2. Dalian Medical University, Dalian 116044, China
2. 大连医科大学,辽宁 大连 116044
The incidence of acute coronary syndrome (ACS) has been on the rise and was reported to occur in about 3 per 1000 in habitants globally [1]. Emergency revascularization restores coronary blood flow to improve the clinical outcomes of patients with ST-segment elevation myocardial infarction (STEMI)[2], which is associated with severe myocardial injury and a high mortality rate[3]. Diagnosis of STEMI as early as possible can be life-saving, and relies mainly on the detection of persistent uplift ST-segment elevation in two or more contiguous relevant leads. A recent trial showed that the mortality of patients with STEMI would increase by around 3.3% if primary percutaneous coronary intervention (PCI) was delayed by 10 min[4].
Primary PCI within 12 h is strongly recommended not only for patients with STEMI, but also for those with high-risk or very high-risk non-STEMI[5]. As a special equivalent of STEMI, de Winter syndrome was firstly described in 2008 by de Winter et al[6], who reported that 2% of patients with acute anterior myocardial infarction presented with a persistent and static hyperacute T wave but their ST segment was not elevated as seen in STEMI. Similar findings were also reported by Verouden et al[7]. de Winter syndrome requires emergency revascularization, otherwise the hyperacute T wave would remain fixed to easily give rise to complications and adverse clinical events [8-9]. The ECG characteristics of this syndrome can be summarized as up-sloping ST-segment depression (about 1 to 3 mm) at the J point in the precordial leads, with a persistent hyperacute T wave as in STEMI that would not progress into classic ST-segment elevation. The QRS waves are usually normal but occasionally can be slightly widened. In addition, poor R-wave progression in the precordial leads can be observed in occasional cases[7, 9-10]. ST elevation by 1-2 mm in aVR lead is a more common finding, which can be easily confused with ST elevations seen in cases of left main coronary artery occlusion. In this case report, we describe a rare case of de Winter syndrome in a 63-year-old male patient, who presented with ST-segment elevation with special electrocardiogram (ECG) characteristics and was successfully rescued by emergency PCI.
CASE REPORTA 63-year-old man with underlying conditions of diabetes mellitus and hypertension was admitted for persistent chest pain for about 3 h after exercise. The patient reported a history of smoking for more than 20 years but quitt smoking 20 years ago. Physical examination of the patient yielded no positive findings. Immediate laboratory tests reported normal liver and kidney functions without elevations of serum creatinine kinase-myocardial band (CK-MB) or troponin I (cTNI). But examination with echocardiogram showed abnormal motion of the left ventricular wall accompanied by a decrease of left ventricular ejection fraction (LVEF) to 38%.
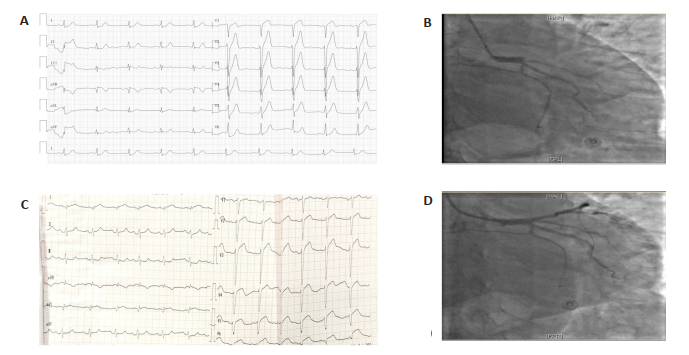
ECG examination showed basically normal findings except for the poor R-wave progression in the leads of V1 to V4. Further careful examination of the ECG revealed obvious depressions of the J point and up-sloping ST segment in the leads of V2 to V6, and a slight ST segment elevation was noted in the lead aVR. Based on these findings, a clinical diagnosis of de Winter syndrome was considered (Fig. 1A), which might result from occlusion of the proximal left anterior descending (LAD) coronary artery[8, 11]. Coronary angiography (CAG) and possible PCI were then scheduled immediately.
|
Fig.1 ECG and coronary angiography findings of the patient before and after PCI. A: Immediate 12- lead ECG of the patient after admission to the emergency department; B: Characteristics of initial coronary angiography; C: Repeated ECG after PCI; D: Repeated coronary angiography after stenting. |
Before the procedures, the patient received medications with aspirin and ticagrelor at the loading doses of 300 mg and 180 mg, respectively. Two experienced interventionists performed CAG via the transradial approach, which, as expected, revealed a thrombotic occlusion of the proximal LAD coronary artery with Thrombolysis in Myocardial Infarction (TIMI) grade 0 in-vessel blood flow (Fig. 1B). PCI was performed subsequently, in which the culprit vessel was pre-dilated using a 2.5 mm×15 mm balloon with a pressure of 10-12 atm and a 3.5 mm × 20 mm BUMA drug eluting stent (DES) was implanted successfully. A TIMI grade 2 to 3 flow was achieved after the procedure (Fig. 1D). A repeat ECG after PCI showed successful revascularization of the occluded vessel (Fig. 1C).
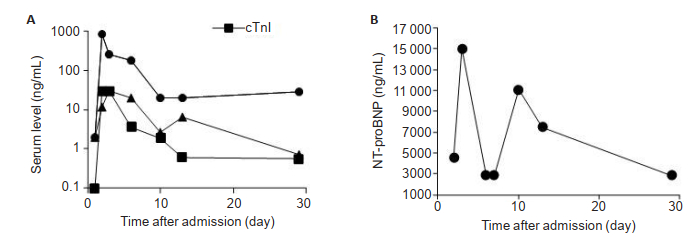
The patient was transferred to the coronary care unit for secondary prevention after PCI, and statins, β-blockers, aldosterone antagonists or angiotensinconverting enzyme inhibitors were given if necessary. Laboratory detections of CK-MB, cTNI, and myoglobin were performed on a daily basis, and the results were consistent with the myocardial enzyme curves diagnostic of acute myocardial infarction (Fig. 2A). On the third day, the level of NT-pro BNP of the patient increased sharply to 15 000 pg/mL (Fig. 2B), and the classic symptoms of congestive heart failure occurred with progressive aggravation. Lyophilized recombinant human brain natriuretic peptide was infused at a loading dose of 1.5 μg/kg followed by a maintenance dose of 0.0075 μg·kg-1· min-1 for 3 days. The patient was discharged 2 weeks later and followed up every month via telephone. The patient experienced no major adverse cardiac events 8 months after the procedure except for recurrence of chronic heart failure every few months.
|
Fig.2 Changes in serum levels of cTnI, CK-MB, myoglobin (A) and NT-pro BNP (B) of the patient after admission. |
de Winter syndrome is a rare form of anterior STEMI equivalent characterized by a unique electrocardiogram (ECG) pattern. Epidemiological studies show that de Winter syndrome is more likely to occur in male patients, who often have a younger age and frequently the comorbidity of dyslipidemia as compared with patients with STEMI[5]. The clinical presentation of de Winter syndrome is mainly extensive anterior-wall myocardial infarction, which leads to contraction dysfunction of the left ventricle [12] and possibly explains the frequent recurrences of chronic heart failure in such patients whose ECG does not report significantly decreased LVEF.
The reasons for the absence of ST-segment elevation in de Winter syndrome remain elusive. A previous study suggested that the special ECG characteristics was associated with the development of collateral circulation following transmural ischemia[13], while in another study, such ECG characteristics was presumed to result from a mutation of Kir 6.2 gene, which was responsible for the activation of sarcolemmal ATP-sensitive potassium (KATP) channels[14].
In the event of STEMI, early reperfusion alleviates ischemic myocardial damage to improve the clinical outcomes of the patients, and primary PCI within 2 h is therefore strongly recommended[15]. de Winter syndrome should be considered as a high-risk STEMI, for which emergency revascularization is strongly recommended within the time window of intervention following the current guidelines[13]. Given the rare incidence of this special syndrome, careful analysis of the ECG patterns for any unusual changes may increase the chances for its accurate early detection and timely intervention to reduce the mortality of the patients.
| [1] |
Fox KA, Eagle KA, Gore JM, et al. The global registry of acute coronary events, 1999 to 2009-GRACE[J]. Heart, 2010, 96(14): 1095-101. DOI:10.1136/hrt.2009.190827 |
| [2] |
Roffi M, Patrono C, Collet JP, et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC)[J]. Eur Heart J, 2016, 37(3): 267-315. DOI:10.1093/eurheartj/ehv320 |
| [3] |
Goldberg RJ, Spencer FA, Gore JM, et al. Thirty-year trends (1975 to 2005) in the magnitude of, management of, and hospital death rates associated with cardiogenic shock in patients with acute myocardial infarction: a population-based perspective[J]. Circulation, 2009, 119(9): 1211-9. DOI:10.1161/CIRCULATIONAHA.108.814947 |
| [4] |
Scholz KH, Maier SKG, Maier LS, et al. Impact of treatment delay on mortality in ST-segment elevation myocardial infarction (STEMI) patients presenting with and without haemodynamic instability: results from the German prospective, multicentre FITT-STEMI trial[J]. Eur Heart J, 2018, 39(13): 1065-74. DOI:10.1093/eurheartj/ehy004 |
| [5] |
Rokos IC, French WJ, Mattu A, et al. Appropriate cardiac Cath Lab activation: optimizing electrocardiogram interpretation and clinical decision-making for acute ST-elevation myocardial infarction[J]. Am Heart J, 2010, 160(6): 995-1003. DOI:10.1016/j.ahj.2010.08.011 |
| [6] |
de Winter RJ, Verouden NJ, Wellens HJ, et al. A new ECG sign of proximal LAD occlusion[J]. N Engl J Med, 2008, 359(19): 2071-3. DOI:10.1056/NEJMc0804737 |
| [7] |
Verouden NJ, Koch K T, Peters R J, et al. Persistent precordial "hyperacute" T-waves signify proximal left anterior descending artery occlusion[J]. Heart, 2009, 95(20): 1701-6. DOI:10.1136/hrt.2009.174557 |
| [8] |
Goktas MU, Sogut O, Yigit M, et al. A novel electrocardiographic sign of an ST-segment elevation myocardial infarction-equivalent: de Winter syndrome[J]. Cardiol Res, 2017, 8(4): 165-8. DOI:10.14740/cr576w |
| [9] |
De Winter RW, Adams R, Verouden N J, et al. Precordial junctional ST-segment depression with tall symmetric T-waves signifying proximal LAD occlusion, case reports of STEMI equivalence[J]. J Electrocardiol, 2016, 49(1): 76-80. DOI:10.1016/j.jelectrocard.2015.10.005 |
| [10] |
Martinez-Losas P, Fernandez-Jimenez R. de Winter syndrome[J]. CMAJ, 2016, 188(7): 528. DOI:10.1503/cmaj.150816 |
| [11] |
Carr MJ, O'Shea JT, Hinfey PB. Identification of the STEMI-equivalent de Winter electrocardiogram pattern after ventricular fibrillation cardiac arrest: a case report[J]. J Emerg Med, 2016, 50(6): 875-80. DOI:10.1016/j.jemermed.2016.03.022 |
| [12] |
Martinez-Losas P, Fernandez-Jimenez R. de Winter syndrome[J]. CMAJ, 2016, 188(7): 528. DOI:10.1503/cmaj.150816 |
| [13] |
Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization[J]. Eur Heart J, 2019, 40(2): 87-165. DOI:10.1093/eurheartj/ehy394 |
| [14] |
Li RA, Leppo M, Miki T, et al. Molecular basis of electrocardiographic ST-segment elevation[J]. Circ Res, 2000, 87(10): 837-9. DOI:10.1161/01.RES.87.10.837 |
| [15] |
Verheugt FW. Acute myocardial infarction associated with ST segment elevation and the new european society of cardiology guidelines[J]. Heart, 2009, 95(13): 1112-7. DOI:10.1136/hrt.2008.151829 |
 2020, Vol. 40
2020, Vol. 40

