南方医科大学学报 ›› 2025, Vol. 45 ›› Issue (1): 197-205.doi: 10.12122/j.issn.1673-4254.2025.01.23
• • 上一篇
周沛珊1,2( ), 阳维1, 李青原2, 郭小芳3, 傅蓉1(
), 阳维1, 李青原2, 郭小芳3, 傅蓉1( ), 刘思德2(
), 刘思德2( )
)
收稿日期:2024-09-30
出版日期:2025-01-20
发布日期:2025-01-20
通讯作者:
傅蓉,刘思德
E-mail:2279626154@qq.com;furong@smu.edu.cn;liuside2011@163.com
作者简介:周沛珊,在读硕士研究生,E-mail: 2279626154@qq.com
基金资助:
Peishan ZHOU1,2( ), Wei YANG1, Qingyuan LI2, Xiaofang GUO3, Rong FU1(
), Wei YANG1, Qingyuan LI2, Xiaofang GUO3, Rong FU1( ), Side LIU2(
), Side LIU2( )
)
Received:2024-09-30
Online:2025-01-20
Published:2025-01-20
Contact:
Rong FU, Side LIU
E-mail:2279626154@qq.com;furong@smu.edu.cn;liuside2011@163.com
摘要:
目的 提出一种基于电子内镜图像的多特征融合模型,结合深度学习与手工特征的优势,用于消化性溃疡再出血风险的分级。 方法 根据溃疡的内镜表现,提取颜色特征以区分活动性出血(Forrest I)与非出血溃疡(Forrest II、III),并利用边缘和纹理特征描述不同级别溃疡的形态与外观。通过融合深度学习网络提取的深度特征与手工提取的视觉特征,形成电子内镜图像的多特征表达,最终用于预测消化性溃疡的再出血风险。 结果 在包含708例患者、3573张图像的Forrest分级数据集上,提出的多特征融合模型在消化性溃疡再出血风险六分级任务中取得了74.94%的准确率,优于进修医生59.9%的分级准确性(P<0.05)。在Ib、IIa和III级溃疡的识别中,F1得分为90.16%、75.44%和77.13%,其中Ib级表现尤为突出。与首个进行溃疡再出血分级研究的模型相比,提出模型的F1得分提升了5.8%。在简化的3类风险分级任务中,模型在高风险、低风险和无需内镜治疗级别上的F1得分为93.74%、81.30%和73.59%。 结论 本文提出的多特征融合模型有效融合卷积神经网络(CNN)提取的深度特征与手工提取的视觉特征,提升了消化性溃疡再出血风险分级的准确性,为临床提供了高效的诊断辅助工具。
周沛珊, 阳维, 李青原, 郭小芳, 傅蓉, 刘思德. 手工提取的视觉特征与深度特征的融合模型用于消化性溃疡再出血风险分级[J]. 南方医科大学学报, 2025, 45(1): 197-205.
Peishan ZHOU, Wei YANG, Qingyuan LI, Xiaofang GUO, Rong FU, Side LIU. A fusion model of manually extracted visual features and deep learning features for rebleeding risk stratification in peptic ulcers[J]. Journal of Southern Medical University, 2025, 45(1): 197-205.
| Ulcer grade | Total cases | Total images | Location | Male | Female | Average age (year) |
|---|---|---|---|---|---|---|
| Ia | 26 | 78 | Duodenum (bulb, descending part), Stomach (antrum) | 22 | 4 | 51.89±16.85 |
| Ib | 194 | 1085 | Duodenum (bulb) | 155 | 40 | 50.98±17.33 |
| IIa | 196 | 1055 | Duodenum (bulb), Stomach (antrum, gastric angle) | 160 | 36 | 50.73±17.89 |
| IIb | 80 | 435 | Duodenum (bulb, descending part), Stomach (antrum) | 64 | 16 | 47.88±16.83 |
| IIc | 69 | 295 | Duodenum (bulb), Stomach (antrum, body) | 59 | 10 | 49.70±16.06 |
| III | 142 | 625 | Duodenum, Stomach (antrum, gastric angle) | 106 | 36 | 49.31±17.61 |
表1 Forrest数据集详细信息
Tab.1 Ulcer grade, total cases, total images, and patient demographic data in the Forrest dataset
| Ulcer grade | Total cases | Total images | Location | Male | Female | Average age (year) |
|---|---|---|---|---|---|---|
| Ia | 26 | 78 | Duodenum (bulb, descending part), Stomach (antrum) | 22 | 4 | 51.89±16.85 |
| Ib | 194 | 1085 | Duodenum (bulb) | 155 | 40 | 50.98±17.33 |
| IIa | 196 | 1055 | Duodenum (bulb), Stomach (antrum, gastric angle) | 160 | 36 | 50.73±17.89 |
| IIb | 80 | 435 | Duodenum (bulb, descending part), Stomach (antrum) | 64 | 16 | 47.88±16.83 |
| IIc | 69 | 295 | Duodenum (bulb), Stomach (antrum, body) | 59 | 10 | 49.70±16.06 |
| III | 142 | 625 | Duodenum, Stomach (antrum, gastric angle) | 106 | 36 | 49.31±17.61 |
| Forrest classification | Endoscopic appearance of ulcer lesions | Risk assessment |
|---|---|---|
| Forrest I active bleeding lesion | Ia: Spurting bleeding Ib: Oozing bleeding | High risk |
| Forrest II signs of recent hemorrhage | IIa: Visible vessel IIb: Adherent clot IIc: Black base | Low risk |
| Forrest III no signs of recent bleeding | III: Clean base | No endoscopic treatment required |
表2 消化性溃疡内镜表现与风险评估分级表
Tab.2 Endoscopic manifestations and risk assessment scale of peptic ulcers
| Forrest classification | Endoscopic appearance of ulcer lesions | Risk assessment |
|---|---|---|
| Forrest I active bleeding lesion | Ia: Spurting bleeding Ib: Oozing bleeding | High risk |
| Forrest II signs of recent hemorrhage | IIa: Visible vessel IIb: Adherent clot IIc: Black base | Low risk |
| Forrest III no signs of recent bleeding | III: Clean base | No endoscopic treatment required |
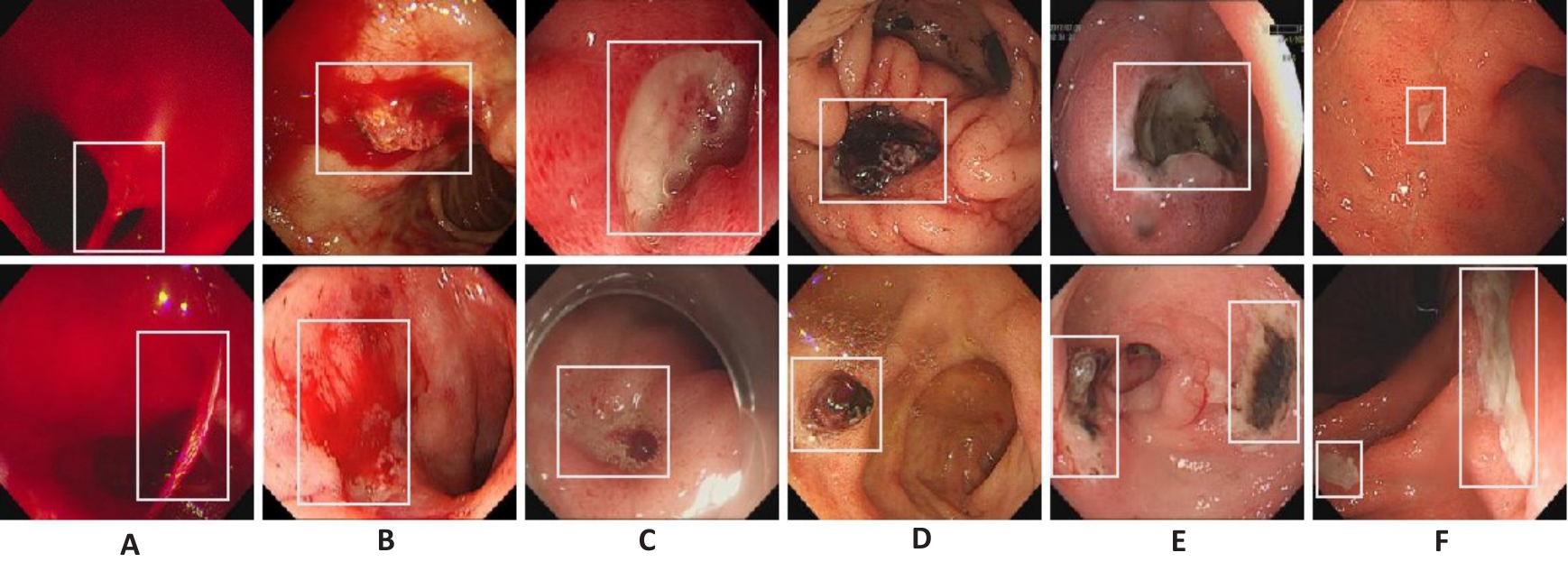
图1 6级再出血风险溃疡示例
Fig.1 Representative endoscopic images of peptic ulcers in the 6 grades of rebleeding risks. A: Images of grade Ia ulcer showing jet-like bleeding. B: Grade Ib ulcer images showing diffuse bleeding. C: Grade IIa ulcer images showing exposure of the vascular head. D: Grade IIb ulcer images showing an attached blood clot. E: Grade IIc ulcer images with black substrate. F: Grade III ulcer images showing a clean base.
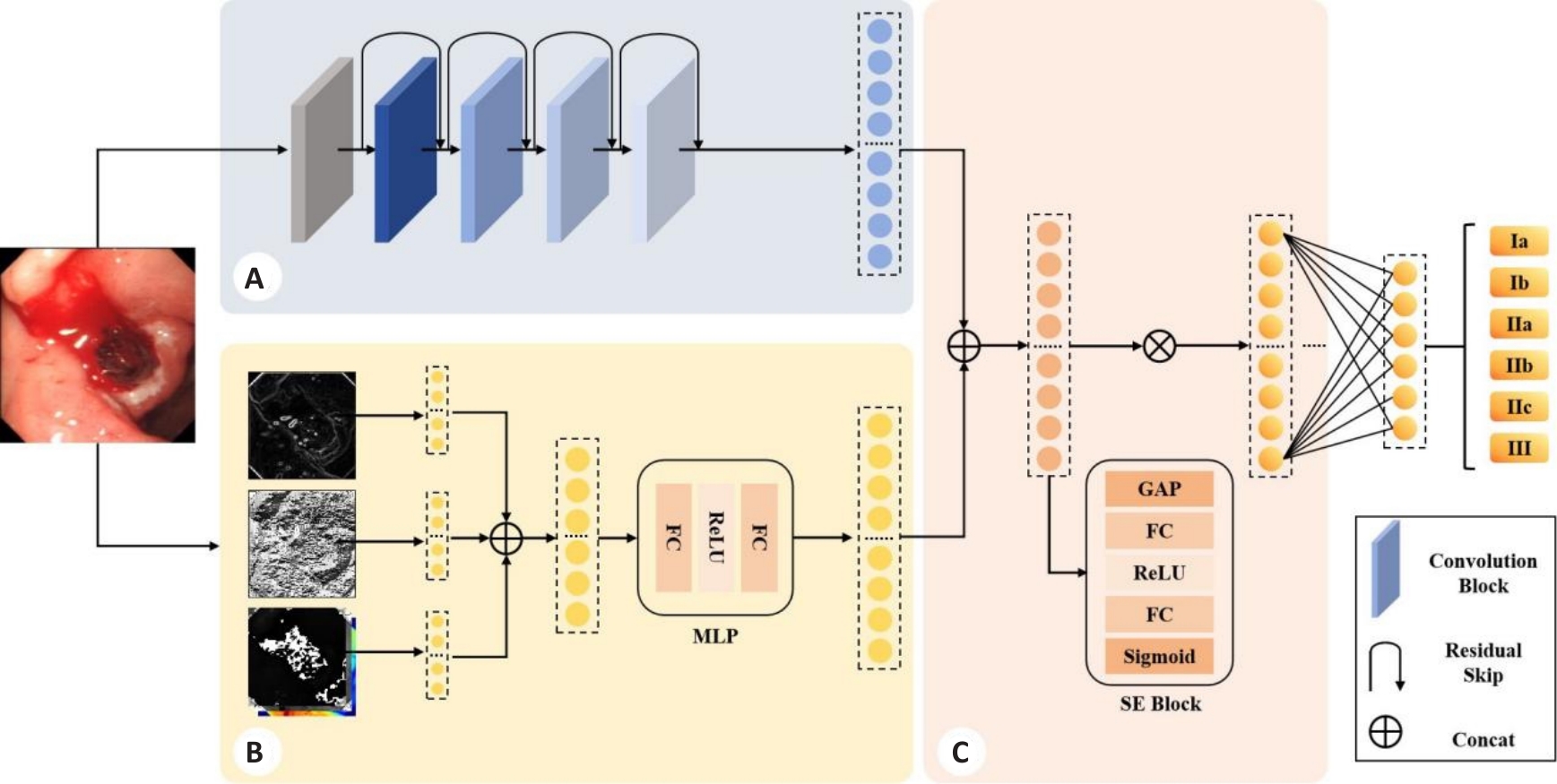
图2 本文方法整体框架
Fig.2 Framework of the proposed method. A: Deep feature extraction module (DFM). B: Handcrafted feature extraction module (HFM). C: Feature fusion module (FFM).
| Methods | Accuracy (%) | Precision (%) | Recall (%) | F1-score (%) |
|---|---|---|---|---|
| Simonyan K[ | 57.13±3.83 | 55.48±4.17 | 57.13±3.83 | 55.08±4.81 |
| Tan M[ | 71.35±1.88 | 72.00±1.76 | 71.35±1.88 | 71.07±2.10 |
| Yen HH[ | 70.50±1.86 | 70.77±1.73 | 70.50±1.86 | 69.99±2.10 |
| Cao W[ | 66.96±1.51 | 67.36±2.00 | 66.96±1.51 | 66.08±1.96 |
| Z. Niu[ | 69.75±1.72 | 70.03±1.27 | 69.75±1.72 | 69.08±1.78 |
| Polat, G[ | 71.41±2.27 | 71.60±1.71 | 71.41±2.27 | 70.97±2.01 |
| MFFM | 74.94±0.73 | 74.45±1.00 | 74.94±0.73 | 74.27±0.66 |
表3 不同方法在消化性溃疡再出血风险评估中的性能对比
Tab.3 Performance comparison of different methods in peptic ulcer rebleeding risk assessment
| Methods | Accuracy (%) | Precision (%) | Recall (%) | F1-score (%) |
|---|---|---|---|---|
| Simonyan K[ | 57.13±3.83 | 55.48±4.17 | 57.13±3.83 | 55.08±4.81 |
| Tan M[ | 71.35±1.88 | 72.00±1.76 | 71.35±1.88 | 71.07±2.10 |
| Yen HH[ | 70.50±1.86 | 70.77±1.73 | 70.50±1.86 | 69.99±2.10 |
| Cao W[ | 66.96±1.51 | 67.36±2.00 | 66.96±1.51 | 66.08±1.96 |
| Z. Niu[ | 69.75±1.72 | 70.03±1.27 | 69.75±1.72 | 69.08±1.78 |
| Polat, G[ | 71.41±2.27 | 71.60±1.71 | 71.41±2.27 | 70.97±2.01 |
| MFFM | 74.94±0.73 | 74.45±1.00 | 74.94±0.73 | 74.27±0.66 |
| Methods | F1-score (%) | |||||
|---|---|---|---|---|---|---|
| Ia | Ib | IIa | IIb | IIc | III | |
| Simonyan K[ | 37.48±12.05 | 78.20±1.48 | 55.40±8.52 | 29.50±11.19 | 18.03±5.53 | 53.63±3.76 |
| Tan M[ | 45.43±7.35 | 88.41±0.76 | 68.32±3.37 | 55.27±4.06 | 44.48±7.86 | 74.83±2.58 |
| Yen HH[ | 35.93±14.47 | 87.05±1.13 | 68.86±2.56 | 53.44±3.69 | 43.49±5.82 | 72.74±2.51 |
| Cao W[ | 14.21±11.31 | 85.86±1.36 | 64.45±2.08 | 45.94±4.09 | 35.77±12.37 | 72.24±1.43 |
| Z. Niu[ | 36.55±7.50 | 87.99±1.22 | 66.85±3.60 | 51.58±2.65 | 38.73±3.83 | 74.61±2.59 |
| Polat, G[ | 27.74±17.36 | 86.62±1.77 | 71.31±4.00 | 57.02±4.19 | 44.97±3.78 | 72.54±3.87 |
| MFFM | 40.07±5.43 | 90.16±0.86 | 75.44±1.27 | 53.97±2.81 | 48.84±5.43 | 77.13±1.64 |
表4 各方法在不同溃疡风险等级中的F1得分比较
Tab.4 Comparison of F1 scores of different methods for assessing rebleeding risk levels of the ulcers
| Methods | F1-score (%) | |||||
|---|---|---|---|---|---|---|
| Ia | Ib | IIa | IIb | IIc | III | |
| Simonyan K[ | 37.48±12.05 | 78.20±1.48 | 55.40±8.52 | 29.50±11.19 | 18.03±5.53 | 53.63±3.76 |
| Tan M[ | 45.43±7.35 | 88.41±0.76 | 68.32±3.37 | 55.27±4.06 | 44.48±7.86 | 74.83±2.58 |
| Yen HH[ | 35.93±14.47 | 87.05±1.13 | 68.86±2.56 | 53.44±3.69 | 43.49±5.82 | 72.74±2.51 |
| Cao W[ | 14.21±11.31 | 85.86±1.36 | 64.45±2.08 | 45.94±4.09 | 35.77±12.37 | 72.24±1.43 |
| Z. Niu[ | 36.55±7.50 | 87.99±1.22 | 66.85±3.60 | 51.58±2.65 | 38.73±3.83 | 74.61±2.59 |
| Polat, G[ | 27.74±17.36 | 86.62±1.77 | 71.31±4.00 | 57.02±4.19 | 44.97±3.78 | 72.54±3.87 |
| MFFM | 40.07±5.43 | 90.16±0.86 | 75.44±1.27 | 53.97±2.81 | 48.84±5.43 | 77.13±1.64 |
| Method | Precision (%) | Recall(%) | F1-score (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| High Risk | Low Risk | No Therapy | High Risk | Low Risk | No Therapy | High Risk | Low Risk | No Therapy | |
| MFFM | 93.34±0.90 | 81.33±1.50 | 74.24±2.59 | 94.14±0.90 | 81.34±3.00 | 73.19±4.95 | 93.74±0.55 | 81.30±1.41 | 73.59±2.09 |
表5 分级模型在简化溃疡风险分级中的性能评估
Tab.5 Performance evaluation of the grading model in simplified ulcer risk stratification
| Method | Precision (%) | Recall(%) | F1-score (%) | ||||||
|---|---|---|---|---|---|---|---|---|---|
| High Risk | Low Risk | No Therapy | High Risk | Low Risk | No Therapy | High Risk | Low Risk | No Therapy | |
| MFFM | 93.34±0.90 | 81.33±1.50 | 74.24±2.59 | 94.14±0.90 | 81.34±3.00 | 73.19±4.95 | 93.74±0.55 | 81.30±1.41 | 73.59±2.09 |
| Subject | Accuracy (%) | Precision (%) | Recall (%) | F1-score (%) |
|---|---|---|---|---|
| Trainee doctor | 59.93 | 71.76 | 59.93 | 58.54 |
| Junior physician | 76.59 | 76.21 | 76.60 | 75.97 |
| Senior physician | 77.02 | 78.12 | 75.48 | 76.34 |
| MFFM | 74.94 | 74.45 | 74.94 | 74.27 |
表6 分级模型与不同经验水平内镜医生诊断结果的比较
Tab.6 Comparison of the diagnostic results by the grading model and endoscopists with different levels of experience
| Subject | Accuracy (%) | Precision (%) | Recall (%) | F1-score (%) |
|---|---|---|---|---|
| Trainee doctor | 59.93 | 71.76 | 59.93 | 58.54 |
| Junior physician | 76.59 | 76.21 | 76.60 | 75.97 |
| Senior physician | 77.02 | 78.12 | 75.48 | 76.34 |
| MFFM | 74.94 | 74.45 | 74.94 | 74.27 |
| Subject | F1-score (%) | |||||
|---|---|---|---|---|---|---|
| Ia | Ib | IIa | IIb | IIc | III | |
| Trainee doctor | 59.09 | 56.17 | 55.25 | 53.93 | 33.73 | 79.47 |
| Junior physician | 88.54 | 70.10 | 53.62 | 60.94 | 75.00 | 82.95 |
| Senior physician | 70.30 | 87.00 | 76.00 | 54.03 | 66.15 | 89.33 |
| MFFM | 40.07 | 90.16 | 75.44 | 53.97 | 48.84 | 77.13 |
表7 分级模型与不同经验水平内镜医生在各溃疡分级中的F1得分比较
Tab.7 Comparison of F1 scores for different ulcer rebleeding risk grades between the grading model and endoscopists with different levels of experience
| Subject | F1-score (%) | |||||
|---|---|---|---|---|---|---|
| Ia | Ib | IIa | IIb | IIc | III | |
| Trainee doctor | 59.09 | 56.17 | 55.25 | 53.93 | 33.73 | 79.47 |
| Junior physician | 88.54 | 70.10 | 53.62 | 60.94 | 75.00 | 82.95 |
| Senior physician | 70.30 | 87.00 | 76.00 | 54.03 | 66.15 | 89.33 |
| MFFM | 40.07 | 90.16 | 75.44 | 53.97 | 48.84 | 77.13 |
| DFM | HFM | FFM | Accuracy (%) | Precision (%) | Recall (%) | F1-score (%) |
|---|---|---|---|---|---|---|
| √ | 69.61±3.22 | 69.84±3.17 | 69.61±3.22 | 68.98±3.07 | ||
| √ | √ | 73.84±1.06 | 73.34±1.39 | 73.84±1.06 | 73.20±1.29 | |
| √ | √ | √ | 74.94±1.10 | 73.88± 1.29 | 74.59±1.10 | 73.83±1.01 |
表8 各特征提取模块在消融实验中的分级性能对比
Tab.8 Hierarchical performance comparison of each feature extraction module in ablation experiments
| DFM | HFM | FFM | Accuracy (%) | Precision (%) | Recall (%) | F1-score (%) |
|---|---|---|---|---|---|---|
| √ | 69.61±3.22 | 69.84±3.17 | 69.61±3.22 | 68.98±3.07 | ||
| √ | √ | 73.84±1.06 | 73.34±1.39 | 73.84±1.06 | 73.20±1.29 | |
| √ | √ | √ | 74.94±1.10 | 73.88± 1.29 | 74.59±1.10 | 73.83±1.01 |
| DFM | HFM | FFM | F1-score (%) | |||||
|---|---|---|---|---|---|---|---|---|
| Ia | Ib | IIa | IIb | IIc | III | |||
| √ | 20.60±13.10 | 86.63±0.87 | 69.09±4.24 | 51.41±5.52 | 38.84±6.88 | 73.11±5.22 | ||
| √ | √ | 36.55±15.75 | 89.22±1.06 | 73.94±0.91 | 56.23±5.05 | 44.84±6.50 | 75.91±3.65 | |
| √ | √ | √ | 40.07±5.43 | 90.16±0.86 | 75.44±1.27 | 53.97±2.81 | 48.84±5.43 | 77.13±1.64 |
表9 消融实验中不同特征提取模块对6级溃疡F1得分的影响
Tab.9 Effect of different feature extraction modules on F1 score for different ulcer rebleeding risk grades in ablation experiments
| DFM | HFM | FFM | F1-score (%) | |||||
|---|---|---|---|---|---|---|---|---|
| Ia | Ib | IIa | IIb | IIc | III | |||
| √ | 20.60±13.10 | 86.63±0.87 | 69.09±4.24 | 51.41±5.52 | 38.84±6.88 | 73.11±5.22 | ||
| √ | √ | 36.55±15.75 | 89.22±1.06 | 73.94±0.91 | 56.23±5.05 | 44.84±6.50 | 75.91±3.65 | |
| √ | √ | √ | 40.07±5.43 | 90.16±0.86 | 75.44±1.27 | 53.97±2.81 | 48.84±5.43 | 77.13±1.64 |
| 1 | 陈 丽, 常青霞, 陈少銮. 在内镜下治疗消化性溃疡并发上消化道出血的临床疗效[J]. 中国药物经济学, 2024, 19(6): 67-9, 73. |
| 2 | Wang BL, Yu WT, Zhang ZY, et al. Assessing peptic ulcer risk with the HAMPROW score in the general Chinese population[J]. Sci Rep, 2024, 14(1): 4442. |
| 3 | Soldner T, Bakke K, Savage S. Surgical management of upper gastrointestinal bleeding[J]. Gastrointest Endosc Clin N Am, 2024, 34(2): 301-16. |
| 4 | Vakil N. Endoscopic diagnosis, grading, and treatment of bleeding peptic ulcer disease[J]. Gastrointest Endosc Clin N Am, 2024, 34(2): 217-29. |
| 5 | 李兆申. 消化性溃疡出血的Forrest分级与内镜治疗[J]. 中华消化内镜杂志, 2013, 30(11): 601-3. |
| 6 | 张秀敏, 赵昌东, 李 雪, 等. 基于Forrset分级分层指导内镜下治疗消化性溃疡出血的临床价值[J]. 中国急救复苏与灾害医学杂志, 2023, 18(3): 362-5. |
| 7 | 付 强. 消化性溃疡出血患者进行内镜下Forrest分级的临床意义[J]. 世界最新医学信息文摘, 2017, 17(9): 74. |
| 8 | Chiu PW. Bleeding peptic ulcers: the current management[J]. Dig Endosc, 2010, 22(): S19-21. |
| 9 | 聂玉强, 李瑜元, 吴惠生, 等. 消化性溃疡出血的FORREST分级及其与预后关系[J]. 内镜, 1995, 12(1): 3. |
| 10 | Romstad KK, Detlie TE, Søberg T, et al. Treatment and outcome of gastrointestinal bleeding due to peptic ulcers and erosions - (BLUE study)[J]. Scand J Gastroenterol, 2022, 57(1): 8-15. |
| 11 | Mackiewicz-Pracka A, Nehring P, Przybyłkowski A. Emergency endoscopic interventions in acute upper gastrointestinal bleeding: a cohort study[J]. Diagnostics, 2023, 13(23): 3584. |
| 12 | Yen HH, Wu PY, Wu TL, et al. Forrest classification for bleeding peptic ulcer: a new look at the old endoscopic classification[J]. Diagnostics, 2022, 12(5): 1066. |
| 13 | Klang E, Barash Y, Levartovsky A, et al. Differentiation between malignant and benign endoscopic images of gastric ulcers using deep learning[J]. Clin Exp Gastroenterol, 2021, 14: 155-62. |
| 14 | 王智杰, 高 杰, 孟茜茜, 等. 基于深度学习的人工智能技术在早期胃癌诊断中的应用[J]. 中华消化内镜杂志, 2018, 35(8): 551-6. |
| 15 | 黄 丽, 李艳霞, 吴练练, 等. 基于深度学习的良恶性胃溃疡人工智能辅助诊断系统研究[J]. 中华消化内镜杂志, 2020, 37(7): 476-80. |
| 16 | Yen HH, Wu PY, Su PY, et al. Performance comparison of the deep learning and the human endoscopist for bleeding peptic ulcer disease[J]. J. Med. Biol. Eng, 2021, 41(4): 504-13. |
| 17 | Yen HH, Wu PY, Chen MF, et al. Current status and future perspective of artificial intelligence in the management of peptic ulcer bleeding: a review of recent literature[J]. J Clin Med, 2021, 10(16): 3527. |
| 18 | Afonso J, Saraiva MJM, Ferreira JPS, et al. Development of a convolutional neural network for detection of erosions and ulcers with distinct bleeding potential in capsule endoscopy[J]. echniques and Innovations in Gastrointestinal Endoscopy, 2021, 23(4): 291-6. |
| 19 | He KM, Zhang XY, Ren SQ, et al. Deep residual learning for image recognition[C]//2016 IEEE Conference on Computer Vision and Pattern Recognition (CVPR). June 27-30, 2016. VegasLas, NV, USA. IEEE, 2016: 770-8, . |
| 20 | Sunitha S, Sujatha SS. An improved bleeding detection method for wireless capsule endoscopy (WCE) images based on AlexNet[C]//2021 3rd International Conference on Signal Processing and Communication (ICPSC). May 13-14, 2021. Coimbatore, India. IEEE, 2021: 11-15. |
| 21 | Sainju S, Bui FM, Wahid K. Bleeding detection in wireless capsule endoscopy based on color features from histogram probability[C]//2013 26th IEEE Canadian Conference on Electrical and Computer Engineering (CCECE). May 5-8, 2013. Regina, SK, Canada. IEEE, 2013: 1-4. |
| 22 | Dilna C, Gopi VP. A novel method for bleeding detection in Wireless Capsule Endoscopic images[C]//2015 International Conference on Computing and Network Communications (CoCoNet). December 16-19, 2015. Trivandrum, India. IEEE, 2015: 854-8. |
| 23 | Yuan YX, Li BP, Meng MQH. Bleeding frame and region detection in the wireless capsule endoscopy video[J]. IEEE J Biomed Health Inform, 2016, 20(2): 624-30. |
| 24 | Tuba E, Tomic S, Beko M, et al. Bleeding detection in wireless capsule endoscopy images using texture and color features[C]//2018 26th Telecommunications Forum (TELFOR). November 20-21, 2018. Belgrade. IEEE, 2018: 1-4. |
| 25 | Chen BZ, Li JX, Lu GM, et al. Lesion location attention guided network for multi-label thoracic disease classification in chest X-rays[J]. IEEE J Biomed Health Inform, 2020, 24(7): 2016-27. |
| 26 | Simonyan K, Zisserman A. Very deep convolutional networks for large-scale image recognition[C]// International Conference on Learning Representations (ICLR). May 7-9, 2015. San Diego, CA, USA. ICLR, 2015: 1-14. |
| 27 | Tan M, Le Q. EfficientNet: Rethinking Model Scaling for Convolutional Neural Networks[C]//Proceedings of the 36th International Conference on Machine Learning (ICML). Jun 9-15, 2019. Long Beach, CA, USA. Proceedings of Machine Learning Research, 97: 6105-14. |
| 28 | Cao WZ, Mirjalili V, Raschka S. Rank consistent ordinal regression for neural networks with application to age estimation[J]. Pattern Recognition Letters, 2020, 140: 325-31. |
| 29 | Niu ZX, Zhou M, Wang L, et al. Ordinal regression with multiple output CNN for age estimation[C]//2016 IEEE Conference on Computer Vision and Pattern Recognition (CVPR). June 27-30, 2016. Las Vegas, NV, USA. IEEE, 2016: 4920-8. |
| 30 | Polat G, Ergenc I, Kani HT, et al. Class distance weighted cross-entropy loss for ulcerative colitis severity estimation[C]//Annual Conference on Medical Image Understanding and Analysis. Cham: Springer, 2022: 157-71. |
| 31 | Liu TJ, Xie SN, Yu J, et al. Classification of thyroid nodules in ultrasound images using deep model based transfer learning and hybrid features[C]//2017 IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP). March 5-9, 2017. New Orleans, LA. IEEE, 2017: 919-23. |
| 32 | Xie JH, Guo LH, Zhao CK, et al. A Hybrid Deep Learning and Handcrafted Features based Approach for Thyroid Nodule Classification in Ultrasound Images[J]. J Physics ConSer, 2020, 1693(1): 012160. |
| No related articles found! |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||