2. 江西省上犹县人民医院普外科,江西 赣州 341200
2. Department of General Surgery, Shangyu People's Hospital, Jiangxi 341200, China
根据2012年WHO公布的全球癌症(CRC)统计资料显示,我国结直肠癌发病率及死亡率呈现快速上升趋势,已跃居所有癌症的第3位[1]。目前,手术仍然是结直肠癌最有效的治疗手段。近20年来,随着腹腔镜技术的迅猛发展及不断进步,腹腔镜技术已在胃肠外科领域中广泛应用,逐渐成为胃肠肿瘤治疗首选的手术方式,在我国,腹腔镜下直肠前切除术被认为是治疗直肠癌最为主要的手术方式之一[2-3]。近年来,关于直肠前切除术中保留左结肠动脉的研究越来越多,臧潞等[4]认为腹腔镜下直肠前切除术中保留左结肠动脉可以减少吻合口瘘的发生率,但不增加手术时间。沈荐等[5]研究发现保留左结肠动脉与不保留组相比,手术时间、术后排气时间、淋巴结清扫数目及预后并无统计学差异。以往的研究主要集中于吻合口瘘的发生率,淋巴结清扫数目,术后复发率等临床疗效指标,但对于术后腹胀、腹痛不适持续时间,住院时间,住院费用等指标的研究尚未见报道。因此,我院收集2014年12月~2016年12月间91例腹腔镜下直肠前切除术患者临床资料,对比两种术式的短期临床疗效指标,结果显示术中保留左结肠动脉能有效减少手术后并发症,缩短术后住院日,减少手术住院期间的总体费用,有效促地进患者术后快速康复,现将研究结果报道如下。
1 资料和方法 1.1 一般资料91例患者,男58例,女33例。年龄35~75岁,60.12±12.46岁。主要临床表现为粘液血便及排便习惯改变。纳入标准:术前经电子结肠镜检查、肿瘤位于腹膜返拆以上,术后病理证实为直肠腺癌。排除标准:术前行新辅助放化疗;并发肠梗阻或肠穿孔而行急诊手术;术前、术中发现远处脏器转移或腹腔广泛种植转移;术后病理证实为非腺癌;危重症患者。术前按术中保留左结肠动脉与否分为两组,保留左结肠动脉40例(观察组),不保留左结肠动脉51例(对照组)。两组在性别构成、年龄、肿瘤长径、肿瘤距肛缘距离方面均具无明显差异(P>0.05,表 1)。
| 表 1 两组患者的临床资料比较 Table 1 Comparison of clinical data between experimental group and control group (Mean±SD) |
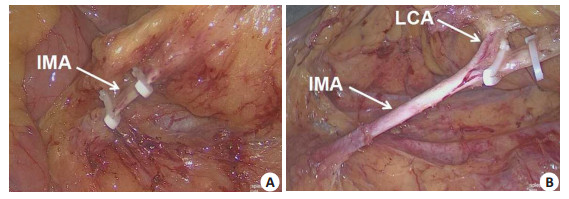
气管内全麻患者取头低足高截石位,建立人工气腹,于脐上约l cm建立观察孔,左、右下腹部置操作孔4个,进镜后常规探查,并根据术中探查情况进行临床分期。观察组于乙状结肠系膜内侧打开浆膜,分离至肾前间隙,向左侧、尾侧、头侧进一步游离、扩大层面间隙,显露并注意保护自主神经、左输尿管、左侧生殖血管。充分游离。肾前间隙后,解剖肠系膜下动脉,彻底清除肠系膜下动脉根部淋巴脂肪组织,脉络化血管。清晰显露左结肠动脉的走行方向,注意保护,避免损伤,在左结肠动脉的远端结扎、切断肠系膜下动脉(图 1B)。对照组直接在肠系膜下动脉根部结扎、切断血管(图 1A)。两组其余步骤均按腹腔镜下直肠癌前切除手术方式进行,切除肿瘤后在保证近端肠管自然下垂无张力的状态下,用管状吻合器行端端吻合,重建肠道。若近端肠管长度不够,则游离结肠脾曲,充分松解结肠,再行吻合以保证近端肠管自然下垂无张力。对于低位直肠癌及重建肠道后观察吻合口肠壁血运欠佳或者吻合质量欠佳者,则将末端回肠经右下腹辅助切口拖出,做预防性末端回肠双腔造口。
|
图 1 肠系膜下动脉不同位置的离断 Figure 1 Inferior mesenteric arterial ligation at different levels. A: Left clonic artery was unpreserved; B: Left colonic artery was preserved. IMA: inferior mesenteric artery; LCA: Left clonic artery. |
手术时间、术中出血量、术后排气排便时间、腹胀腹痛持续时间、术后住院天数、术后住院期间总费用、肠系膜根部淋巴结清扫数及预防性回肠造口和吻合口瘘的发生情况,其中手术时间、术中出血量以麻醉记录单为准,术后排气排便时间的统计排除回肠造口病例。
1.4 统计方法所有数据均采用SPSS16.0软件包进行分析处理,两独立样本采用均数的t检验分析,计量资料采用用均数±标准差,P < 0.05为差异有统计学意义;吻合口瘘等并发症发生率采用采用四格表资料的χ2检验,行×列表χ2检验及Fisher确切概率法分析,P < 0.05为差异有统计学意义。
2 结果91例患者均顺利完成手术,术中无中转开腹手术病例,术中无直肠破裂穿孔,无血管、输尿管及邻近器官损伤,吻合口无张力。两组患者手术时间、术中出血量及肠系膜根部淋巴结清扫数差异无统计学意义(P> 0.05),因低位直肠癌或吻合口血运欠佳行末端回肠预防性造口,观察组有3例,对照组有5例;观察组术后40例患者全部无发生吻合口瘘,对照组术后有3例患者发生吻合口瘘;术后腹胀持续时间,术后排气时间,术后排便时间,术后住院时间,住院费用见表 2,统计分析结果显示两组间术后腹胀持续时间、术后住院时间及住院费用,差异有统计学差异(P < 0.05)。
| 表 2 两组术后情况比较 Table 2 Comparison of post-operative features between experimental group and control group (Mean±SD) |
直肠癌术后吻合口瘘是直肠癌手术的最常见的并发症之一,也是直肠癌手术的严重的并发症之一[6-10]。直肠癌术后并发吻合口瘘可导致患者腹腔感染,加重患者术后腹胀、腹痛及发热等不适,多需加强抗感染、持续负压冲洗引流等进一步治疗措施,甚至再次手术等处理,大大延长患者的住院时间、增加患者的住院费用,严重损害患者的健康及经济利益[11-13]。其中导致吻合口瘘的原因除患者自身年龄、营养状况、术前放化疗等因素影响外,与患者术中吻合口血运及张力有着重要的密切关系[14-15]。
对于进展期直肠癌,术中要求清扫中央淋巴结,传统手术方式均在根部结扎离断肠系膜下动脉,即把左结肠动脉、乙状结肠动脉和直肠上动脉同时离断,以清扫中央淋巴结,提高根治效果。然而,有一部分患者术中出现降结肠血供不足,被迫扩大切除范围,需游离脾曲甚至切除降结肠,甚至有部分需要切除左侧横结肠,行横结肠直肠吻合,另外,还有一部分患者因吻合口血运欠佳,术后发生吻合口瘘,吻合口瘘是结直肠癌手术术后严重并发症之一[16-18]。吻合口血液供应是影响吻合口愈合的关键因素,同时也是术者决定是否行预防性回肠造口的重要因素[19-20]。吻合口近端血液供应主要依靠中结肠动脉与左结肠动脉之间的两支血管弓,即边缘动脉弓与罗兰弓。但人群中罗兰弓缺失率约为5% [21],边缘动脉在脾曲处的吻合缺失高达43% [22]。传统的直肠癌前切除术中对肠系膜下动脉的处理是于肠系膜下动脉根部进行结扎切断,切除左结肠动脉的主干,这势必会造成患有粥样硬化、缺失上述血管弓患者降结肠的血液供应不佳,从而引起吻合口瘘的发生。有学者现已开展了保留左结肠动脉的腹腔镜下直肠癌前切除手术,以保证吻合口充足的血运,降低吻合口瘘的发生,从而减少预防性回肠造口。Hinoi等[23]的研究得出保留左结肠动脉可降低中低位直肠癌吻合口瘘发生率,进而降低预防性回肠造口率。沈荐等[5]的对照研究中72例保留左结肠动脉患者无一例行预防性回肠造口,且无吻合口瘘发生;而41例不保留左结肠动脉患者中3例行预防性回肠造口。本研究中不保留左结肠动脉组患者中有5例加行预防性回肠造口,且术后3例发生吻合口瘘,而保留左结肠动脉组患者有3例行预防性回肠造口,但无吻合口瘘发生,虽然两组无统计学意义,这可能与本研究样本量不大有关,如扩大样本量,则可能有统计学差异,这与以往的研究基本一致。因此,术中保留左结肠动脉将可避免出现降结肠血供不足,也可改善吻合口血运欠佳情况,减少吻合口瘘的发生。
淋巴结转移是直肠癌的主要转移途径之一,是否发生淋巴转移是直肠癌患者预后的重要因素[24],术中淋巴结清扫的范围直接关系到直肠癌患者的预后效果。其中肠系膜下动脉根部淋巴结是进展期直肠癌淋巴结转移最常见部位之一[25]。我们采用血管鞘内清扫的方法,在清扫肠系膜下动脉根部旁淋巴结的同时,保留左结肠动脉结扎离断乙状结肠动脉和直肠上动脉。比较腹腔镜下直肠前切除术中保留左结肠动脉和不保留左结肠动脉两组间的手术时间、术中出血量、术后排气排便时间、术后腹胀、腹痛不适持续时间、肠系膜根部淋巴结清扫数以及预防性回肠造口和吻合口瘘的发生情况,以及术后肿瘤的局部复发率。结果显示:两组患者手术时间、术中出血量、肠系膜根部淋巴结清扫数及末端回肠预防性造口差异无统计学意义(P>0.05),两组患者术后发生腹痛持续时间、术后住院时间及手术住院期间的总体费用,两组比较具有统计学差异(P < 0.05)。腹腔镜下直肠前切除术中保留左结肠动脉能有效保证降结肠和吻合口近端的血供,减少术后吻合口漏发生率,有利于创伤肠道功能的恢复,使患者术后提早排气排便,从而减轻患者术后腹胀、腹痛不适,有利于患者早期下床活动,早期进食,最终减少患者术后住院日、并发症的发生以及手术住院期间总体费用的效果。
综上所述,有熟练腹腔镜经验的医师团队可在保留左结肠动脉同时完成肠系膜下动脉至左结肠动脉的淋巴结清扫,既完成了中央组淋巴结的清扫,又可保证吻合口良好的血液供应,有利于直肠癌患者术后的快速康复。理论上术后局部复发率和生存期应无差别,但由于缺少大规模随机对照研究试验,且患者随访时间不长、手术技巧也有待进一步提高,故其远期疗效尚需进一步探究。
| [1] | Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012[J]. Int J Cancer, 2015, 136(5): E359-86. DOI: 10.1002/ijc.29210. |
| [2] | 王自强, 周总光. 不断提高我国腹腔镜直肠癌根治规范化水平[J]. 中华普外科手术学杂志(电子版), 2015, 9(3): 157-60. |
| [3] | 吴孟超, 吴在德, 黄家驷. 外科学[M]. 北京: 人民卫生出版社, 2008: 1644-5. |
| [4] | 臧潞, 马君俊, 郑民华. 直肠癌根治术中保留左结肠动脉对吻合口瘘及手术时间的影响[J]. 中华胃肠外科杂志, 2016, 19(4): 386-7. |
| [5] | 沈荐, 李敏哲, 杜燕夫, 等. 腹腔镜直肠癌前切除术中保留左结肠动脉与否的临床对照研究[J]. 中国微创外科杂志, 2014, 20(1): 22-4, 28. |
| [6] | 周灿, 陈武科, 何建军, 等. 国内直肠癌术后吻合口瘘危险因素的Meta分析[J]. 西安交通大学学报:医学版, 2010, 31(1): 115-21. |
| [7] | 王勇. 直肠癌前切除术患者术前营养情况与术后吻合口瘘的相关性研究[J]. 河北中医, 2015, 37(9): 1435-8. |
| [8] | Aytac E, Lavery IC, Kalady MF, et al. Impact of obesity on operation performed, complications, and long-term outcomes in terms of restoration of intestinal continuity for patients with mid and low rectal cancer[J]. Dis Colon Rectum, 2013, 56(6): 689-97. DOI: 10.1097/DCR.0b013e3182880ffa. |
| [9] | Sebag-Montefiore D, Stephens RJ, Steele R, et al. Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial[J]. Lancet, 2009, 373(9666): 811-20. DOI: 10.1016/S0140-6736(09)60484-0. |
| [10] | Slim K, Vicaut E, Launay-Savary MV, et al. Updated systematic review and meta-analysis of randomized clinical trials on the role of mechanical bowel preparation before colorectal surgery[J]. Ann Surg, 2009, 249(2): 203-9. DOI: 10.1097/SLA.0b013e318193425a. |
| [11] | JiangZ. The strategies of of treatment in middle and low rectal cancer[J]. 中华结直肠疾病电子杂志, 2015, 4(5): 487-9. |
| [12] | Kang L, Wang J. Present conditions and problems of transanal total mesorectal excision in rectal cancer[J]. Zhonghua Wei Chang Wai Ke Za Zhi, 2015, 18(5): 413-6. |
| [13] | Yoon WH, Kim HJ, Kim CH, et al. Oncologic impact of pathologic response on clinical outcome after preoperative chemoradiotherapy in locally advanced rectal cancer[J]. Ann Surg Treat Res, 2015, 88(1): 15-20. DOI: 10.4174/astr.2015.88.1.15. |
| [14] | Junginger T, Goenner U, Hitzler M, et al. Long-term oncological outcome after transanal endocopic microsurgery for rectal carcinoma[J]. Dis Colon Rectum, 2016, 59(5): 8-15. |
| [15] | Yun JA, Huh JW, Kim HC, et al. Local recurrence after curative resection for rectal carcinoma: The role of surgical resection[J]. Medicine (Baltimore), 2016, 95(27): e3942. DOI: 10.1097/MD.0000000000003942. |
| [16] | Taflampas P CM, Tsiftsis D EA. Anastomotic leakage after low anterior resection for rectal cancer: facts, obscurity, and fiction[J]. Surg Today, 2009, 39(3): 183-8. DOI: 10.1007/s00595-008-3835-2. |
| [17] | Makela J KH, Laitinen S EA. Risk factors for anastomotic leakage after left-sided colorectal resection with rectal anastomosis[J]. Dis Colon Rectum, 2003, 46(5): 653-60. DOI: 10.1007/s10350-004-6627-9. |
| [18] | Nesbakken A, Nygaard K, Lunde OC. Outcome and late functional results after anastomotic leakage following mesorectal excision for rectal cancer[J]. Br J Surg, 2001, 88(3): 400-4. DOI: 10.1046/j.1365-2168.2001.01719.x. |
| [19] | Trencheva K, Morrissey KP, Wells M, et al. Identifying important predictors for anastomotic leak after colon and rectal resection: prospective study on 616 patients, Ann[J]. Surg, 2013, 257(9): 108-13. |
| [20] | den Dulk M, Marijnen CA, Collette L, et al. Multicentre analysis of oncological and survival outcomes following anastomotic leakage after rectal cancer surgery[J]. Br J Surg, 2009, 96(9): 1066-75. DOI: 10.1002/bjs.v96:9. |
| [21] | Hida J, Okuno K. High ligation of the inferior mesenteric artery in rectal cancer surgery[J]. Surg Today, 2013, 43(1): 8-19. DOI: 10.1007/s00595-012-0359-6. |
| [22] | Buunen M, Lange MM, Ditzel M, et al. Level of arterial ligation in total mesorectal excision (TME): an anatomical study[J]. Colorectal Dis, 2009, 24(11): 1317-20. DOI: 10.1007/s00384-009-0761-8. |
| [23] | Hinoi T, Okajima M, Shimomura M, et al. Effect of left colonic artery preservation on anastomotic leakage in laparoscopic anterior resection for middle and low rectal cancer[J]. World J Surg, 2013, 37(12): 2935-43. DOI: 10.1007/s00268-013-2194-3. |
| [24] | Huh JW, Kim YJ, Kim HR. Distribution of lymph node metastases is an Independent predictor of survival for sigmoid colon and rectal cancer[J]. Ann Surg, 2012, 255(1): 70-8. DOI: 10.1097/SLA.0b013e31823785f6. |
| [25] | Kim JC, Lee KH, Yu CS, et al. The clinicopathological significance of inferior mesenteric lymph node metastasis in colorectal cancer[J]. Eur J Surg Oncol, 2004, 30(3): 271-9. DOI: 10.1016/j.ejso.2003.12.002. |
 2017, Vol. 9
2017, Vol. 9

