020(11): 94-7, 101. |
| [11] | Anand M, Parikh A, Shah SP. Comparison of thermoplastic masks and knee wedge as immobilization devices for image-guided pelvic radiation therapy using Cone Beam Computed Tomography[J]. Indian J Cancer, 2020, 57(2): 182-6. doi:10.4103/ijc.ijc_602_18 |
| [12] | Wang L, Chen Z, Li X, et al.Setup errors in radiotherapy for prostate cancer: A retrospective analysis of Chinese patients with different immobilization techniques[J].Cancer Manag Res. 2020;12:12439-12447. |
| [13] | Inui S, Ueda Y, Ohira S, et al.Impact of body mass index on setup reproducibility in image-guided radiotherapy for prostate cancer[J]. J Appl Clin Med Phys, 2021, 22(3): 214-21. |
| [14] | Stroom JC, Heijmen BJ. Geometrical uncertainties, radiotherapy planning margins, and the ICRU-62 report[J]. Radiother Oncol, 2002, 64(1): 75-83. doi:10.1016/s0167-8140(02)00140-8 |
| [15] | Van HM, Remeijer P, Lebesque JV. Errors and margins in radiotherapy[J]. Semin Radiat Oncol, 2004, 14(1): 52-64. doi:10.1053/j.semradonc.2003.10.003 |
| [16] | Serizawa I, Kozuka T, Soyano T, et al. Clinical and dosimetric comparison between non-image guided radiation therapy and fiducial-based image guided radiation therapy with or without reduced margin in intensity modulated radiation therapy for prostate cancer[J]. Adv Radiat Oncol, 2024, 9(10): 101612. doi:10.1016/j.adro.2024.101612 |
| [17] | Mirzaei M, Gill S, Sabet M, et al. Treatment efficiency and quality improvement via double imaging modality (DIM) versus single imaging modality (SIM) image-guided radiotherapy for prostate cancer[J]. Tech Innov Patient Support Radiat Oncol, 2025, 33: 100307. doi:10.1016/j.tipsro.2025.100307 |
| [18] | Duffton A, McNee S, Muirhead R, et al. Clinical commissioning of online seed matching protocol for prostate radiotherapy[J]. Br J Radiol, 2012, 85(1020): e1273-81. doi:10.1259/bjr/72368557 |
| [19] | Greer PB, Dahl K, Ebert MA, et al. Comparison of prostate set-up accuracy and margins with off-line bony anatomy corrections and online implanted fiducial-based corrections[J]. J Med Imaging Radiat Oncol, 2008, 52(5): 511-6. doi:10.1111/j.1440-1673.2008.02005.x |
| [20] | 彭庆国, 尹 勇, 余宁莎,等. 三种体位固定技术在盆腔肿瘤放疗中的应用比较[J]. 中华肿瘤防治杂志, 2015, 22(12): 974-7, 983. |
| [21] | Guckenberger M, Meyer J, Wilbert J, et al. Cone-beam CT based image-guidance for extracranial stereotactic radiotherapy of intrapulmonary tumors[J]. Acta Oncol, 2006, 45(7): 897-906. doi:10.1080/02841860600904839 |
| [22] | Foster R, Meyer J, Iyengar P, et al. Localization accuracy and immobilization effectiveness of a stereotactic body frame for a variety of treatment sites[J]. Int J Radiat Oncol Biol Phys, 2013, 87(5): 911-6. doi:10.1016/j.ijrobp.2013.09.020 |
| [23] | Fonteyne V, Villeirs G, Speleers B, et al. Intensity-modulated radiotherapy as primary therapy for prostate cancer: report on acute toxicity after dose escalation with simultaneous integrated boost to intraprostatic lesion[J]. Int J Radiat Oncol Biol Phys, 2008, 72(3): 799-807. doi:10.1016/j.ijrobp.2008.01.040 |
| [24] | De Crevoisier R, Tucker SL, Dong L, et al. Increased risk of biochemical and local failure in patients with distended rectum on the planning CT for prostate cancer radiotherapy[J]. Int J Radiat Oncol Biol Phys, 2005, 62(4): 965-73. doi:10.1016/j.ijrobp.2004.11.032 |
| [25] | 黄伯天, 张丹丹, 彭应林, 等. 图像配准条件对头颈部CBCT引导放疗精度影响[J]. 中华放射肿瘤学杂志, 2016, 25(4): 391-4. |
| [26] | 彭清河, 彭应林, 朱金汉, 等. 图像配准方式对宫颈癌后装自适应放射治疗图像配准精度的影响[J]. 南方医科大学学报, 2018, 38(11): 1344-8. |
| [27] | Shinde P, Jadhav A, Shankar V, et al. Assessment of dosimetric impact of interfractional 6D setup error in tongue cancer treated with IMRT and VMAT using daily kV-CBCT[J]. Rep Pract Oncol Radiother, 2023, 28(2): 224-40. doi:10.5603/rpor.a2023.0020 |
| [28] | Dekker J, Essers M, Verheij M, et al. Dose coverage and breath-hold analysis of breast cancer patients treated with surface-guided radiotherapy[J]. Radiat Oncol, 2023, 18(1): 72. doi:10.1186/s13014-023-02261-0 |
| [29] | 李雅宁, 林承光, 杨 鑫. 体质量指数对宫颈癌调强放疗摆位误差影响[J]. 中华放射肿瘤学杂志, 2021, 30(2): 186-90. |
| [30] | Price RG, Lloyd S, Wang XC, et al. Adipose tissue distribution and body mass index (BMI) correlation with daily image-guided radiotherapy (IGRT) shifts of abdominal radiation therapy patients[J]. Cureus, 2023, 15(6): e40979. |
| [31] | Mulla Z, Hashem R, AlMohamad A, et al. Effect of body mass factors on setup displacement in gynecologic tumors and subsequent effect on PTV margins[J]. Adv Radiat Oncol, 2022, 8(1): 101108. doi:10.1016/j.adro.2022.101108 |
| [32] | 李 军. 不同年龄前列腺癌患者的临床病理特征与生存状况分析[J]. 新乡医学院学报, 2020, 37(9): 862-4. |
| [33] | 潘启勇, 丁秋娥, 姜仁伟, 等. 盆腔肿瘤常规放疗摆位误差分析[J]. 中国实用医药, 2010, 5(24): 47-8. |
| [34] | 丁伟杰, 孙 菁, 陈一兴. 肝肿瘤螺旋断层放疗中患者年龄对摆位误差的影响[J]. 肿瘤, 2016, 36(7): 810-3. |
| [35] | Bossuyt E, Nevens D, Weytjens R, et al. Assessing the impact of adaptations to the clinical workflow in radiotherapy using transit in vivo dosimetry[J]. Phys Imaging Radiat Oncol. 2023,25:100420. doi:10.1016/j.phro.2023.100420 |
| [36] | 王春霞, 宋 真, 李红燕, 等. 不同年龄前列腺癌患者疾病不确定感与生活质量[J]. 中国老年学杂志, 2019, 39(1): 200-3. |
| [1] | 陈子贤, 周家伟, 谭磊, 黄志鹏, 薛康颐, 陈明坤. 基于免疫抑制性Neu_2中性粒细胞亚群模型精准预测前列腺癌生存预后及免疫治疗应答[J]. 南方医科大学学报, 2025, 45(8): 1643-1653. |
| [2] | 骆金光, 陶怀祥, 闻志远, 陈龙, 胡昊, 关翰. 肿瘤相关成纤维细胞上调hsa-miR-18b-5p靶向FBXL3促进前列腺癌的增殖及转移[J]. 南方医科大学学报, 2024, 44(7): 1284-1296. |
| [3] | 谢 彦, 李 澄, 张露露, 俞 飞, 臧士明, 王书奎, 王 峰. 68Ga-PSMA-I&T PET/CT评估初诊前列腺癌原发灶的肿瘤负荷[J]. 南方医科大学学报, 2022, 42(8): 1143-1148. |
| [4] | 杨 明, 朱旭东, 沈 炀, 何 麒, 秦 远, 邵轶群, 袁 琳, 叶和松. MYBL2在前列腺癌患者组织中高表达并与不良预后相关[J]. 南方医科大学学报, 2022, 42(8): 1109-1118. |
| [5] | 李国平, 常秀亭, 罗小菊, 赵映淑, 王为服, 康新立. 褐藻素通过线粒体通路和氧化应激诱导前列腺癌细胞凋亡[J]. 南方医科大学学报, 2021, 41(6): 953-959. |
| [6] | 徐彬兵, 郝敬兰, 谢倩文, 萨娜尔, 王诗虞, 杜晓文, 卢海成, 高 平, 石光耀, 董小明. 敲低EEFSEC可体外抑制前列腺癌细胞的增殖、迁移和侵袭[J]. 南方医科大学学报, 2021, 41(12): 1787-1794. |
| [7] | 张河元, 陈南辉, 王晓红, 高白云, 凌木安, 陈 果, 吴志明, 李宇同, 钟伟枫, 潘 斌. 加权基因共表达网络挖掘并验证调控前列腺癌转移的枢纽基因[J]. 南方医科大学学报, 2021, 41(11): 1631-1640. |
| [8] | 韦莉莉,罗周翔,李金龙,李红卫,梁 瑶,李金连,申玉婷,李天柏,宋 捷,胡志明. 二甲双胍抑制酸性环境下的调节性T细胞增殖及功能[J]. 南方医科大学学报, 2019, 39(12): 1427-1435. |
| [9] | 何强,王学涛,李欣,甄鑫. 基于多模态特征和多分类器融合的前列腺癌放疗中直肠并发症预测模型[J]. 南方医科大学学报, 2019, 39(08): 972-. |
| [10] | 陈海平,向玘,刘大伟,魏强. 沉默CIT基因可抑制前列腺癌细胞的增殖和转移[J]. 南方医科大学学报, 2019, 39(03): 257-. |
| [11] | 肖卓裕,陈明坤,杨建昆,杨诚,吕娴媛,田湖,刘存东. MTBP调控前列腺癌细胞的迁移和侵袭[J]. 南方医科大学学报, 2019, 39(01): 6-. |
| [12] | 欧艺虹,姜耀东,李琦,庄永江,党强,谭万龙. 肥大细胞通过上调p21促进前列腺癌神经内分泌分化及增加对多西他赛化疗的抵抗性[J]. 南方医科大学学报, 2018, 38(06): 723-. |
| [13] | 赖桂华,黄爱兰,赵志,卢兴浩,祖文轩. MircoRNA-218下调BMI-1表达水平介导的抗骨肉瘤作用[J]. 南方医科大学学报, 2018, 38(05): 505-. |
| [14] | 殷昭阳,齐思勇,成祥,郭靓,陈泓宇,施明. 经股动脉注射途径建立前列腺癌和乳腺癌骨转移模型[J]. 南方医科大学学报, 2017, 37(07): 914-. |
| [15] | 邓煜麟,郭凯,曾颖科,吴凯辉,唐晨,郑少波. 雄激素受体对IgG蛋白表达及前列腺癌细胞增殖和迁移的影响[J]. 南方医科大学学报, 2017, 37(03): 388-. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||