即刻种植以其可以缩短治疗周期、减少手术次数、保存牙槽嵴的体量以及获得术后更为协调的美学形态而日益受到重视[1-2]。实施即刻种植,具有比较充足的骨量使植体能够获得稳妥的初期稳定性是以往认可的关键因素[3-4],充足骨量的具体体现之一就是根尖下应该至少有3~5 mm骨质存在[5-7]。关于即刻种植的认识目前还存在争议,也有认为只要能够获得初期稳定性,即使骨质条件不够理想,也仍然适于即刻种植[8-9]。前牙区或前磨牙区的即刻种植应用,已经形成了成熟的手术操作规范,取得良好而明确的效果。关于后牙区的即刻种植应用资料尚不多见,效果也不够明确。在后牙区实施即刻种植,由于多根牙的特点、骨质缺损以及崎岖起伏的骨质形态,无论拔牙手术、种植窝洞制备或者植体安放等都存在较大困难,对医生的经验和操作技巧都存在挑战性[10-11]。为了能够平稳操作以获取最大程度骨质保存,有尝试在拔牙前实施种植窝洞制备,试图借助牙体在位达到平稳操作的目的,获得理想的种植位点,并最大程度保存残存骨质使能提供必要的初期稳定性[12-13]。但骨质与牙质硬度的差异以及牙周炎的松动牙体、或根尖周存在病变,在牙体在位前提下制备,并不容易实现平稳控制钻头的目标,现有的工具设备的限制反而可能使操作更为复杂。上颌磨牙区的拔牙病例,往往牙槽窝骨壁可能保持完整,牙龈没有显著缺损,仅仅牙槽窝底部骨质菲薄,放弃即刻种植改行延期种植除延长疗程,还可能因牙槽嵴废用性萎缩后需要开展创伤大、操作复杂的上颌窦底外提升术。本文对于上颌后牙区上颌窦底骨质菲薄的拔牙病例,尝试微创拔牙后实施种植窝洞制备,开展即刻种植,收集资料进行回顾性的总结分析,探讨磨牙区拔牙后即刻种植操作的可能性及可行性。
1 资料和方法 1.1 一般资料收集南方医科大学口腔医院(广东省口腔医院)自2010年1月~2017年12月上颌磨牙牙槽窝与上颌窦底间隔骨质薄弱的拔牙病例,开展新鲜拔牙创同期上颌窦底提升并即刻种植。研究项目经过学术伦理委员会审查同意,参与研究项目的病员均被告知有关治疗事宜及风险,并签署术前手术治疗同意书。病例纳入标准:无系统性手术禁忌;牙槽窝、上颌窦底平均骨质厚度约1 mm;牙槽窝骨壁完整;牙龈形态没有显著退缩缺损;牙位上颌窦底最低点至牙槽嵴顶高度达到8 mm;至少一侧邻牙存留;上颌窦没有明显化脓性感染或仅有轻度牙源性上颌窦炎。排除标准:存在系统性或代谢性疾患不适于手术;急性炎症期;上颌窦底骨质薄弱不足0.5 mm或存在洞穿性缺损;上颌窦底骨质厚度超过2 mm;牙龈显著萎缩或缺损;牙龈瘘管;牙位上颌窦底最低点至牙槽嵴顶高度不足7 mm;邻牙存在未经控制的牙髓炎、根尖周炎或牙周炎;牙槽窝骨壁缺损(失);双侧邻牙同时缺失;上颌窦存在显著弥漫性、化脓性炎症。
1.2 手术方法术前MCT影像学检查,确定牙槽窝、牙槽骨形态和上颌窦底骨质厚度等,并进行相关测量记录。微创拔除病患牙,彻底清除炎性肉芽组织,在牙槽窝底部的中央制备种植洞形。制备时一旦阻力消失、有落空感后即刻收力停止操作。逐级扩大洞形,植入根状植体。植体长度参照现存牙龈形态、牙槽嵴高度以及邻牙牙槽骨高度确定,植体平面应位于牙槽嵴顶骨缘下1~2 mm。植体稳定就位后,安置愈合基台,愈合基台顶部平面平齐牙龈缘或低于牙龈缘。植体与牙槽窝空隙填塞植入人工骨粉,视残余牙槽窝口面积大小及牙龈游离程度缝合或不缝合伤口,缝线的阻挡机械性缩小伤口。植体呈暴露状态,开放式愈合。
术后给予常规3日处方抗生素及止痛药,1周后拆除缝线。嘱避免触碰患牙。术后6月完成种植牙冠修复,牙冠固定螺丝旋紧扭力要求达到30 Ncm;MCT检查,确定种植体生长愈合情况,测量牙槽骨质高度。随访种植牙功能的发挥情况。
1.3 即刻种植成功标准触诊无松动,无明显叩痛,无感染,无明显牙周袋,发挥正常咀嚼功能,无咀嚼不适。X光影像学检查:植体周围骨质无吸收破坏征象[14]。
1.4 参数指标测定术前及术后6月MCT检查,测量相应参数。术前后近中牙槽嵴高度:牙齿或种植体近中牙槽嵴顶中点至相应上颌窦底水平面的垂直距离;术前后远中牙槽嵴高度:牙齿或种植体远中牙槽嵴顶中点至相应上颌窦底水平面的垂直距离;术前后颊侧牙槽嵴高度:牙齿或种植体颊侧牙槽嵴顶中点至相应上颌窦最底点水平面的垂直距离;术前后腭侧牙槽嵴高度:牙齿或种植体腭侧牙槽嵴顶中点至相应上颌窦最底点水平面的垂直距离;术前后牙槽嵴宽度:牙齿或种植体颊、腭侧牙槽嵴顶中点之间的颊腭径宽度。
1.5 统计学采用SPSS 20.0统计软件进行统计学处理,本文变量参数属于手术前后配对样本均数的比较,采用配对t检验。取单侧检验,检验水准设为α=0.05,P < 0.5为差异有统计学意义。
2 结果共收集32例样本纳入本研究,病员年龄53~68岁,平均年龄59.8岁。随访时间最短12月,最长8年(96月),累计成功率100%。植体长度8.5~10 mm,植体直径4.5~5.5 mm。在制备洞形后,可见灰白色上颌窦底粘膜完整,鼻腔鼓气试验未见上颌窦粘膜破损、穿孔征象。植体初始稳定性或就位扭力,为最小仅仅依靠手指轻松旋入就位后,可以维持静立不动,不足10 Ncm,较大外力可使植体倾倒或移动;最大则可达到30 Ncm,可以抵御较大外力的作用而维持不动,坚固稳定。
术后过程平稳,没有明显炎性征象。术后1周牙龈肿胀消褪,色泽质地外观等已基本接近正常,植体保持稳定。牙龈收缩使牙槽窝口面积缩小,残留牙槽窝口虽可见骨粉颗粒暴露,但已被粉红色质地致密肉芽组织包裹,伤口清洁。术后1月,牙龈生长关闭牙槽窝口,并包围愈合基台形成袖口。术后6月,植体稳定性良好,牙龈质地坚实。影像学检查显示植体周围骨质生长良好,种植后6月颊、腭、近、远中牙槽嵴高度以及颊腭宽度有轻微减少,经过统计学t检验,显示种植前后的牙槽骨尺寸变化不具有统计学意义(表 1)。
| 表 1 术前及术后6月牙槽骨的变化 Tab.1 Variation of the alveolar bone at 6 months after the operation (mm) |
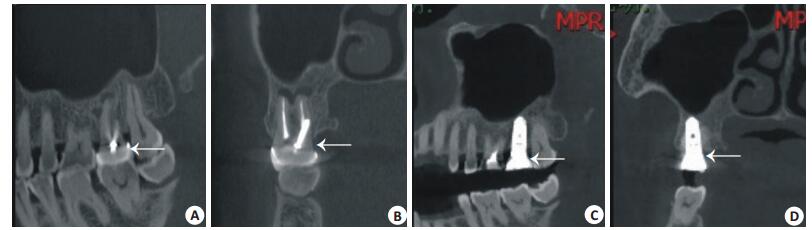
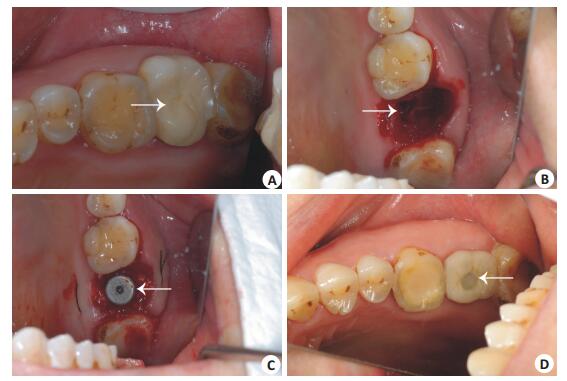
未见上颌窦明显炎性征象,植体端部平齐或突入上颌窦底约1 mm(图 1)。安装牙冠,固定螺丝扭力30 Ncm。牙龈形态良好,种植牙可以发挥正常咀嚼功能,咀嚼时无明显疼痛不适,患者对于治疗效果满意(图 2)。
|
图 1 MCT影像学资料 Fig.1 Micro-CT images of a patient before and after the operation. The images before tooth extraction show the antero-posterior (A) and coronal (B) view of 17 (arrows) with poor bone quality at the bottom of the socket. At 6 months after the implantation, the anteroposterior (C) and coronal (D) view of the implants at 17 (arrows) showed that the end of implants were close to the bottom of the sinus. |
|
图 2 种植示意图 Fig.2 Procedure of implantation immediately following tooth extraction. A: Tooth 17 before extraction (arrow); B: The socket following the extraction, and the arrow indicates the cavity for implantation; C: Anchoring of the implant (the arrow indicates the healing abutment); D: Crown (arrow) installation. |
即刻种植面临的主要困难是不易获得足够的初期稳定性,其根源在于拔牙创的不良骨质条件,尤其以磨牙区多根牙拔牙创更为显著。所谓的骨质条件不佳,具体表现为骨质缺损不全、牙槽窝骨床崎岖不平而且起伏度较大、骨质薄弱等,使种植窝洞的制备变得极为困难,操作时工具容易打滑形成制备偏差,薄弱骨质在工具的震动下容易崩溃,最终可能造成植体不良就位或缺乏初期稳定性,导致丧失种植时机。为克服骨质条件不佳也能够获得足够的初期稳定性,在植体的外形设计方面开展了诸多的尝试努力,比如设计成锥形植体,使其具有一定的自攻性,更易获得牢固的初期稳定性[15-20]。本项研究选择根状植体,在上颌磨牙区骨质薄弱的情况下获得了必要的初期稳定性,其植入扭力在部分病例甚至达到了30 Ncm。在骨质薄弱的新鲜拔牙创开展即刻种植,种植体的选择以根状种植体首选为宜。在操作层面为克服骨床凹凸不平、骨质薄弱对于制备种植窝洞造成的困难,已经有尝试在多根牙拔牙之前制备种植窝洞[21-23]。其设计思路是在牙根在位时,创造出一种平坦的操作界面,使钻头能够平稳、精确运作,获得良好的种植洞形。然而这种方法仅适用于不多的理想牙根条件,存在局限性,比如:(1)如果牙根骨质粘连紧密难以拔出,制备后再拔牙不能避免破坏薄弱的窝洞骨质,反而丧失种植洞形;(2)如果牙根松散,钻头仍然难于保持平稳运作,而且操作中牙根可能随着钻头发生运动,进而破坏薄弱的骨质,失去种植条件;(3)牙根本身溃烂不堪,则不存在形成平坦操作界面的条件;(4)需要足够锋利的制备钻头才能达到高效切割牙齿。本研究显示,在拔牙后再进行种植窝洞地制备,可以形成合适的种植窝洞洞形,并使植体获得相应的初期稳定性,操作具有可行性。在上颌拔牙创紧邻上颌窦底的骨质进行制备,并不必然造成上颌窦粘膜的损伤穿破,非即刻种植禁忌症。我们的经验是,在多根牙微创拔牙后制备种植窝洞,可以精确评估骨质面貌,选择适当的器械在种植位点准确操作,有利于种植位点、深度及角度的把握。种植窝洞制备时,需要注意2个关键技巧:(1)充分利用根分叉间隔骨质较多的优势,使尽可能多的骨质对植体形成夹持固定作用;(2)控制好力度,仔细体验钻头阻力的微妙变化,一旦阻力消失应迅速收力回撤,应避免强烈的落空感损伤上颌窦粘膜。本项目病例可以经由种植窝洞观察到完整的灰白色上颌窦底粘膜,表明上颌窦粘膜没有发生穿破损伤。植体就位不宜进入窦底过深,深度应控制在1~2 mm之内。进入上颌窦过长的植体对于骨整合属于无效长度,还有存在激惹上颌窦感染的隐患。本研究的根状植体系列最短为8.5 mm,故选择纳入的病例要求其上颌窦底至牙槽嵴顶距离不少于7 mm。也必须指出,多根牙拔牙后制备种植窝洞的手术操作,在现有的技术条件下对于医生的专业素养确实存在很大的挑战性。除了需要具备丰富的实践经验以及有意识的操作训练外,也需要未来在手术操作方式上采取某种必要的改进和简化,使其更有利于获得普及开展。
在骨质条件欠佳的前提下,希望即刻种植植体达到高植入扭力的初期稳定性是不现实的。根据文献检索,主流的观认为即刻种植的植入扭力越高越好,30~40 Ncm是即刻种植初始稳定性的阈值,最好能达到40 Ncm以上,甚至高至50~60 Ncm才能保证植体获得骨整合[24-26]。也有少数观点认为低植入扭力无碍于即刻种植获得理想的骨整合[27-30]。本研究虽然有植体的植入扭力达到30 Ncm,但也有植体植入扭力不到10 Ncm,甚至仅仅依靠手指力旋入就位后维持不动,稳定性是不可靠的,轻微外力就可能造成植体松动,结果最终仍然获得了良好的骨整合效果。本结果提示:(1)薄弱的骨质条件,在精确制备以及选择锥形种植体的前提下,即刻种植植体仍然可能获得足够的初期稳定性;(2)高初期稳定性可能并非即刻种植的必要条件,植体低植入扭力就位,也可能获得种植成功;(3)选用根状植体,即刻种植的初始稳定性也存在不确定性,取决于复杂的骨床条件,如骨面形态以及骨质强度等。即刻种植骨整合的关键,在于愈合期植体能够始终维持固定,不发生运动,使骨质可以不受干扰地生长。可能施加于植体的外力在于各种形式的口腔运动,如:进食咀嚼、吞咽、讲话、刷牙、漱口等等,这些运动持续性地作用于植体,就有可能使植体发生松动,影响骨质愈合。如果能够避免这些口腔运动作用于植体,无论植入扭力的大小,都有可能获得骨整合。理论上,植入扭力越大,初始稳定性越好,植体的抗干扰能力越强。即刻种植,在低植入扭力无法获得高初始稳定性的条件下,为避免口腔运动对于植体愈合的扰动,需要病患方面给予配合,比如:避免术区咀嚼、避免经常性潜意识的舌体触碰、刷牙时避免触碰术区等;在医生方面,植入植体时需要控制植体愈合基台表面不高于牙龈缘,最好低于牙龈缘1 mm左右,必要时使用愈合帽并适度延长愈合时间。
本研究中,虽然即刻种植涉及上颌窦底,但并未在窦底粘膜下植骨。有认为上颌窦底内提升术,是否植骨,对于临床效果没有显著影响[31]。因为植体的主体部分位于牙槽嵴内,暂未观察到不良影响,对于其远期效果还需要进一步随访追踪观察。
3.2 即刻种植的伤口处理如何处理伤口,也是即刻种植面临的一个主要困惑。目前有3种不同的方式选择,包括埋入式(闭合式)、穿龈式(开放式)以及半闭合式(半开放式)等。有研究认为穿龈式伤口,对于种植伤口愈合及植体良好的功能发挥等,与埋入式之间并无显著差异[32-34]。主流观点倾向于选择闭合式伤口处理方式,认为可以保证植体获得骨整合,避免植骨材料流失或感染[35-36]。理论上,闭合式伤口在形式上利于屏蔽口腔运动对于植体的扰动,此点对于即刻种植植体初始稳定性较小或不可靠时尤为重要。但采取埋入式的伤口方式,需要切取转移牙龈瓣,使手术程序变得复杂,还可能加剧创伤,破坏局部组织的解剖形态。而且种植材料占位形成支撑,即使切断骨膜也不能彻底松解张力,术后伤口容易裂开,可能不能达到关闭伤口的预期效果。半闭合式的创伤以及复杂程度介于埋入式和开放式之间,解剖形态的破坏不及闭合式,可以缩小伤口,部分屏蔽口腔运动的扰动,有一定合理性。虽然即刻种植拔牙创可能较大,但植体形成空间占位,减少了骨粉植入量,使渗血可以比较快速渗透骨粉并凝血机化,粘滞固定了骨粉,最终完成骨化的时间也较短;另外,植体对于骨粉也具有一定的支撑固定作用,植体愈合基台在牙槽窝口占位也缩小了牙槽窝口的缺损面积,缩短了牙龈生长关闭伤口的时间,客观上进一步减少了骨粉流失的可能性。即使开放式伤口,也不会发生骨粉的显著流失[37-38]。本项研究病例,选择自然牙槽窝口的开放式愈合方式,通过平齐或降低植体愈合基台平面避免口腔运动的扰动,最终也显示出良好的愈合效果,避免了牙龈瓣转移所造成的创伤和破坏,显示开放式伤口可以是即刻种植恰当的伤口处理方式。缝合的意义在于:(1)固定游离的牙龈,有利于愈合;(2)缝线的物理性阻挡作用可以缩小伤口,初期固定骨粉。
本研究结果显示种植术后6月,各个维度的牙槽嵴高度以及牙槽嵴颊腭宽度,均存在微小程度的减少,提示即刻种植后牙槽嵴仍然存在吸收现象,但经统计学检验显示这种术前后的差异没有统计学意义,牙槽嵴尺寸的减少变化不具有显著的临床意义,即刻种植牙的牙槽嵴维持作用良好。从伤口处理以及牙槽嵴维持的角度,即刻种植是更合适的种植位点保存技术[39-41]。
综上所述,在上颌磨牙区拔牙创骨质条件欠佳、上颌窦底骨质薄弱的情况下实施即刻种植,能够避免损伤上颌窦底粘膜并取得良好的种植修复效果。本研究病例样本数较小,关于即刻种植有关技术要点的阐述,有必要在未来能够开展更大规模的调查来获得支持。
| [1] |
Zuffetti F, Capelli M, Galli F, et al. Post-extraction implant placement into infected versus non-infected sites: a multicenter retrospective clinical study[J].
Clin Implant Dent Relat Res, 2017, 19(5): 833-40.
DOI: 10.1111/cid.2017.19.issue-5. |
| [2] |
石磊, 黄盛兴, 刘慧凤, 等. 前牙区数字化即刻种植即刻修复病例报道及文献回顾[J].
口腔疾病防治, 2017, 25(2): 119-22.
|
| [3] |
Narad C, Lingraj JB, Aulakh KK, et al. Assessment of primary stability of the implant placed in prepared infected extraction sockets[J].
J Oral Biol Craniofac Res, 2016, 8(3): 154-7.
|
| [4] |
Abi-Aad HL, Daher FI, Baba NZ, et al. Insertion torque of variablethread tapered implants in the posterior maxilla: a clinical study[J].
J Prosthodont, 2018: 12965.
|
| [5] |
Luay Y, Asraa T, Mohemad I, et al. Evaluation of bone healing following immediate and delayed dental implant placement[J].
J Contemp Dent Pract, 2009, 10(4): 35-42.
|
| [6] |
周磊, 岳新新. All-on-Four技术在口腔种植领域中的应用进展[J].
口腔疾病防治, 2017, 25(1): 1-7.
|
| [7] |
Tallarico M, Xhanari E, Pisano M, et al. Single post-extractive ultrawide 7 mm-diameter implants versus implants placed in molar healed sites after socket preservation for molar replacement: 6- month post-loading results from a randomised controlled trial[J].
Eur J Oral Implantol, 2016, 9(3): 263-75.
|
| [8] |
Levin BP. The correlation between immediate implant insertion torque and implant stability quotient[J].
Int J Periodontics Restorative Dent, 2016, 36(6): 833-40.
|
| [9] |
Tettamanti L, Andrisani C, Bassi MA, et al. Post extractive implant: evaluation of the critical aspects[J].
Oral Implantol (Rome), 2017, 10(2): 119-28.
DOI: 10.11138/orl/2017.10.2.119. |
| [10] |
Crespi R, Cappare P, Gastaldi G, et al. Buccal-lingual bone remodeling in immediately loaded fresh socket implants: a cone beam computed tomography study[J].
Int J Periodontics Restorative Dent, 2018, 38(1): 43-50.
|
| [11] |
Gluckman H, Pontes CC, Du Toit J. Radial plane tooth position and bone wall dimensions in the anterior maxilla: a CBCT classification forimmediateimplantplacement[J].
JProsthDen, 2018, 120(1): 50-6.
|
| [12] |
Chen YQ, Yuan SS, Zhou N, et al. Transcrestal sinus floor augmentation with immediate implant placement applied in three types of fresh extraction sockets: a clinical prospective study with 1- year follow-up[J].
Clin Implant Dent Relat Res, 2017, 19(6): 1034-43.
|
| [13] |
Jun SH, Park CJ, Hwang SH, et al. The influence of bone graft procedures on primary stability and bone change of implants placed in fresh extraction sockets[J].
Maxillofac Plast Reconstr Surg, 2018, 40(1): 10.
DOI: 10.1186/s40902-018-0149-1. |
| [14] |
Becker CM, Wilson J, Jensen OT. Minimum criteria for immediate provisionalization of single-tooth dental implants in extraction sites: a 1-Year retrospective study of 100 consecutive cases[J].
J Oral Maxillofac Surg, 2011, 69(2): 491-7.
|
| [15] |
Cucchi A, Vignudelli E, Franco SA, et al. Tapered, double-lead threads single implants placed in fresh extraction sockets and healed sites of the posterior Jaws: a multicenter randomized controlled trial with 1 to 3 years of Follow-Up[J].
Biomed Res Int, 2017, 13(9): 5.
|
| [16] |
Matys J, Swider K, Flieger R, et al. Assessment of the primary stability of root analog zirconia implants designed using cone beam computed tomography software by means of the periotest (R) device: An ex vivo study. A preliminary report[J].
Adv Clin Exp Med, 2017, 26(5): 803-9.
|
| [17] |
Aimetti M, Manavella V, Corano L, et al. Three-dimensional analysis of bone remodeling following ridge augmentation of compromised extraction sockets in periodontitis patients: A randomized controlled study[J].
Clin Oral Implants Res, 2018, 29(2): 202-14.
DOI: 10.1111/clr.13099. |
| [18] |
Chappuis V, Araujo MG, Buser D. Clinical relevance of dimensional bone and soft tissue alterations post- extraction in esthetic sites[J].
Periodontol 2000, 2017, 73(1): 73-83.
DOI: 10.1111/prd.12167. |
| [19] |
Gluckman H, Salama M, Du Toit J. A retrospective evaluation of 128 socket-shield cases in the esthetic zone and posterior sites: partial extraction therapy with up to 4 years follow-up[J].
Clin Implant Dent Relat Res, 2018, 20(2): 122-9.
DOI: 10.1111/cid.2018.20.issue-2. |
| [20] |
Heckmann SM, Moertlbauer B, Rieder D, et al. Alveolar ridge dimension 6 months after implant placement with simultaneous hard tissue augmentation[J].
Int J Oral Maxillofac Implants, 2017, 32(2): 408-14.
|
| [21] |
Scarano A. Traditional postextractive implant site preparation compared with pre-extractive interradicular implant bed preparation in the mandibular molar region, using an ultrasonic device: a randomized pilot study[J].
Int J Oral Maxillofac Implants, 2017, 32(3): 655-60.
|
| [22] |
Valenzuela S, Olivares JM, Weiss N. Immediate implant placement by interradicular bone drilling before molar extraction: clinical case report with one-year follow-Up[J].
Case Rep Dent, 2018, 7(1): 6.
|
| [23] |
Kara MI, Yanik S, Sari F. Simultaneous retrieval of root fragment, sinus lifting with particulated bone graft, and immediate dental implant insertion[J].
J Craniofac Surg, 2016, 27(3): e309-11.
|
| [24] |
Jun SH, Park CJ, Hwang SH, et al. The influence of bone graft procedures on primary stability and bone change of implants placed in fresh extraction sockets[J].
Maxillofac Plast Reconstr Surg, 2018, 40(1): 10.
DOI: 10.1186/s40902-018-0149-1. |
| [25] |
Demircan S, Cankaya AB. Is immediate implant placement possible in the maxillary molar area? An anatomical study[J].
Quintessence Int, 2016, 47(10): 853-9.
|
| [26] |
Feng L, Zhang L, Cui Y, et al. Clinical evaluations of mineralized collagen in the extraction sites preservation[J].
Regene biomate, 2016, 3(1): 41-8.
DOI: 10.1093/rb/rbv027. |
| [27] |
Norton MR. The influence of low insertion torque on primary stability, implant survival, and maintenance of marginal bone levels: a closed-cohort prospective study[J].
Int J Oral Maxillofac Implants, 2017, 32(4): 849-57.
DOI: 10.11607/jomi.5889. |
| [28] |
Valdec S, Pasic P, Soltermann A, et al. Alveolar ridge preservation with autologous particulated dentin-a case series[J].
International J Implant Dentister, 2017, 3(1): 10.
|
| [29] |
Maiorana C, Poli PP, Deflorian M, et al. Alveolar socket preservation with demineralised bovine bone mineral and a collagen matrix[J].
J Period Imp Sci, 2017, 47(4): 194-210.
|
| [30] |
Malchiodi L, Balzani L, Cucchi A, et al. Primary and secondary stability of implants in postextraction and healed sites: a randomized controlled clinical trial[J].
Int J Oral Maxillofac Implants, 2016, 31(6): 1435-43.
DOI: 10.11607/jomi.4710. |
| [31] |
赖红昌, 史俊宇. 上颌窦提升术[J].
口腔疾病防治, 2017, 25(1): 8-12.
|
| [32] |
许竞, 崔宝仪, 高文峰, 等. 即刻种植牙龈软组织伤口的特点及其愈合方式[J].
广东医学, 2013, 34(7): 1066-9.
DOI: 10.3969/j.issn.1001-9448.2013.07.031. |
| [33] |
Di Girolamo M, Arullani CA, Calcaterra R, et al. Preservation of extraction socket in immediate implant placement: a clinical study[J].
Oral Implantol (Rome), 2016, 9(4): 222-32.
|
| [34] |
Choi HK, Cho HY, Lee SJ, et al. Alveolar ridge preservation with an open-healing approach using single-layer or double-layer coverage with collagen membranes[J].
J Periodontal Implant Science, 2017, 47(6): 372-80.
|
| [35] |
Zuiderveld EG, Meijer H, den Hartog L, et al. Effect of connective tissue grafting on peri-implant tissue in single immediate implant sites:ARCT[J].
J Clin Periodontol, 2017, 45(2): 253-64.
|
| [36] |
El Chaar E, Oshman S, Cicero G, et al. Soft tissue closure of grafted extraction sockets in the anterior maxilla: a modified palatal pedicle connective tissue flap technique[J].
Int J Periodontics Restorative Dent, 2017, 37(1): 99-107.
DOI: 10.11607/prd.2746. |
| [37] |
Assaf JH, Assaf DD, Antoniazzi RP, et al. Correction of buccal dehiscence during immediate implant placement using the flapless technique: a tomographic evaluation[J].
J Periodontol, 2017, 88(2): 173-80.
DOI: 10.1902/jop.2016.160276. |
| [38] |
Chang H, Kim S, Hwang JW, et al. Comparative, randomized, double-blind clinical study of alveolar ridge preservation using an extracellular matrix-based dental resorbable membrane in the extraction socket[J].
J Periodontal Implant Science, 2017, 47(3): 165-73.
DOI: 10.5051/jpis.2017.47.3.165. |
| [39] |
Pirker W, Immediate KA, Non-Submerged N. Root-analogue zirconia implant in single tooth replacement[J].
Int J Oral Maxillofac Surg, 2008, 37(3): 293-5.
|
| [40] |
Felice P, Zucchelli G, Cannizzaro GA, et al. Immediate, immediatedelayed (6 weeks) and delayed (4 months) post-extractive single implants: 4-month post-loading data from a randomised controlled trial[J].
Eur J Oral Implantol, 2016, 9(3): 233-47.
|
| [41] |
Al Qabbani A, Razak NH, Al Kawas SA, et al. The efficacy of immediate implant placement in extraction sockets for alveolar bone preservation: a clinical evaluation using three-dimensional cone beam computerized tomography and resonance frequency analysis value[J].
J Craniofac Surg, 2017, 28(4): e318-25.
DOI: 10.1097/SCS.0000000000003569. |
 2019, Vol. 39
2019, Vol. 39
