Journal of Southern Medical University ›› 2025, Vol. 45 ›› Issue (3): 643-649.doi: 10.12122/j.issn.1673-4254.2025.03.22
Previous Articles Next Articles
Huali LI1( ), Ting SONG1, Jiawen LIU1, Yongbao LI2, Zhaojing JIANG4, Wen DOU4, Linghong ZHOU1,3(
), Ting SONG1, Jiawen LIU1, Yongbao LI2, Zhaojing JIANG4, Wen DOU4, Linghong ZHOU1,3( )
)
Received:2024-11-26
Online:2025-03-20
Published:2025-03-28
Contact:
Linghong ZHOU
E-mail:3178010219@i.smu.edu.cn;smart@smu.edu.cn
Supported by:Huali LI, Ting SONG, Jiawen LIU, Yongbao LI, Zhaojing JIANG, Wen DOU, Linghong ZHOU. Prognosis-guided optimization of intensity-modulated radiation therapy plans for lung cancer[J]. Journal of Southern Medical University, 2025, 45(3): 643-649.
Add to citation manager EndNote|Ris|BibTeX
URL: https://www.j-smu.com/EN/10.12122/j.issn.1673-4254.2025.03.22
| Model | Form | Dose metric | Clinical metric |
|---|---|---|---|
| LRF[ | Cox | Average BED for PTV | Age, Sex, Stage, Combined chemotherapy or not |
| RCT[ | Cox | Average EQD2 for heart | Previous cardiac history |
| RP≥2[ | Logistic | Average EQD2 for lungs | Age, Chemotherapy, Smoke |
Tab.1 The prognostic prediction model used to develop outcome-based objective
| Model | Form | Dose metric | Clinical metric |
|---|---|---|---|
| LRF[ | Cox | Average BED for PTV | Age, Sex, Stage, Combined chemotherapy or not |
| RCT[ | Cox | Average EQD2 for heart | Previous cardiac history |
| RP≥2[ | Logistic | Average EQD2 for lungs | Age, Chemotherapy, Smoke |
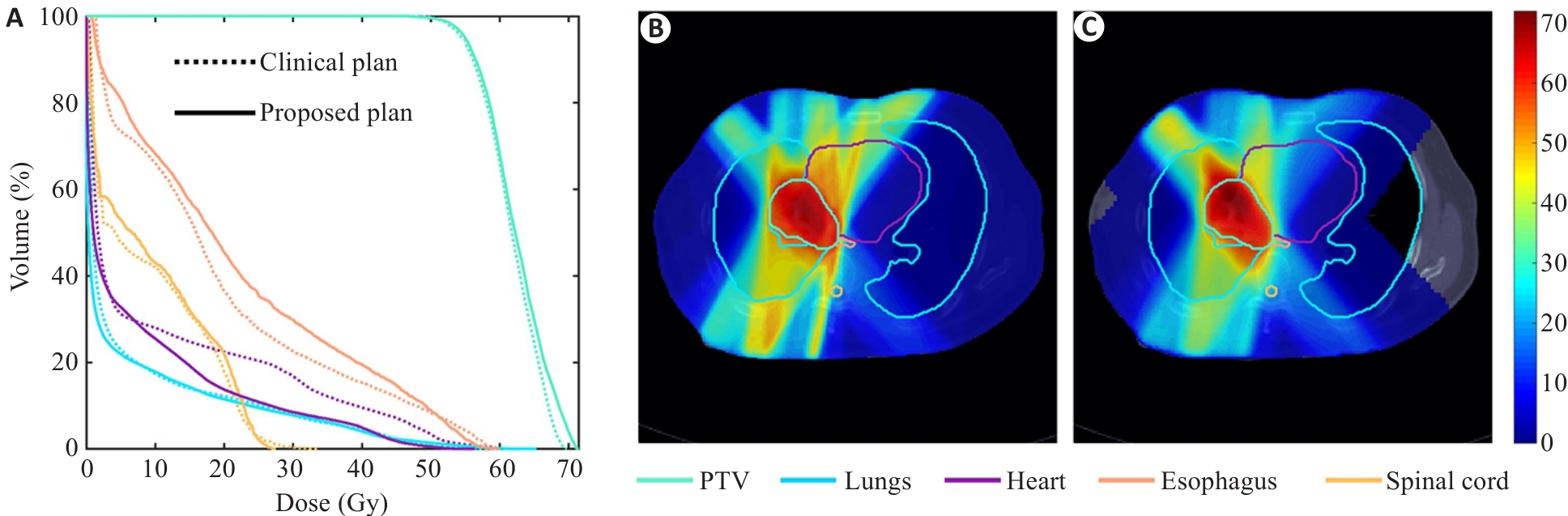
Fig.1 Comparison of dose-volume histogram (DVH) and transversal dose distribution in a case of lung cancer. A: DVH. B: Reference clinical plan. C: Proposed plan.
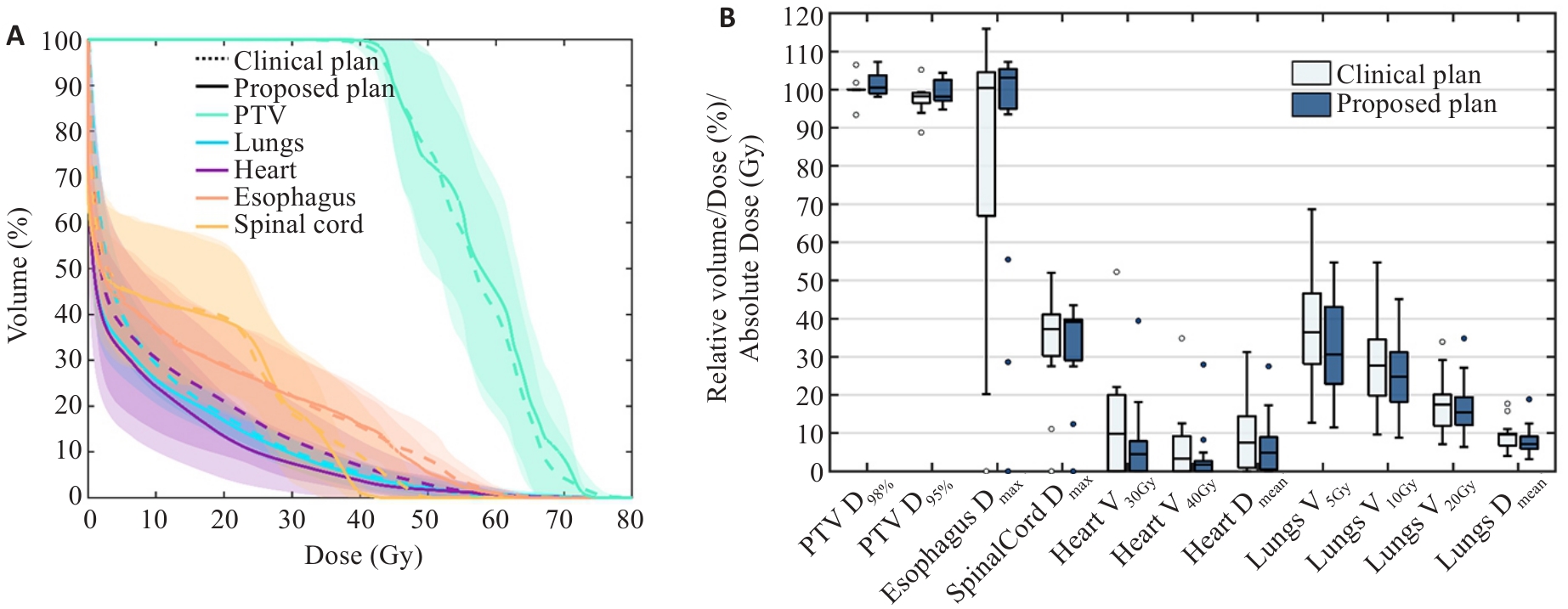
Fig.2 Comparison of dosimetric parameters in different plans for 15 lung cancer cases. A: Average DVH with 95% confidence interval. B: Dosimetric indices. *: Absolute dose (Gy). Dx%: Relative dose received by x% of the volume; Vx Gy: Relative volume receiving at least x Gy; Dmax: Maximum dose; Dmean: Mean dose.
| ROI | Metric | Constraint | Clinical plan | Proposed plan | t/z | P |
|---|---|---|---|---|---|---|
| PTV | D95%(%) | ≥98 | 100.33±1.93 | 102.57±3.30 | -2.087 | 0.056 |
| D98%(%) | - | 95.52±5.23 | 99.80±2.66 | -1.647 | 0.100a | |
| Lungs | V20Gy(%) | ≤30 | 18.21±6.23 | 16.74±7.12 | 2.007 | 0.064 |
| V10Gy(%) | ≤45 | 29.09±11.03 | 26.27±8.91 | 3.216 | 0.006 | |
| V5Gy(%) | ≤60 | 40.40±14.75 | 34.98±13.15 | 2.759 | 0.015 | |
| Dmean(Gy) | - | 9.50±3.24 | 8.40±4.01 | 4.104 | 0.001 | |
| Heart | V30Gy(%) | ≤40 | 13.4±16.07 | 7.83±11.90 | -2.845 | 0.004a |
| V40Gy(%) | ≤30 | 7.21±10.46 | 4.18±8.51 | -2.803 | 0.005a | |
| Dmean(Gy) | - | 9.83±9.41 | 7.02±8.16 | 4.537 | <0.001 | |
| Esophagus | Dmax(Gy) | ≤105 | 74.51±39.51 | 80.19±38.48 | -0.722 | 0.470a |
| V60%(%) | - | 1.20±3.27 | 0.93±2.24 | -0.338 | 0.735a | |
| Spinal cord | Dmax(Gy) | ≤45 | 31.49±15.49 | 30.11±14.04 | 0.809 | 0.432 |
Tab.2 Comparison of average dosimetric indications for 15 lung cancer cases (Mean±SD)
| ROI | Metric | Constraint | Clinical plan | Proposed plan | t/z | P |
|---|---|---|---|---|---|---|
| PTV | D95%(%) | ≥98 | 100.33±1.93 | 102.57±3.30 | -2.087 | 0.056 |
| D98%(%) | - | 95.52±5.23 | 99.80±2.66 | -1.647 | 0.100a | |
| Lungs | V20Gy(%) | ≤30 | 18.21±6.23 | 16.74±7.12 | 2.007 | 0.064 |
| V10Gy(%) | ≤45 | 29.09±11.03 | 26.27±8.91 | 3.216 | 0.006 | |
| V5Gy(%) | ≤60 | 40.40±14.75 | 34.98±13.15 | 2.759 | 0.015 | |
| Dmean(Gy) | - | 9.50±3.24 | 8.40±4.01 | 4.104 | 0.001 | |
| Heart | V30Gy(%) | ≤40 | 13.4±16.07 | 7.83±11.90 | -2.845 | 0.004a |
| V40Gy(%) | ≤30 | 7.21±10.46 | 4.18±8.51 | -2.803 | 0.005a | |
| Dmean(Gy) | - | 9.83±9.41 | 7.02±8.16 | 4.537 | <0.001 | |
| Esophagus | Dmax(Gy) | ≤105 | 74.51±39.51 | 80.19±38.48 | -0.722 | 0.470a |
| V60%(%) | - | 1.20±3.27 | 0.93±2.24 | -0.338 | 0.735a | |
| Spinal cord | Dmax(Gy) | ≤45 | 31.49±15.49 | 30.11±14.04 | 0.809 | 0.432 |
| Prognostic | Clinical plan | Proposed plan | t/z | P |
|---|---|---|---|---|
| LRF | 60.05±12.38 | 59.66±11.88 | 1.053 | 0.310 |
| CE | 7.99±5.20 | 6.55±3.97 | -3.296 | 0.001a |
| RP | 3.84±1.60 | 3.59±2.08 | -2.556 | 0.011a |
| TCP | 57.37±11.26 | 57.95±11.36 | -0.614 | 0.549 |
| NTCP_heart | 3.67±5.78 | 2.20±5.56 | -3.045 | 0.002a |
| NTCP_lung | 2.56±2.10 | 2.34±2.92 | -2.556 | 0.011a |
Tab.3 Comparison of average predicted rates of prognostic events in 15 lung cancer cases (Mean±SD, %)
| Prognostic | Clinical plan | Proposed plan | t/z | P |
|---|---|---|---|---|
| LRF | 60.05±12.38 | 59.66±11.88 | 1.053 | 0.310 |
| CE | 7.99±5.20 | 6.55±3.97 | -3.296 | 0.001a |
| RP | 3.84±1.60 | 3.59±2.08 | -2.556 | 0.011a |
| TCP | 57.37±11.26 | 57.95±11.36 | -0.614 | 0.549 |
| NTCP_heart | 3.67±5.78 | 2.20±5.56 | -3.045 | 0.002a |
| NTCP_lung | 2.56±2.10 | 2.34±2.92 | -2.556 | 0.011a |
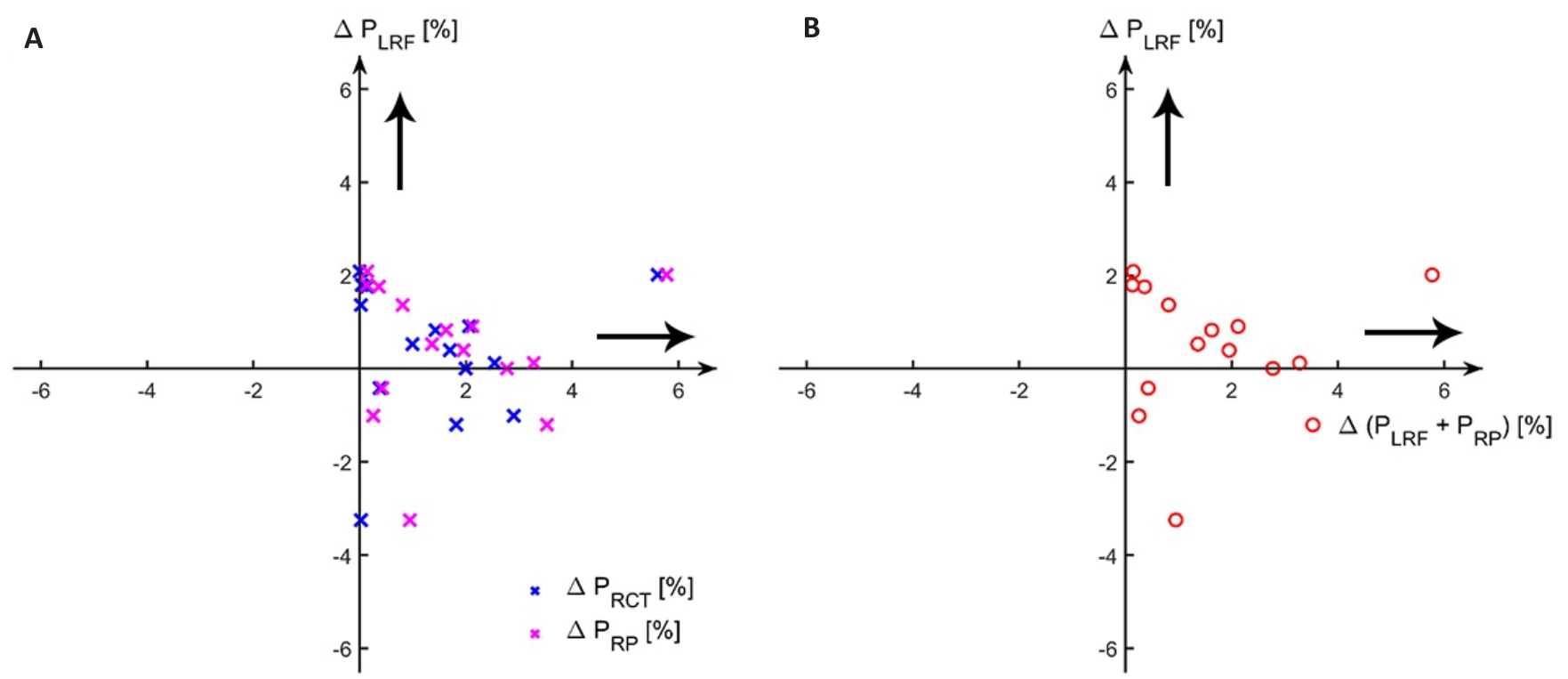
Fig.3 Comparison of predicted prognosis probability among different plans for 15 lung cancer patients. A: ∆PLRF vs ∆PRP/∆PRCT . B. ∆PLRF vs ∆(PRP+PRCT). ∆= item of clinical plan-item of proposed plan; The direction of the black arrow indicates that the proposed plan have a better prognosis. LRF: Local control failure; RCT: Radiation-induced cardiac toxicity; RP: Radiation pneumonitis.
| 1 | 中华医学会肿瘤学分会, 中华医学会杂志社. 中华医学会肺癌临床诊疗指南(2023版)[J]. 中华医学杂志, 2023, 103(27): 2037-74. |
| 2 | Kong FM, Zhao J, Wang J, et al. Radiation dose effect in locally advanced non-small cell lung cancer[J]. J Thorac Dis, 2014, 6(4): 336-47. |
| 3 | Bradley JD, Paulus R, Komaki R, et al. Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small-cell lung cancer (RTOG 0617): a randomised, two-by-two factorial phase 3 study[J]. Lancet Oncol, 2015, 16(2): 187-99. |
| 4 | Arroyo-Hernández M, Maldonado F, Lozano-Ruiz F, et al. Radiation-induced lung injury: current evidence[J]. BMC Pulm Med, 2021, 21(1): 9. |
| 5 | García-Pardo M, Chang A, Schmid S, et al. Respiratory and cardiometabolic comorbidities and stages I to III NSCLC survival: a pooled analysis from the international lung cancer consortium[J]. J Thorac Oncol, 2023, 18(3): 313-23. |
| 6 | Boonyawan K, Gomez DR, Komaki R, et al. Clinical and dosimetric factors predicting grade ≥2 radiation pneumonitis after postoperative radiotherapy for patients with non-small cell lung carcinoma[J]. Int J Radiat Oncol, 2018, 101(4): 919-26. |
| 7 | Overgaard J, Aznar MC, Bacchus C, et al. Personalised radiation therapy taking both the tumour and patient into consideration[J]. Radiother Oncol, 2022, 166: A1-5. |
| 8 | Khan FM, Gibbons JP.The physics of radiation therapy [M]. Baltimore and Philadelphia: Lippincott Williams & Wilkins, 2019. |
| 9 | Deasy JO, Mayo CS, Orton CG. Treatment planning evaluation and optimization should be biologically and not dose/volume based[J]. Med Phys, 2015, 42(6): 2753-6. |
| 10 | Wu QW, Mohan R, Niemierko A, et al. Optimization of intensity-modulated radiotherapy plans based on the equivalent uniform dose[J]. Int J Radiat Oncol, 2002, 52(1): 224-35. |
| 11 | Kierkels RGJ, Korevaar EW, Steenbakkers RJHM, et al. Direct use of multivariable normal tissue complication probability models in treatment plan optimisation for individualised head and neck cancer radiotherapy produces clinically acceptable treatment plans[J]. Radiother Oncol, 2014, 112(3): 430-6. |
| 12 | Mazonakis M, Tzanis E, Lyraraki E, et al. Automatic radiobiological comparison of radiation therapy plans: an application to gastric cancer[J]. Cancers: Basel, 2022, 14(24): 6098. |
| 13 | Thomas E, Chapet O, Kessler ML, et al. Benefit of using biologic parameters (EUD and NTCP) in IMRT optimization for treatment of intrahepatic tumors[J]. Int J Radiat Oncol Biol Phys, 2005, 62(2): 571-8. |
| 14 | Allen Li X, Alber M, Deasy JO, et al. The use and QA of biologically related models for treatment planning: short report of the TG-166 of the therapy physics committee of the AAPM[J]. Med Phys, 2012, 39(3): 1386-409. |
| 15 | Modiri A, Vogelius I, Rechner LA, et al. Outcome-based multiobjective optimization of lymphoma radiation therapy plans[J]. Br J Radiol, 2021, 94(1127): 20210303. |
| 16 | Modiri A, Stick LB, Rice SR, et al. Individualized estimates of overall survival in radiation therapy plan optimization - A concept study[J]. Med Phys, 2018, 45(11): 5332-42. |
| 17 | Machtay M, Bae K, Movsas B, et al. Higher biologically effective dose of radiotherapy is associated with improved outcomes for locally advanced non-small cell lung carcinoma treated with chemoradiation: an analysis of the radiation therapy oncology group[J]. Int J Radiat Oncol, 2012, 82(1): 425-34. |
| 18 | Dess RT, Sun Y, Matuszak MM, et al. Cardiac events after radiation therapy: combined analysis of prospective multicenter trials for locally advanced non-small-cell lung cancer[J]. J Clin Oncol, 2017, 35(13): 1395-402. |
| 19 | Thor M, Deasy J, Iyer A, et al. Toward personalized dose-prescription in locally advanced non-small cell lung cancer: Validation of published normal tissue complication probability models[J]. Radiother Oncol, 2019, 138: 45-51. |
| 20 | Wieser HP, Cisternas E, Wahl N, et al. Development of the open-source dose calculation and optimization toolkit matRad[J]. Med Phys, 2017, 44(6): 2556-68. |
| 21 | Okunieff P, Morgan D, Niemierko A, et al. Radiation dose-response of human tumors[J]. Int J Radiat Oncol, 1995, 32(4): 1227-37. |
| 22 | Gagliardi G, Lax I, Ottolenghi A, et al. Long-term cardiac mortality after radiotherapy of breast cancer: application of the relative seriality model[J]. Br J Radiol, 1996, 69(825): 839-46. |
| 23 | Seppenwoolde Y, Lebesque JV, de Jaeger K, et al. Comparing different NTCP models that predict the incidence of radiation pneumonitis. Normal tissue complication probability[J]. Int J Radiat Oncol Biol Phys, 2003, 55(3): 724-35. |
| 24 | Yegya-Raman N, Wang K, Kim S, et al. Dosimetric predictors of symptomatic cardiac events after conventional-dose chemoradiation therapy for inoperable NSCLC[J]. J Thorac Oncol, 2018, 13(10): 1508-18. |
| 25 | Cui S, Hope A, Dilling TJ, et al. Artificial intelligence for outcome modeling in radiotherapy[J]. Semin Radiat Oncol, 2022, 32(4): 351-64. |
| 26 | Niraula D, Cui SN, Pakela J, et al. Current status and future developments in predicting outcomes in radiation oncology[J]. Br J Radiol, 2022, 95(1139): 20220239. |
| 27 | Choi MS, Choi BS, Chung SY, et al. Clinical evaluation of atlas- and deep learning-based automatic segmentation of multiple organs and clinical target volumes for breast cancer[J]. Radiother Oncol, 2020, 153: 139-45. |
| 28 | Herr DJ, Yin HY, Bergsma D, et al. Factors associated with acute esophagitis during radiation therapy for lung cancer[J]. Radiother Oncol, 2024, 197: 110349. |
| 29 | Bergom C, Bradley JA, Ng AK, et al. Past, present, and future of radiation-induced cardiotoxicity: refinements in targeting, surveillance, and risk stratification[J]. JACC CardioOncology, 2021, 3(3): 343-59. |
| 30 | Hussein M, Heijmen BJM, Verellen D, et al. Automation in intensity modulated radiotherapy treatment planning-a review of recent innovations[J]. Br J Radiol, 2018, 91(1092): 20180270. |
| 31 | Potrebko PS, Fiege J, Biagioli M, et al. Investigating multi-objective fluence and beam orientation IMRT optimization[J]. Phys Med Biol, 2017, 62(13): 5228-44. |
| [1] | . Constraint priority list-based multi-objective optimization for intensity-modulated radiation therapy [J]. Journal of Southern Medical University, 2018, 38(06): 691-. |
| [2] | . Prediction of three-dimensional dose distribution in intensity-modulated radiation therapy based on neural network learning [J]. Journal of Southern Medical University, 2018, 38(06): 683-. |
| [3] | ZHAO Dang, LIU Xing-jing, XIE Qiang, HUANG Zuo-ping, ZOU Bing-xin, GE Yong-bin Department of Oncology, Hospital of Military police Guangdong General Team, Guangzhou 510507, China. Intensity-modulated radiation combined with Delisheng injection for naspharyngeal carcinoma [J]. Journal of Southern Medical University, 2006, 26(06): 874-875. |
| [4] | TANG Mu-tao, CHEN Chao-min, ZHOU Ling-hong, LU Qing-wen, WANG Zhuo-yu, CHEN Guang-jie School of Biomedical Engineering, Southern Medical University, Guangzhou 510515, China. A preliminary study of beam weight optimization of intensity-modulated radiation therapy with genetic algorithm [J]. Journal of Southern Medical University, 2006, 26(04): 456-458. |
| Viewed | ||||||
|
Full text |
|
|||||
|
Abstract |
|
|||||