结直肠癌是常见的恶性肿瘤,我国结直肠癌的发病率在恶性肿瘤中占第3位。对于已明确诊断的结直肠癌病人,对预后做出准确评估具有重要意义。目前临床上主要采用美国癌症联合会(AJCC)的TNM分期系统[1]对结直肠癌的预后进行评估,研究发现,这种基于肿瘤解剖学范围的分期方法可能夸大了肿瘤的生物学潜能及总死亡和复发风险[2],近年来一些与肿瘤侵袭性相关的非解剖学的预测因子被加入TNM分期系统,以增加评估的准确性。大量早期同近期的研究都证实治疗前癌胚抗原(CEA)水平可作为独立的危险因素预测结直肠癌的不良预后[3-8],而AJCC早在15年前就拟将治疗前血清CEA水平(C stage)加入结直肠癌TNM分期系统[9],但缺乏长期生存的数据支持,直到近期来自美国SEER 数据库的证据证实在相同TNM 分期下,高Cstage病人预后差[10],这些研究结果都证实了CEA水平对判断病人的预后的价值。因此,为获得我国结直肠癌病人的相关信息,我们设计此试验,拟对我院收治的TNMⅠ~Ⅲ期结直肠癌病人的长期生存数据进行回顾性分析,目的是通过在TNM分期系统中加入治疗前癌胚抗原水平后重新评估Ⅰ~Ⅲ期结直肠癌病人的预后。
1 研究对象 1.1 一般资料回顾性分析广州市第一人民医院2003年1月~2013年12月行手术治疗的结直肠癌病人的临床病例资料,病人病历及随访信息完整。病人入选标准:年龄>18岁;术后病理证实的原发性结、直肠腺癌及粘液腺癌;完成肿瘤根治性切除手术;术后对病人行以5-FU为基础的方案辅助化疗。根据治疗前CEA水平将病人分成两组,即升高组(CEA≥5 ng/mL)和未升高组(CEA<5 ng/mL)。
1.2 观察指标年龄、性别、肿瘤位置、大小、分化程度、TNM 分期及术前CEA 值。两组病人复发率、复发类型、总死亡率、累计总生存率及累计无瘤生存率。
1.3 随访及统计学方法末次随访定为2014年8月,总生存时间定义为手术日起至末次随访日或死亡所经历的时间。无瘤生存时间定义为手术日起至肿瘤复发所经历的时间,以月为单位。复发需有明确的影像学或病理学证据支持。计量资料用独立样本t检验或Mann-Whitney U检验,计数资料采用χ2检验或Fisher 确切概率法,用Kaplan-Meier 法比较两组病人的累积总生存率、无瘤生存率,用log-rank 法检验,COX模型分析影响术后病人生存及复发的危险因素,P值取双尾,P<0.05 差异具有统计学意义,所有计算采用spss17.0软件包进行。
2 结果 2.1 两组病人临床、病理数据的比较查阅病历,提取有完整临床及随访信息的病人共393例,其中升高组136例,未升高组257例,两组病人的肿瘤大小、分化程度、淋巴结转移的差异有统计学意义(P<0.05),两组病人年龄、性别、肿瘤位置、病理类型、浸润深度、TNM分期差异无统计学意义(表 1)。
| 表 1 两组病人临床、病理数据的比较 Table 1 Comparison of clinicopathologic data between the two groups |
以病人的性别、年龄、肿瘤病理类型、肿瘤分化程度、肿瘤大小、肿瘤浸润深度、淋巴结转移及术前CEA水平为自变量进行COX 回归分析,结果显示,中或低的肿瘤分化程度,有淋巴结转移,年龄大于60岁及术前高CEA水平是影响病人术后病人生存的危险因素,详见表 2;而中或低的肿瘤分化程度、有淋巴结转移,肿瘤浸润肌层以上,年龄大于60岁及术前高CEA水平是影响病人术后病人复发的危险因素(表 3)。
| 表 2 影响结直肠癌术后生存的COX 模型 Table 2 Multivariate analysis of the patients' survival |
| 表 3 影响结直肠癌术后复发的COX 模型 Table 3 Multivariate analysis of tumor recurrence in the patients |
在随访期内,CEA升高组的死亡率及复发率均高于未升高组,差异有统计学意义(P<0.05,表 4)。
| 表 4 两组病人生存及复发的比较 Table 4 Comparison of survival and tumor recurrence between the two groups |
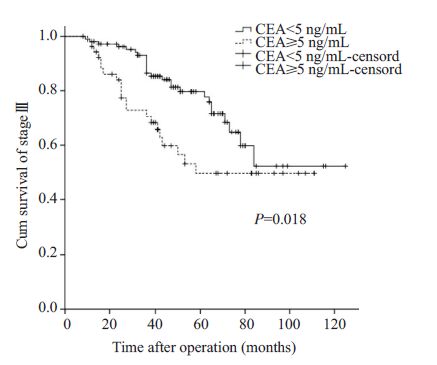
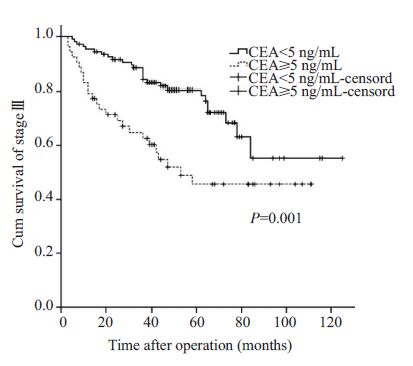
病生存率的比较升高组病人的累积总生存率(P=0.006)及累积无瘤生存率(P=0.000)明显低于未升高组病人,差异有统计学意义;TNMⅠ~Ⅱ期两组病人的累积总生存率及累积无瘤生存率差异无统计学意义;TNM Ⅲ期升高组病人的累积总生存率及累积无瘤生存率明显低于CEA 未升高组病人,差异有统计学意义(P<0.05,图 1、2)。
|
图 1 两组Ⅲ期病人累计总生存率比较 Figure 1 Comparison of overall survival between two groups of stage Ⅲ |
|
图 2 两组Ⅲ期病人累计无瘤生存率比较 Figure 2 Comparison of recurrence-free survival between stage III patients in the two groups |
本文目的旨在探讨治疗前癌胚抗原水平与TNMⅠ~Ⅲ期结直肠癌病人预后的关系。研究发现单一的TNM分期方法可能夸大了肿瘤的生物学潜能及总死亡和复发风险,因此,美国癌症联合会通过在TNM分期系统中加入一些肿瘤侵袭性相关的非解剖学的预测因子以增加评估的准确性。鉴于大量研究证实治疗前癌胚抗原水平(C stage)可作为独立的危险因素预测结直肠癌的不良预后[11-14],因此,根据AJCC结直肠癌组的关于C stage的分类的指导意见将我院收治的393例结直肠癌病人分为未升高组(CEA<5 ng/mL)及升高组(CEA≥5 ng/mL),其中未升高组136例,升高组257例。
通过对我院病人临床数据回顾性分析发现,升高组病人的肿瘤直径大,分化程度低、常见淋巴结转移,两组间差异有统计学意义(P<0.05)。Huh等[15]研究发现高水平组(CEA≥5 ng/mL)结直肠癌病人肿瘤直径大、T和N分期较晚且阳性的周围神经侵犯,这些指标同CEA水平一样都可以判断结直肠癌病人的不良预后。因此CEA水平越高,结直肠癌病人肿瘤的恶性程度越高,临床分期越晚[16],死亡率越高[17]。另外,本研究COX回归分析的结果也证实,术前高CEA水平是影响病人术后生存及复发的危险因素,升高组病人死亡及复发风险分别提高1.59及1.89倍。
本研究比较了两组病人的总死亡率及复发率,在随访期内,升高组病人总死亡率(28.7%)高于未升高组病人(19.8%),且升高组病人复发率(32.4%)高于未升高组病人(19.1%),差异均有统计学意义(P<0.05)。国外的研究也得出同样结论,Huh等[18]回顾分析了474例病人的生存数据,结果显示血清CEA正常组(CEA<5 ng/mL)患者的五年生存率为81.%,而升高组患者的生存率明显降低,仅为69.9%。Takagawa等[19]对638例病人回顾性分析发现CEA升高组病人(CEA>10 ng/mL)的术后复发率高达41.3%,而CEA 未升高组的复发率仅为15.4%。由此可见,CEA水平的升高可预示肿瘤病人的高死亡率及复发率[20-21]。
本文进一步通过Kaplan-Meier 法比较两组病人的累积总生存率、无瘤生存率,结果发现,CEA升高组病人的累积总生存率(P=0.006)及累积无瘤生存率(P=0.000)明显低于CEA未升高组病人,差异有统计学意义。对病人分期后再对上述指标比较发现,在Ⅲ期结直肠癌病人中,CEA 升高组病人的累积总生存率(P=0.018)及累积无瘤生存率(P=0.001)明显低于CEA未升高组病人,差异有统计学意义。Wuxiao等[22]的研究发现,在Ⅲ期结直肠癌病人中CEA水平的升高提示结直肠癌病人的不良预后。Lin等[23]对363例Ⅲa期结直肠癌病人的数据进行回顾性分析发现,CEA水平正常组病人的5年总生存率明显高于CEA水平升高组。因此,对Ⅲ期结直肠癌病人,联合C stage可更准确的判断病人的预后。
综上所述,在TNM分期系统中加入C stage后可产生新的生存及复发数据,指导临床医生更准确的判断病人的预后。
| [1] |
Edge SB, Byrd DR, Compton CC, et al.
AJCC cancer staging handbook. 7thed. NewYork: Springer[M]. 2010 .
( 0) 0)
|
| [2] |
Sobin LH. TNM: evolution and relation to other prognostic factors[J].
Semin Surg Oncol,2003, 21 (1) : 3-7.
DOI: 10.1002/(ISSN)1098-2388. ( 0) 0)
|
| [3] |
Lee JH, Kim SH, Jang HS, et al. Preoperative elevation of carcinoembryonic antigen predicts poor tumor response and frequent distant recurrence for patients with rectal cancer who receive preoperative chemoradiotherapy and total mesorectal excision: a multi-institutional analysis in an[J].
Int J Colorectal Dis,2013, 28 (4) : 511-7.
DOI: 10.1007/s00384-012-1584-6. ( 0) 0)
|
| [4] |
Wiratkapun S, Kraemer M, Seow-Choen F, et al. High preoperative serum carcinoembryonic antigen predicts metastatic recurrence in potentially curative colonic cancer: results of a five-year study[J].
Dis Colon Rectum,2001, 44 (2) : 231-5.
DOI: 10.1007/BF02234298. ( 0) 0)
|
| [5] |
Canbay E, Ishibashi H, Sako S, et al. Preoperative carcinoembryonic antigen level predicts prognosis in patients with pseudomyxoma peritonei treated with cytoreductive surgery and hyperthermic intraperitoneal chemotherapy[J].
World J Surg,2013, 37 (6) : 1271-6.
DOI: 10.1007/s00268-013-1988-7. ( 0) 0)
|
| [6] |
Park YJ, Park KJ, Park JG, et al. Prognostic factors in 2230 Korean colorectal cancer patients: analysis of consecutively operated cases[J].
World J Surg,1999, 23 (7) : 721-6.
DOI: 10.1007/PL00012376. ( 0) 0)
|
| [7] |
Pakdel A, Malekzadeh M, Naghibalhossaini F. The association between preoperative serum CEA concentrations and synchronous liver metastasis in colorectal cancer patients[J].
Cancer Biomark,2016, 16 (2) : 245-52.
DOI: 10.3233/CBM-150561. ( 0) 0)
|
| [8] |
Tsai HL, Huang CW, Chen CW, et al. Survival in resected stage II colorectal cancer is dependent on tumor depth, vascular invasion, postoperative CEA level, and the number of examined lymph nodes[J].
World J Surg,2016, 40 (4) : 1002-9.
DOI: 10.1007/s00268-015-3331-y. ( 0) 0)
|
| [9] |
Compton C, Fenoglio-Preiser CM, Pettigrew N, et al. American joint committee on cancer prognostic factors consensus conference: colorectal working group[J].
Cancer,2000, 88 (7) : 1739-57.
DOI: 10.1002/(ISSN)1097-0142. ( 0) 0)
|
| [10] |
Thirunavukarasu P, Talati C, Munjal S, et al. Effect of incorporation of pretreatment serum carcinoembryonic antigen levels into AJCC staging for colon cancer on 5-Year survival[J].
JAMA Surg,2015, 150 (8) : 747-55.
DOI: 10.1001/jamasurg.2015.0871. ( 0) 0)
|
| [11] |
Lucha PA, Rosen L, Olenwine JA, et al. Value of carcinoembryonic antigen monitoring in curative surgery for recurrent colorectal carcinoma[J].
Dis Colon Rectum,1997, 40 (2) : 145-9.
DOI: 10.1007/BF02054978. ( 0) 0)
|
| [12] |
Tsai PL, Su WJ, Leung WH, et al. Neutrophil-lymphocyte ratio and CEA level as prognostic and predictive factors in colorectal cancer: A systematic review and meta-analysis[J].
J Cancer Res Ther,2016, 12 (2) : 582-9.
DOI: 10.4103/0973-1482.144356. ( 0) 0)
|
| [13] |
Tampellini M, Ottone A, Alabiso I, et al. The prognostic role of baseline CEA and CA 19-9 values and their time-dependent variations in advanced colorectal cancer patients submitted to first-line therapy[J].
Tumour Biol,2015, 36 (3) : 1519-27.
DOI: 10.1007/s13277-014-2693-3. ( 0) 0)
|
| [14] |
Jain P, Mondal SK, Sinha SK, et al. Diagnostic and prognostic significance of different mucin expression, preoperative CEA, and CA-125 in colorectal carcinoma: A clinicopathological study[J].
J Nat Sci Biol Med,2014, 5 (2) : 404-8.
DOI: 10.4103/0976-9668.136207. ( 0) 0)
|
| [15] |
Huh JW, Kim CH, Lim SW, et al. Factors predicting long-term survival in colorectal cancer patients with a normal preoperative serum level of carcinoembryonic antigen[J].
J Cancer Res Clin Oncol,2013, 139 (9) : 1449-55.
DOI: 10.1007/s00432-013-1459-4. ( 0) 0)
|
| [16] |
Vukobrat-Bijedic Z, Husic-Selimovic A, Sofic A, et al. Cancer antigens (CEA and CA 19-9) as markers of advanced stage of colorectal carcinoma[J].
Med Arch,2013, 67 (6) : 397-401.
DOI: 10.5455/medarh.. ( 0) 0)
|
| [17] |
Kirat HT, Ozturk E, Lavery IC, et al. The predictive value of preoperative carcinoembryonic antigen level in the prognosis of colon cancer[J].
Am J Surg,2012, 204 (4) : 447-52.
DOI: 10.1016/j.amjsurg.2011.11.007. ( 0) 0)
|
| [18] |
Huh JW, Oh BR, Kim HR, et al. Preoperative carcinoembryonic antigen level as an Independent prognostic factor in potentially curative colon cancer[J].
J Surg Oncol,2010, 101 (5) : 396-400.
( 0) 0)
|
| [19] |
Takagawa R, Fujii S, Ohta M, et al. Preoperative serum carcinoembryonic antigen level as a predictive factor of recurrence after curative resection of colorectal cancer[J].
Ann Surg Oncol,2008, 15 (12) : 3433-9.
DOI: 10.1245/s10434-008-0168-8. ( 0) 0)
|
| [20] |
Nicholson BD, Shinkins B, Pathiraja I, et al. Blood CEA levels for detecting recurrent colorectal cancer[J].
Cochrane Database Syst Rev,2015, 10 (12) : CD011134.
( 0) 0)
|
| [21] |
Dawood S, Sirohi B, Shrikhande SV, et al. Potential prognostic impact of baseline CEA level and surgery of primary tumor among patients with synchronous stage IV colorectal cancer: a large population based study[J].
Indian J Surg Oncol,2015, 6 (3) : 198-206.
DOI: 10.1007/s13193-015-0419-7. ( 0) 0)
|
| [22] |
Wuxiao ZJ, Zhou HY, Wang KF, et al. A prognostic model to predict survival in stage III colon cancer patients based on histological grade, preoperative carcinoembryonic antigen level and the neutrophil lymphocyte ratio[J].
Asian Pac J Cancer Prev,2015, 16 (2) : 747-51.
DOI: 10.7314/APJCP.2015.16.2.747. ( 0) 0)
|
| [23] |
Lin BR, Lin YL, Lai HS, et al. Overall survival of stage III colon cancer with only one lymph node metastasis is independently predicted by preoperative carcinoembryonic antigen level and lymph node sampling status[J].
PLoS One,2015, 10 (9) : e0137053.
DOI: 10.1371/journal.pone.0137053. ( 0) 0)
|
 2016, Vol. 36
2016, Vol. 36
