南方医科大学学报 ›› 2024, Vol. 44 ›› Issue (7): 1345-1354.doi: 10.12122/j.issn.1673-4254.2024.07.14
陶怀祥1,2( ), 骆金光1,2, 闻志远1, 虞亘明1,2, 苏萧1, 王鑫玮1, 关翰1, 陈志军1(
), 骆金光1,2, 闻志远1, 虞亘明1,2, 苏萧1, 王鑫玮1, 关翰1, 陈志军1( )
)
收稿日期:2023-12-18
出版日期:2024-07-20
发布日期:2024-07-25
通讯作者:
陈志军
E-mail:2240489402@qq.com;byczj@bbmc.edu.cn
作者简介:陶怀祥,在读硕士研究生,E-mail: 2240489402@qq.com
基金资助:
Huaixiang TAO1,2( ), Jinguang LUO1,2, Zhiyuan WEN1, Genming YU1,2, Xiao SU1, Xinwei WANG1, Han GUAN1, Zhijun CHEN1(
), Jinguang LUO1,2, Zhiyuan WEN1, Genming YU1,2, Xiao SU1, Xinwei WANG1, Han GUAN1, Zhijun CHEN1( )
)
Received:2023-12-18
Online:2024-07-20
Published:2024-07-25
Contact:
Zhijun CHEN
E-mail:2240489402@qq.com;byczj@bbmc.edu.cn
摘要:
目的 探讨STING在肾缺血再灌注损伤(IRI)中的表达水平以及相关作用机制。 方法 在体内水平,将24只C57BL/6小鼠分为假手术组(Sham)、IRI组、IRI+药物溶剂组(IRI+DMSO)、IRI+SN-011组,6只/组。通过肾动脉夹闭方法建立IRI模型,通过血清肌酐和尿素氮检测、PAS染色检测肾组织损伤变化,采用RT-qPCR、ELISA、Western blotting和IHC法检测肾组织中STING、KIM-1、Bcl-2、Bax、caspase-3、TLR4、P65、NLRP3、caspase-1、CD68、MPO、 IL-1β、IL-6、TNF-α的水平。在体外水平,将HK-2细胞分为对照组、缺氧复氧(H/R)组、H/R+药物溶剂组(H/R+DMSO)、H/R+SN-011组,用厌氧包模拟缺氧环境,RT-qPCR和Western blotting法检测STING表达水平,流式细胞术检测各组细胞凋亡率。 结果 在体内水平,与Sham组相比,IRI组的PAS染色显示组织损伤增加(P<0.05),小鼠血清肌酐、尿素氮含量以及组织KIM-1、STING、TLR4、P65、NLRP3、caspase-1、caspase-3、Bax、CD68、MPO、IL-1β、IL-6、TNF-α表达水平升高(P<0.05),Bcl-2水平降低(P<0.05),SN-011抑制STING表达后,逆转了上述结果(P<0.05)。在体外水平,与对照组相比,H/R组STING的mRNA与蛋白水平升高(P<0.05),流式细胞仪检测显示细胞凋亡率上升(P<0.05),SN-011抑制STING表达,细胞凋亡率下降(P<0.05)。 结论 STING在肾脏IRI中表达水平上升,且可通过作用于TLR4/NF-κB/NLRP3通路以及影响炎症与凋亡水平促进肾损伤。
陶怀祥, 骆金光, 闻志远, 虞亘明, 苏萧, 王鑫玮, 关翰, 陈志军. STING高表达通过调控TLR4/NF-κB/NLRP3通路和影响炎症与凋亡水平促进小鼠肾脏缺血再灌注损伤[J]. 南方医科大学学报, 2024, 44(7): 1345-1354.
Huaixiang TAO, Jinguang LUO, Zhiyuan WEN, Genming YU, Xiao SU, Xinwei WANG, Han GUAN, Zhijun CHEN. High STING expression exacerbates renal ischemia-reperfusion injury in mice by regulating the TLR4/NF-κB/NLRP3 pathway and promoting inflammation and apoptosis[J]. Journal of Southern Medical University, 2024, 44(7): 1345-1354.
| Gene | Primer sequence |
|---|---|
| STING | F:GTCCCTTGCACATGGTGTTG |
| R:CAGGTCATGCTGTCGCCTAT | |
| KIM-1 | F:AGAAGACCCACAACTACAAGGC |
| R:TAGATGTTGGAGGAGTGGAGGT | |
| IL-1β | F:GCCTGTGTTTTCCTCCTTGC |
| R:TGCTGCCTAATGTCCCCTTG | |
| IL-6 | F:GTGGCTAAGGACCAAGACCAT |
| R:TCTGACCACAGTGAGGAATGTC | |
| TNF-α | F:AGCCGATGGGTTGTACCTTG |
| R:ATAGCAAATCGGCTGACGGT | |
| GAPDH | F:TGGAAAGCTGTGGCGTGAT |
| R:AGATCCACGACGGACACATT |
表 1 RT-qPCR引物序列
Tab.1 Primer sequence for RT-qPCR
| Gene | Primer sequence |
|---|---|
| STING | F:GTCCCTTGCACATGGTGTTG |
| R:CAGGTCATGCTGTCGCCTAT | |
| KIM-1 | F:AGAAGACCCACAACTACAAGGC |
| R:TAGATGTTGGAGGAGTGGAGGT | |
| IL-1β | F:GCCTGTGTTTTCCTCCTTGC |
| R:TGCTGCCTAATGTCCCCTTG | |
| IL-6 | F:GTGGCTAAGGACCAAGACCAT |
| R:TCTGACCACAGTGAGGAATGTC | |
| TNF-α | F:AGCCGATGGGTTGTACCTTG |
| R:ATAGCAAATCGGCTGACGGT | |
| GAPDH | F:TGGAAAGCTGTGGCGTGAT |
| R:AGATCCACGACGGACACATT |
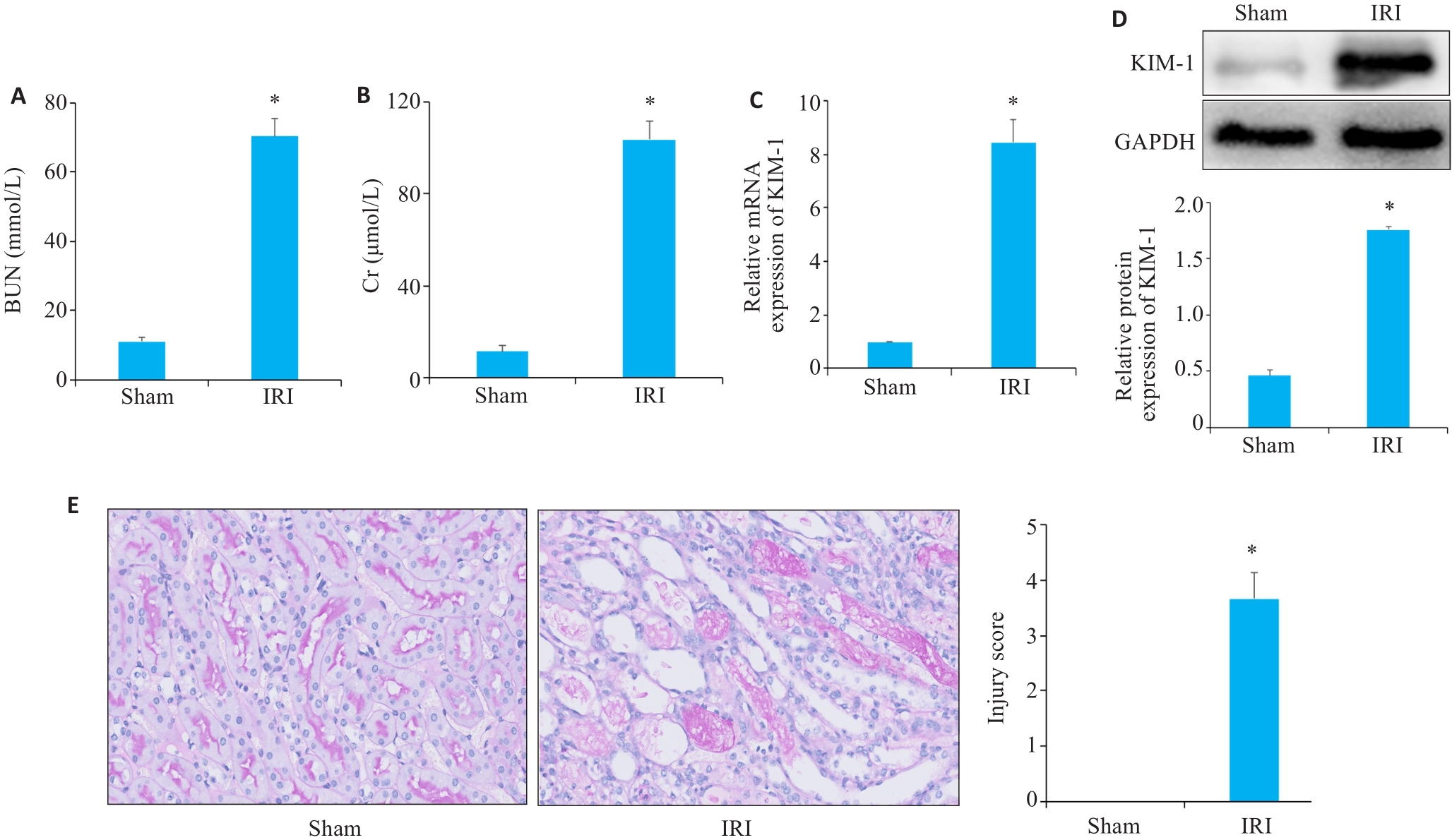
图2 血清生化、Western blotting、RT-qPCR、PAS染色验证小鼠缺血再灌注模型构建效果
Fig.2 Serum biochemistry, Western blotting, RT-qPCR and PAS staining for assessing the effect of ischemia-reperfusion modeling. A, B: Serum BUN (A) and Cr (B) levels of the mice in sham and IRI group. C: RT-qPCR analysis of KIM-1 in Sham and IRI groups mice. D: Western blotting of KIM-1 in sham and IRI group. E: PAS staining of renal tissue from mice in sham and IRI groups (Original magnification: ×400). *P<0.05 vs Sham group.
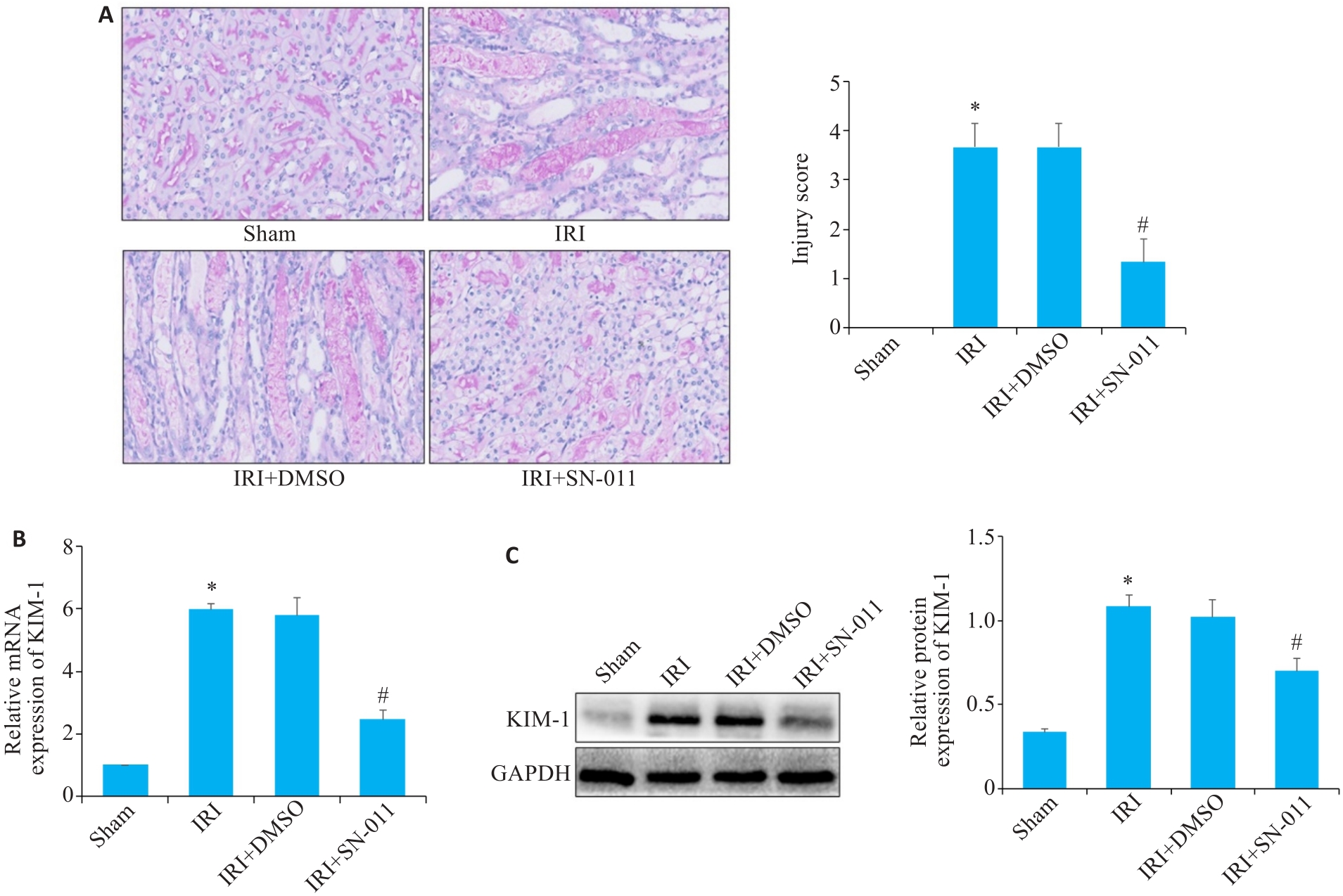
图5 RT-qPCR、Western blotting、PAS染色检测肾组织损伤程度
Fig.5 RT-qPCR, Western blotting and PAS staining for detecting renal tissue injury. A: PAS staining of kidney tissues from mice in the sham, IRI, IRI+DMSO and IRI+SN-011 groups (×400). B, C: RT-qPCR and Western blotting of the expressions of KIM-1 in sham, IRI, IRI+DMSO and IRI+SN-011 groups. *P<0.05 vs Sham; #P<0.05 vs IRI.
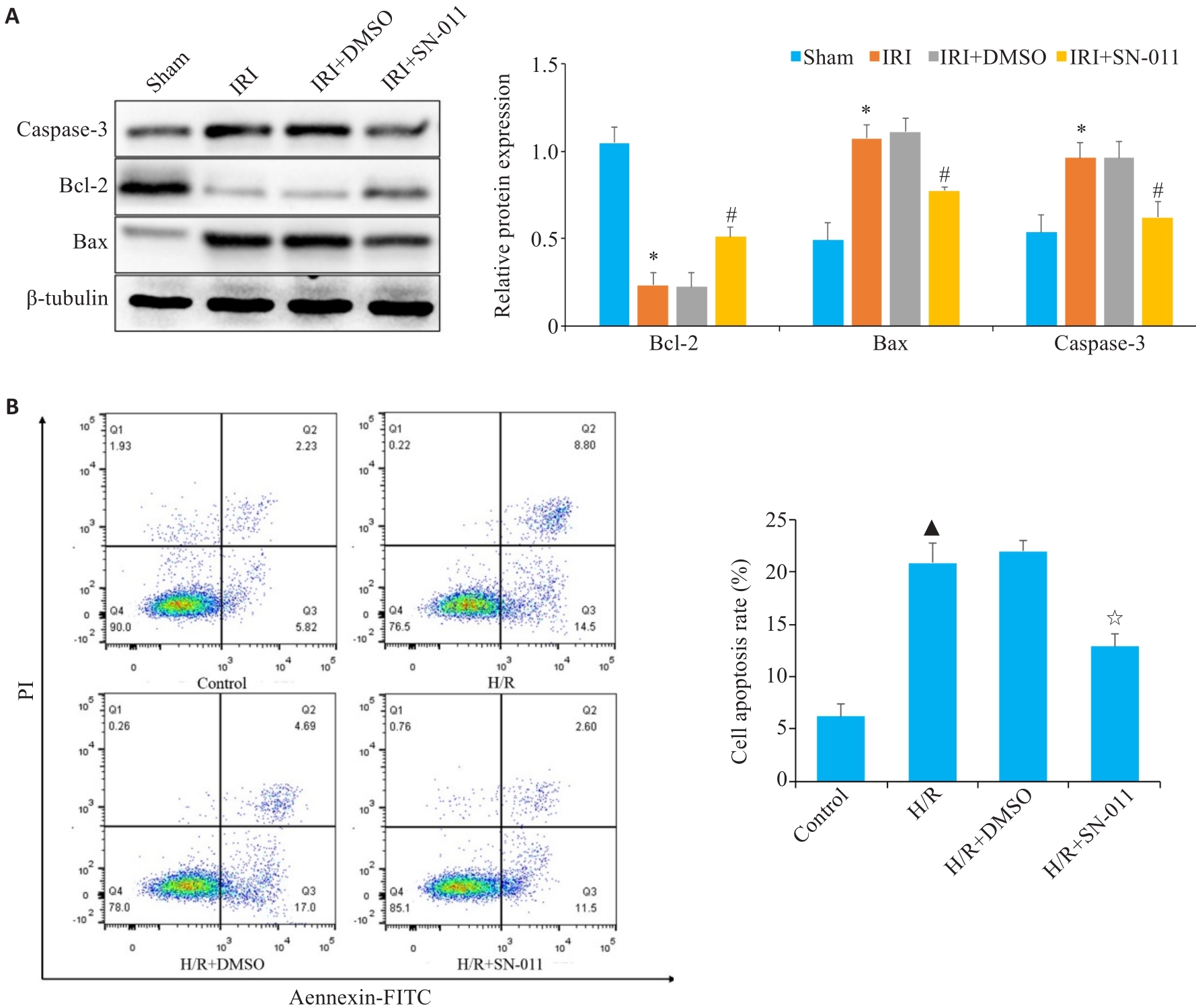
图7 Western blotting、流式细胞仪技术检测凋亡水平
Fig.7 Cell apoptosis analyzed using Western blotting and flow cytometry. A: Western blotting of relative expression levels of caspase-3, Bcl-2 and Bax in mouse kidney tissue from sham, IRI, IRI+DMSO and IRI+SN-011 groups. B: Flow cytometric analysis of HK-2 cell apoptosis in control, H/R, H/R+DMSO, and H/R+SN-011 groups. *P<0.05 vs Sham; #P<0.05 vs IRI; ▲P<0.05 vs control; ☆P<0.05 vs H/R.
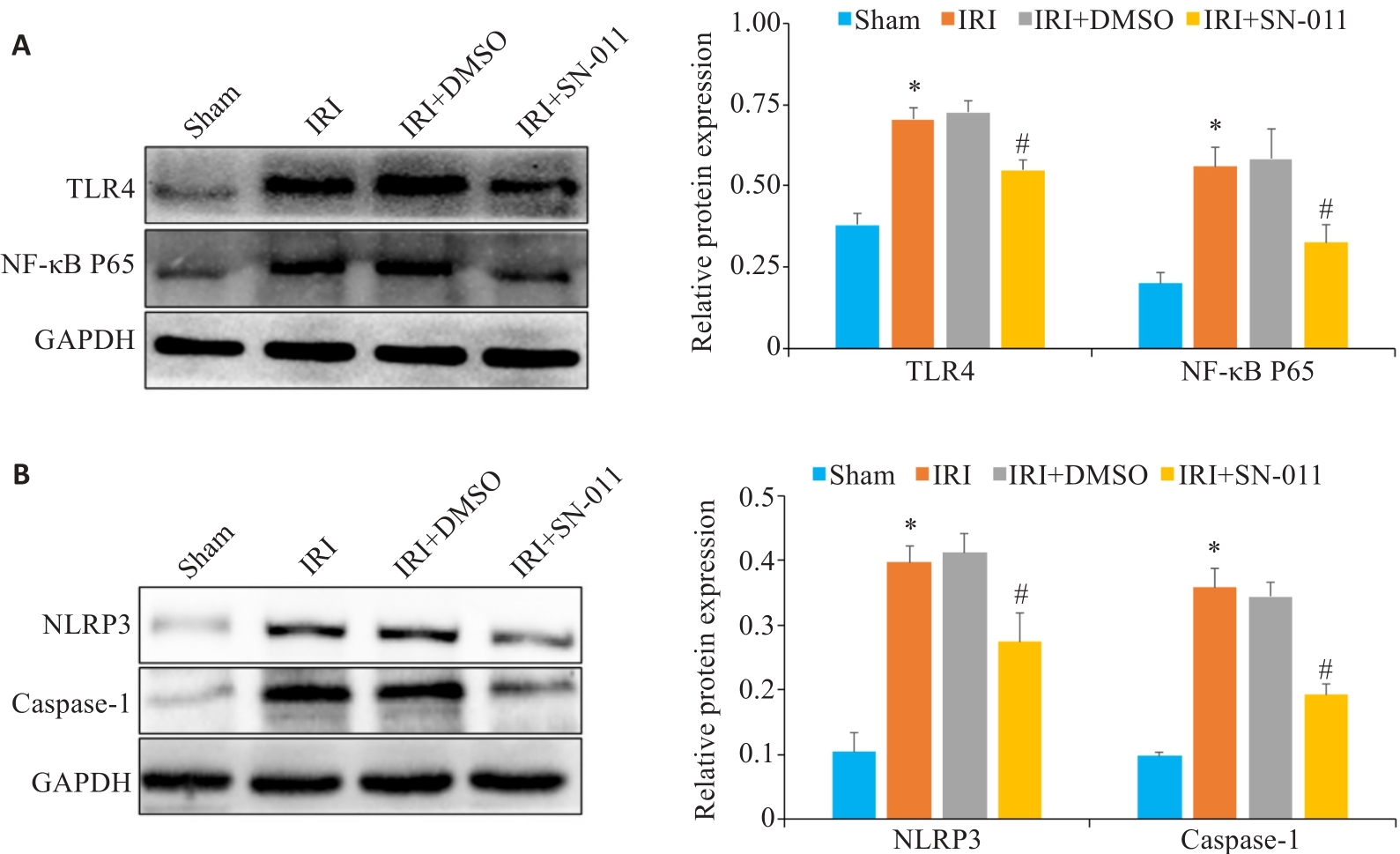
图8 Western blotting检测肾组织中TLR4、NF-κB P65、NLRP3、caspase-1蛋白表达水平
Fig.8 Western blotting for detecting TLR4, NF‑κB P65, NLRP3, and caspase-1 protein expressions in the renal tissue. A: Western blotting of TLR4 and NF-κB P65 in mouse kidney tissues from sham, IRI, IRI+DMSO and IRI+SN-011 groups. B: Western blotting of NLRP3 and caspase-1 in mice kidney tissue from the sham, IRI, IRI+DMSO and IRI+SN-011 groups. *P<0.05 vs Sham; #P<0.05 vs IRI.
| 1 | Hoste EAJ, Kellum JA, Selby NM, et al. Global epidemiology and outcomes of acute kidney injury[J]. Nat Rev Nephrol, 2018, 14(10): 607-25. |
| 2 | Zuk A, Bonventre JV. Acute kidney injury[J]. Annu Rev Med, 2016, 67: 293-307. |
| 3 | Arai S, Kitada K, Yamazaki T, et al. Apoptosis inhibitor of macrophage protein enhances intraluminal debris clearance and ameliorates acute kidney injury in mice[J]. Nat Med, 2016, 22(2): 183-93. |
| 4 | Inagi R, Ishimoto Y, Nangaku M. Proteostasis in endoplasmic reticulum: new mechanisms in kidney disease[J]. Nat Rev Nephrol, 2014, 10(7): 369-78. |
| 5 | Yan MJ, Tang CY, Ma ZW, et al. DNA damage response in nephrotoxic and ischemic kidney injury[J]. Toxicol Appl Pharmacol, 2016, 313: 104-8. |
| 6 | Malek M, Nematbakhsh M. Renal ischemia/reperfusion injury; from pathophysiology to treatment[J]. J Renal Inj Prev, 2015, 4(2): 20-7. |
| 7 | Fang R, Wang CG, Jiang QF, et al. NEMO-IKKβ are essential for IRF3 and NF-κB activation in the cGAS-STING pathway[J]. J Immunol, 2017, 199(9): 3222-33. |
| 8 | Fang R, Jiang QF, Guan YK, et al. Golgi apparatus-synthesized sulfated glycosaminoglycans mediate polymerization and activation of the cGAMP sensor STING[J]. Immunity, 2021, 54(5): 962-75.e8. |
| 9 | Ren P, Cao JL, Lin PL, et al. Molecular mechanism of luteolin regulating lipoxygenase pathway against oxygen-glucose deprivation/reperfusion injury in H9c2 cardiomyocytes based on molecular docking[J]. Zhongguo Zhong Yao Za Zhi, 2021, 46(21): 5665-73. |
| 10 | Bi R, Yang YL, Liao HW, et al. Porphyromonas gingivalis induces an inflammatory response via the cGAS-STING signaling pathway in a periodontitis mouse model[J]. Front Microbiol, 2023, 14: 1183415. |
| 11 | Pressly JD, Park F. DNA repair in ischemic acute kidney injury[J]. Am J Physiol Renal Physiol, 2017, 312(4): F551-5. |
| 12 | Hu HL, Zou C. Mesenchymal stem cells in renal ischemia-reperfusion injury: biological and therapeutic perspectives[J]. Curr Stem Cell Res Ther, 2017, 12(3): 183-7. |
| 13 | Inagi R. Endoplasmic reticulum stress in the kidney as a novel mediator of kidney injury[J]. Nephron Exp Nephrol, 2009, 112(1): e1-9. |
| 14 | Cao Q, Wang YP, Niu ZG, et al. Potentiating tissue-resident type 2 innate lymphoid cells by IL-33 to prevent renal ischemia-reperfusion injury[J]. J Am Soc Nephrol, 2018, 29(3): 961-76. |
| 15 | Havasi A, Borkan SC. Apoptosis and acute kidney injury[J]. Kidney Int, 2011, 80(1): 29-40. |
| 16 | Yang DH, Tang M, Zhang MM, et al. Downregulation of G protein-coupled receptor kinase 4 protects against kidney ischemia-reperfusion injury[J]. Kidney Int, 2023, 103(4): 719-34. |
| 17 | Li XR, Liao J, Su XJ, et al. Human urine-derived stem cells protect against renal ischemia/reperfusion injury in a rat model via exosomal miR-146a-5p which targets IRAK1 [J]. Theranostics, 2020, 10(21): 9561-78. |
| 18 | Wang J, Xiong MR, Fan Y, et al. Mecp2 protects kidney from ischemia-reperfusion injury through transcriptional repressing IL-6/STAT3 signaling[J]. Theranostics, 2022, 12(8): 3896-910. |
| 19 | van Timmeren MM, van den Heuvel MC, Bailly V, et al. Tubular kidney injury molecule-1 (KIM-1) in human renal disease[J]. J Pathol, 2007, 212(2): 209-17. |
| 20 | Gkirtzimanaki K, Kabrani E, Nikoleri D, et al. IFNα impairs autophagic degradation of mtDNA promoting autoreactivity of SLE monocytes in a STING-dependent fashion[J]. Cell Rep, 2018, 25(4): 921-33.e5. |
| 21 | Gao YP, Zhang NN, Zeng ZH, et al. LncRNA PCAT1 activates SOX2 and suppresses radioimmune responses via regulating cGAS/STING signalling in non-small cell lung cancer[J]. Clin Transl Med, 2022, 12(4): e792. |
| 22 | Li X, Liu YJ, Wang Y, et al. Epoxy triglyceride enhances intestinal permeability via caspase-1/NLRP3/GSDMD and cGAS-STING pathways in dextran sulfate sodium-induced colitis mice[J]. J Agric Food Chem, 2023, 71(10): 4371-81. |
| 23 | Wu JJ, Zhao L, Hu HG, et al. Agonists and inhibitors of the STING pathway: potential agents for immunotherapy[J]. Med Res Rev, 2020, 40(3): 1117-41. |
| 24 | Barber GN. STING: infection, inflammation and cancer[J]. Nat Rev Immunol, 2015, 15(12): 760-70. |
| 25 | Lu L, Zhou HM, Ni M, et al. Innate immune regulations and liver ischemia-reperfusion injury[J]. Transplantation, 2016, 100(12): 2601-10. |
| 26 | DeWolf SE, Kasimsetty SG, Hawkes AA, et al. DAMPs released from injured renal tubular epithelial cells activate innate immune signals in healthy renal tubular epithelial cells[J]. Transplantation, 2022, 106(8): 1589-99. |
| 27 | Raup-Konsavage WM, Wang YM, Wang WW, et al. Neutrophil peptidyl arginine deiminase-4 has a pivotal role in ischemia/reperfusion-induced acute kidney injury[J]. Kidney Int, 2018, 93(2): 365-74. |
| 28 | Salvadori M, Rosso G, Bertoni E. Update on ischemia-reperfusion injury in kidney transplantation: Pathogenesis and treatment[J]. World J Transplant, 2015, 5(2): 52-67. |
| 29 | Liu CH, Wang QD, Niu L. Sufentanil inhibits Pin1 to attenuate renal tubular epithelial cell ischemia-reperfusion injury by activating the PI3K/AKT/FOXO1 pathway[J]. Int Urol Nephrol, 2023, 55(8): 1903-16. |
| 30 | Wu B, Xu MM, Fan C, et al. STING inhibitor ameliorates LPS-induced ALI by preventing vascular endothelial cells-mediated immune cells chemotaxis and adhesion[J]. Acta Pharmacol Sin, 2022, 43(8): 2055-66. |
| 31 | Liu R, Li JY, Shao JC, et al. Innate immune response orchestrates phosphoribosyl pyrophosphate synthetases to support DNA repair[J]. Cell Metab, 2021, 33(10): 2076-89.e9. |
| 32 | Yang B, Li X, Fu Y, et al. MEK inhibition remodels the immune landscape of mutant KRAS tumors to overcome resistance to PARP and immune checkpoint inhibitors[J]. Cancer Res, 2021, 81(10): 2714-29. |
| 33 | Zhang YN, Dong YL, Hao WP, et al. Increased cGAS/STING signaling components in patients with Mooren's ulcer[J]. Int J Ophthalmol, 2021, 14(11): 1660-5. |
| 34 | Hong Z, Mei JH, Li CH, et al. STING inhibitors target the cyclic dinucleotide binding pocket[J]. Proc Natl Acad Sci U S A, 2021, 118(24): e2105465118. |
| 35 | Diao FF, Bai J, Jiang CL, et al. The papain-like protease of porcine reproductive and respiratory syndrome virus impedes STING translocation from the endoplasmic reticulum to the Golgi apparatus by deubiquitinating STIM1[J]. J Virol, 2023, 97(4): e0018823. |
| 36 | Yang BX, Xie XR, Wu ZY, et al. DNA damage-mediated cellular senescence promotes hand-foot syndrome that can be relieved by thymidine prodrug[J]. Genes Dis, 2022, 10(6): 2557-71. |
| 37 | Ablasser A, Chen ZJ. cGAS in action: expanding roles in immunity and inflammation[J]. Science, 2019, 363(6431): eaat8657. |
| 38 | Gulen MF, Koch U, Haag SM, et al. Signalling strength determines proapoptotic functions of STING[J]. Nat Commun, 2017, 8(1): 427. |
| 39 | Lehnardt S, Massillon L, Follett P, et al. Activation of innate immunity in the CNS triggers neurodegeneration through a Toll-like receptor 4-dependent pathway[J]. Proc Natl Acad Sci USA, 2003, 100(14): 8514-9. |
| 40 | Wang L, Yang JW, Lin LT, et al. Acupuncture attenuates inflammation in microglia of vascular dementia rats by inhibiting miR-93-mediated TLR4/MyD88/NF‑κB signaling pathway[J]. Oxid Med Cell Longev, 2020, 2020: 8253904. |
| 41 | Zhang NX, Guan C, Liu ZY, et al. Calycosin attenuates renal ischemia/reperfusion injury by suppressing NF‑κB mediated inflammation via PPARγ/EGR1 pathway[J]. Front Pharmacol, 2022, 13: 970616. |
| 42 | Alaaeldin R, Bakkar SM, Mohyeldin RH, et al. Azilsartan modulates HMGB1/NF-κB/p38/ERK1/2/JNK and apoptosis pathways during renal ischemia reperfusion injury[J]. Cells, 2023, 12(1): 185. |
| 43 | Ding HS, Huang Y, Qu JF, et al. Panaxynol ameliorates cardiac ischemia/reperfusion injury by suppressing NLRP3-induced pyroptosis and apoptosis via HMGB1/TLR4/NF-κB axis[J]. Int Immunopharmacol, 2023, 121: 110222. |
| 44 | Liu YY, Lei ZL, Chai H, et al. Salidroside alleviates hepatic ischemia-reperfusion injury during liver transplant in rat through regulating TLR-4/NF‑κB/NLRP3 inflammatory pathway[J]. Sci Rep, 2022, 12(1): 13973. |
| 45 | Li N, Zhou H, Wu HM, et al. STING-IRF3 contributes to lipopolysaccharide-induced cardiac dysfunction, inflammation, apoptosis and pyroptosis by activating NLRP3[J]. Redox Biol, 2019, 24: 101215. |
| [1] | 常笑语, 张瀚文, 曹红亭, 侯玲, 孟鑫, 陶虹, 罗彦, 李光华. 热应激对大鼠胸主动脉内皮细胞生物钟基因 Bmal1和细胞周期蛋白表达水平的影响[J]. 南方医科大学学报, 2025, 45(7): 1353-1362. |
| [2] | 范正媛, 沈子涵, 李亚, 沈婷婷, 李高峰, 李素云. 补肺益肾方对香烟烟雾提取物诱导的人支气管上皮细胞损伤的保护作用及其机制[J]. 南方医科大学学报, 2025, 45(7): 1372-1379. |
| [3] | 周海忆, 何斯怡, 韩瑞芳, 关永格, 董丽娟, 宋阳. 艾灸通过调控miR-223-3p/NLRP3焦亡通路修复薄型子宫内膜[J]. 南方医科大学学报, 2025, 45(7): 1380-1388. |
| [4] | 王立明, 陈宏睿, 杜燕, 赵鹏, 王玉洁, 田燕歌, 刘新光, 李建生. 益气滋肾方通过抑制PI3K/Akt/NF-κB通路改善小鼠慢性阻塞性肺疾病的炎症反应[J]. 南方医科大学学报, 2025, 45(7): 1409-1422. |
| [5] | 夏冰, 彭进, 丁九阳, 王杰, 唐国伟, 刘国杰, 王沄, 万昌武, 乐翠云. ATF3通过NF-κB信号通路调控动脉粥样硬化斑块内的炎症反应[J]. 南方医科大学学报, 2025, 45(6): 1131-1142. |
| [6] | 王心恒, 邵小涵, 李童童, 张璐, 杨勤军, 叶卫东, 童佳兵, 李泽庚, 方向明. 平喘宁方通过调控HMGB1/Beclin-1轴介导的自噬改善患寒哮证大鼠的气道炎症[J]. 南方医科大学学报, 2025, 45(6): 1153-1162. |
| [7] | 杨毓甲, 杨丽芳, 吴雅玲, 段兆达, 于春泽, 吴春云, 于建云, 杨力. 大麻二酚经PERK-eIF2α-ATF4-CHOP通路减轻多重脑震荡大鼠的神经元内质网应激和凋亡[J]. 南方医科大学学报, 2025, 45(6): 1240-1250. |
| [8] | 牛民主, 殷丽霞, 乔通, 尹林, 张可妮, 胡建国, 宋传旺, 耿志军, 李静. 旱莲苷A通过调控JAK2/STAT3通路抑制M1型巨噬细胞极化改善葡聚糖硫酸钠诱导的小鼠结肠炎[J]. 南方医科大学学报, 2025, 45(6): 1297-1306. |
| [9] | 田芷华, 杨青青, 陈欣, 张方方, 钟柏茂, 曹虹. 精胺抑制巨噬细胞中GBP5介导的NLRP3炎性小体活化减轻感染肠道病毒71型的新生小鼠脏器损伤[J]. 南方医科大学学报, 2025, 45(5): 901-910. |
| [10] | 卞芬兰, 倪诗垚, 赵鹏, 戚毛男星, 唐碧, 王洪巨, 康品方, 刘进军. 积雪草苷通过抑制NLRP3炎症体介导的细胞焦亡减轻大鼠心肌缺血再灌注损伤[J]. 南方医科大学学报, 2025, 45(5): 977-985. |
| [11] | 梁晓涛, 熊一凡, 刘雪琪, 梁小珊, 朱晓煜, 谢炜. 活血疏风颗粒通过抑制TLR4/NF-κB通路改善慢性偏头痛小鼠的中枢敏化[J]. 南方医科大学学报, 2025, 45(5): 986-994. |
| [12] | 孙亚磊, 罗萌, 郭长胜, 高静, 苏凯奇, 陈立典, 冯晓东. 穗花杉双黄酮通过抑制细胞焦亡减轻小鼠急性肺损伤[J]. 南方医科大学学报, 2025, 45(4): 692-701. |
| [13] | 杨洋, 王凯, 柳鉴修, 周志谟, 贾雯, 吴思谋, 李金星, 何方, 程如越. 生命早期两歧双歧杆菌BD-1干预可缓解注意缺陷多动障碍雌性大鼠幼年期的多动行为[J]. 南方医科大学学报, 2025, 45(4): 702-710. |
| [14] | 朱正望, 王琳琳, 赵静涵, 马瑞雪, 余雨春, 蔡庆春, 王兵, 朱平生, 苗明三. 退黄合剂通过调控法尼醇X受体抑制NLRP3炎症小体改善α-萘异硫氰酸酯诱导的大鼠胆汁淤积[J]. 南方医科大学学报, 2025, 45(4): 718-724. |
| [15] | 陈悦, 肖林雨, 任侣, 宋雪, 李静, 胡建国. 水晶兰苷通过抑制PI3K/AKT信号通路减少神经元凋亡改善脊髓损伤后小鼠的运动功能[J]. 南方医科大学学报, 2025, 45(4): 774-784. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||