3手术室,广东广州510515;
2南京医科大学附属淮安第一医院 心脏外科,江苏淮安223300
2Department of Heart Surgery, Huai'an First People's Hospital Affiliated to Nanjing Medical University, Huai'an 223300, China;
3Operating Room, Nanfang hospital, Southern Medical University, Guangzhou 510515, China
由于手术既可根治性切除肿瘤,又可改善患者生活质量,因此至今为止,外科仍然是食管癌的首选治疗方式[1]。食管癌能否手术切除很大程度上取决于病变的大小和侵犯的范围[2]。食管癌越长,手术难度越大,手术风险越高。《克氏外科学》第15版将病变长度为10~15 cm的食管癌定义为“巨块型食管癌”[3]。从前,巨块型食管癌难以切除,多数患者被迫选择放疗、化疗等姑息性疗法。因无法避免食管完全性梗阻、食管气管瘘、食管主动脉瘘等并发症的发生,患者最终痛苦地死亡[4]。现我们报道巨块型食管癌1例,肿瘤长度为18.3 cm直径为5.1 cm。经术式改良,病变被成功切除,并获得了良好疗效。
1 资料和方法 1.1 术前资料患者男性,53岁,嗜酒及咖啡20年,因“吞咽梗阻及吞咽痛1个月,饮水呛咳及声音嘶哑1周”前来就诊。上消化道造影提示18.3 cm的胸段食管癌(图1A)。胃镜提示距门齿22 cm处表面溃烂的占位性病变,病理诊断为食管鳞状细胞癌;纤维支气管镜提示气管膜部外压性狭窄,粘膜尚光滑;胸部增强CT+胸主动脉成像提示胸主动脉移位,与肿瘤组织界限模糊;PET-CT提示纵隔内巨大的高代谢灶,伴右下肺吸入性肺炎,但未见肿瘤远处转移(图1B)。临床肿瘤分期:局部晚期的食管鳞状细胞癌T3-4N2M0[5]。

|
图1 上消化道造影及PET-CT(术前) Fig.1 Results of postoperative esphagogram and PET-CT. A: Esphagogram revealing thoracic esophagus with a filling-defect measuring 18.3 cm in length; B: PET-CT showing a huge hyper-metabolic mass in the mediastinum with aspiration pneumonia in the right lower lung but no evidence of distant organ metastasis. |
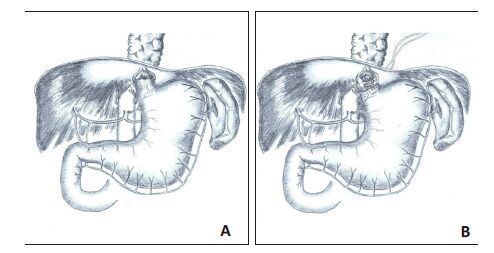
我们改良了常规的颈胸腹三切口食管癌切除食管胃颈部吻合术(吴氏法),步骤如下:(1)摆左侧卧位,取胸腔镜辅助小切口,行胸腔探查,明确病变范围及手术切除的可行性;(2)摆平卧位,取上腹正中切口,离断腹段食管,系食管吊带,并送入胸腔;(3)再次摆左侧卧位,牵拉食管吊带,以腹段食管为起点向上游离,将病变逐步分离并取出肿瘤;(4)再次摆平卧位,制作管状胃,取左颈前切口,行食管胃颈部吻合术(图2)。
|
图2 手术步骤二图解(吴氏法) Fig.2 Diagrams of step 2 of the operation (Wu's). A: Disconnecting the distal esophagus from the cardia via a median abdominal incision before esophagectomy; B: Pulling the distal esophagus along with the esophageal bed when dissociating the lesion. |
手术成功切除长18.3 cm巨块型食管癌(图3);术后第7天患者自行食用鸡腿110个,无碍;术后第10天嘱患者开始半流食;术后第20天患者顺利出院;术后随访半年,患者普食,食欲良好,未见术后并发症,未见肿瘤复发和播散的征象。

|
图3 肿瘤标本大体观 Fig.3 Gross observation of the resected tumor. |
患者系来自上海的音乐人,嗜酒及咖啡20年,每日饮酒及咖啡均超过500 mL。不良生活方式是患者罹患食管癌的主要诱因[6];患者短期内即出现吞咽困难、吞咽痛、饮水呛咳及声音嘶哑。此外待至入院后第3天,患者已无法继续饮水。这提示了食管梗阻和淋巴结压迫喉返神经的可能;患者气管膜部和胸主动脉已受肿瘤侵犯(但尚未侵入)。我们预测患者在近期内发生食管气管瘘或食管胸主动脉瘘的风险极高。
食管梗阻和瘘是局部晚期食管癌两个最严重的并发症。食管重度梗阻可导致患者频繁呕吐、水电解质紊乱和营养状况恶化[7];食管气管瘘可导致源源不断的消化液误吸、严重的吸入性肺炎、顽固的咳嗽咳痰,并最终发展为持续性高热、消耗性衰竭及感染性休克[8];而食管胸主动脉瘘可导致大出血和立即死亡[9]。该患者肿瘤巨大,生长迅速,已彻底堵塞食管并且即将突破主气管或胸主动脉。所以该手术应视为以解除梗阻和避免瘘的发生为目的的抢救性手术,应予立即手术。延长生存时间则为手术的第二目标。
一般认为长度超过5 cm的胸中上段食管癌宜选择颈胸腹三切口食管癌切除食管胃颈部吻合术。但对于这例巨块型食管癌,因病变已经占据了整个胸段食管,常规手术入路已无法便利地游离肿瘤。“先经腹离断腹段食管作为牵引”这一方法很好地解决了上述难题。然而,手术正真开始前的胸腔探查尤为重要,确定病变范围和切除可行性是决定手术是否继续的前提。
传统的颈胸腹三切口食管癌切除术一般要求在右侧胸壁第4肋间作一长约20 cm的前外侧切口[10]。而我们选择在右侧腋中线第5肋间作一长约8 cm的小切口作为主操作口。该主操作口可用于腔镜操作,也可在必要时做直视下操作。更为重要的是,本例巨块型食管癌明显外侵,气管和胸主动脉受压。而在胸骨角水平(即气管、食管、主动脉交汇处)的气管膜部和食管主动脉毗邻区最为薄弱,手术风险最高。8 cm恰好相当于一只手的宽度,我们在手的触摸下逐步分离气管膜部和主动脉,确保了气管和胸主动脉的完整性,最大程度地减少了手术的风险。这是手术成功的关键。此外,我们还在在右侧锁骨中线第2肋间和第5肋间各作一长约1 cm的小切口作为辅助操作口和观察口,以便于显露食管床和离断食管。
局部晚期食管癌多数已经外侵,可能无法从食管床满意剥除[11]。对于瘤床,可通过氩气刀局部烧灼、碘酒局部涂擦、45 ℃蒸馏水浸泡、顺铂溶液胸腔冲洗等手段作补救处理[12]。此外,胃排空障碍是食管癌切除术后常见的难治性并发症之一,我们在手术结束前预防性实施了纵切横缝式幽门肌层切开[13]。术后患者吞咽通畅,未发生排空障碍。
综上所述,局部晚期巨块型食管癌切除本质上是一种抢救性手术,其目的在于解除食管梗阻,消除发生食管气管瘘和食管主动脉瘘的风险。本例手术最终能取得较好的临床治疗效果,可归功于充分的术前评估、合适的手术时机和合理的手术设计。该手术方法的特点在于将游离肿瘤的起始点改在了腹段食管,因而在处理巨块型食管癌时有明显优势。据教育部科技查新报告(201436000Y010104),从检索到的国内外文献看,未见手术切除病变长度超过18.3 cm的巨块型食管癌的相关报道,本例为目前世界最长。
| [1] |
胡盛寿. 胸心外科学[M]. 北京: 人民卫生出版社, 2014: 107. ( 1) 1)
|
| [2] |
Pennathur A, Farkas A, Krasinskas AM, et al. Esophagectomy forT1 esophageal cancer: outcomes in 100 patients and implicationsfor endoscopic therapy[J]. Ann Thorac Surg, 2009, 87(4): 1048-54;discussion 1054-5. ( 1) 1)
|
| [3] |
王德炳. 克氏外科学[M]. 15版. 北京: 人民卫生出版社, 2002: 628. ( 1) 1)
|
| [4] |
Akl FM, Elsayed-Abd-Alkhalek S, Salah T. Palliative concurrentchemoradiotherapy in locally advanced and metastatic esophagealcancer patients with dysphagia[J]. Ann Palliat Med, 2013, 2(3):118-23. ( 1) 1)
|
| [5] |
吴阶平. 黄家驷外科学[M]. 7版. 北京: 人民卫生出版社, 2008: 2102. ( 1) 1)
|
| [6] |
Peng Q, Chen H, Huo JR. Alcohol consumption and correspondingfactors: A novel perspective on the risk factors of esophageal cancer[J]. Oncol Lett, 2016, 11(5): 3231-9. ( 1) 1)
|
| [7] |
Amdal CD, Jacobsen AB, Tausjø JE, et al. Palliative interventionsand prognosis in patients with advanced esophageal cancer[J]. DisEsophagus, 2011, 24(7): 502-9. ( 1) 1)
|
| [8] |
Adler L, Kabnick EM, Patel M, et al. Tracheoesophageal fistulasecondary to esophageal carcinoma presenting with aspirationpneumonia[J]. J Natl Med Assoc, 1985, 77(5): 401-3. ( 1) 1)
|
| [9] |
Lee RY, Flaherty L, Khushalani NI, et al. Aorto-esophageal fistula:a rare fatal case caused by esophageal malignancy[J]. J GastrointestOncol, 2010, 1(1): 64-5. ( 1) 1)
|
| [10] |
Domergue J, Saint-Aubert B, Rouanet P, et al. A new technique oftotal three-stage esophagectomy for carcinoma with a combinedright cervical and thoracic approach[J]. Surg Gynecol Obstet, 1989,169(6): 555-7. ( 1) 1)
|
| [11] |
Zheng B, Hu Y, Wang JY, et al. Associated factors and prognosis ofresidual cancer after esophagectomy for squamous cell carcinomaof the esophagus[J]. Chi J Gastrointest Surg, 2010, 13(1): 44-7. ( 1) 1)
|
| [12] |
Pi Z, Wang X, Liu G, et al. Experimental studies on hyperthermicdistilled water combining with saline and dextran for preventingintraperitoneal cancer recurrence due to neoplasm seeding[J]. JHunan Med Uni , 1999, 24(6): 525-8. ( 1) 1)
|
| [13] |
Khan OA, Manners J, Rengarajan A, et al. Does pyloroplastyfollowing esophagectomy improve early clinical outcomes[J]?Interact Cardiovasc Thorac Surg, 2007, 6(2): 247-50. ( 1) 1)
|
 2016, Vol. 36 Issue (7): 1018-1020 DOI:
2016, Vol. 36 Issue (7): 1018-1020 DOI: 
