南方医科大学学报 ›› 2024, Vol. 44 ›› Issue (6): 1040-1047.doi: 10.12122/j.issn.1673-4254.2024.06.04
收稿日期:2023-12-25
出版日期:2024-06-20
发布日期:2024-07-01
通讯作者:
张建杏
E-mail:88519598@qq.com;Jianxing0710@sina.com
作者简介:胡家祺,主治医师,E-mail: 88519598@qq.com
基金资助:Received:2023-12-25
Online:2024-06-20
Published:2024-07-01
Contact:
Jianxing ZHANG
E-mail:88519598@qq.com;Jianxing0710@sina.com
摘要:
目的 探讨高流量鼻导管(HFNC)吸氧在妊娠合并心脏病患者剖宫产中的应用。 方法 本研究为单中心、单盲、随机临床试验。拟行剖宫产的妊娠合并心脏病患者被随机分为2组:HFNC组接受HFNC疗法(n=27,吸气流量30 L/min,氧浓度40%),传统吸氧(COT)组接受传统氧疗(n=31,通过鼻导管输送,氧流量5L/min)。主要观察指标为母体血氧饱和度下降(SpO2<94%,持续3 min以上,或PaO2/FIO2≤300 mmHg)。母体及新生儿不良事件数据分析中,对于近似高斯分布的连续变量,使用Student的t检验;对于倾斜分布的变量,进行Wilcoxon秩和检验。分类变量采用Fisher的确切检验或卡方检验。 结果 HFNC组中有7.4% 的孕妇(n=2/27)出现母体血氧饱和度下降,而COT组中有32.3%的孕妇(n=10/31)出现。在围手术期间,没有任何病例需要气管插管。HFNC组在术后白细胞增多的发生率较高(P<0.05),但没有母体发热及其他与炎症相关的症状。在母体次要结局指标(呼吸支持需求、母体重症监护室入住时间、术后呼吸系统并发症和心血管系统并发症)以及新生儿结局方面,两组之间无显著差异(P>0.05)。 结论 HFNC疗法显著降低了妊娠合并心脏病患者围手术期母体血氧饱和度下降的发生率,并且对母体或胎儿的短期临床结果没有不良影响。
胡家祺, 张建杏. 高流量鼻导管吸氧在妊娠合并心脏病患者剖宫产中的随机对照研究[J]. 南方医科大学学报, 2024, 44(6): 1040-1047.
Jiaqi HU, Jianxing ZHANG. High-flow nasal oxygen versus conventional oxygen therapy during cesarean section under neuraxial anesthesia in pregnant women with heart disease: a randomized controlled trial[J]. Journal of Southern Medical University, 2024, 44(6): 1040-1047.
| Characteristic | COT (n=31) | HFNC (n=27) | P |
|---|---|---|---|
| Age (year) | 29.0±0.9 | 30.4±1.1 | 0.28 |
| BMI (kg/m2) | 24.7±0.4 | 25.7±0.8 | 0.29 |
| Gestational age(weeks) | 36.7±2.2 | 35.8±3.0 | 0.18 |
| Primigravida | 14 (45.2%) | 10 (37%) | 0.53 |
| Primiparity | 22 (71%) | 17 (63%) | 0.52 |
| NYHA functional classification | 0.33 | ||
| I | 26 (83.9%) | 18 (66.7%) | |
| II | 1 (3.2%) | 1 (3.7%) | |
| III | 4 (12.9%) | 6 (22.2%) | |
| IV | 0 (0) | 2 (7.4%) | |
| mWHO classification | 0.82 | ||
| Missing# | 1 (3.2%) | 2 (7.4%) | |
| I | 7 (22.6%) | 4 (14.8%) | |
| II | 3 (9.7%) | 2 (7.4%) | |
| II-III | 5 (16.1%) | 4 (14.8%) | |
| III | 8 (25.8%) | 5 (18.5%) | |
| IV | 7 (22.6%) | 10 (37%) | |
| Hemoglobin (115-150 g/L) | 0.19 | ||
| Low | 15 (48.4%) | 18 (66.7%) | |
| Normal | 16 (51.6%) | 9 (33.3%) | |
| High | 0 (0) | 0 (0) | |
| Emergent CS | 11 (35.5%) | 8 (29.6%) | 0.64 |
| Maternal hypertension | 2 (6.5%) | 3 (11.1%) | 0.66 |
| Maternal gestational diabetes mellitus | 4 (12.9%) | 5 (18.5%) | 0.72 |
| Systolic pressure (mmHg) | 108.4±1.9 | 111.6±3.0 | 0.36 |
| Diastolic pressure (mmHg) | 68.4±1.6 | 66.1±2.3 | 0.42 |
| Heart rate (beat/min) | 81.5±2.4 | 85.4±2.5 | 0.28 |
| SpO2 (%) | 98.4±0.2 | 98.1±0.4 | 0.47 |
| Oxygen flow rate (L/min) ## | 0.64 | ||
| 3 | 29 (93.5%) | 25 (92.6%) | |
| 4 | 2 (6.5%) | 2 (7.4%) |
表1 患者术前临床基本资料
Tab.1 Baseline maternal characteristics
| Characteristic | COT (n=31) | HFNC (n=27) | P |
|---|---|---|---|
| Age (year) | 29.0±0.9 | 30.4±1.1 | 0.28 |
| BMI (kg/m2) | 24.7±0.4 | 25.7±0.8 | 0.29 |
| Gestational age(weeks) | 36.7±2.2 | 35.8±3.0 | 0.18 |
| Primigravida | 14 (45.2%) | 10 (37%) | 0.53 |
| Primiparity | 22 (71%) | 17 (63%) | 0.52 |
| NYHA functional classification | 0.33 | ||
| I | 26 (83.9%) | 18 (66.7%) | |
| II | 1 (3.2%) | 1 (3.7%) | |
| III | 4 (12.9%) | 6 (22.2%) | |
| IV | 0 (0) | 2 (7.4%) | |
| mWHO classification | 0.82 | ||
| Missing# | 1 (3.2%) | 2 (7.4%) | |
| I | 7 (22.6%) | 4 (14.8%) | |
| II | 3 (9.7%) | 2 (7.4%) | |
| II-III | 5 (16.1%) | 4 (14.8%) | |
| III | 8 (25.8%) | 5 (18.5%) | |
| IV | 7 (22.6%) | 10 (37%) | |
| Hemoglobin (115-150 g/L) | 0.19 | ||
| Low | 15 (48.4%) | 18 (66.7%) | |
| Normal | 16 (51.6%) | 9 (33.3%) | |
| High | 0 (0) | 0 (0) | |
| Emergent CS | 11 (35.5%) | 8 (29.6%) | 0.64 |
| Maternal hypertension | 2 (6.5%) | 3 (11.1%) | 0.66 |
| Maternal gestational diabetes mellitus | 4 (12.9%) | 5 (18.5%) | 0.72 |
| Systolic pressure (mmHg) | 108.4±1.9 | 111.6±3.0 | 0.36 |
| Diastolic pressure (mmHg) | 68.4±1.6 | 66.1±2.3 | 0.42 |
| Heart rate (beat/min) | 81.5±2.4 | 85.4±2.5 | 0.28 |
| SpO2 (%) | 98.4±0.2 | 98.1±0.4 | 0.47 |
| Oxygen flow rate (L/min) ## | 0.64 | ||
| 3 | 29 (93.5%) | 25 (92.6%) | |
| 4 | 2 (6.5%) | 2 (7.4%) |
| Outcomes | COT (n=31) | HFNC (n=27) | P |
|---|---|---|---|
| Level of block (Above T6) | 2 (6.5%) | 0(0) | 0.37 |
| Volume of local anesthetics (0.5% Bupivacaine, mL) | 1.84±0.03 | 1.89±0.03 | 0.23 |
| Intravenous opioid adjuvant | 2 (6.5%) | 1 (3.7%) | 1.00 |
| Arrhythmia | 18 (58.1%) | 16 (59.3%) | 0.57 |
| Nausea or vomiting | 3 (9.7%) | 0 (0) | 0.24 |
| Shivering | 1 (3.2%) | 0 (0) | 1.00 |
| Treatment of hypotension | 9 (29%) | 9 (33.3%) | 0.78 |
| Furosemide | 0 (0) | 3 (11.1%) | 0.10 |
| Blood loss (mL) | 240.3±45.2 | 247±77.1 | 0.68 |
| Duration of surgery (min) | 69.8±16.3 | 70.3±19.8 | 0.91 |
| Reduced respiratory rate# | 15 (48.4%) | 16 (59.3%) | 0.41 |
| SpO2≤94%## | 2 (6.5%) | 0 (0) | 0.49 |
| Oxygen partial pressure increase(T2-T1, mmHg)### | 51.5±37.9 | 83.7±41.7 | <0.01 |
| Oxygen partial pressure increase(T3-T1, mmHg)### | 47.9±48.1 | 88.5±40.7 | <0.01 |
| Maternal desaturation (PaO2:FIO2, T2) ### | 5 (16.1%) | 1 (3.7%) | 0.20 |
| Maternal desaturation (PaO2:FIO2,T3) ### | 10(32.3%) | 2(7.4%) | 0.02 |
表2 患者术中各项临床指标
Tab.2 Intraoperative clinical and parturition conditions of the mothers who gave birth under neuraxial anesthesia
| Outcomes | COT (n=31) | HFNC (n=27) | P |
|---|---|---|---|
| Level of block (Above T6) | 2 (6.5%) | 0(0) | 0.37 |
| Volume of local anesthetics (0.5% Bupivacaine, mL) | 1.84±0.03 | 1.89±0.03 | 0.23 |
| Intravenous opioid adjuvant | 2 (6.5%) | 1 (3.7%) | 1.00 |
| Arrhythmia | 18 (58.1%) | 16 (59.3%) | 0.57 |
| Nausea or vomiting | 3 (9.7%) | 0 (0) | 0.24 |
| Shivering | 1 (3.2%) | 0 (0) | 1.00 |
| Treatment of hypotension | 9 (29%) | 9 (33.3%) | 0.78 |
| Furosemide | 0 (0) | 3 (11.1%) | 0.10 |
| Blood loss (mL) | 240.3±45.2 | 247±77.1 | 0.68 |
| Duration of surgery (min) | 69.8±16.3 | 70.3±19.8 | 0.91 |
| Reduced respiratory rate# | 15 (48.4%) | 16 (59.3%) | 0.41 |
| SpO2≤94%## | 2 (6.5%) | 0 (0) | 0.49 |
| Oxygen partial pressure increase(T2-T1, mmHg)### | 51.5±37.9 | 83.7±41.7 | <0.01 |
| Oxygen partial pressure increase(T3-T1, mmHg)### | 47.9±48.1 | 88.5±40.7 | <0.01 |
| Maternal desaturation (PaO2:FIO2, T2) ### | 5 (16.1%) | 1 (3.7%) | 0.20 |
| Maternal desaturation (PaO2:FIO2,T3) ### | 10(32.3%) | 2(7.4%) | 0.02 |
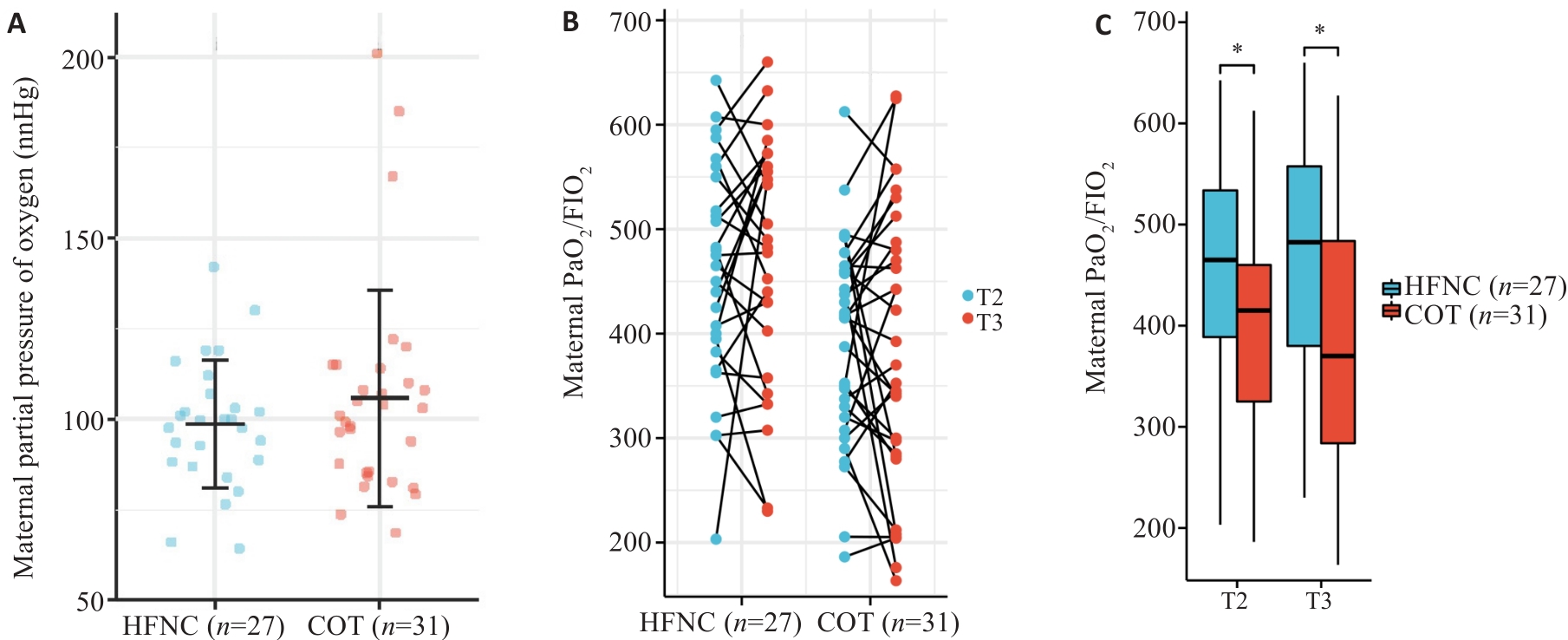
图2 母体动脉血氧分压变化
Fig.2 Levels of maternal partial pressure of oxygen during the operation. A: Maternal partial pressure of oxygen at T1 (baseline). B: Pairing diagram of maternal partial pressure of oxygen at T2 (at delivery of the fetus) and T3 (at the end of the operation). Among them, there were 2 cases in the HFNC group and 9 cases in the CON group, and the value at T3 was lower than that at T2 and was less than 300. C: Box-plot of maternal partial pressure of oxygen at T2 and T3. *P<0.05.
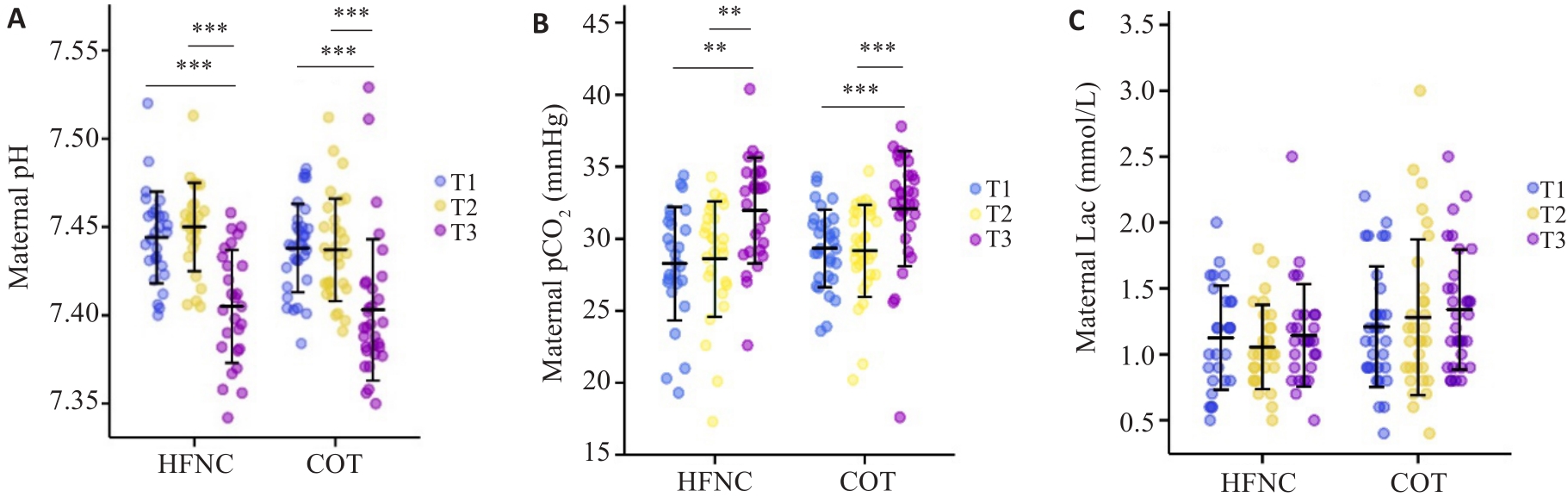
图3 母体动脉血气pH、pCO2和Lac散点图
Fig.3 Scatter plot of maternal pH, pCO2 and Lac. A: Maternal pH values. B: Maternal partial pressure of carbon dioxide. C: Maternal lactate values. **P<0.01; ***P<0.001.
| Variables | COT (n=31) | HFNC (n=27) | P |
|---|---|---|---|
| Respiratory complications | 1 (3.2%) | 2 (7.4%) | 0.59 |
| Cardiovascular complications | 5 (16.1%) | 8 (29.6%) | 0.34 |
| Pyrexia | 1 (3.2%) | 1 (3.7%) | 1.00 |
| Pelvic adhesion | 8 (25.8%) | 10 (37%) | 0.40 |
| Postoperative leukocytosis# | 12 (38.7%) | 18 (66.7%) | 0.04 |
| Need for respiratory support## | 11(35.5%) | 13(48.1%) | 0.43 |
| Maternal ICU admission | 7 (22.6%) | 10 (37%) | 0.26 |
| Admission time in ICU (h)### | 78.42 (32, 94) | 142.43 (94, 253) | 0.11 |
| Length of stay (d) | 9.5±4.9 | 10.3±4.4 | 0.50 |
| Postoperative hospital stay (d) | 5.8±2.3 | 7±3.6 | 0.16 |
表3 母体次要指标
Tab.3 Maternal secondary outcomes
| Variables | COT (n=31) | HFNC (n=27) | P |
|---|---|---|---|
| Respiratory complications | 1 (3.2%) | 2 (7.4%) | 0.59 |
| Cardiovascular complications | 5 (16.1%) | 8 (29.6%) | 0.34 |
| Pyrexia | 1 (3.2%) | 1 (3.7%) | 1.00 |
| Pelvic adhesion | 8 (25.8%) | 10 (37%) | 0.40 |
| Postoperative leukocytosis# | 12 (38.7%) | 18 (66.7%) | 0.04 |
| Need for respiratory support## | 11(35.5%) | 13(48.1%) | 0.43 |
| Maternal ICU admission | 7 (22.6%) | 10 (37%) | 0.26 |
| Admission time in ICU (h)### | 78.42 (32, 94) | 142.43 (94, 253) | 0.11 |
| Length of stay (d) | 9.5±4.9 | 10.3±4.4 | 0.50 |
| Postoperative hospital stay (d) | 5.8±2.3 | 7±3.6 | 0.16 |
| Outcomes | COT (n=31) | HFNC (n=27) | P |
|---|---|---|---|
| Intubation | 1 (3.2%) | 5 (18.5%) | 0.09 |
| Mechanical ventilation | 5 (16.1%) | 6 (22.2%) | 0.74 |
| Neonatal death≤72 hour | 0 (0) | 1 (3.7%) | 0.47 |
| Severe respiratory complication# | 9 (29%) | 12 (44.4%) | 0.22 |
| Admission to intermediate care nursery or NICU | 13 (41.9%) | 16 (59.3%) | 0.19 |
| Admission time in ICU (h)## | 212 (117, 364) | 215 (70, 541) | 0.91 |
| Umbilical cord around the neck | 6 (19.4%) | 3 (11.1%) | 0.48 |
| Gestational age (week) | 0.33 | ||
| >36 | 24(77.4%) | 19 (70.4%) | |
| 32-36 | 6(19.4%) | 4 (14.8%) | |
| 28-32 | 1(3.2%) | 4 (14.8%) | |
| Birth weight (kg) | 2757.3±489.8 | 2558.1±649.2 | 0.19 |
| Body length (cm) | 47.8±2.9 | 46.7±3.9 | 0.23 |
| Head circumference (cm) | 33.1±2 | 32.6±2.1 | 0.36 |
| 1 min Apgar≤7 | 0 (0) | 3 (11.1%) | 0.10 |
| 5 min Apgar≤7 | 0 (0) | 1 (3.7) | 0.47 |
| Hyperbilirubinemia | 8 (25.8%) | 9 (33.3%) | 0.53 |
| Umbilical vein gas analysis### UV pH (7.23-7.44) | 1.00 | ||
| Low level | 1 (3.3%) | 0 (0) | |
| Normal | 29 (96.7%) | 26 (100%) | |
| High level | 0 (0) | 0 (0) |
表4 新生儿各项临床指标
Tab.4 Neonatal outcomes
| Outcomes | COT (n=31) | HFNC (n=27) | P |
|---|---|---|---|
| Intubation | 1 (3.2%) | 5 (18.5%) | 0.09 |
| Mechanical ventilation | 5 (16.1%) | 6 (22.2%) | 0.74 |
| Neonatal death≤72 hour | 0 (0) | 1 (3.7%) | 0.47 |
| Severe respiratory complication# | 9 (29%) | 12 (44.4%) | 0.22 |
| Admission to intermediate care nursery or NICU | 13 (41.9%) | 16 (59.3%) | 0.19 |
| Admission time in ICU (h)## | 212 (117, 364) | 215 (70, 541) | 0.91 |
| Umbilical cord around the neck | 6 (19.4%) | 3 (11.1%) | 0.48 |
| Gestational age (week) | 0.33 | ||
| >36 | 24(77.4%) | 19 (70.4%) | |
| 32-36 | 6(19.4%) | 4 (14.8%) | |
| 28-32 | 1(3.2%) | 4 (14.8%) | |
| Birth weight (kg) | 2757.3±489.8 | 2558.1±649.2 | 0.19 |
| Body length (cm) | 47.8±2.9 | 46.7±3.9 | 0.23 |
| Head circumference (cm) | 33.1±2 | 32.6±2.1 | 0.36 |
| 1 min Apgar≤7 | 0 (0) | 3 (11.1%) | 0.10 |
| 5 min Apgar≤7 | 0 (0) | 1 (3.7) | 0.47 |
| Hyperbilirubinemia | 8 (25.8%) | 9 (33.3%) | 0.53 |
| Umbilical vein gas analysis### UV pH (7.23-7.44) | 1.00 | ||
| Low level | 1 (3.3%) | 0 (0) | |
| Normal | 29 (96.7%) | 26 (100%) | |
| High level | 0 (0) | 0 (0) |
| 1 | Okoth K, Chandan JS, Marshall T, et al. Association between the reproductive health of young women and cardiovascular disease in later life: umbrella review[J]. BMJ, 2020, 371: m3502. |
| 2 | Ramlakhan KP, Johnson MR, Roos-Hesselink JW. Pregnancy and cardiovascular disease[J]. Nat Rev Cardiol, 2020, 17(11): 718-31. |
| 3 | Hu KM, Hong AS. Resuscitating the crashing pregnant patient[J]. Emerg Med Clin North Am, 2020, 38(4): 903-17. |
| 4 | Hoefnagel A, Yu A, Kaminski A. Anesthetic complications in pregnancy[J]. Crit Care Clin, 2016, 32(1): 1-28. |
| 5 | Ducsay CA, Goyal R, Pearce WJ, et al. Gestational hypoxia and developmental plasticity[J]. Physiol Rev, 2018, 98(3): 1241-334. |
| 6 | Tong W, Giussani DA. Preeclampsia link to gestational hypoxia[J]. J Dev Orig Health Dis, 2019, 10(3): 322-33. |
| 7 | Cheng C, Liao AH, Chen CY, et al. A systematic review with network meta-analysis on mono strategy of anaesthesia for preeclampsia in Caesarean section[J]. Sci Rep, 2021, 11(1): 5630. |
| 8 | Hu JQ, Ye YX, Lu AY, et al. Pregnancy outcomes in patients with heart disease in China[J]. Am J Cardiol, 2020, 125(11): 1718-24. |
| 9 | Rex S, Devroe S. Anesthesia for pregnant women with pulmonary hypertension[J]. Curr Opin Anaesthesiol, 2016, 29(3): 273-81. |
| 10 | Meng ML, Arendt KW. Obstetric anesthesia and heart disease: practical clinical considerations[J]. Anesthesiology, 2021, 135(1): 164-83. |
| 11 | Corcione N, Karim H, Mina B, et al. Non-invasive ventilation during surgery under neuraxial anaesthesia: a pathophysiological perspective on application and benefits and a systematic literature review[J]. Anaesthesiol Intensive Ther, 2019, 51(4): 289-98. |
| 12 | Lapinsky SE. Management of acute respiratory failure in pregnancy[J]. Semin Respir Crit Care Med, 2017, 38(2): 201-7. |
| 13 | Rochwerg B, Einav S, Chaudhuri D, et al. The role for high flow nasal cannula as a respiratory support strategy in adults: a clinical practice guideline[J]. Intensive Care Med, 2020, 46(12): 2226-37. |
| 14 | Chaudhuri D, Granton D, Wang DX, et al. High-flow nasal Cannula in the immediate postoperative period: a systematic review and meta-analysis[J]. Chest, 2020, 158(5): 1934-46. |
| 15 | Rochwerg B, Granton D, Wang DX, et al. High-flow nasal cannula compared with conventional oxygen therapy for acute hypoxemic respiratory failure: author’s reply[J]. Intensive Care Med, 2019, 45(8): 1171. |
| 16 | Zhao HY, Wang HX, Sun F, et al. High-flow nasal cannula oxygen therapy is superior to conventional oxygen therapy but not to noninvasive mechanical ventilation on intubation rate: a systematic review and meta-analysis[J]. Crit Care, 2017, 21(1): 184. |
| 17 | Shippam W, Preston R, Douglas J, et al. High-flow nasal oxygen vs. standard flow-rate facemask pre-oxygenation in pregnant patients: a randomised physiological study[J]. Anaesthesia, 2019, 74(4): 450-6. |
| 18 | Tan P, Dennis AT. High flow humidified nasal oxygen in pregnant women[J]. Anaesth Intensive Care, 2018, 46(1): 36-41. |
| 19 | Tan PCF, Millay OJ, Leeton L, et al. High-flow humidified nasal preoxygenation in pregnant women: a prospective observational study[J]. Br J Anaesth, 2019, 122(1): 86-91. |
| 20 | Preston KL, Butler P, Mudannayake R. Determining time to preoxygenation using high-flow nasal oxygen in pregnant women[J]. J Clin Anesth, 2020, 62: 109722. |
| 21 | Zimmerman ME, Hodgson DS, Bello NM. Effects of oxygen insufflation rate, respiratory rate, and tidal volume on fraction of inspired oxygen in cadaveric canine heads attached to a lung model[J]. Am J Vet Res, 2013, 74(9): 1247-51. |
| 22 | Mohamed TM, Ahmed TM. Chestnut’s obstetric anesthesia: principles and practice, 6th ed[J]. Anesth Analg, 2019, 129(5):1213. |
| 23 | Chatmongkolchart S, Prathep S. Supplemental oxygen for Caesarean section during regional anaesthesia[J]. Cochrane Database Syst Rev, 2016, 3(3): CD006161. |
| 24 | Siriussawakul A, Triyasunant N, Nimmannit A, et al. Effects of supplemental oxygen on maternal and neonatal oxygenation in elective cesarean section under spinal anesthesia: a randomized controlled trial[J]. Biomed Res Int, 2014, 2014: 627028. |
| 25 | Pacheco LD, Saad AF, Saade G. Early acute respiratory support for pregnant patients with coronavirus disease 2019 (COVID-19) infection[J]. Obstet Gynecol, 2020, 136(1): 42-5. |
| 26 | Cole DE, Taylor TL, McCullough DM, et al. Acute respiratory distress syndrome in pregnancy[J]. Crit Care Med, 2005, 33(10 ): S269-78. |
| 27 | Ukah UV, de Silva DA, Payne B, et al. Prediction of adverse maternal outcomes from pre-eclampsia and other hypertensive disorders of pregnancy: a systematic review[J]. Pregnancy Hypertens, 2018, 11: 115-23. |
| 28 | Millman AL, Payne B, Qu ZG, et al. Oxygen saturation as a predictor of adverse maternal outcomes in women with preeclampsia[J]. J D’obstetrique Gynecol Du Can, 2011, 33(7): 705-14. |
| 29 | Crooks CJ, West J, Morling JR, et al. Pulse oximeter measurements vary across ethnic groups: an observational study in patients with COVID-19[J]. Eur Respir J, 2022, 59(4): 2103246. |
| 30 |
Fuentes S, Chowdhury YS. Fraction of Inspired Oxygen. 2022 Nov 29. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. PMID:.
pmid: 32809702 |
| 31 | McDonald CF. Low-flow oxygen: how much is your patient really getting[J]? Respirology, 2014, 19(4): 469-70. |
| 32 |
Sharma S, Danckers M, Sanghavi DK, et al. High-Flow Nasal Cannula. Updated 2023 Apr 6. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. PMID:.
pmid: 30252327 |
| 33 | Sorg ME, Chatburn RL. Comparison of FIO2 Delivery With Low Flow vs High Flow Cannulas: A Simulation Study [J]. Respirat Care, 2021, 66(): 3597405. |
| 34 | Feiner JR, Weiskopf RB. Evaluating pulmonary function: an assessment of PaO2/FIO2[J]. Crit Care Med, 2017, 45(1): e40-e48. |
| 35 | Collins JA, Rudenski A, Gibson J, et al. Relating oxygen partial pressure, saturation and content: the haemoglobin-oxygen dissociation curve[J]. Breathe, 2015, 11(3): 194-201. |
| 36 | Pelaia C, Armentaro G, Lupia C, et al. Effects of high-flow nasal Cannula on right heart dysfunction in patients with acute-on-chronic respiratory failure and pulmonary hypertension[J]. J Clin Med, 2023, 12(17): 5472. |
| 37 | Ahuja V, Gombar S, Jaswal S, et al. Effect of maternal oxygen inhalation on foetal free radical activity: a prospective, randomized trial[J]. Acta Anaesthesiol Scand, 2018, 62(1): 26-37. |
| 38 | Raghuraman N, Temming LA, Doering MM, et al. Maternal oxygen supplementation compared with room air for intrauterine resuscitation: a systematic review and meta-analysis[J]. JAMA Pediatr, 2021, 175(4): 368-76. |
| 39 | Cohen B, Schacham YN, Ruetzler K, et al. Effect of intraoperative hyperoxia on the incidence of surgical site infections: a meta-analysis[J]. Br J Anaesth, 2018, 120(6): 1176-86. |
| 40 | Klingel ML, Patel SV. A meta-analysis of the effect of inspired oxygen concentration on the incidence of surgical site infection following cesarean section[J]. Int J Obstet Anesth, 2013, 22(2): 104-12. |
| 41 | Dahlke JD, Mendez-Figueroa H, Rouse DJ, et al. Evidence-based surgery for cesarean delivery: an updated systematic review[J]. Am J Obstet Gynecol, 2013, 209(4): 294-306. |
| [1] | 王志鹏,马珏,王晟,郁丽娜,韦锦锋,徐金东. 七氟醚与喉罩在妊娠合并心脏病产妇剖宫产手术中的应用[J]. 南方医科大学学报, 2018, 38(02): 229-. |
| 阅读次数 | ||||||
|
全文 |
|
|||||
|
摘要 |
|
|||||
