系统性红斑狼疮(SLE)是一种多系统、多脏器受累的自身免疫性疾病,多发生于育龄期女性.过去,SLE患者妊娠后出现多种并发症,对孕妇及胎儿均造成严重伤害,通常这些患者不建议生育.随着SLE治疗的进步,多数患者病情可得到长期良好的控制,这些患者妊娠问题也成为关注的重点.近几年,国外学者对SLE患者妊娠期间病情变化、母体及胎儿的影响进行了一些探讨,发现尽管SLE患者妊娠后母婴结局较过去有所改善[1-3],但仍有23.3%~33%患者妊娠期间SLE复发[4-6],16.6%~30%狼疮肾炎复发[4, 7-8],同普通妇女妊娠相比,SLE患者具有更高的死亡率、子痫前期发生率及胎儿早产率[9-10],且妊娠期间药物治疗及处理意见并不统一.在国内,类似研究开展不多,样本量少,因此,本研究拟调查我院过去10年SLE患者的妊娠转归,并分析不良妊娠结局的危险因素,为进一步改善SLE患者妊娠结局提供临床经验和资料.现报导如下.
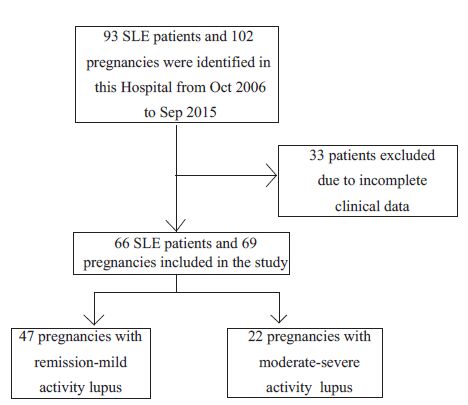
1 资料和方法 1.1 研究对象2006 年10 月~2015 年09 月在我院住院的SLE妊娠患者.期间共有93 位SLE患者的102 次妊娠入选,33例因资料不全剔除,最后66位SLE住院患者的69次妊娠临床资料纳入研究(图 1),包括患者一般情况、孕产史、SLE病史、妊娠期间临床表现、实验室检查结果、妊娠期间用药情况、妊娠结局、母婴并发症等.
|
图 1 患者流程图 Figure 1 Flow chart of patient enrollment |
根据1997年美国风湿病学会修订的SLE诊断标准,所有患者均符合诊断标准.采用多伦多大学的SLE疾病活动指数(SLEDAI)作为判断SLE 活动性的标准[11].SLEDAI评分<5 分为SLE无活动;SLEDAI评分≥5 分为SLE活动,其中5~9分为轻度活动;10~14分为中度活动;≥15 分为重度活动.活动性狼疮肾炎为持续性尿蛋白(>0.5 g/d 或+++)或管型尿(红细胞、颗粒或混合管型),伴或不伴血肌酐升高.肾功能不全为血肌酐≥123.76 μmol/L,或短时间(48 h)内血肌酐绝对值增加≥26.4 μmol/L或增加50%,或者尿量<0.5 mL/(kg·h).高血压为妊娠期间连续3次测得收缩压≥140 mmHg和/或舒张压≥90 mmHg,或服用抗高血压药物.不良妊娠结局为胎儿丢失(包括流产、死胎)、早产、低出生体质量儿或胎儿宫内生长迟缓(IUGR).
1.3 研究方法采用回顾性分析方法,统计SLE患者的临床特征.并根据SLE 患者妊娠期间最高SLEDAI 评分分为疾病缓解-轻度活动组(SLEDAI≤9 分)和中-重度活动组(SLEDAI>9分),比较两组胎儿结局、母婴并发症,分析不良妊娠结局危险因素.
1.4 统计学处理采用SPSS 19.0统计学软件对实验数据进行统计学处理.计算各统计量的均数、标准差、频率、中位数,计量资料采用t检验,计数资料采用卡方检验或Fisher确切概率法,危险因素采用Logistic回归分析,α入=0.05,α出=0.01.以P<0.05为差异有统计学意义.
2 结果 2.1 临床特征共纳入66位SLE患者的69次妊娠,确诊SLE平均年龄为22.9±5.1 岁,确诊SLE后第1 次妊娠平均年龄26.4±3.9岁,妊娠时SLE平均病程为4.1±3.6年,妊娠期间因病情需要平均住院次数1.2±0.5 次/人,妊娠期间SLEDAI最高评分平均为6.8±7.4分,其中非活动组38例(55.1%),轻度活动组9例(13.0%),中度活动组9例(13.0%),重度活动组13 例(18.8%).妊娠结束时SLEDAI 评分平均为6.4±7.0 分.妊娠过程中45 例(65.2%)接受药物治疗,44例(63.8%)应用糖皮质激素,其中27例(39.1%)剂量<20 mg/d,17例(24.6%)剂量≥20 mg/d,其中,19例(27.5%)应用羟氯喹,2例(2.9%)应用硫唑嘌呤,2例(2.9%)应用环孢素,为疾病中-重度活动者,且均联合糖皮质激素、羟氯喹治疗.27 例(39.1%)既往合并狼疮肾炎,18例(26.1%)既往行肾穿刺活检术,妊娠期间15 例(21.7%)高血压,17 例(24.6%)血小板减少,补体C3平均值为0.82±0.36 g/L,血肌酐中位数为47.0(21.0~407.5)μmol/L.
2.2 胎儿结局及其并发症除去2例非计划生育及1例母亲尖锐湿疣选择人工流产外,余胎儿丢失共24例(34.8%),治疗性流产18例(26.1%),死胎3例(4.3%),自然流产2例(2.9%),母婴死亡1例(1.4%),胎儿丢失主要发生在孕中期,共17例(24.6%).69次妊娠共分娩新生儿42例(60.9%),平均出生体质量2640.5±672.0 g,平均妊娠周期37.0±2.6周,足月产27例(39.1%),低出生体质量儿15例(21.7%),早产15例(21.7%),IUGR 6例(8.7%),Apgar评分1 min≤7分者7例(10.1%).详见表 1.
| 表 1 SLE妊娠患者胎儿结局及其并发症 Table 1 Fetal outcomes and complications in SLE pregnancies |
之后,我们根据SLE活动指数,将患者分成缓解-轻度活动组(SLEDAI≤9分)和中-重度活动组(SLEDAI>9分),比较胎儿结局、活产婴儿并发症.如表 1所示:胎儿丢失率在中-重度活动组明显升高;而足月产、新生儿出生体质量明显降低.
2.3 孕妇并发症妊娠期间新发SLE患者15例(21.7%),9例(60%)合并狼疮肾炎,其中8 例(53.3%)发生在孕早期,7 例(46.7%)孕中期.高血压15例(21.7%),活动性狼疮肾炎26 例(37.7%),糖尿病7 例(10.1%),肺部感染7 例(10.1%),子痫前期或子痫7例(10.1%),肾功能不全10例(14.5%),HELLP综合征1 例(1.4%),孕妇死亡1 例(1.4%),该孕妇既往SLE多次复发,且因孕期病情加重曾于孕晚期治疗性流产1次,此次妊娠期间自行停药,孕13周时出现病情加重,孕16周因心力衰竭死亡.
中-重度活动组SLE新发、高血压、活动性狼疮肾炎、肺部感染、肾功能不全明显多于疾病缓解-轻度活动组,差异有统计学意义(P<0.05,表 2).
| 表 2 SLE妊娠患者母亲并发症 Table 2 Maternal complications in SLE pregnancies |
本研究发现胎儿丢失、早产、低出生体质量儿、IUGR发生率较高,由于病例数较少,我们将这些结局统称为不良妊娠结局,并分析了其相关危险性.利用单因素Logistic回归分析,可知高血压、活动性狼疮肾炎、血小板减少症为不良妊娠结局的危险因素,孕期药物治疗是不良妊娠结局的保护性因素,差异有统计学意义(P<0.05).将以上变量行多因素Logistic回归分析,结果显示活动性狼疮肾炎(OR=6.10,P=0.014)为不良妊娠结局的独立危险因素(表 3).
| 表 3 不良妊娠结局危险因素分析 Table 3 Risk factors related to adverse pregnancy outcomes |
本临床研究回顾性分析了SLE妊娠患者的病例资料,发现69次妊娠共分娩出新生儿42例(60.9%),15例(21.7%)早产;母亲中15 例(21.7%)出现高血压,26 例(37.7%)出现活动性狼疮肾炎,因此,SLE患者妊娠仍存在一定风险.
国外文献[6, 12-13]报道的胎儿丢失率差异较大,在4.6%~34.0%之间,可能与入选的病例病情不同有关,国内回顾性研究[14-15]显示胎儿丢失率为28.6%~31%,本研究胎儿丢失率为34.8%.此外,国内外文献报道早产率为20.8%~31%[9, 13-14],低出生体质量儿14.9%~32%[14-16],IUGR5.6%~18.5%[9, 12, 14],本研究中早产率为21.7%,低出生体质量儿为21.7%,IUGR为8.7%,妊娠合并SLE患者胎儿结局并不理想.我们将胎儿丢失、早产、低出生体质量儿、IUGR统称为不良妊娠结局,发现高血压、活动性狼疮肾炎、血小板减少症是不良妊娠结局的危险因素.Buyon等[17]近期一项队列研究证明狼疮抗凝物、抗高血压药物、血小板减少症、疾病活动度高均预示不良妊娠结局.Moroni等[18]发现蛋白尿、活动性狼疮肾炎患者早产率明显升高;Wagner等[19]也发现活动性狼疮肾炎妊娠患者早产、胎儿丢失明显高于非活动性狼疮肾炎患者,且肾脏未受累的SLE患者与缓解期狼疮肾炎相比,早产、胎儿丢失无明显差异,我们的研究也证实了活动性狼疮肾炎是不良妊娠结局的独立危险因素,所以,SLE患者妊娠期间应密切监测血常规、血压,尤其是尿常规情况.
SLE患者妊娠期间疾病活动风险增加2~3倍[20],且妊娠期间SLE活动增加母亲并发症的风险[21-22],我们的研究中约一半(49%)的患者妊娠期间出现狼疮活动.有文献报导SLE患者妊娠期间高血压发生率为15%~23.6%[1, 8, 23],本研究中21.7%的患者出现高血压,且病情中-重度活动组高血压发生率明显高于缓解-轻度活动组,这提示控制SLE活动,有利于降低高血压发生.此外,子痫前期/子痫也是母亲主要并发症之一,国内外研究报导子痫前期/子痫的发生率为20%~28.4%[23-25],与SLE活动有关,本研究中子痫前期/子痫的患者共7 例(10.1%),低于上述研究,发生率与病情活动无明显差异,可能与本研究样本量少有关.另外,本研究有1位妊娠妇女孕16周因心力衰竭死亡,该患者既往SLE多次复发,有不良孕产史,且妊娠期间自行停药,孕13周出现狼疮活动.Clowse等[9]报导SLE妊娠妇女死亡率为0.32%,是非SLE妊娠妇女的20 倍,可见,妊娠合并SLE妇女死亡率明显高于普通人群.
有关妊娠新发SLE的临床特征及妊娠结局的报道很少.少量研究提示妊娠初发SLE患者63.1%~75%孕早期及孕中期发病,65.9%~68.8%的患者合并狼疮性肾炎,妊娠初发SLE患者肾脏、血液系统更易受累,且易合并间质性肺炎和血栓性血小板减少性紫癜[21, 26-28].本研究中,妊娠初发SLE15例,均在孕早期及孕中期发病,其中9例(60%)合并狼疮肾炎,胎儿丢失11例(73.3%),3例(20%)早产,1例(6.7%)足月产,妊娠新发SLE患者的妊娠结局较差.目前妊娠新发SLE的治疗及处理尚无明确报导,因此,我们还需进一步研究妊娠新发SLE,提高此类患者的妊娠结局.
本临床研究属于回顾性研究,部分患者因资料不完整而被剔除,导致样本量偏少,不能进行分层分析;另一方面,本研究只选择了在我院结束妊娠的SLE住院患者,病情较重,不能很好的反映所有SLE患者妊娠情况,后续研究需考虑纳入门诊或多个医疗中心的SLE妊娠患者.
综上所述,大部分SLE妊娠患者仍然可以成功分娩,但是母亲并发症及不良妊娠结局发生率仍有待控制,所以,建议SLE患者应在病情稳定及多专科医生共同指导下受孕,并定期随访、合理用药,控制狼疮活动,从而获得良好的妊娠结局,减少母婴并发症.
| [1] | Yan Yuen S, Krizova A, OuimetJM, et al. Pregnancy outcome in systemic lupus erythematosus (SLE) is improving: Results from a case control study and literature review[J]. Open Rheumatol J, 2008, 2 (1): 89-98. |
| [2] | Clark A, Spitzer A, Laskin A. Decrease in pregnancy loss rates in patients with systemic lupus erythematosus over a 40-year period[J]. J Rheumatol, 2005, 32 (9): 1709-12. |
| [3] | Wallenius M, Salvesen KA, DaltveitAK, et al. Secular trends of pregnancies in women with inflammatory connective tissue disease[J]. ActaObstetGynecolScand, 2015, 94 (11): 1195-202. |
| [4] | Cervera R, Font J, Carmona F, et al. Pregnancy outcome in systemic lupus erythematosus: good news for the new millennium[J]. Autoimmun Rev, 2002, 1 (6): 354-9. DOI: 10.1016/S1568-9972(02)00082-4. |
| [5] | Carvalheiras G, Vita P, Marta S, et al. Pregnancy and systemic lupus erythematosus: review of clinical features and outcome of 51 pregnancies at a single institution[J]. Clin Rev Allergy Immunol, 2010, 38 (2/3): 302-6. |
| [6] | Cortés-Hernández J, Ordi-Ros J, Paredes F, et al. Clinical predictors of fetal and maternal outcome in systemic lupus erythematosus: a prospective study of 103 pregnancies[J]. Rheumatology (Oxford), 2002, 41 (6): 643-50. DOI: 10.1093/rheumatology/41.6.643. |
| [7] | Moroni G, Doria A, Giglio E, et al. Maternal outcome in pregnant women with lupus nephritis. A prospective multicenter study[J]. J Autoimmun, 2016, 74 (8): 194-200. |
| [8] | Imbasciati E, Tincani A, Gregorini G, et al. Pregnancy in women with pre-existing lupus nephritis: predictors of fetal and maternal outcome[J]. Nephrol Dial Transplant, 2009, 24 (2): 519-25. |
| [9] | Clowse E, Jamison M, Myers E, et al. A National study of the complications of lupus in pregnancy[J]. Am J ObstetGynecol, 2008, 199 (2): 127. |
| [10] | Molokhia M, Maconochie N, Patrick L, et al. Cross-sectional analysis of adverse outcomes in 1,029 pregnancies of Afro-Caribbean women in Trinidad with and without systemic lupus erythematosus[J]. Arthritis Res Ther, 2007, 9 (6): R124. DOI: 10.1186/ar2332. |
| [11] | Bombardier C, Gladman DD, Urowitz MB, et al. Derivation of the SLEDAI.A disease activity index for lupus patients. The Committee on Prognosis Studies in SLE[J]. Arthritis Rheum, 1992, 35 (6): 630-40. DOI: 10.1002/(ISSN)1529-0131. |
| [12] | Madazli R, Yuksel A, Oncul M, et al. Obstetric outcomes and prognostic factors of lupus pregnancies[J]. Arch GynecolObstet, 2014, 289 (1): 49-53. |
| [13] | Clowse E, Magder S, Witter Frank, et al. The impact of increased lupus activity on obstetric outcomes[J]. Arthritis Rheum, 2005, 52 (2): 514-21. DOI: 10.1002/(ISSN)1529-0131. |
| [14] | 高彦彦, 叶华, 郭衍秋, 等. 系统性红斑狼疮合并妊娠49例分析[J]. 中 华风湿病学杂志, 2012, 16 (8): 553-6. |
| [15] | 张红卫, 陈国强, 陈蔚瑜, 等. 系统性红斑狼疮对妊娠结局影响的病例 对照研究[J]. 中华风湿病学杂志, 2006, 10 (5): 293-6. |
| [16] | Chen Y, Chen H, Lin C, et al. Increased risk of adverse pregnancy outcomes for hospitalisation of women with lupus during pregnancy: a nationwide population-based study[J]. ClinExpRheumatol, 2010, 28 (1): 49-55. |
| [17] | Buyon JP, Kim M, Guerra MM, et al. Predictors of Pregnancy Outcomes in Patients With Lupus: A Cohort Study[J]. Ann Intern Med, 2015, 163 (3): 153-163. DOI: 10.7326/M14-2235. |
| [18] | Moroni G, Doria A, Giglio E, et al. Fetal outcome and recommendations of pregnancies in lupus nephritis in the 21st century[J]. J Autoimmun, 2016, 74 (10): 6-12. |
| [19] | Wagner SJ, Craici I, Reed D, et al. Maternal and foetal outcomes in pregnant patients with active lupus nephritis[J]. Lupus, 2009, 18 (4): 342-7. DOI: 10.1177/0961203308097575. |
| [20] | Stojan G, Baer AN. Flares of systemic lupus erythematosus during pregnancy and the puerperium: prevention, diagnosis and management[J]. Expert Rev ClinImmunol, 2012, 8 (5): 439-53. DOI: 10.1586/eci.12.36. |
| [21] | Yang H, Liu H, Xu D, et al. Pregnancy-related systemic lupus erythematosus: clinical features, outcome and risk factors of disease flares--a case control study[J]. PLoS One, 2014, 9 (8): e104375. DOI: 10.1371/journal.pone.0104375. |
| [22] | Yang J, Chen Y, Chang H, et al. Pregnancy outcome of systemic lupus erythematosus in relation to lupus activity before and during pregnancy[J]. J Chin Med Assoc, 2015, 78 (4): 235-40. DOI: 10.1016/j.jcma.2014.11.008. |
| [23] | Kwok LW, Tam LS, Zhu T, et al. Predictors of maternal and fetal outcomes in pregnancies of patients with systemic lupus erythematosus[J]. Lupus, 2011, 20 (8): 829-36. DOI: 10.1177/0961203310397967. |
| [24] | Liu J, Zhao Y, Song Y, et al. Pregnancy in women with systemic lupus erythematosus: a retrospective study of 111 pregnancies in Chinese women[J]. J Matern Fetal Neonatal Med, 2012, 25 (3): 261-6. DOI: 10.3109/14767058.2011.572310. |
| [25] | 宋亦军, 刘冬舟, 刘俊涛, 等. 妊娠合并系统性红斑狼疮94例临床分析[J]. 中华内科杂志, 2008, 47 (12): 1008-11. |
| [26] | Zhao C, Zhao J, Huang Y, et al. New-onset systemic lupus erythematosus during pregnancy[J]. ClinRheumatol, 2013, 32 (6): 815-22. |
| [27] | Miyamoto T, Hoshino T, Hayashi N, et al. Preeclampsia as a manifestation of New-Onset systemic lupus erythematosus during pregnancy: a case-based literature review[J]. AJP Rep, 2016, 6 (1): e62-7. |
| [28] | Ku M, Guo S, Shang W, et al. Pregnancy outcomes in Chinese patients with systemic lupus erythematosus (SLE): A retrospective study of 109 pregnancies[J]. PLoS One, 2016, 11 (7): e0159364. DOI: 10.1371/journal.pone.0159364. |
 2016, Vol. 36
2016, Vol. 36

