Purtscher's or Purtscher-like retinopathy is an occlusive retinal microangiopathy most commonly developed after craniocerebral trauma, thoracic crushing injury, acute pancreatitis, renal failure, various kinds of autoimmune diseases, or due to the administration of a multitude of chemotherapeutic agents or [1-2]. We describe here a case of Purtscher-like retinopathy associated with systemic antibiotic anaphylaxis, and review the literatures on this rare condition.
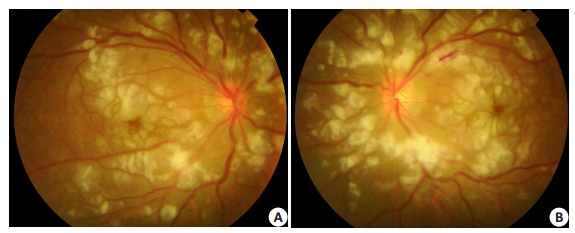
CASE REPORTAn 18-year-old female inpatient of rheumatology department presented subacute painless decreased vision in both eyes. She had a history of intravenous use of pazufloxacin 2 weeks before admission due to high fever, chill and sore-throat. Itching rashes appeared on her chest and back 3 days after the drug administration and consequently the drug was withdrawn and changed to cefazolin. One week later she was admitted because of deterioration of her whole body condition and was diagnosed as anaphylaxis probably due to pazufloxacin. During the first week after admission, she underwent epileptic seizure twice. Imaging examination showed pulmonary interstitial changes, plural effusion, pericardial effusion, and pelvic carving effusion. Visual acuity was counting fingers in each eye. No inflammation in anterior chamber and vitreous body presented. Ocular fundus examination showed bilateral multiple cottonwool spots and Purtscher flecken around the optic disc, and a few intra-retinal hemorrhages (Fig. 1).
|
Figure 1 Ocular fundus examination. A: Right eye; B: Left eye. Photos showed bilateral symmetric multiple cotton-wool spots and Purtscher flecken surround the optic disc, and a few intra-retinal hemorrhages. |
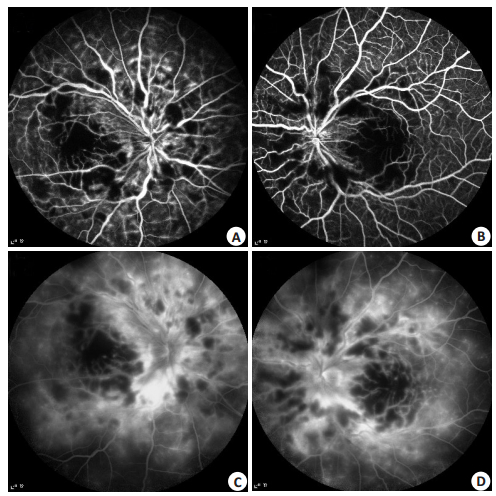
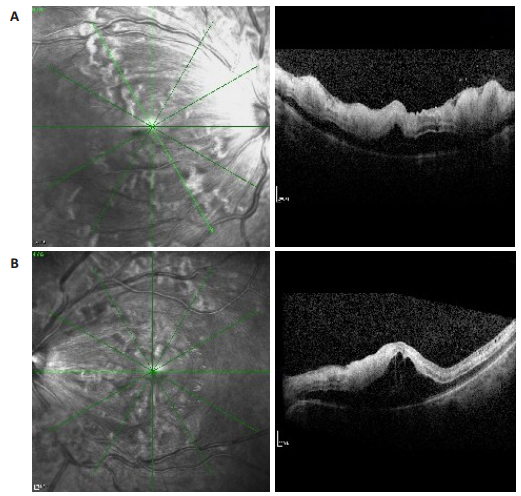
Fluorescein angiography showed retinal vein tortuous expansion, retinal arterial and capillary occlusion around the optic disc and macular non-perfusion in the early stage (Fig. 2A & B) and vessel wall staining, leakage of veins, venules and some arterioles in the late phase (Fig. 2C & D). OCT showed inter-retinal edema and structure disorganization of macular due to exudate and leakage (Fig. 3). Bilateral Purtscher-like retinopathy was diagnosed, probably caused by antibiotic pazufloxacin anaphylaxis. After pulse corticosteroid, administration of anti-anaphylactic agent, and general support therapy for one month, the patient recovered systemically. Despite twice intravitreal injection of steroid and Ranibizumab, there were still large area of capillary non-perfusion and neovacularizations developed in the bilateral retina, resulting in vitreous hemorrhage. The patient's visual acuity was still light perception after right-eye vitrectomy and presented no improvement during the postoperative follow-up of two years.
|
Figure 2 Fudus fluorescein angiography. A, B: retinal vein tortuous expansion, retinal arteriolar and capillary occlusion around the optic disc and macular nonperfusion in early stage of the right eye and left eye; C, D: Vessel wall staining and leakage of veins, venules and some arterioles in the late phase. |
|
Figure 3 Optical coherence tomography(OCT) bilaterally. A: right eye; B: left eye. Tomography showed inter-retinal edema and structural disorganization of macular due to exudate and leakage. |
Purtscher's retinopathy generally occurs as a result of craniocerebral trauma, thoracic crushing injury, or long bone fracture. It was first described in 1910 by Otmar Purtscher a middle-aged man who fell off a tree and suffered cranial trauma [2, 11]. When there is a non-traumatic etiology, the correct designation is Purtscher-like retinopathy. Purtscher-like retinopathy has been reported to occur in several pathologic conditions and after different medical disorders and interventions, including acute pancreatitis, collagen diseases, renal failure, childbirth, retrobulbar anesthesia, periorbital injections, chemotherapy for cancer, cerebro-or cardiovascular surgery, and acute myocardial infarction [3-10]. Patients with Purtscher-like retinopathy usually present with a wide range of visual acuities, from a visual acuity (VA) of 6/6 with minimal visual disturbance, to severe visual loss with a vision of light perception, which have similar appearance in the ocular fundus. The most common signs of this retinopathy are cotton-wool spots, retinal hemorrhages, Purtscher flecken, pseudo-cherry red spot, and macular edema[2, 9, 11]. Relative afferent pupillary defects have been reported in cases with unilateral disease[12]as well as bilateral disease[13]. It is widely assumed that the Purtscher flecken is the result of occlusion of the precapillary arterioles [13]. The characteristic finding is intra-retinal whitening but with a clear zone (within 50 mm) on either side of the retinal arterioles, venules, and precapillary arterioles. This is in contrast to cotton-wool spots, which have ill-defined edges and are located superficially over vessels [2]. Fluorescein angiography may show leakage of dye from retinal arterioles, capillaries, and venules in patients with relatively mild Purtscher's retinopathy. Arteriolar obstruction is noted in more severe cases[3-11]. The typical appearance of the macula on optical coherence tomography (OCT) at initial diagnosis is that of varying degrees of retinal thickening and edema with some cases even presenting subretinal serous fluid[14-16]. Several months on, most cases have resolution of the thickening, but some still show retinal atrophy and destruction of the foveal architecture. There are many theories about pathogenesis but Purtscher's microangiopathy is typically thought to be caused by precapillary occlusion, fat emboli, leukoaggregation, or other mechanisms [4, 17-18].
Because of the small frequency of this pathology, estimated as 0.24 per million[2], it's hard to perform prospective trial for the evidence-based treatment guideline. At present, there is no consensus on the treatment. The most frequent treatment prescribed is high-dose intravenous steroids, usually with a tapering dose of oral steroids subsequently. The rationale behind corticosteroid use is sound, as it is capable to inhibit complement activation and granulocyte aggregation, as well as to allow nerve fiber recovery by stabilizing damaged neuronal membranes and microvascular channels. However, there are controversies over the visual recovery via the administration of steroid[2, 17, 19]. Observation and treatment of the underlying etiology may be the most reasonable therapeutic option with no adverse drug effects. There are isolated reports using peripheral vasodilator, hyperbaric oxygen therapy, or low molecular weight heparin postulated intravenously to increase choroidal and retinal blood flow, dilate retinal arterioles, or increases oxygen supply to the choroids and inner retina[17, 19, 21-22]. For sever cases, the visual prognosis was usually poor. Large area of arteriole occlusion leads to hypoxia and neovascularization subsequently. Like the case we report here, prompt intra-vitreous injection of anti-VEGF agent or panretinal photocoagulation is necessary. Unfortunately, this patient could not obtain enough injections due to her poor systemic condition then.
CONCLUSIONFor the first time, we present here a sever case of Purtscher-like retinopathy associated with antibiotic anaphylaxis probably due to pazufloxacin. The literatures associated with Purtscher-like retinopathy have pointed out diverse causes and the consequent visual impairment varies significantly [1, 23]. Prompt management of the underlying condition is crucial in giving the patient the best chance to restore vision [11].
| [1] | Agrawal A, Mckibbin M. Purtscher's retinopathy: epidemiology, clinical features and outcome[J]. Br J Ophthalmol, 2007, 91(11): 1456-9. DOI: 10.1136/bjo.2007.117408. |
| [2] | Agrawal A, Mckibbin MA. Purtscher's and purtscher-like retinopa-thies: a review[J]. Surv Ophthalmol, 2006, 51(2): 129-36. DOI: 10.1016/j.survophthal.2005.12.003. |
| [3] | Holló G. Frequency of purtscher's retinopathy[J]. Br J Ophthalmol, 2008, 92(8): 1159. |
| [4] | Kincaid MC, Green WR, Knox DL, et al. A clinicopathological case report of retinopathy of pancreatitis[J]. Br J Ophthalmol, 1982, 66(4): 219-26. DOI: 10.1136/bjo.66.4.219. |
| [5] | Wu C, Dai R, Dong F, et al. Purtscher-like retinopathy in systemic lupus erythematosus[J]. Am J Ophthalmol, 2014, 158(6): 1335-41. DOI: 10.1016/j.ajo.2014.09.001. |
| [6] | Okwuosa TM, Lee EW, Starosta M, et al. Purtscher-like retinopathy in a patient with adult-onset Still's disease and concurrent thrombotic thrombocytopenic purpura[J]. Arthritis Rheum, 2007, 57(1): 182-5. DOI: 10.1002/(ISSN)1529-0131. |
| [7] | Ustaoglu M, Önder F, Solmaz N, et al. Purtscher-Like retinopathy associated with atypical hemolytic uremic syndrome[J]. Turk J Ophthalmol, 2017, 47(6): 348-50. |
| [8] | Blodi BA, Williams CA. Purtscher-like retinopathy after uncomplicated administration of retrobulbar anesthesia[J]. Am J Ophthalmol, 1997, 124(5): 702-3. DOI: 10.1016/S0002-9394(14)70917-1. |
| [9] | Ang LJPS, Chang BCM. Purtscher-like retinopathy -A rare complication of acute myocardial infarction and a review of the literature[J]. Saudi J Ophthalmol, 2017, 31(4): 250-6. DOI: 10.1016/j.sjopt.2017.05.009. |
| [10] | Oshida E, Machida S, Nishimura T, et al. Purtscher-like retinopathy associated with cerebro-or cardiovascular surgery[J]. Am J Ophthalmol Case Rep, 2017, 8(8): 62-6. |
| [11] | Miguel AI, Henriques F, Azevedo LF, et al. Systematic review of Purtscher's and Purtscher-like retinopathies[J]. Eye (Lond), 2013, 27(1): 1-13. |
| [12] | Kuroda M, Nishida A, Kikuchi M, et al. Purtscher's retinopathy followed by neovascular glaucoma[J]. Clin Ophthalmol, 2013, 7(4): 2235-7. |
| [13] | Olson J, Rouhani B, Mandava N. Sub-Tenon's triamcinolone for post-partum purtscher's-like retinopathy[J]. Clin Ophthalmol, 2008, 2(1): 195-8. |
| [14] | Alasil T, Tokuhara K, Bowes LD, et al. Purtscher-like retinopathy: optical coherence tomography and visual field findings[J]. Ophthalmic Surg Lasers Imaging, 2010, 9(6): 1-4. |
| [15] | Yaylali SA, Bromand N, Kilic G. A new OCT finding in Purtscher-Like retinopathy[J]. Ophthalmic Surg Lasers Imaging Retina, 2018, 49(1): 64-9. DOI: 10.3928/23258160-20171215-11. |
| [16] | Coady PA, Cunningham ET, Vora RA, et al. Spectral domain optical coherence tomography findings in eyes with acute ischaemic retinal whitening[J]. Br J Ophthalmol, 2015, 99(5): 586-92. DOI: 10.1136/bjophthalmol-2014-304900. |
| [17] | Wang AG, Yen MY, Liu JH. Pathogenesis and neuroprotective treatment in Purtscher's retinopathy[J]. Jpn J Ophthalmol, 1988, 42(4): 318-22. |
| [18] | Harrison TJ, Abbasi CO, Khraishi TA. Purtscher retinopathy: an alternative etiology supported by computer fluid dynamic simulations[J]. Invest Ophthalmol Vis Sci, 2011, 52(11): 8102-7. DOI: 10.1167/iovs.11-7734. |
| [19] | Atabay C, Kansu T, Nurlu G. Late visual recovery after intravenous methylprednisolone treatment of Purtscher's retinopathy[J]. Ann Ophthalmol, 1993, 25(9): 330-3. |
| [20] | Nesmith BL, Bitar MS, Schaal S. The anatomical and functional benefit of bevacizumab in the treatment of macular edema associated with Purtscher-like retinopathy[J]. Eye (Lond), 2014, 28(8): 1038-40. |
| [21] | Dollery CT, Bulpitt CJ, Kohner EM. Oxygen supply to the retina from the retinal and choroidal circulation at normal and increased arterial Oxygen tension[J]. Invest Ophthalmol, 1969, 8(3): 588-94. |
| [22] | Beiran I, Goldenberg I, Adir Y, et al. Early hyperbaric oxygen therapy for retinal artery occlusion[J]. Eur J Ophthalmol, 2001, 11(4): 345-50. DOI: 10.1177/112067210101100405. |
| [23] | Holak HM, Holak S. Prognostic factors for visual outcome in purtscher retinopathy[J]. Surv Ophthalmol, 2007, 52(1): 117-8. DOI: 10.1016/j.survophthal.2006.10.012. |
 2018, Vol. 38
2018, Vol. 38

