2. Department of Ophthalmology, Zhejiang Hospital, Hangzhou 310013, China
2. 浙江医院眼科,浙江 杭州 310013
Primary uveal lymphoma is a type of intra-ocular lymphoma. Unlike the intra-ocular lymphomas involving the retina and vitreous, primary uveal lymphoma generally has a low-grade nature and an indolent clinical course. [1] It is a relatively rare condition, and the diagnosis can be challenging. Primary uveal lymphoma can be subdivided into primary choroidal, iridal and ciliary body lymphoma. Since 1920, approximately 80 cases have been reported in the literature.[2] Primary choroidal lymphoma accounts for the majority of these cases. Uveal lymphoma is typically a non-Hodgkin's lymphoma, most frequently of B-cell origin. The predominant subtype is extra-nodal marginal zone B-cell lymphoma (EMZL) or mucosa-associated lymphoid tissue (MALT). Here, we present a rare case of primary uveal lymphoma involving the choroid, ciliary body, iris and conjunctiva that was successfully treated with radiotherapy and achieved a full remission.
CASE REPORTA 36-year-old systemically healthy man was referred to our clinic in December 2013, with a complaint of recurrent episodes of redness and blurred vision of the right eye over the previous year. He had been diagnosed with uveitis of the right eye at other hospitals. Systemic and topical corticosteroids were prescribed, but the treatment was ineffective, and his vision progressively worsened. He had an unremarkable ocular history and denied any significant past medical history.
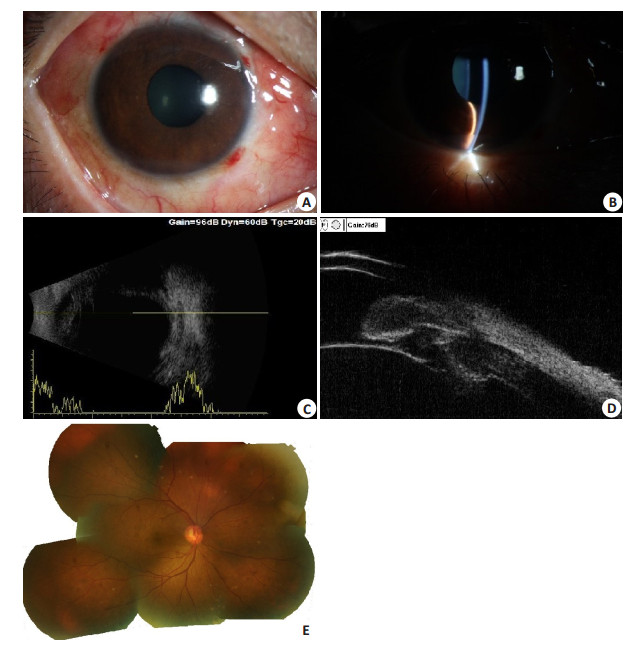
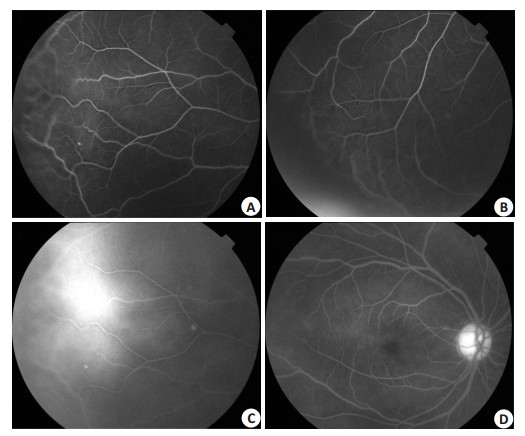
On ocular examination, the visual acuity (VA) was 0.25 for the right eye and 1.0 for the left eye. The intraocular pressure (IOP) was 25.5 mmHg for the right eye and 10.7 mmHg for the left eye. Slit-lamp examination of the right eye revealed conjunctival hyperemia and hyperplasia(Fig. 1A), a clear cornea without keratic precipitates (KP), flare in the anterior chamber(+), a wavily bulged iris, a shallow peripheral anterior chamber, and a 2 mm high thin leukocyte-like exudate settled in the inferior anterior chamber with a hypopyon appearance (Fig. 1B). The vitreous cavity was clear of cells. A dilated fundic examination revealed irregular peripheral sub-retinal elevation (Fig. 1E). B-scan ultrasonography showed choroidal thickening and detachment (Fig. 1C). Ultrasound biomicroscopy(UBM) revealed irregular thickening of the iris, ciliary body and cyst formation (Fig. 1D). Fluorescein angiography demonstrated peripheral sub-retinal elevation with dilated and tortuous vessels (Fig. 2A, Fig. 2B), late stage leakage of peripheral blood vessels (Fig. 2C), and late stage hyper-fluorescence of the choroidal background and optic disk at (Fig. 2D). Examination of the left eye was unremarkable. The results of blood cell counts, cranial MRI, chest X-ray, cerebrospinal fluid (CSF) evaluation, serology for HIV and syphilis, were normal or negative. Further evaluation of aqueous fluid demonstrated only occasional degenerated lymphocytes.
|
Figure 1 Ocular examination of right eye. A: Color picture of anterior segment showed conjunctival congestion and hyperplasia; B: Wavily bulged iris, and leukocyte-like exudate like hypopyon appearance; C: UBM showed irregular thickening of the iris, ciliary body and cyst formation; D: B-scan ultrasonography showed choroidal thickening and detachment; E: Jigsaw of fundus color photograph showed irregular peripheral sub-retinal elevation. |
|
Figure 2 Fundus fluorescein angiography of right eye. A and B: Peripheral sub-retinal elevation with the dilated and tortuous vessels; C: Leakage of the peripheral retinal vessels; D: Late stage hyper-fluorescence of the choroidal background and optic disk. |
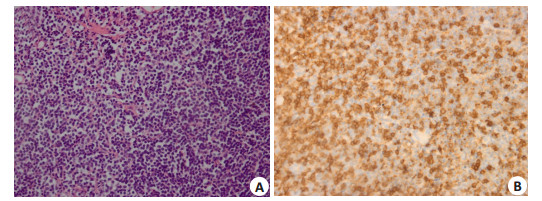
In March 2014, we noticed bulbar and palpebral pink-colored conjunctival lesions of the right lower lid. An incisional conjunctival and scleral biopsy was performed and the results revealed only lymphoid hyperplasia (ALH). The diagnosis remained unclear. When the patient returned almost 1 year later in January 2015, the symptoms were not relieved. His IOP was 34 mmHg in the right eye with distinct conjunctival hyperemia. Fundic examination showed an exacerbation of the sub-retinal lesions. The ultrasonographic scanning showed a significant thickening of the choroid. A second conjunctival biopsy was then performed. Histomorphological examination revealed a lymphoid hyperplastic change(Fig. 3A). Immunohistochemistry (Fig. 3B) showed positive staining for CD20, CD43, CD3, CD5, and Ki-67 (5% positive cells), whereas CD10 was negative. IgH/IgK gene rearrangement analysis revealed a monoclonal population of B lymphocytes. The pathological diagnosis of mucosa-associated lymphoid tissue (MALT) lymphoma was made. A patient was then treated with low-dose external beam radiotherapy (total 35 Gy). Two months after the treatment, his VA in the right eye had improved to 1.0, and IOP was 14.0 mmHg. The conjunctival lesions had regressed excellently. The choroid reattached and the thickening disappeared in ultrasound examination. He was still in complete remission at the final follow up in October 2017.
|
Figure 3 Histomorphological and Immunohistochemistry examination of conjunctival biopsy. A: Histomorphology revealed a lymphoid hyperplasia change; B: Immunohistochemistry showed positive staining for CD43 (Original magnification: ×200). |
Primary uveal lymphoma is found predominantly in males and occurs unilaterally [2-5]. Because of its prolonged, benign course, it has been called ''uveal pseudotumours'' or ''reactive lymphoid hyperplasia''[6, 7]. Since the symptoms and signs of uveal lymphoma can mimic many other ophthalmic diseases, such as scleritis, uveal effusion syndrome, uveal metastases, and various uveitis, patients frequently go undiagnosed or misdiagnosed for long periods before the correct diagnosis is established[8-10]. The key early finding on ophthalmic examination is yellow-white choroidal infiltrates [3]. In some advanced cases, including this case, sub-conjunctival extension can occur [10-13]. A correlation has been observed between uveal lymphoma and coexisting ocular adnexal lymphoma (OAL). Uveal lymphoma may in fact be classified as a variant of OAL[14-17].
Diagnosis of primary uveal lymphoma should be made after a histopathological examination of the lesion and exclusion of any other systemic lymphoma, as was done in this case. Immunohistochemistry and gene rearrangement analysis have allowed for a more accurate diagnosis[18]. Primary uveal EMZL or MALT lymphoma is generally believed to be an indolent tumor with a good prognosis. Systemic extension only appears in a handful of cases and occurs a couple of years after treatment without CNS involvement[15]. However, if untreated, it can cause glaucoma and retinal detachment, eventually making the eye blind and painful.[19]In most previously reported cases of primary uveal EMZL, patients are initially treated with steroids, laser, glaucoma medications, surgery, and other therapies before the initiation of proper treatment. Many of the eyes were ultimately enucleated either due to difficulties in diagnosis or unbearable pain secondary to glaucoma.
Currently, there is no optimal treatment consensus because of its rare nature and the limited information about treatment and long-term effects. Treatment options proposed in the literature include radiotherapy and Rituximab [2]. Chlorambucil has been effectively used in one reported case [20]. Low-dose external beam radiotherapy (EBRT) has frequently been reported to induce full remission with few side effects[3]. In our case, the patient obtained full remission with excellent vision 2 months after EBRT, and no systemic extension was noted at the two year follow up.
CONCLUSIONSThe diagnosis of primary uveal lymphoma is usually delayed due to its insidious onset, nonspecific manifestation and masquerading symptoms. The tumor is commonly indolent and carries a favorable prognosis. It tends to respond well to external radiation treatment, and patients usually obtain full remission, as was the case with our patient. It is important for ophthalmologists to consider this rare disease in the differential diagnosis of persistent uveitis.
| [1] | Chan CC, Haen SP, Möhle R, et al. Primary intraocular lymphoma [D]. Springer: Berlin Heidelberg, 2016. |
| [2] | Coupland SE. Lymphomas BE:Understanding intraocular damato[J]. Clin Exp Ophthalmol, 2008, 36: 564-78. DOI: 10.1111/ceo.2008.36.issue-6. |
| [3] | Aronow ME, Portell CA, Sweetenham JW, et al. Uveal lymphoma: clinical features, diagnostic studies, treatment selection, and outcomes[J]. Ophthalmology, 2014, 121(1): 334-41. DOI: 10.1016/j.ophtha.2013.09.004. |
| [4] | Chute DJ, Biscotti CV, Singh AD. Uveal lymphoma[J]. Monogr Clin Cytol, 2012, 21(21): 31-43. |
| [5] | Coupland SE, Foss HD, Hidayat AA, et al. Extranodal marginal zone B cell lymphomas of the uvea: an analysis of 13 cases[J]. J Pathol, 2002, 197(3): 333-40. DOI: 10.1002/path.1130. |
| [6] | Cockerham GC, Hidayat AA, Bijwaard KE, et al. Re-evaluation of "reactive lymphoid hyperplasia of the uvea": an immunohistochemical and molecular analysis of 10 cases[J]. Ophthalmology, 2000, 107(1): 151-8. DOI: 10.1016/S0161-6420(99)00025-1. |
| [7] | Ryan SJ, Zimmerman LE, King FM. Reactive lymphoid hyperplasia, an unusual form of intraocular pseudotumor[J]. Trans Am Acad Ophthalmol Otolaryngol, 1972, 76(13): 652-71. |
| [8] | Tavallali A, Shields CL, Bianciotto C, et al. Choroidal lymphoma masquerading as anterior ischemic optic neuropathy[J]. Eur J Ophthalmol, 2010, 20(5): 959-62. DOI: 10.1177/112067211002000525. |
| [9] | O'keefe JS, Sippy BD, Martin DF, et al. Anterior chamber infiltrates associated with systemic lymphoma: report of two cases and review of the literature[J]. Ophthalmology, 2002, 109(2): 253-7. DOI: 10.1016/S0161-6420(01)00934-4. |
| [10] | Rasic DM, Stankovic Z, Terzi T, et al. Primary extranodal marginal zone lymphoma of the uvea associated with massive diffuse epibulbar extension and focal infiltration of the optic nerve and meninges, clinically presented as uveitis masquerade syndrome: a case report[J]. Med Oncol, 2010, 27(3): 1010-6. DOI: 10.1007/s12032-009-9325-6. |
| [11] | Holz FG, Boehmer HV, Mechtersheimer G, et al. Uveal non-Hodgkin's lymphoma with epibulbar extension simulating choroidal effusion syndrome[J]. Retina, 1999, 19(4): 343-6. DOI: 10.1097/00006982-199919040-00015. |
| [12] | Ciulla TA, Bains RA, Jakobiec FA, et al. Uveal lymphoid neoplasia: a clinical-pathologic correlation and review of the early form[J]. Surv Ophthalmol, 1997, 41(6): 467-76. DOI: 10.1016/S0039-6257(97)00015-5. |
| [13] | Chang TS, Byrne SF, Gass JD, et al. Echographic findings in benign reactive lymphoid hyperplasia of the choroid[J]. Arch Ophthalmol, 1996, 114(6): 669-75. DOI: 10.1001/archopht.1996.01100130661005. |
| [14] | Fuller ML, Sweetenham J, Schoenfield L, et al. Uveal lymphoma:a variant of ocular adnexal lymphoma[J]. Leuk Lymphoma, 2008, 49(7): 2393-7. |
| [15] | Sarraf D, Jain A, Dubovy S, et al. Mucosa-associated lymphoid tissue lymphoma with intraocular involvement[J]. Retina, 2005, 25(1): 94-8. DOI: 10.1097/00006982-200501000-00018. |
| [16] | Baryla J, Allen LH, Kwan K, et al. Choroidal lymphoma with orbital and optic nerve extension: case and review of literature[J]. Can J Ophthalmol, 2012, 47(12): 79-81. |
| [17] | Tagami M, Nagai T, Sekimukai D, et al. Uveal extranodal marginal zone B-cell lymphoma of the mucosa-associated lymphoid tissue type with concomitant extraocular lesions in a Japanese man[J]. Jpn J Ophthalmol, 2011, 55(10): 585-7. |
| [18] | Sharara N, Holden JT, Wojno TH, et al. Ocular adnexal lymphoid proliferations: clinical, histologic, flow cytometric, and molecular analysis of forty-three cases[J]. Ophthalmology, 2003, 110(6): 1245-54. DOI: 10.1016/S0161-6420(03)00330-0. |
| [19] | Duker JS, Shields JA, Ross M. Intraocular large cell lymphoma presenting as massive thickening of the uveal tract[J]. Retina, 1987, 7(1): 41-5. DOI: 10.1097/00006982-198700710-00010. |
| [20] | Rospond-Kubiak I, Kocięcki J, Stopa M. Primary uveal lymphoma effectively managed with oral chlorambucil:a case report[J]. J Med Case Reports, 2013(7): 173-9. |
 2018, Vol. 38
2018, Vol. 38

