南方医科大学学报 ›› 2025, Vol. 45 ›› Issue (9): 1880-1888.doi: 10.12122/j.issn.1673-4254.2025.09.08
• • 上一篇
刘炎忠1,2, 朱润2, 李玉柱2, 马鑫2( ), 麦海星2(
), 麦海星2( )
)
收稿日期:2025-02-12
出版日期:2025-09-20
发布日期:2025-09-28
通讯作者:
马鑫,麦海星
E-mail:urologist@foxmail.com;maihx1981@163.com
作者简介:刘炎忠,在读博士研究生,主治医师,E-mail: 15001168010 @163.com
基金资助:
Yanzhong LIU1,2, Run ZHU2, Yuzhu LI2, Xin MA2( ), Haixing MAI2(
), Haixing MAI2( )
)
Received:2025-02-12
Online:2025-09-20
Published:2025-09-28
Contact:
Xin MA, Haixing MAI
E-mail:urologist@foxmail.com;maihx1981@163.com
摘要:
目的 探讨肾部分切除术后继发同侧上尿路结石的发病情况及其危险因素。 方法 回顾性分析我中心行肾部分切除术的患者基线资料(年龄、性别、体质量指数),生活习惯(吸烟、饮酒),基础病(高血压、糖尿病、高甘油三酯血症、高胆固醇血症、高尿酸血症、心血管疾病),肾肿瘤术前情况(肿瘤最大直径、肿瘤多发、肿瘤位置、肿瘤伴有出血、肿瘤伴有坏死、肿瘤伴有囊性变、肿瘤生长方式),术前肾小球滤过率、术中情况(肾脏集合系统受损、肾脏缺血时间、手术时间、手术方式、术中预计出血量)。分析肾部分切除术后继发同侧上尿路结石的临床特征及危险因素。 结果 肾部分切除术后上尿路结石发病率为7.80%(112/1435),其中同侧上尿路结石发病率高于对侧上尿路结石发病率(4.95% vs 1.46%,P<0.001)。同侧上尿路结石发病率高于双侧上尿路结石发病率(4.95% vs 1.39%,P<0.001)。术中肾脏集合系统受损是肾部分切除术后继发同侧上尿路结石的危险因素(OR=4.550,95% CI:2.237~9.252,P<0.001);糖尿病可能是肾部分切除术后继发同侧上尿路结石的危险因素(OR=2.419,95% CI:0.973~6.012,P=0.057)。 结论 肾部分切除术后同侧上尿路结石发病率高于对侧及双侧。术中肾脏集合系统是肾部分切除术后继发同侧上尿路结石的危险因素。
刘炎忠, 朱润, 李玉柱, 马鑫, 麦海星. 术中肾脏集合系统受损是肾部分切除术后同侧上尿路结石发病的危险因素:一项1∶2匹配病例对照研究[J]. 南方医科大学学报, 2025, 45(9): 1880-1888.
Yanzhong LIU, Run ZHU, Yuzhu LI, Xin MA, Haixing MAI. Intraoperative renal collecting system damage increases risks of ipsilateral upper urinary tract stones after partial nephrectomy: a 1∶2 propensity-matched case-control study[J]. Journal of Southern Medical University, 2025, 45(9): 1880-1888.
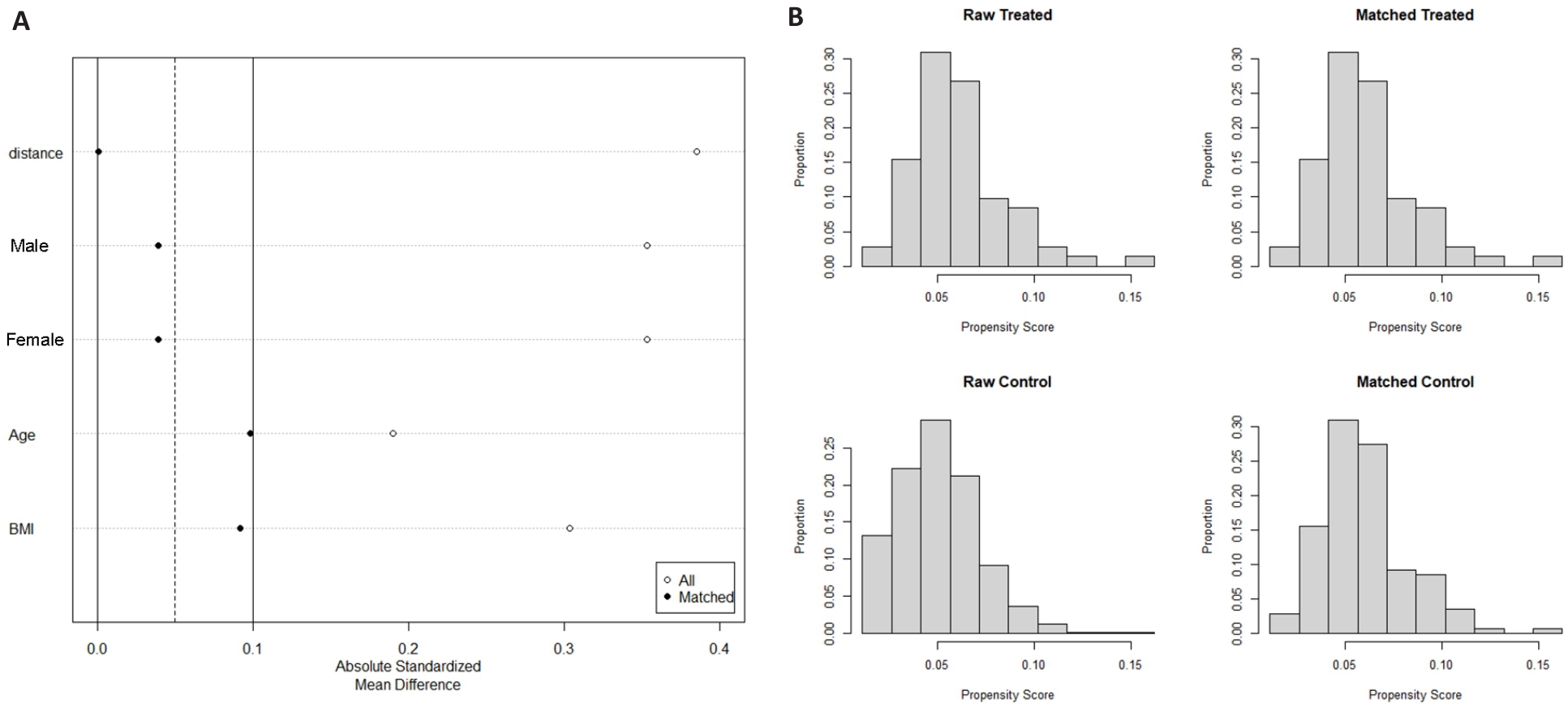
图2 倾向性评分匹配图
Fig.2 Plot of the propensity score-matched study. A: Dot plot of standardized mean difference. B: Histogram of standardized mean differences (before and after).
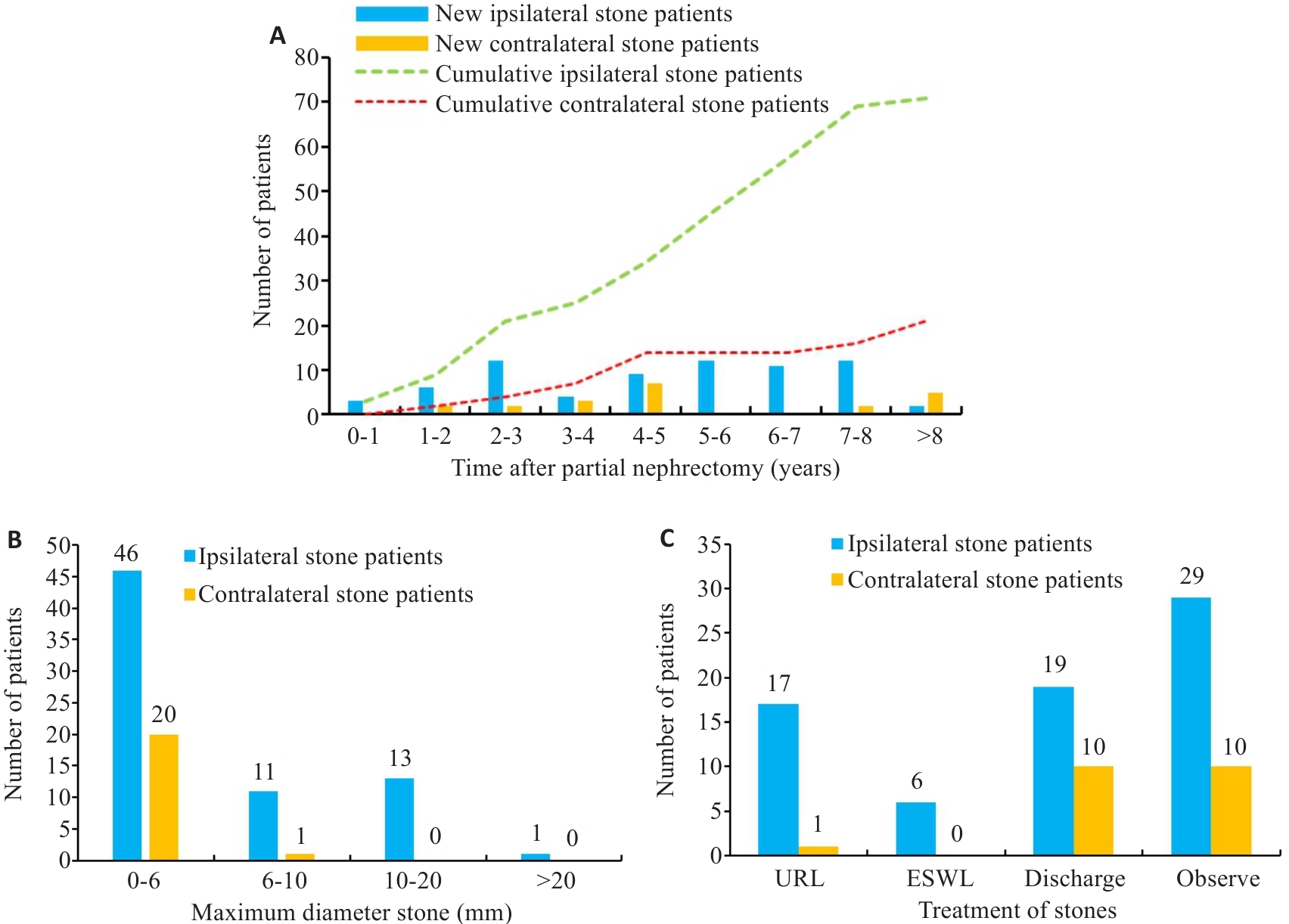
图3 肾部分切除术后同侧及对侧上尿路结石发病情况、临床特征及治疗
Fig.3 Incidence, clinical features and treatment of ipsilateral and contralateral stones after partial nephrectomy. A: Number of new and accumulated patients with ipsilateral and contralateral upper urinary tract stones. B: Difference of maximum diameter between ipsilateral and contralateral upper urinary tract stones after operation. C: The treatment difference of ipsilateral and contralateral upper urinary tract stones after operation.
| Clinical characteristics | Patients with unilateral stones | Patients with bilateral stones | ||||||
|---|---|---|---|---|---|---|---|---|
Surgical side (n=71) | Non-surgical side (n=21) | T/ | P | Surgical side (n=20) | Non-surgical side (n=20) | T/ | P | |
| Age (years, Mean±SD) | 50.18±10.77 | 46.43±10.05 | 1.424a | 0.158 | 45.75±12.11 | 45.75±12.11 | ||
| BMI (Mean±SD) | 27.00±3.68 | 26.2±3.50 | 0.891a | 0.375 | 26.17±4.57 | 26.17±4.57 | ||
| Gender [n (%)] | 1.840b | 0.205 | ||||||
| Male | 60 (84.51) | 15 (71.43) | 16 (80.00) | 16 (80.00) | ||||
| Female | 11 (15.49) | 6 (28.57) | 4 (20.00) | 4 (20.00) | ||||
| Maximum diameter (mm) | 3 (2-18) | 3 (2-8) | -2.140c | 0.032 | 2 (2-20) | 2.5 (2-19) | 1.296c | 0.195 |
| Maximum diameter >6 mm [n (%)] | 7.411b | 0.005 | 0.784b | 0.661 | ||||
| Yes | 25 (35.21) | 1 (4.76) | 2 (10.00) | 4 (20.00) | ||||
| No | 46 (64.79) | 20 (95.24) | 18 (90.00) | 16 (80.00) | ||||
| Surgical treatment [n (%)] | 6.418b | 0.011 | 0.229b | 1.000 | ||||
| Yes | 23 (32.39) | 1 (4.76) | 2 (10.00) | 3 (15.00) | ||||
| No | 48 (67.61) | 20 (95.24) | 18 (80.00) | 17 (85.00) | ||||
表1 肾部分切除术后继发上尿路结石患者的一般资料
Tab.1 Clinical characteristics of patients with upper urinary tract stones after partial nephrectomy
| Clinical characteristics | Patients with unilateral stones | Patients with bilateral stones | ||||||
|---|---|---|---|---|---|---|---|---|
Surgical side (n=71) | Non-surgical side (n=21) | T/ | P | Surgical side (n=20) | Non-surgical side (n=20) | T/ | P | |
| Age (years, Mean±SD) | 50.18±10.77 | 46.43±10.05 | 1.424a | 0.158 | 45.75±12.11 | 45.75±12.11 | ||
| BMI (Mean±SD) | 27.00±3.68 | 26.2±3.50 | 0.891a | 0.375 | 26.17±4.57 | 26.17±4.57 | ||
| Gender [n (%)] | 1.840b | 0.205 | ||||||
| Male | 60 (84.51) | 15 (71.43) | 16 (80.00) | 16 (80.00) | ||||
| Female | 11 (15.49) | 6 (28.57) | 4 (20.00) | 4 (20.00) | ||||
| Maximum diameter (mm) | 3 (2-18) | 3 (2-8) | -2.140c | 0.032 | 2 (2-20) | 2.5 (2-19) | 1.296c | 0.195 |
| Maximum diameter >6 mm [n (%)] | 7.411b | 0.005 | 0.784b | 0.661 | ||||
| Yes | 25 (35.21) | 1 (4.76) | 2 (10.00) | 4 (20.00) | ||||
| No | 46 (64.79) | 20 (95.24) | 18 (90.00) | 16 (80.00) | ||||
| Surgical treatment [n (%)] | 6.418b | 0.011 | 0.229b | 1.000 | ||||
| Yes | 23 (32.39) | 1 (4.76) | 2 (10.00) | 3 (15.00) | ||||
| No | 48 (67.61) | 20 (95.24) | 18 (80.00) | 17 (85.00) | ||||
| Item | Before matched | After matched | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
Total (n=1394) | Control group (n=1323) | Case group (n=71) | t/ | P | Total (n=207) | Control group (n=138) | Case group (n=69) | t/ | P | ||
| Age (year) | 52.13±11.41 | 52.23±11.44 | 50.18±10.77 | 1.474 | 0.141 | 49.86±11.49 | 49.54±11.88 | 50.49±10.74 | -0.559 | 0.577 | |
| BMI | 25.95±3.43 | 25.89±3.41 | 27.01±3.68 | -2.679 | 0.007 | 26.51±3.39 | 26.40±3.46 | 26.72±3.27 | -0.635 | 0.526 | |
| Gender | 5.502 | 0.019 | 0.076 | 0.783 | |||||||
| Male | 1009(72.38) | 949 (71.73) | 60 (84.51) | 176 (85.02) | 118 (85.51) | 58 (84.06) | |||||
| Female | 385 (27.62) | 374 (28.27) | 11 (15.49) | 31 (14.98) | 20 (14.49) | 11 (15.94) | |||||
表2 匹配前后患者年龄、性别和BMI差异性分析
Tab.2 Analysis of the differences in age, gender and BMI of the patients before and after matching
| Item | Before matched | After matched | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
Total (n=1394) | Control group (n=1323) | Case group (n=71) | t/ | P | Total (n=207) | Control group (n=138) | Case group (n=69) | t/ | P | ||
| Age (year) | 52.13±11.41 | 52.23±11.44 | 50.18±10.77 | 1.474 | 0.141 | 49.86±11.49 | 49.54±11.88 | 50.49±10.74 | -0.559 | 0.577 | |
| BMI | 25.95±3.43 | 25.89±3.41 | 27.01±3.68 | -2.679 | 0.007 | 26.51±3.39 | 26.40±3.46 | 26.72±3.27 | -0.635 | 0.526 | |
| Gender | 5.502 | 0.019 | 0.076 | 0.783 | |||||||
| Male | 1009(72.38) | 949 (71.73) | 60 (84.51) | 176 (85.02) | 118 (85.51) | 58 (84.06) | |||||
| Female | 385 (27.62) | 374 (28.27) | 11 (15.49) | 31 (14.98) | 20 (14.49) | 11 (15.94) | |||||
| Variable | Control group after matching (n=138) | Case group after matching (n=69) | T/ | P | |
|---|---|---|---|---|---|
| Tumor size (cm) | 2.93±1.10 | 2.72±1.04 | 1.296a | 0.196 | |
| Multiple tumors | Yes | 1 (0.72) | 1 (1.45) | 0.252b | 0.615 |
| No | 137 (99.28) | 68 (98.55) | |||
| Operation time (min) | 130.00 (95.75, 155.00) | 120.00 (91.50, 148.50) | -1.110c | 0.267 | |
| Tumor location | Left | 67 (48.55) | 40 (57.97) | 1.635b | 0.201 |
| Right | 71 (51.45) | 29 (42.03) | |||
| Tumor hemorrhage | Yes | 71 (51.45) | 26 (37.68) | 3.502b | 0.061 |
| No | 67 (48.55) | 43 (62.32) | |||
| Tumor cystic change | Yes | 47 (34.06) | 21 (30.43) | 0.274b | 0.601 |
| No | 91 (65.94) | 48 (69.57) | |||
| Tumor necrosis | Yes | 9 (6.52) | 4 (5.80) | 0.041b | 0.839 |
| No | 129 (93.48) | 65 (94.20) | |||
| Diabetes | Yes | 15 (10.87) | 12 (17.39) | 1.725b | 0.189 |
| No | 123 (89.13) | 57 (82.61) | |||
| Ardiovascular diseases | Yes | 9 (6.52) | 2 (2.90) | 1.200b | 0.273 |
| No | 129 (93.48) | 67 (97.10) | |||
| Hypertension | Yes | 39 (28.26) | 16 (23.19) | 0.607b | 0.436 |
| No | 99 (71.74) | 53 (76.81) | |||
| Smoke | Yes | 21 (15.22) | 11 (15.94) | 0.018b | 0.892 |
| No | 117 (84.78) | 58 (84.06) | |||
| Drink | Yes | 22 (15.94) | 7 (10.14) | 1.283b | 0.257 |
| No | 116 (84.06) | 62 (89.86) | |||
| Hematuria | Yes | 5 (3.62) | 3 (4.35) | 0.065b | 0.799 |
| No | 133 (96.38) | 66 (95.65) | |||
| Endogenous tumor | Yes | 86 (62.77) | 40 (57.97) | 0.446b | 0.504 |
| No | 51 (37.23) | 29 (42.03) | |||
| RPCI | Yes | 58 (42.34) | 52 (75.36) | 20.110b | <0.001 |
| No | 79 (57.66) | 17 (24.64) | |||
| Hyperlipidemia | Yes | 48 (34.78) | 23 (33.33) | 0.043b | 0.836 |
| No | 90 (65.22) | 46 (66.67) | |||
| Hyperuricemia | Yes | 22 (15.94) | 13 (18.84) | 0.275b | 0.600 |
| No | 116 (84.06) | 56 (81.16) | |||
| Surgical method | Robot-assisted | 66 (47.83) | 30 (43.48) | 0.350b | 0.554 |
| Laparoscopy | 72 (52.17) | 39 (56.52) | |||
| Estimated intraoperative blood loss (mL) | 50.00 (20.00, 80.00) | 50.00 (20.00, 50.00) | -0.284c | 0.776 | |
| Renal ischemia-reperfusion time (min) | 19.90±7.42 | 20.03±7.67 | -0.116a | 0.908 | |
| Glomerular filtration rate (mL/min) | 103.78±8.69 | 102.58±7.45 | 1.032a | 0.304 | |
表3 匹配后肾部分切除术后患者一般资料及围手术期情况
Tab.3 General and perioperative data of the patientsafter partial nephrectomy (after propensity score matching)
| Variable | Control group after matching (n=138) | Case group after matching (n=69) | T/ | P | |
|---|---|---|---|---|---|
| Tumor size (cm) | 2.93±1.10 | 2.72±1.04 | 1.296a | 0.196 | |
| Multiple tumors | Yes | 1 (0.72) | 1 (1.45) | 0.252b | 0.615 |
| No | 137 (99.28) | 68 (98.55) | |||
| Operation time (min) | 130.00 (95.75, 155.00) | 120.00 (91.50, 148.50) | -1.110c | 0.267 | |
| Tumor location | Left | 67 (48.55) | 40 (57.97) | 1.635b | 0.201 |
| Right | 71 (51.45) | 29 (42.03) | |||
| Tumor hemorrhage | Yes | 71 (51.45) | 26 (37.68) | 3.502b | 0.061 |
| No | 67 (48.55) | 43 (62.32) | |||
| Tumor cystic change | Yes | 47 (34.06) | 21 (30.43) | 0.274b | 0.601 |
| No | 91 (65.94) | 48 (69.57) | |||
| Tumor necrosis | Yes | 9 (6.52) | 4 (5.80) | 0.041b | 0.839 |
| No | 129 (93.48) | 65 (94.20) | |||
| Diabetes | Yes | 15 (10.87) | 12 (17.39) | 1.725b | 0.189 |
| No | 123 (89.13) | 57 (82.61) | |||
| Ardiovascular diseases | Yes | 9 (6.52) | 2 (2.90) | 1.200b | 0.273 |
| No | 129 (93.48) | 67 (97.10) | |||
| Hypertension | Yes | 39 (28.26) | 16 (23.19) | 0.607b | 0.436 |
| No | 99 (71.74) | 53 (76.81) | |||
| Smoke | Yes | 21 (15.22) | 11 (15.94) | 0.018b | 0.892 |
| No | 117 (84.78) | 58 (84.06) | |||
| Drink | Yes | 22 (15.94) | 7 (10.14) | 1.283b | 0.257 |
| No | 116 (84.06) | 62 (89.86) | |||
| Hematuria | Yes | 5 (3.62) | 3 (4.35) | 0.065b | 0.799 |
| No | 133 (96.38) | 66 (95.65) | |||
| Endogenous tumor | Yes | 86 (62.77) | 40 (57.97) | 0.446b | 0.504 |
| No | 51 (37.23) | 29 (42.03) | |||
| RPCI | Yes | 58 (42.34) | 52 (75.36) | 20.110b | <0.001 |
| No | 79 (57.66) | 17 (24.64) | |||
| Hyperlipidemia | Yes | 48 (34.78) | 23 (33.33) | 0.043b | 0.836 |
| No | 90 (65.22) | 46 (66.67) | |||
| Hyperuricemia | Yes | 22 (15.94) | 13 (18.84) | 0.275b | 0.600 |
| No | 116 (84.06) | 56 (81.16) | |||
| Surgical method | Robot-assisted | 66 (47.83) | 30 (43.48) | 0.350b | 0.554 |
| Laparoscopy | 72 (52.17) | 39 (56.52) | |||
| Estimated intraoperative blood loss (mL) | 50.00 (20.00, 80.00) | 50.00 (20.00, 50.00) | -0.284c | 0.776 | |
| Renal ischemia-reperfusion time (min) | 19.90±7.42 | 20.03±7.67 | -0.116a | 0.908 | |
| Glomerular filtration rate (mL/min) | 103.78±8.69 | 102.58±7.45 | 1.032a | 0.304 | |
| Variable | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| P | OR | 95% CI | P | OR | 95% CI | |
| Tumor size (cm) | 0.182 | 0.821 | 0.615-1.096 | |||
| Multiple tumors | 0.624 | 2.000 | 0.125-31.975 | |||
| Operation time (min) | 0.222 | 0.996 | 0.989-1.003 | |||
| Tumor location | 0.182 | 0.66 | 0.358-1.215 | |||
| Tumor hemorrhage | 0.072 | 0.584 | 0.325-1.050 | 0.160 | 0.629 | 0.329-1.201 |
| Tumor cystic change | 0.586 | 0.835 | 0.436-1.599 | |||
| Tumor necrosis | 0.845 | 0.889 | 0.274-2.886 | |||
| Diabetes | 0.208 | 1.669 | 0.753-3.700 | 0.057 | 2.419 | 0.973-6.012 |
| Ardiovascular diseases | 0.277 | 0.415 | 0.085-2.025 | |||
| Hypertension | 0.429 | 0.76 | 0.385-1.501 | |||
| Smokeing | 0.894 | 1.055 | 0.483-2.303 | |||
| Drinking | 0.289 | 0.627 | 0.264-1.487 | |||
| Hematuria | 0.803 | 1.2 | 0.287-5.021 | |||
| Endogenous tumor | 0.523 | 0.816 | 0.438-1.522 | |||
| RPCI | <0.001 | 4.103 | 2.110-7.978 | <0.001 | 4.550 | 2.237-9.252 |
| Hyperlipidemia | 0.819 | 0.924 | 0.470-1.815 | 0.964 | 0.982 | 0.444-2.173 |
| Hyperuricemia | 0.580 | 1.257 | 0.559-2.825 | 0.493 | 1.398 | 0.536-3.650 |
| Surgical method | 0.545 | 1.203 | 0.661-2.190 | |||
| Estimated intraoperative blood loss (mL) | 0.544 | 0.999 | 0.996-1.002 | |||
| Renal ischemia-reperfusion time (min) | 0.907 | 1.002 | 0.964-1.042 | |||
| Glomerular filtration rate (mL/min) | 0.333 | 0.983 | 0.948-1.018 | |||
表4 匹配后肾部分切除术患者继发同侧上尿路结石的条件回归分析
Tab.4 Conditional regression analyses of secondary operative renal ureteral calculi in patients after partial nephrectomy (after propensity score matching)
| Variable | Univariate analysis | Multivariate analysis | ||||
|---|---|---|---|---|---|---|
| P | OR | 95% CI | P | OR | 95% CI | |
| Tumor size (cm) | 0.182 | 0.821 | 0.615-1.096 | |||
| Multiple tumors | 0.624 | 2.000 | 0.125-31.975 | |||
| Operation time (min) | 0.222 | 0.996 | 0.989-1.003 | |||
| Tumor location | 0.182 | 0.66 | 0.358-1.215 | |||
| Tumor hemorrhage | 0.072 | 0.584 | 0.325-1.050 | 0.160 | 0.629 | 0.329-1.201 |
| Tumor cystic change | 0.586 | 0.835 | 0.436-1.599 | |||
| Tumor necrosis | 0.845 | 0.889 | 0.274-2.886 | |||
| Diabetes | 0.208 | 1.669 | 0.753-3.700 | 0.057 | 2.419 | 0.973-6.012 |
| Ardiovascular diseases | 0.277 | 0.415 | 0.085-2.025 | |||
| Hypertension | 0.429 | 0.76 | 0.385-1.501 | |||
| Smokeing | 0.894 | 1.055 | 0.483-2.303 | |||
| Drinking | 0.289 | 0.627 | 0.264-1.487 | |||
| Hematuria | 0.803 | 1.2 | 0.287-5.021 | |||
| Endogenous tumor | 0.523 | 0.816 | 0.438-1.522 | |||
| RPCI | <0.001 | 4.103 | 2.110-7.978 | <0.001 | 4.550 | 2.237-9.252 |
| Hyperlipidemia | 0.819 | 0.924 | 0.470-1.815 | 0.964 | 0.982 | 0.444-2.173 |
| Hyperuricemia | 0.580 | 1.257 | 0.559-2.825 | 0.493 | 1.398 | 0.536-3.650 |
| Surgical method | 0.545 | 1.203 | 0.661-2.190 | |||
| Estimated intraoperative blood loss (mL) | 0.544 | 0.999 | 0.996-1.002 | |||
| Renal ischemia-reperfusion time (min) | 0.907 | 1.002 | 0.964-1.042 | |||
| Glomerular filtration rate (mL/min) | 0.333 | 0.983 | 0.948-1.018 | |||
| Variable | Tumor size≤3 cm | Tumor size>3 cm | ||||
|---|---|---|---|---|---|---|
| P | OR | 95% CI | P | OR | 95% CI | |
| Tumor hemorrhage | 0.215 | 0.612 | 0.282-1.330 | 0.373 | 0.590 | 0.184-1.885 |
| Diabetes | 0.014 | 3.820 | 1.317-11.078 | 0.173 | 0.204 | 0.021-2.010 |
| Hyperlipidemia | 0.988 | 1.007 | 0.420-2.411 | 0.776 | 1.192 | 0.356-3.985 |
| Hyperuricemia | 0.294 | 1.837 | 0.590-5.718 | 0.827 | 1.165 | 0.296-4.580 |
| RPCI | 0.001 | 4.001 | 1.761-9.091 | 0.001 | 9.913 | 2.440-40.279 |
表5 肿瘤大小亚组分析
Tab.5 Subgroup analysis of tumor size
| Variable | Tumor size≤3 cm | Tumor size>3 cm | ||||
|---|---|---|---|---|---|---|
| P | OR | 95% CI | P | OR | 95% CI | |
| Tumor hemorrhage | 0.215 | 0.612 | 0.282-1.330 | 0.373 | 0.590 | 0.184-1.885 |
| Diabetes | 0.014 | 3.820 | 1.317-11.078 | 0.173 | 0.204 | 0.021-2.010 |
| Hyperlipidemia | 0.988 | 1.007 | 0.420-2.411 | 0.776 | 1.192 | 0.356-3.985 |
| Hyperuricemia | 0.294 | 1.837 | 0.590-5.718 | 0.827 | 1.165 | 0.296-4.580 |
| RPCI | 0.001 | 4.001 | 1.761-9.091 | 0.001 | 9.913 | 2.440-40.279 |
| Variable | Endogenous tumor | Tumor outreach | ||||
|---|---|---|---|---|---|---|
| P | OR | 95% CI | P | OR | 95% CI | |
| Tumor hemorrhage | 0.069 | 0.469 | 0.208-1.061 | 0.813 | 0.880 | 0.306-2.535 |
| Diabetes | 0.332 | 1.731 | 0.572-5.241 | 0.129 | 3.430 | 0.699-16.825 |
| Hyperlipidemia | 0.630 | 1.239 | 0.519-2.958 | 0.994 | 1.004 | 0.295-3.421 |
| Hyperuricemia | 0.773 | 1.174 | 0.395-3.492 | 0.453 | 1.735 | 0.412-7.313 |
| RPCI | 0.005 | 3.747 | 1.478-9.501 | <0.001 | 8.718 | 2.883-26.362 |
表6 肿瘤内生生长亚组分析
Tab.6 Subgroup analysis of endogenous tumor growth
| Variable | Endogenous tumor | Tumor outreach | ||||
|---|---|---|---|---|---|---|
| P | OR | 95% CI | P | OR | 95% CI | |
| Tumor hemorrhage | 0.069 | 0.469 | 0.208-1.061 | 0.813 | 0.880 | 0.306-2.535 |
| Diabetes | 0.332 | 1.731 | 0.572-5.241 | 0.129 | 3.430 | 0.699-16.825 |
| Hyperlipidemia | 0.630 | 1.239 | 0.519-2.958 | 0.994 | 1.004 | 0.295-3.421 |
| Hyperuricemia | 0.773 | 1.174 | 0.395-3.492 | 0.453 | 1.735 | 0.412-7.313 |
| RPCI | 0.005 | 3.747 | 1.478-9.501 | <0.001 | 8.718 | 2.883-26.362 |
| Variable | Robot-assisted | Laparoscopy | ||||
|---|---|---|---|---|---|---|
| P | OR | 95% CI | P | OR | 95% CI | |
| Tumor hemorrhage | 0.720 | 0.842 | 0.330-2.150 | 0.147 | 0.396 | 0.159-1.089 |
| Diabetes | 0.067 | 3.616 | 0.914-14.315 | 0.704 | 1.273 | 0.365-4.438 |
| Hyperlipidemia | 0.390 | 1.578 | 0.558-4.463 | 0.310 | 0.602 | 0.227-1.601 |
| Hyperuricemia | 0.267 | 1.919 | 0.608-6.061 | 0.756 | 1.235 | 0.327-4.655 |
| RPCI | 0.012 | 3.784 | 1.348-10.622 | 0.000 | 5.604 | 2.254-13.932 |
表7 手术方式亚组分析
Tab.7 Subgroup analysis of surgical approaches
| Variable | Robot-assisted | Laparoscopy | ||||
|---|---|---|---|---|---|---|
| P | OR | 95% CI | P | OR | 95% CI | |
| Tumor hemorrhage | 0.720 | 0.842 | 0.330-2.150 | 0.147 | 0.396 | 0.159-1.089 |
| Diabetes | 0.067 | 3.616 | 0.914-14.315 | 0.704 | 1.273 | 0.365-4.438 |
| Hyperlipidemia | 0.390 | 1.578 | 0.558-4.463 | 0.310 | 0.602 | 0.227-1.601 |
| Hyperuricemia | 0.267 | 1.919 | 0.608-6.061 | 0.756 | 1.235 | 0.327-4.655 |
| RPCI | 0.012 | 3.784 | 1.348-10.622 | 0.000 | 5.604 | 2.254-13.932 |
| [1] | Hill AJ, Basourakos SP, Lewicki P, et al. Incidence of kidney stones in the United States: the continuous national health and nutrition examination survey[J]. J Urol, 2022, 207(4): 851-6. doi:10.1097/ju.0000000000002331 |
| [2] | Sorokin I, Mamoulakis C, Miyazawa K, et al. Epidemiology of stone disease across the world[J]. World J Urol, 2017, 35(9): 1301-20. doi:10.1007/s00345-017-2008-6 |
| [3] | Li H, Shkolyar E, Wang J, et al. SLIPS-LAB-a bioinspired bioanalysis system for metabolic evaluation of urinary stone disease[J]. Sci Adv, 2020, 6(21): eaba8535. doi:10.1126/sciadv.aba8535 |
| [4] | Balentine CJ, Xie RB, Kirklin JK, et al. Failure to diagnose hyperparathyroidism in 10, 432 patients with hypercalcemia[J]. Ann Surg, 2017, 266(4): 632-40. doi:10.1097/sla.0000000000002370 |
| [5] | Chang AR, Grams ME, Navaneethan SD. Bariatric surgery and kidney-related outcomes[J]. Kidney Int Rep, 2017, 2(2): 261-70. doi:10.1016/j.ekir.2017.01.010 |
| [6] | Thongprayoon C, Krambeck AE, Rule AD. Determining the true burden of kidney stone disease[J]. Nat Rev Nephrol, 2020, 16(12): 736-46. doi:10.1038/s41581-020-0320-7 |
| [7] | 邓利娟, 智喜梅, 吴 文. 2型糖尿病合并肾结石的危险因素分析[J]. 南方医科大学学报, 2007, 27(9): 1395-6. doi:10.3321/j.issn:1673-4254.2007.09.037 |
| [8] | Boga MS, Sönmez MG. Long-term renal function following zero ischemia partial nephrectomy[J]. Res Rep Urol, 2019, 11: 43-52. doi:10.2147/rru.s174996 |
| [9] | Shanmugasundaram S, Cieslak JA, Sare A, et al. Preoperative embolization of renal cell carcinoma prior to partial nephrectomy: a systematic review and meta-analysis[J]. Clin Imag, 2021, 76: 205-12. doi:10.1016/j.clinimag.2021.04.021 |
| [10] | Ohba K, Matsuo T, Mitsunari K, et al. Preservation of split renal function after laparoscopic and robot-assisted partial nephrectomy[J]. Anticancer Res, 2022, 42(6): 3055-60. doi:10.21873/anticanres.15792 |
| [11] | Bayles AC, Bhatti A, Sakthivel A, et al. "Clip-strasse": a novel complication following partial nephrectomy[J]. Scand J Urol, 2015, 49(5): 424-5. doi:10.3109/21681805.2015.1040450 |
| [12] | Sun J, Zhao LW, Wang XL, et al. Migration of a Hem-o-Lok clip to the renal pelvis after laparoscopic partial nephrectomy: a case report[J]. World J Clin Cases, 2022, 10(10): 3188-93. doi:10.12998/wjcc.v10.i10.3188 |
| [13] | Baumert H, Ballaro A, Arroyo C, et al. The use of polymer (hem-o-lok) clips for management of the renal hilum during laparoscopic nephrectomy[J]. Eur Urol, 2006, 49(5): 816-9. |
| [14] | Van OA, De Kernion JB. Clinical management of foreign bodies of the genitourinary tract[J]. J Urol, 2000, 164(2): 274-87. doi:10.1016/s0022-5347(05)67342-9 |
| [15] | Park KS, Sim YJ, Jung H. Migration of a hem-o-lok clip to the ureter following laparoscopic partial nephrectomy presenting with lower urinary tract symptoms[J]. Int Neurourol J, 2013, 17(2): 90-2. doi:10.5213/inj.2013.17.2.90 |
| [16] | Dasgupta R, Hannah K, Glass J. Case report: percutaneous nephrolithotomy for a stone on a Hem-o-lok clip[J]. J Endourol, 2008, 22(3): 463-4. doi:10.1089/end.2007.0318 |
| [17] | Zhou H, Li Y, Li G, et al. Hem-o-Lok clip migration into renal pelvis and stone formation as a long-term complication following laparoscopic pyelolithotomy: a case report and literature review[J]. BMC Urol, 2022, 22(1): 66. doi:10.1186/s12894-022-01015-6 |
| [18] | Ganpule A, Patil A, Singh A, et al. Migration of hem-O-lok in pelvicaliceal system mimicking renal Calculus following robotic nephron-sparing surgery: a case report with review of literature[J]. J Endourol Case Rep, 2020, 6(1): 22-5. doi:10.1089/cren.2019.0087 |
| [19] | Kiremit MC, Koseoglu E, Acar O, et al. Distal ureteral stone formation over migrated Hem-o-lok clip after robot-assisted partial nephrectomy[J]. Int J Surg Case Rep, 2019, 58: 201-4. doi:10.1016/j.ijscr.2019.03.024 |
| [20] | Shrivastava P, Nayak B, Singh P. Migrated hem-o-lok clips in the ureter: a rare cause of recurrent urinary tract infection[J]. BMJ Case Rep, 2017, 2017: bcr2016219143. doi:10.1136/bcr-2016-219143 |
| [21] | Chen S, Tu X, Xu M, et al. Bladder outlet obstruction induced by the compression of displaced hemipelvic prosthesis after pelvic reconstruction: a case report[J]. Urology, 2019, 133: e9-10. doi:10.1016/j.urology.2019.07.015 |
| [22] | Güzel Ö, Aykanat C, Aslan Y, et al. Does previous open or percutaneous renal stone surgery affect retrograde intrarenal surgery outcomes?[J]. Turk J Med Sci, 2021, 51(3): 1310-6. doi:10.3906/sag-2007-76 |
| [23] | Alkan E, Saribacak A, Ozkanli AO, et al. Retrograde intrarenal surgery in patients who previously underwent open renal stone surgery[J]. Minim Invasive Surg, 2015, 2015: 198765. doi:10.1155/2015/198765 |
| [24] | 张汉荣, 高清河, 杨镇有, 等.中国成人泌尿系结石相关危险因素的Meta分析[J].中华泌尿外科杂志, 2018,39(12):935-9. doi:10.3760/cma.j.issn.1000-6702.2018.12.012 |
| [25] | Ferraro PM, Taylor EN, Curhan GC. 24-hour urinary chemistries and kidney stone risk[J]. Am J Kidney Dis, 2024, 84(2): 164-9. doi:10.1053/j.ajkd.2024.02.010 |
| [26] | Geraghty R, Lovegrove C, Howles S, et al. Role of genetic testing in kidney stone disease: a narrative review[J]. Curr Urol Rep, 2024, 25(12): 311-23. doi:10.1007/s11934-024-01225-5 |
| [27] | 洪 扬,许清泉. 2024年泌尿系结石诊治进展[J].泌尿外科杂志,2025, 17(1): 3-10. |
| [28] | Wang G, Mi J, Bai J, et al. Non-coding RNAs in kidney stones[J]. Biomolecules, 2024, 14(2): 213. doi:10.3390/biom14020213 |
| [1] | 胡正飞,吕世栋,黄建锋,张林,黄婵桃,黎依文,黄文华,叶建平,魏强. 3D空间测量与传统CT规划在肾肿瘤微创手术中的对比[J]. 南方医科大学学报, 2018, 38(05): 606-. |
| [2] | 刘成山. 体外冲击波治疗右肾旋转不良结石1例报告[J]. 南方医科大学学报, 2004, 24(09): 1063-1063. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||